Abstract
Purpose of Review
The study aims to assess the current scientific evidence on the clinical performance of all-ceramic dental restorations.
Recent Findings
Silica-based and oxide-based ceramics provide esthetic treatment alternatives but rely on proper case selection and handling. Clinical long-term success rates are generally high for both tooth-supported and implant-supported restorations. Due to limited flexural strength and high brittleness, silica-based ceramics are limited in respect to clinical indications and their success greatly depends on resin bonding for final insertion. High-strength oxide-based ceramics can be inserted with conventional cements and reveal high success rates. More recently developed materials, such as resin matrix ceramics, zirconia-reinforced silicate ceramics, and monolithic translucent zirconia, reveal promising properties in the laboratory. However, they lack scientific validation through long-term clinical trials.
Summary
Established silica-based and oxide-based ceramic materials demonstrate high long-term clinical survival rates; however, recently developed ceramics need further assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Porcelain-fused-to-metal (PFM) restorations have long been considered the gold standard in prosthetic dentistry for full-coverage crowns and multi-unit fixed dental prostheses (FDPs). Patients’ and dentists’ growing demand for more esthetic, metal-free, and biocompatible restorations has led to the development of all-ceramic materials. Proper selection of ceramic materials based on specific esthetic and functional needs is essential for clinical longevity of dental restorations, especially in light of the increasing number of new materials available today [1].
Some of these newly developed materials provide novel formulations and compositions outside of previously established dental ceramic material categories. As classification systems are useful for communication and educational purposes, updated versions have become recently available. Current ceramic materials used in dentistry can be classified into three general groups: resin matrix ceramics, silicate ceramics, and oxide ceramics [2].
Resin matrix ceramics (RMCs) were included in accordance with the 2013 version of the ADA code on Dental Procedures and Nomenclature, which defines the term “porcelain/ceramic” as pressed, fired, polished, or milled materials containing predominantly inorganic refractory compounds that may include porcelains, glasses, ceramics, and glass-ceramics. They can be divided into two sub-groups: resin-based ceramics and hybrid ceramics. Both of them show better loading capacity, modulus of elasticity, and milling properties when compared to traditional glass-ceramics [3, 4].
Silica-based ceramics are mainly non-metallic inorganic ceramic materials that contain a glass phase. They are divided into feldspathic and silicate ceramics.
Traditional feldspathic ceramics are described as the most translucent and esthetic material. Due to their inherent brittleness and low flexural strength, adhesive bonding with composite resin luting agents is recommended to enhance retention, fracture resistance, and longevity [5]. Lithium silicate ceramics are heat-pressed or computer-aided design (CAD)/computer-aided manufacturing (CAM)-fabricated glass-ceramic materials with a crystalline phase consisting of lithium disilicate and lithium orthophosphate, which increases fracture resistance without negatively influencing translucency. This material is used for both high-strength cores for veneer porcelain support and full-contour (monolithic) restorations.
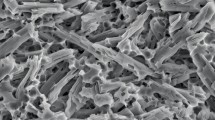
High-strength oxide ceramics are non-metallic inorganic materials that typically do not contain any glass phase. The main feature of their fine-grain crystalline structure is strength and fracture toughness. In dentistry, this group commonly features aluminum oxide (“alumina”) and zirconium dioxide (“zirconia”) ceramics, including newer, more translucent zirconia versions [6]. Initially, these metal oxide ceramics were solely intended for the fabrication of copings and frameworks to support weaker, but more esthetic and customized veneering porcelains. They were monochromatic in color and far less translucent than silica-based ceramics. With structural changes for improved esthetics and shade customization options, monolithic zirconia restorations have most recently become extremely popular among practicing dentists. The main advantages of monolithic restorations are considered to be no veneering ceramic chipping, faster and less expensive production through CAD/CAM processes, and reduced thickness for less invasive tooth preparation [7]. Combining these ceramic materials with optimized resin-bonding protocols offers novel and less invasive clinical treatment options. One of these options is the zirconia-based resin-bonded fixed dental prosthesis (RBFDP), which provides very high clinical success rates when recommended protocols are followed properly [8]. A major disadvantage of metal-based RBFDPs, grayish discoloration of the abutment teeth, is thereby eliminated.
In light of the new material developments and rapid market changes, the main objective of this article was to assess and discuss the most recent literature on the clinical performance of all-ceramic restorations and to provide an update on proper material selection.
Materials and Methods
Search Strategy
A MEDLINE (PubMed) and Cochran Library search from October 2013 to October 2016 was conducted for English language articles in dental journals by two reviewers.
Clinical studies meeting the following criteria were included: (1) studies related to restorations made of feldspathic ceramic, hybrid ceramic, silicate ceramic, and oxide ceramics; (2) prospective, retrospective, or randomized controlled trials conducted in humans; and (3) studies with a follow-up of 5 years.
For this purpose, Mesh terms and free text words were used. The detailed search terms were as follows: ((clinical[tw]) AND (((((((((((dental prosthesis[tw]) OR “Dental prosthesis”[Mesh]) OR dental restoration*[tw]) OR dental implant*[tw]) OR implant supported restoration*[tw]) OR crown*[tw]) OR fixed dental prosthesis[tw]) OR dental veneers[tw]) OR inlay*[tw]) OR onlay*[tw])) AND ((((((((Ceramics[Mesh]) OR ceramic*[tw]) OR resin-based material*[tw]) OR zirconium[tw]) OR Zirconium[Mesh]) OR zirconia[tw]) OR zirconium oxide[tw]) OR porcelain[tw])).
The filters applied were publication date from October 1, 2013 to October 1, 2016 and English language.
A specialized librarian supported the literature search. Finally, the electronic search was complemented by a manual search. All titles obtained were screened for additional relevant clinical studies.
Results
The electronic database search revealed 991 titles. Full-text screening was carried out for 72 studies, yielding 57 articles that complied with the inclusion criteria (Figs. 1 and 2).
From the final 57 articles selected, the specific ceramic material, restoration type, mean follow-up, and number of patients were analyzed (Table 1). The great inhomogeneity of the studies and variety of applied materials and methods did not allow for statistical assessment through meta-analyses.
Discussion
Resin Matrix Ceramics
No clinical studies on the use of RMCs, resin-based ceramics or hybrid ceramics, could be identified. As this material group is new to the market, clinical evidence to support their performance use in practice is missing.
Several polymer and indirect composite resin materials may have similar physical properties but do not specifically belong into this category due to their composition, filler particle size, content, and distribution. The clinical success of such polymer crowns was assessed in one clinical study, which compared three groups: (1) polymer composite resin with a glass fiber framework, (2) polymer composite resin without frameworks stabilization, and (3) PFM crowns as the control. After a median follow-up of 4 years, the clinical survival of posterior polymer crowns with and without a glass fiber framework was not significantly different from the PFM group. However, the number of catastrophic failures of polymer composite crowns was higher than that of PFM crowns [9]. Those results cannot be directly applied to RMCs, but it can be assumed that their clinical behavior is somewhat similar. It is noteworthy, however, that one manufacturer of a RMC product for chair-side CAD/CAM fabrication recently retracted its initial indication for full-coverage crowns and limited it to inlays and onlays. Discussions about the use of some RMCs for full-coverage restorations ensued, highlighting the importance of clinical trials being performed before new materials are being recommended for clinical practice.
Silicate Ceramics
According to recommendations by the Society for Dental Ceramics (SDC), ceramic materials with a fracture strength below 350 MPa must be adhesively bonded [10]. Most silicate ceramics fall into this category. They are characterized by their susceptibility to etching with hydrofluoric acid (HF) and high translucency, ensuring optimal esthetics, a natural appearance, and reliable clinical performance [11]. Popular representatives of this material group are feldspathic, leucite-reinforced glass, and lithium silicate ceramics.
Feldspathic Ceramics
There are numerous studies demonstrating high clinical survival rates of feldspathic ceramic restorations, despite having the lowest fracture strength of all dental ceramics. They are also referred to as feldspathic “porcelain.” Otto and Mormann reported a 95% survival rate for CAD/CAM feldspathic ceramic shoulder crowns on molars and a 94.7% on premolars after up to 12 years [12]. For endo-crowns, survival rates were 90.5% for molars and 75% for premolars. The longevity of Vita Mark II (Vita Zahnfabrik, Bad Sackingen, Germany) feldspathic ceramic restorations made with the CEREC 3 (Sirona, Bensheim, Germany) CAD/CAM system seems to be acceptable for use in private practice, except for premolar endo-crowns, which had a substantially higher risk for failure. Dierens and coworkers reported on the prosthetic survival and complication rate of single-implant crowns with a mean follow-up of 18.5 years. Six out of 33 feldspathic ceramic crowns, 7 of 23 PFM crowns, and 3 of 3 gold acrylic crowns needed to be replaced. Despite the developmental phase of these prosthetic procedures at the time, 73% of the crowns were still in function after more than 16 years [13].
Feldspathic ceramics are the preferred materials for resin-bonded laminate veneers due to their inherent optical properties. This type of restoration typically features a minimally invasive preparation design and relies on resin bonding. Adequate pretreatment of both tooth and ceramic bonding surfaces is key for clinical success, which is very high, given that clinical protocols are followed closely. In a recent systematic review of silica ceramic laminate veneers, Morimoto et al. found cumulative survival rates of 89% at a median follow-up period of 9 years [14].
Leucite-Reinforced Glass-Ceramics
A clinical evaluation of ceramic inlay and onlays made of sintered (Duraceram, Dentsply Degussa, Dentsply International Inc., PA, USA) and pressable leucite-reinforced glass-ceramics (IPS Empress, Ivoclar Vivadent, Schaan, Liechstenstein) after 12-year follow-up reported that from a total of 48 restorations, 7 were fractured, 8 presented secondary caries, and 9 showed unacceptable defects at the restoration margin [15]. A 5-year retrospective study on CAD/CAM partial coverage posterior ceramic restorations showed a survival rate of 96% for CEREC Blocs and a 94.6% for Empress CAD Blocs, respectively. Ceramic fracture was significantly more prevalent on non-vital teeth [16]. A similar study by Guess and colleagues reported a survival rate of 100% for pressed partial coverage restorations (PCRs) made of lithium disilicate (IPS e.max, Ivoclar Vivadent) and a 97% for CAD/CAM PCRs made from leucite-reinforced glass-ceramics (ProCAD) after 7 years.
Forty-nine single-retainer cantilever ceramic RBFDPs made from IPS Empress (n = 3) and IPS e.max Press (n = 46) had a survival rate of 100% after 6 years. All restorations were adhesively bonded to the abutment teeth. Chipping of the ceramic was found in 5.7% [17].
Guess and colleagues reported 100% survival rate for full veneer restorations and 97.6% for overlap veneers after 7 years. All restorations were made of leucite-reinforced glass-ceramic [18]. Laminate veneers are a predictable treatment option that provides excellent results but have a higher risk of failure in patients with bruxism activity. Wearing occlusal guards reduces the risk of fractures [19].
This material group has been quite popular, especially for anterior crowns and posterior inlays/onlays. As with all silica-based ceramics, resin bonding with composite resin luting agents after pretreatment of the tooth and ceramic surfaces is necessary for clinical success. In recent years, leucite-reinforced glass-ceramics were largely replaced by lithium silicate ceramics, which have better physical properties while still providing excellent optical properties.
Lithium Silicate Ceramics
Lithium silicate ceramics have become quite popular for a number of indications, especially crowns, inlays, and onlays. With a biaxial flexural strength of around 407 ± 45 MPa, they are considered the strongest silica-based ceramics in dentistry. Favorable physical properties have led clinicians and researchers to use the material in a variety of clinical indications, sometimes stretching its applications beyond its capabilities. As an example, a recent clinical study on double-crown-retained overdentures with metal and metal-free secondary crowns and frameworks made of glass fiber-reinforced composite material after 14 years concluded that lithium silicate ceramics should not be recommended for primary crowns [20]. As one might expect, success rates are much better when such materials are used for more conventional indications. Toman and Toksavul showed a cumulative survival rate of 87.1% for 121 lithium disilicate all-ceramic crowns after a mean follow-up of 104.6 months. Failure rates were significantly higher for endodontically treated teeth [21]. Simeone and Gracis reported a cumulative survival rate of 98.2% on 275 veneered lithium disilicate single crowns after 11-year follow-up. Of the five failed crowns, three reported veneer ceramic chippings and two core fractures [22]. Cumulative survival rates of tooth-supported and implant-supported lithium disilicate restorations ranged from 95.46 to 100%, while cumulative success rates ranged from 95.39 to 100%, in a study by Fabri and coworkers [11]. They concluded that lithium disilicate restorations are effective and reliable in the short and mid-term. A retrospective study on the clinical outcomes of different types of tooth-supported bilayer lithium disilicate all-ceramic restorations after up to 5 years demonstrated excellent mid-term reliability. Failures occurred mainly in the first 3 months after cementation, and the main reasons were ceramic chipping and fracture. Due to higher failure risk in those categories, the authors caution their use for FDPs, 2-unit or multiple-unit splinted crowns, and single molar crowns [23]. Huettig and Gehrke reported on early complications and performance of 327 heat-pressed lithium disilicate crowns up to 5 years. They concluded that besides careful luting, clinicians should consider patients’ biological prerequisites (degree of caries, oral hygiene) to reach optimal success with these crowns [24].
Although the manufacturers’ guidelines for lithium disilicate recommend a 1.0-mm butt joint cervical margin for full-coverage restorations, Valenti and Valenti reported an overall survival probability of 96.1% after up to 9 years with feather-edge marginal preparations. The elaboration method for the restorations (pressed or milled) was not specified. The great popularity of lithium disilicate ceramic materials is based on their favorable optical qualities paired with good physical properties. Excellent success rates are well documented in the recent literature, especially for single-unit restorations. For multi-unit reconstructions and crowns on endodontically treated teeth and molars, however, success rates are somewhat lower [25].
Oxide Ceramics
Oxide ceramics (alumina and zirconia) are characterized by excellent mechanical properties, which are far greater than those of silica-based ceramics. These materials, fabricated with CAD/CAM technologies, are mostly indicated for crowns, implant components, and FDPs with multiple units in anterior and posterior areas. The low translucency of some polycrystalline materials may be an esthetic disadvantage in certain clinical situations but simplifies the treatment of discolored abutments [11]. They are typically used as copings and frameworks and veneered with a feldspathic ceramic to achieve optimal, tooth-like esthetics.
Aluminum Oxide
Glass-infiltrated aluminum oxide core ceramics (InCeram Alumina, VITA Zahnfabrik, Bad Säckingen, Germany) were introduced in 1989, followed by the stronger densely sintered alumina (Procera Alumina, Nobel Biocare, Zurich, Switzerland). InCeram Alumina ceramic reveals a flexural strength of 500 MPa and is recommended for crowns and anterior three-unit FDPs. Glass-infiltrated alumina crowns can be considered a reliable treatment option for posterior teeth, in combination with adhesive as well as conventional cementation [26].
In a practice-based clinical evaluation of ceramic single crowns made of bilayered alumina cores (n = 192), zirconia cores (n = 17), and monolayer-pressed lithium disilicate-zirconia (n = 11), the authors reported survival rates of ceramic single crowns of 95.1% at 5 years and 92.8% at 10 years. Core fractures in posterior areas (7.4% after 3.3 years) were the most common complication that prompted replacement [27]. In a clinical evaluation of anterior all-ceramic RBFDPs, prostheses with a conventional two-retainer design and 8-year follow-up revealed 85.2% success. Patient selection was identified as key for clinical success [28]. All-ceramic cantilever RBFDPs are considered a promising alternative to metal-ceramic RBFDPs for replacing missing anterior incisors [29].
Aluminum oxide-based implant abutments show 100% survival rate after a mean observation period of 7.2 years [30•]. No recent studies were found on crowns and FDPs made from glass-infiltrated and densely sintered alumina. This is due to the fact that, in recent years, alumina ceramics were largely replaced by the currently extremely popular zirconia ceramics, which provide superior and unique physical properties.
Zirconium Oxide
Tooth-Supported Zirconia Single Crowns
Over the last few years, three articles reported on the survival rate of tooth-supported porcelain-fused-to zirconia (PFZ) single crowns. Ozer and colleagues reported excellent long-term success of PFZ single crowns with three different coping systems (Lava, 3M ESPE; Procera, Nobel Biocare; and Katana, Noritake) versus PFM crowns, evaluated by 13 private practitioners over a mean period of 7.4 years. There were over 1000 units in each experimental group [31••]. Another practice-based clinical evaluation by Rinke and coworkers on the survival and success of PFM and PFZ single crowns found no statistical difference between both groups [32]. For predoctoral dental students, zirconia single crowns had a 89% survival and 80% success rate after a mean follow-up of 3.88 years [33]. Only one study reported on the use of monolithic zirconia crowns; however, the material used in this investigation cannot be recommended for posterior tooth restorations, and it is not distributed anymore [34]. Assessing the capabilities of the material for other clinical applications than restorations, one study suggested that zirconia endodontic posts represent an esthetic alternative to metal posts [35].
Tooth-Supported Single-Unit and Multi-Unit Zirconia Restorations
Guncu and colleagues reported on zirconia-based single and multi-unit crowns up to 5 years in function and found a cumulative survival rate of 98.1%. No zirconia core fractures were observed, but 12 veneer fractures required crown replacement [36].
A retrospective cohort study from the AIOP Clinical Research Group on tooth-supported zirconia-based FDPs estimated a cumulative survival rate of 94.7% on anterior and posterior restorations. Several factors such as framework design, mismatch of the thermal expansion coefficients between zirconia and the veneering ceramic, heat treatment, or the thermal conductivity of yttria-tetragonal zirconia polycrystal (Y-TZP) can generate residual stresses that induce chipping or fracture [37]. At 5 years, 97% of the Y-TZP-based (Lava) FDPs, placed in patients in UK dental practices, performed satisfactorily [38]. A retrospective study on zirconia FDPs made by predoctoral dental students reported a survival rate of 100% and a success rate of 89% after 4.9 years. The most common complication was chipping of the veneering porcelain (14.7%) [39].
A dental laboratory survey on the fracture rate of monolithic zirconia single crowns and FDPs revealed extremely high success with an overall fracture rate of 1.09% after up to 5 years [40].
Zirconia RBFDPs
Single-retainer zirconia RBFDPs had a survival rate of 100% after a mean observation time of 64.2 months, bonded with either a phosphate-monomer containing resin luting agent (Panavia 21, Kuraray Noritake, Japan; n = 16) or an adhesive bonding system with a phosphoric acid acrylate primer (Multilink Automix with Metal/Zirconia primer, n = 14). Of the 30 restorations, 2 had to be rebonded [41]. In another investigation on 42 anterior single-retainer RBFDPs made from Y-TZP after a mean observation time of 61.8 months, two debondings occurred. Both were rebounded, and an overall survival rate of 100% was reported [42•]. For posterior zirconia ceramic inlay-retained FDPs with a modified design, the 5-year cumulative survival was 95.8%. Debonding was also reported for 6.9% (n = 2). One of them ultimately failed after 49.4 months due to repeated decementation [43]. Success rates for this type of indication are, therefore, very high.
Implant-Supported Single-Unit and Multi-Unit Zirconia Prostheses
Three articles reported on implant-supported zirconia-based SCs and FDPs with a cumulative survival rate between 90.5 and 96.4% after 5 to 7-year follow-up [44,45,46]. Larsson and Von Steyern, in a study on implant-supported zirconia-based FDPs in 18 patients, suggested that all-ceramic implant-supported FDPs are an acceptable alternative. This was despite the occurrence of veneering material fractures, as the survival rate (100%) and patient satisfaction were excellent [47]. When assessing the complications and failures of three-unit zirconia-based and PFM implant-supported FDPs, an overall survival rate of 95% in the Y-TZP group and 94.7% in the PFM group was reported [48]. Mikeli and Walter concluded that bruxism may be a risk factor for ceramic fractures [49].
Implant-Supported Cross-Arch Zirconia FDPs
Tooth replacement by means of full-arch screw-retained implant-supported fixed dental prostheses has been reported to be a valuable treatment option for edentulous patients. The results of Vizcaya’s study indicate that full-arch CAD/CAM screw-retained, stained, monolithic zirconia and gingiva-colored ceramic implant-supported FDPs without or with partial digital cutback and veneering ceramic were a reliable therapeutic option [50]. This is in accordance with manuscripts published by Pozzi and coworkers [51, 52].
Zirconia Implant Abutments
Y-TZP has been extensively used for the fabrication of implant abutments. In recent years, five articles reported high success rates between 93.8 and 100% after observation periods between 4 and 12 years [53].
In most recent years, there has been an extreme shift in the industry and clinical practice towards zirconia ceramic restorations. While early non-scientific reports of high failure rates of bilayer porcelain-fused-to-zirconia restorations dampened clinical expectations, recent studies find clinical success of PFZ restorations to be similar to those of PFM restorations. Most recent trends, however, are geared towards monolithic restorations. New zirconia materials, such as high-translucent zirconia, have become extremely popular: they are more translucent, customizable, and fabricated with CAD/CAM technologies. While early reports seem favorable, there is currently very little scientific data that would support the clinical application of these materials.
Conclusions
Silica-based feldspathic, leucite-reinforced, and lithium disilicate ceramics have high success rates for single-unit partial and full-coverage restorations. However, adhesive cementation is needed to maximize their outcomes. Among oxide ceramics, alumina demonstrates high success rates, especially for single-unit anterior and posterior restorations and cantilever RBFDPs. Zirconia reveals high success rates for various restoration designs, such as anterior and posterior tooth-supported and implant-supported SC, FDPs, and RBFDPs. Full-arch screw-retained implant-supported fixed dental prostheses and implant abutments are reliable. However, recent RMC, silicate, and oxide-based ceramics lack clinical scientific validation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent.Mater. 2011;27:83–96. doi:10.1016/j.dental.2010.10.024.
Rohr N, Fischer C, Fischer J. Werkstoffkunde – nein danke! Zahnmedizin up2date. 2015:357–77. doi:10.1055/s-0033-1358160.
Rohr N, Coldea A, Zitzmann NU, Fischer J. Loading capacity of zirconia implant supported hybrid ceramic crowns. DentMater. 2015;31:e279–88. doi:10.1016/j.dental.2015.09.012.
Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J.Prosthet.Dent. 2015;114:587–93. doi:10.1016/j.prosdent.2015.04.016.
Bindl A, Mormann WH. Survival rate of mono-ceramic and ceramic-core CAD/CAM-generated anterior crowns over 2-5 years. Eur J Oral Sci. 2004;112:197–204. doi:10.1111/j.1600-0722.2004.00119.x.
Gracis S, Thompson VP, Ferencz JL, Silva NR, Bonfante EA. A new classification system for all-ceramic and ceramic-like restorative materials. Int J Prosthodont. 2015;28:227–35. doi:10.11607/ijp.4244.
Sorrentino R, Triulzio C, Tricarico MG, Bonadeo G, Gherlone EF, Ferrari M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J Mech Behav BiomedMater. 2016;61:328–33. doi:10.1016/j.jmbbm.2016.04.014.
Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin EducDent. 2016;37:611–7. quiz 618
Ohlmann B, Bermejo JL, Rammelsberg P, Schmitter M, Zenthofer A, Stober T. Comparison of incidence of complications and aesthetic performance for posterior metal-free polymer crowns and metal-ceramic crowns: results from a randomized clinical trial; 2014
Beier US, Dumfahrt H. Longevity of silicate ceramic restorations. Quintessence Int. 2014;45:637–44. doi:10.3290/j.qi.a32234.
Fabbri G, Zarone F, Dellificorelli G, Cannistraro G, de Lorenzi M, Mosca A, Sorrentino R. Clinical evaluation of 860 anterior and posterior lithium disilicate restorations: retrospective study with a mean follow-up of 3 years and a maximum observational period of 6 years. Int J Periodontics Restorative Dent. 2014;34:165–77. doi:10.11607/prd.1769.
Otto T, Mormann WH. Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int J Comput Dent. 2015;18:147–61.
Dierens M, de Bruyn H, Kisch J, Nilner K, Cosyn J, Vandeweghe S. Prosthetic survival and complication rate of single implant treatment in the periodontally healthy patient after 16 to 22 years of follow-up. Clin Implant Dent Relat Res. 2016;18:117–28. doi:10.1111/cid.12266.
Morimoto S, Albanesi RB, Sesma N, Agra CM, Braga MM, et al. Int J Prosthodont. 2016;29:38–49. doi:10.11607/ijp.4315.
Santos MJ, Freitas MC, Azevedo LM, Santos GC, Navarro MF, Francischone CE, Mondelli RF. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin. Oral Investig. 2016;20:1683–90. doi:10.1007/s00784-015-1669-z.
Nejatidanesh F, Amjadi M, Akouchekian M, Savabi O. Clinical performance of CEREC AC Bluecam conservative ceramic restorations after five years—a retrospective study. J Dent. 2015;43:1076–82. doi:10.1016/j.jdent.2015.07.006.
Sailer I, Bonani T, Brodbeck U, Hammerle CH. Retrospective clinical study of single-retainer cantilever anterior and posterior glass-ceramic resin-bonded fixed dental prostheses at a mean follow-up of 6 years. Int. J.Prosthodont. 2013;26:443–50. doi:10.11607/ijp. 3368.
Guess PC, Selz CF, Voulgarakis A, Stampf S, Stappert CF. Prospective clinical study of press-ceramic overlap and full veneer restorations: 7-year results. Int. J.Prosthodont. 2014;27:355–8. doi:10.11607/ijp.3679.
Granell-Ruiz M, Agustin-Panadero R, Fons-Font A, Roman-Rodriguez JL, Sola-Ruiz MF. Influence of bruxism on survival of porcelain laminate veneers. Med Oral Patol Oral Cir Bucal. 2014;19:e426–32.
Zahn T, Zahn B, Janko S, Weigl P, Gerhardt-Szep S, Lauer HC. Long-term behavior of double crown retained dentures with metal and metal-free secondary crowns and frameworks made of Vectris((c)) on all-ceramic primary crowns: a prospective, randomized clinical trial up to 14 years. Clin. Oral Investig. 2016;20:1087–100. doi:10.1007/s00784-015-1597-y.
Toman M, Toksavul S. Clinical evaluation of 121 lithium disilicate all-ceramic crowns up to 9 years. Quintessence Int. 2015;46:189–97. doi:10.3290/j.qi.a33267.
Simeone P, Gracis S. Eleven-year retrospective survival study of 275 veneered lithium disilicate single crowns. Int J Periodontics Restorative Dent. 2015;35:685–94. doi:10.11607/prd.2150.
Yang Y, Yu J, Gao J, Guo J, Li L, Zhao Y, Zhang S. Clinical outcomes of different types of tooth-supported bilayer lithium disilicate all-ceramic restorations after functioning up to 5 years: a retrospective study. J Dent. 2016;51:56–61. doi:10.1016/j.jdent.2016.05.013.
Huettig F, Gehrke UP. Early complications and performance of 327 heat-pressed lithium disilicate crowns up to five years. J. Adv. Prosthodont. 2016;8:194–200. doi:10.4047/jap.2016.8.3.194.
Valenti M, Valenti A. Retrospective survival analysis of 110 lithium disilicate crowns with feather-edge marginal preparation. Int J Esthet Dent. 2015;10:246–57.
Selz CF, Strub JR, Vach K, Guess PC. Long-term performance of posterior InCeram Alumina crowns cemented with different luting agents: a prospective, randomized clinical split-mouth study over 5 years. Clin. Oral Investig. 2014;18:1695–703. doi:10.1007/s00784-013-1137-6.
Dhima M, Paulusova V, Carr AB, Rieck KL, Lohse C, Salinas TJ. Practice-based clinical evaluation of ceramic single crowns after at least five years. J.Prosthet.Dent. 2014;111:124–30. doi:10.1016/j.prosdent.2013.06.015.
Galiatsatos AA, Bergou D. Clinical evaluation of anterior all-ceramic resin-bonded fixed dental prostheses. Quintessence Int. 2014;45:9–14. doi:10.3290/j.qi.a30766.
Saker S, El-Fallal A, Abo-Madina M, Ghazy M, Ozcan M. Clinical survival of anterior metal-ceramic and all-ceramic cantilever resin-bonded fixed dental prostheses over a period of 60 months. Int. J.Prosthodont. 2014;27:422–4. doi:10.11607/ijp.3776.
• Fenner N, Hammerle CH, Sailer I, Jung RE. Long-term clinical, technical, and esthetic outcomes of all-ceramic vs. titanium abutments on implant supporting single-tooth reconstructions after at least 5 years. Clin. Oral Implants Res. 2016;27:716–23. doi:10.1111/clr.12654. This manuscript represents an important and comprehensive study on long-term performance of zirconia abutments.
•• Ozer F, Mante FK, Chiche G, Saleh N, Takeichi T, Blatz MB. A retrospective survey on long-term survival of posterior zirconia and porcelain-fused-to-metal crowns in private practice. Quintessence Int. 2014;45:31–8. doi:10.3290/j.qi.a30768. This manuscript represents the first comparative study on the long-term clinical performance of veneered zirconia crowns in private practice with a large sample size.
Rinke S, Kramer K, Burgers R, Roediger M. A practice-based clinical evaluation of the survival and success of metal-ceramic and zirconia molar crowns: 5-year results. J Oral Rehabil. 2016;43:136–44. doi:10.1111/joor.12348.
Napankangas R, Pihlaja J, Raustia A. Outcome of zirconia single crowns made by predoctoral dental students: a clinical retrospective study after 2 to 6 years of clinical service. J.Prosthet.Dent. 2015;113:289–94. doi:10.1016/j.prosdent.2014.09.025.
Passia N, Stampf S, Strub JR. Five-year results of a prospective randomised controlled clinical trial of posterior computer-aided design-computer-aided manufacturing ZrSiO4-ceramic crowns; 2013.
Bateli M, Kern M, Wolkewitz M, Strub JR, Att W. A retrospective evaluation of teeth restored with zirconia ceramic posts: 10-year results. Clin. Oral Investig. 2014;18:1181–7. doi:10.1007/s00784-013-1065-5.
Guncu MB, Cakan U, Muhtarogullari M, Canay S. Zirconia-based crowns up to 5 years in function: a retrospective clinical study and evaluation of prosthetic restorations and failures. Int. J.Prosthodont. 2015;28:152–7. doi:10.11607/ijp.4168.
Monaco C, Caldari M, Scotti R, Group ACR. Clinical evaluation of tooth-supported zirconia-based fixed dental prostheses: a retrospective cohort study from the AIOP clinical research group. Int. J.Prosthodont. 2015;28:236–8. doi:10.11607/ijp.4023.
Burke FJ, Crisp RJ, Cowan AJ, Lamb J, Thompson O, Tulloch N. Five-year clinical evaluation of zirconia-based bridges in patients in UK general dental practices. J Dent. 2013;41:992–9. doi:10.1016/j.jdent.2013.08.007.
Pihlaja J, Napankangas R, Raustia A. Outcome of zirconia partial fixed dental prostheses made by predoctoral dental students: a clinical retrospective study after 3 to 7 years of clinical service. J.Prosthet.Dent. 2016;116:40–6. doi:10.1016/j.prosdent.2015.10.026.
Sulaiman TA, Abdulmajeed AA, Donovan TE, Cooper LF, Walter R. Fracture rate of monolithic zirconia restorations up to 5 years: a dental laboratory survey. JProsthetDent. 2016;116:436–9. doi:10.1016/j.prosdent.2016.01.033.
Sasse M, Kern M. CAD/CAM single retainer zirconia-ceramic resin-bonded fixed dental prostheses: clinical outcome after 5 years; 2013.
• Sasse M, Kern M. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J Dent. 2014;42:660–3. doi:10.1016/j.jdent.2014.02.021. This manuscript represents the most significant clinical study on zirconia resin-bonded fixed dental prostheses.
Chaar MS, Kern M. Five-year clinical outcome of posterior zirconia ceramic inlay-retained FDPs with a modified design. J Dent. 2015;43:1411–5. doi:10.1016/j.jdent.2015.11.001.
Kolgeci L, Mericske E, Worni A, Walker P, Katsoulis J, Mericske-Stern R. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: a case series. Int. J.Prosthodont. 2014;27:544–52. doi:10.11607/ijp.3807.
Monaco C, Caldari M, Scotti R, Group ACR. Clinical evaluation of zirconia-based restorations on implants: a retrospective cohort study from the AIOP clinical research group. Int JProsthodont. 2015;28:239–42. doi:10.11607/ijp.4038.
Worni A, Kolgeci L, Rentsch-Kollar A, Katsoulis J, Mericske-Stern R. Zirconia-based screw-retained prostheses supported by implants: a retrospective study on technical complications and failures. Clin Implant Dent Relat Res. 2015;17:1073–81. doi:10.1111/cid.12214.
Larsson C, von Vult Steyern P. Ten-year follow-up of implant-supported all-ceramic fixed dental prostheses: a randomized, prospective clinical trial. Int J Prosthodont. 2016;29:31–4. doi:10.11607/ijp.4328.
Shi JY, Zhang XM, Qiao SC, Qian SJ, Mo JJ, Lai HC. Hardware complications and failure of three-unit zirconia-based and porcelain-fused-metal implant-supported fixed dental prostheses: a retrospective cohort study with up to 8 years. Clin Oral Implants Res. 2016; doi:10.1111/clr.12836.
Mikeli A, Walter MH. Impact of bruxism on ceramic defects in implant-borne fixed dental prostheses: a retrospective study. Int J Prosthodont. 2016;29:296–8. doi:10.11607/ijp.4610.
Rojas VF. Retrospective 2- to 7-year follow-up study of 20 double full-arch implant-supported monolithic zirconia fixed prostheses: measurements and recommendations for optimal design. J Prosthodont. 2016; doi:10.1111/jopr.12528.
Pozzi A, Holst S, Fabbri G, Tallarico M. Clinical reliability of CAD/CAM cross-arch zirconia bridges on immediately loaded implants placed with computer-assisted/template-guided surgery: a retrospective study with a follow-up between 3 and 5 years. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e86–96. doi:10.1111/cid.12132.
Pozzi A, Tallarico M, Barlattani A. Monolithic lithium disilicate full-contour crowns bonded on CAD/CAM zirconia complete-arch implant bridges with 3 to 5 years of follow-up. J Oral Implantol. 2015;41:450–8. doi:10.1563/AAID-JOI-D-13-00133.
Rinke S, Lattke A, Eickholz P, Kramer K, Ziebolz D. Practice-based clinical evaluation of zirconia abutments for anterior single-tooth restorations. Quintessence Int. 2015;46:19–29. doi:10.3290/j.qi.a32818.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Digital and Esthetic Dentistry
Rights and permissions
About this article
Cite this article
Conejo, J., Nueesch, R., Vonderheide, M. et al. Clinical Performance of All-Ceramic Dental Restorations. Curr Oral Health Rep 4, 112–123 (2017). https://doi.org/10.1007/s40496-017-0132-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-017-0132-4