Abstract
Introduction
Zirconia posts can be used as an esthetic alternative to metal posts. Despite their advantages, there is a lack of information about the long-term performance of zirconia posts.
Objectives
This retrospective clinical study examined the survival probability, clinical performance, and reasons for failure of teeth restored with zirconia posts after an observation period of up to 10 years.
Materials and methods
After a mean observation period of 10 years, clinical and radiographic examinations were carried out for a total of 64 posts in 45 patients. The posts received mainly either ceramic or direct composite buildups. All posts were adhesively cemented, after air abrasion with alumina particles or silica coating and silanization. The majority of the reconstructed teeth were used as abutments for metal ceramic or ceramic fixed dental prostheses. Kaplan–Meier analysis was employed to compute the survival probability of teeth restored with zirconia posts. Cox regression analysis was used to assess the risk of failure and to identify possible covariates.
Results
During the follow-up period, a drop-out rate of 49.4 % was recorded. The survival probability for teeth with zirconia posts was 81.3 % after 10 years.
Conclusion
Within the limits of this study, zirconia posts can be used for abutments that will be restored with ceramic restorations. However, due to the high patient drop-out rate, careful interpretation of the current results is suggested.
Clinical relevance
The present paper is the first 10-year clinical study on teeth restored with zirconia posts and could serve as a reference for future research. In addition, it provides long-term data about restorations already implemented by dental practitioners.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post and core systems have been implemented to provide retention and support for the restoration of structurally compromised teeth. Several materials have been implemented for the fabrication of posts. Metals, such as gold or titanium, have been extensively used in the past decades. However, the main drawback of such post and core buildups was the potential discoloration of the surrounding soft tissue, thus compromising esthetics. Therefore, there was a need for more esthetic replications of the natural dentition, which led to the use of ceramic materials for the fabrication of posts as well as of core buildups [1].
In the late 1980s, prefabricated glass–ceramic post and core buildups were described in the literature [1]. However, the use of this material for the fabrication of post and core restorations, especially in small diameters, was questionable. Two years later, post and core buildups made of glass-infiltrated aluminum oxide ceramic were fabricated [2]. The main disadvantage of such constructions was their low fracture strength, which could lead to fracture of the post and core restoration. Clinical studies about such one-piece post and core restorations are not available. In 1995, Pissis proposed a “monobloc” technique for the fabrication of the post and core and the crown made out of glass–ceramic material [3]. Studies demonstrated that the fracture strength of this ceramic material was very low (100–220 MPa), and it was, therefore, not considered ideal for the fabrication of post and core restorations [4]. To overcome these limitations, in 1995, zirconia ceramic was introduced as a material for the fabrication of prefabricated endodontic posts [5].
The introduction of zirconium dioxide in restorative dentistry led to a new era in the fabrication of posts, combining esthetics with superior mechanical strength and fracture toughness, when compared to other dental ceramics [2]. A zirconia ceramic post can be combined with a ceramic core made of alumina or alumina–magnesia ceramics, fabricated by either a copy-milling or slip-casting technique [2]. Another technique is the heat-pressed technique, in which a glass–ceramic core (Empress Cosmo; Ivoclar, Liechtenstein, Fürstentum Liechtenstein) is heat pressed over a prefabricated zirconium dioxide post (CosmoPost; Ivoclar, Liechtenstein, Fürstentum Liechtenstein), forming a unique ceramic reconstruction [2]. In addition, when a substantial amount of remaining tooth structure is available, a self-curing composite buildup can be also used in combination with a zirconia ceramic post [6].
Several in vitro studies have documented the mechanical properties of zirconia posts, combined either with a ceramic or a composite resin core [7–14]. However, despite the plethora of laboratory studies, clinical data concerning the long-term survival probability and success of zirconia posts are not available. Therefore, the aim of the present retrospective study was to evaluate the long-term outcome of teeth restored with zirconia ceramic posts after an observation period of 10 years.
Materials and methods
Materials
In February 2008, patient archives of the Department of Prosthodontics, University of Freiburg, and the Department of Prosthodontics, University of Kiel, were screened by two independent examiners (M.B. and W.A) for patients with teeth that had received zirconia ceramic posts. The search was mainly based on patients of both universities that had participated in a previous study about zirconia posts [15]. Post placement had been performed predominantly by faculty members of both universities. A few patients were treated by students in both departments under the strict supervision of faculty members. Between November 1994 and January 2003, 89 patients with 138 endodontically treated teeth had received 141 zirconia posts. Thirty-one patients received more than one post. Table 1 illustrates the distribution of post and core buildups for different tooth and jaw locations. Post diameters (International Standards Organization (ISO) number) in relation to the type of tooth treated are also displayed in Table 1.
The majority of the posts were CeraPost (Brasseler, Lemgo, Germany) zirconia posts (n = 134), while the remaining posts were CosmoPost (Ivoclar Vivadent, Liechtenstein, Fürstentum Liechtenstein) zirconia posts (n = 7). Both types are made of zirconia ceramic and are characterized by high biocompatibility, increased flexural strength, and superior fracture toughness. CeraPost zirconia posts are available in four different sizes (ISO 50, 70, 90, and 110), whereas CosmoPost posts are available in two different sizes (1.4 and 1.7 mm in diameter). Core buildups were fabricated either by ceramic [In-Ceram (Vita, Bad Säckingen, Germany) and IPS Empress Cosmo (Ivoclar Vivadent, Liechtenstein, Fürstentum Liechtenstein)] or by composite (Clearfil Core; Kuraray, Osaka, Japan) material (Fig. 1).
After clinical and radiographic examinations as well as verification that the involved teeth were symptom free, root canal treatment was performed through stepwise filling with K-Files and Hedstrom files to the respective ISO size. Then, the existing root canal filling was reduced so that 3–4 mm of root canal filling material was left at the apical portion. Largo drills were used to enlarge the root canals to the corresponding diameter followed by final conditioning of the root canals using the ER-Set (Brasseler, Lemgo, Germany).
All the composite core buildups were constructed after cementation of the posts. The dentin surface was previously etched for 10–15 s with 37 % orthophosphoric acid and cleaned with water for 60 s. A dentin bonding agent (Clearfil Newbond; Kuraray, Osaka, Japan) was then mixed and applied to the dentin surface according to the manufacturer's recommendations. After application of the chemically polymerized composite (Clearfil Core or Clearfil FII), the core was prepared to the adequate form using diamond drills.
The ceramic cores were either adhesively luted (In-Ceram; Vita, Bad Säckingen, Germany) or heat pressed (IPS Empress Cosmo; Ivoclar Vivadent, Fürstentum Liechtenstein) to the posts. To enhance the bond strength of zirconia posts to root dentin, the surface of the zirconia posts was treated using either airborne particle abrasion (50 μm aluminum oxide at 2.5 bars) or tribochemical silicatization and silanization (Rocatec; Espe Seefeld, Germany) [15–17]. All posts were bonded into root canals using resin composite cements (Panavia EX and Panavia 21; Kuraray, Osaka, Japan). The majority of the reconstructed teeth were used as abutments for metal–ceramic or all-ceramic fixed dental prostheses (FDPs).
Methods
All patients were invited to participate in the follow-up examination. Clinical and radiographic examinations of the post and core buildups were performed. At evaluation time, the study population was divided into five groups. Patients who were not able to participate in the follow-up examination or had moved were categorized as “moved.” Deceased patients were categorized as “dead,” and those who were not reached were categorized as “missing.” Patients who came for a clinical examination and their post and core build-ups which met all the success criteria were categorized as “intact.” Failed post and core restorations were categorized as “failure.”
The success criteria were established as follows:
-
Lack of tooth sensitivity to horizontal and vertical percussion tests.
-
Probing depths of ≤3 mm at six aspects.
-
Lack of mobility of the crown and/or the post.
-
Lack of periapical radiolucency.
Failures were divided into the following categories: tooth loss/extraction, periapical radiolucency, sensitivity to percussion test with existence of periapical radiolucency, post/core/root/restoration fracture, and post dislodgment with or without rebonding.
Follow-up examinations consisted of intraoral photographs, polyvinylsiloxane impressions of the tooth, and/or the fixed dental prosthesis with a post and core restoration and direct clinical measurements. Periapical radiographs were performed in cases of sensitivity to percussion test, inflammation, excessive pocket depth measurement, and/or mobility of the post/prosthetic restoration. Occlusal analysis, including recording of occlusal contacts in intercuspal position as well as in lateral excursions, was also performed.
Statistical analysis
The statistical analysis was performed at the Institute of Medical Biometry and Medical Informatics, Albert-Ludwigs University, Freiburg, Germany. For the statistical analysis of the retrospective data, a tooth treated with a post and core was identified as “success” if the post and core as well as its prosthetic restoration were still in place and without any signs of clinical and radiographic complications. A failure was defined as a post and core that was no longer in place or showed signs of periapical radiolucency, percussion test hypersensitivity, and/or fracture or dissolution of the post and core and/or the restoration. Survival probability was assessed using the Kaplan–Meier analysis. It should be mentioned that the Kaplan–Meier curves represent the “unit” failure and not the post failure. Additionally, we intended to identify whether there is a statistically significant difference between the core materials, the maxilla and the mandible, as well as among different tooth types (incisors, canines, premolars, and molars), different restoration materials, and different post diameters (ISO 50, 90, and 110). Cox regression analysis was performed to assess the risk of failure and to identify possible covariates, with a cutoff value of p = 0.05. In an effort to minimize heterogeneity originating from the retrospective study design, molars were excluded from the statistical analysis.
Results
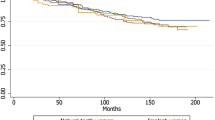
The observation time for the post and core restorations ranged from 10 to 14.5 years (mean observation period, 12.3 years). The average survival probability for teeth with zirconia posts was 81.3 % after an observation period of 10 years (Fig. 2a). The Kaplan–Meier curve shows the teeth at risk for the corresponding time points. We also plotted 95 % confidence bands. For the purposes of the statistical analysis, all zirconium dioxide posts were pooled together. Due to the lack of sufficient data, one post and core restoration was excluded from the statistical analysis. Forty-five patients (50.6 % of the total number of patients) with 64 posts (46.4 % of the total number of posts) participated in the follow-up study. Accounting for drop-out rate of 49.4 % (44 patients) are the following: 38.2 % of the patients could not be traced, 5.6 % of the patients died during the follow-up period, and 5.6 % of the patients moved to another city or country.
Among 64 post and core buildups examined, 51 restorations were in clinical use without signs of failure. Failures were recorded in 13 posts at the time of the follow-up examination (Table 2). The most common type of failure was extraction. Unfortunately, the reasons for extraction were not documented. Furthermore, failure-related factors were sensitivity to percussion, periapical radiolucency, a loss of retention of the post without rebonding, and fracture of porcelain. A representative image of periapical radiolucency is presented (Fig. 3). Due to the small number of failures, a statistical evaluation of the data was not possible.
Initially, we intended to check for possible influence of co-variables, such as post diameter, type of jaw, type of tooth, and type of prosthetic restoration. However, the number of available teeth restored with zirconia posts in some cells did not justify analyses regarding these aspects. Thus, the analyses of these secondary variables could not be conclusive. Due to the small number of cases in the other subgroups, statistical analysis was possible only between composite and non-composite cores. The hazard ratio comparing composite with no composite was 1.288 (95 % CI, 0.322–5.156). No statistically significant differences were ascertained between the two groups (p = 0.7210) (Fig. 2b).
Discussion
The selection of zirconium dioxide for the fabrication of posts has been based on its material properties, like high flexural strength, hardness, biocompatibility, and low solubility [18, 19]. However, although fracture strength values and mechanical properties of zirconia posts have been extensively examined [7–11], long-term data about the clinical behavior and the survival probability of teeth with zirconia posts are not available. Considering the lack of clinical studies on zirconia posts, along with the increasing demand for more esthetic and biocompatible restorations, a long-term evaluation of the clinical performance of such posts was essential. Therefore, this study aimed to evaluate the long-term outcome of teeth restored with zirconia ceramic posts over an observation period of up to 10 years and to identify possible covariates that may influence the failure risk.
The overall survival probability for teeth with zirconia posts are within the range reported in the literature for different types of post and core buildups after a main observation period of 10 years (71–98 %) [20–27]. For teeth with zirconia posts, only one midterm clinical study is available [6]. The authors evaluated the treatment outcome of zirconia posts (CosmoPost; Ivoclar Vivadent, Liechtenstein, Fürstentum Liechtenstein) with either direct composite or indirect ceramic cores after 4 years of clinical service. In this study, the success rate of zirconia posts with direct composite cores (100 % after a mean period of 4.8 years) exceeded that of zirconia posts with indirect ceramic cores (95 % after a mean period of 3.9 years). These results conflict with the results of the present study. These results conflict with the results of the present study. However straight forward comparison is hindered by the high drop out rates exhibited in in both studies. Another study showed that no tooth or post fractures occurred during a mean observation period of 16.6 ± 9.1 months and that no post was lost due to debonding [15]. The authors suggested that zirconia posts could be a promising new treatment option but also highlighted the need for further long-term clinical studies [15], which was also the instigating factor for this study. Other clinical studies on zirconia ceramic posts are either case reports [28, 29] or pilot studies [30]. Regarding other tooth-colored post and core buildups, unfavorable results have been reported for carbon fiber-reinforced posts (Composipost) [31], while a failure rate of 7–11 % for three types of fiber posts (n = 985) is documented after an observation period of 7, 8, 9, 10, and 11 years [32].
In the current study, few failures were reported, and the most common failure was tooth extraction. Unfortunately, it was not possible to relate any of the extractions to dental, periodontal, or endodontic problems as well as malfunctioning of the post and core and/or prosthetic restoration, occurred prior to tooth removal. Neither the data of the clinic nor the patients themselves could provide adequate insight into the reasons for extraction. Periodontal, endodontic, and prosthetic problems as well as extractions and debonding cases were pooled together to provide the dental clinician with the “worst-case scenario” regarding the survival probability at tooth level related to the post and core restoration.
However, in case of a failure, it should be noted that the main disadvantage of zirconia posts is associated with the rigidity of this material, which tends to transfer stresses to the compromised tooth structure, thus enhancing the risk of root fracture [33]. The difficulty in the removal of zirconia posts may also be attributed to the rigidity of the material, leaving no other choice but the extraction of the involved tooth.
The risk of failure found in the present study is within the range reported for other tooth-colored post materials, such as glass or carbon fiber posts [31, 32, 34]. Unfortunately, the number of failures (13 posts) was too small to allow for a thorough statistical analysis with respect to failure characteristics. However, the types of failures could be reported and categorized. As an example, it can be mentioned that almost 30 % of the failures were clearly an account of periapical radiolucency, as shown in Table 2.
Another discussion point associated with the retrospective design of the present study is the high drop-out rate (49.4 %) associated with the fact that the patients were not in a continuous recall program. Patient retrieval was difficult; therefore, some patients' data and radiographs were retrieved either from the patient records (n = 10) and/or patients' dentist (n = 5). For the purposes of the statistical analysis, all zirconia posts were pooled into one group. Considered as the major drawback of the current study, the reported drop-out rate was mainly an account of losing track of patients because of moving. Nevertheless, such drop-out rates are a common experience in long-term clinical studies, especially when the patients are not regularly recalled by the same research group, as in the present study.
As for the core material, zirconia-based ceramic posts are commonly used in combination with heat-pressed glass–ceramic or composite resin cores [2–6]. In the present study, the survival probability of teeth restored with zirconia posts and non-composite buildups did not differ from that of teeth restored with zirconia posts and direct composite buildups (p > 0.05). These results differ from the results of a 4-year retrospective study, in which 145 endodontically treated teeth restored with zirconia posts in conjunction with either composite or ceramic cores were examined [6]. In this study, success rates were 91–100 and 53–95 % for the direct and the indirect groups, respectively. As mentioned in the “Results” section, an analysis of the secondary variables was not possible, since the statistical analysis was possible for one variable only, namely, the core material. As far as the material of the prosthetic restoration is concerned, it can be pointed that no spurious relationship could be identified between incisors and premolars. Both were restored with either metal ceramic or ceramic restorations. However, a statistical analysis was not possible.
In review of the current literature and in view of the results of the current study, it is obvious that there is a lack in clinical knowledge about the long-term outcome of teeth restored with zirconia posts. Hence, it should be highlighted that the present paper is the first 10-year clinical study on teeth restored with zirconia posts.
Conclusions
Within the limits of the present retrospective clinical study, it can be concluded that although the 10-year survival probability of teeth restored with zirconia posts seems to be similar to that reported in the literature for teeth restored with other post materials, the high patient drop-out rate suggests careful interpretation of the current results and yields the need for long-term randomized clinical trials.
References
Kwiatkowski S, Geller W (1989) A preliminary consideration of the glass-ceramic dowel post and core. Int J Prosthodont 2:51–55
Koutayas SO, Kern M (1999) All-ceramic posts and cores: the state of the art. Quintessence Int 30:383–392
Pissis P (1995) Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract Periodontics Aesthet Dent 7:83–94
Wagner WC, Chu TM (1996) Biaxial flexural strength and indentation fracture toughness of three new dental core ceramics. J Prosthet Dent 76:140–144
Meyenberg KH, Luthy H, Scharer P (1995) Zirconia posts: a new all-ceramic concept for nonvital abutment teeth. J Esthet Dent 7:73–80
Paul SJ, Werder P (2004) Clinical success of zirconium oxide posts with resin composite or glass-ceramic cores in endodontically treated teeth: a 4-year retrospective study. Int J Prosthodont 17:524–528
Butz F, Lennon AM, Heydecke G, Strub JR (2001) Survival rate and fracture strength of endodontically treated maxillary incisors with moderate defects restored with different post-and-core systems: an in vitro study. Int J Prosthodont 14:58–64
Heydecke G, Butz F, Hussein A, Strub JR (2002) Fracture strength after dynamic loading of endodontically treated teeth restored with different post-and-core systems. J Prosthet Dent 87:438–445
Heydecke G, Butz F, Strub JR (2001) Fracture strength and survival rate of endodontically treated maxillary incisors with proximal cavities after restoration with different post and core systems: an in-vitro study. J Dent 29:427–433
Jeong SM, Ludwig K, Kern M (2002) Investigation of the fracture resistance of three types of zirconia posts in all-ceramic post-and-core restorations. Int J Prosthodont 15:154–158
Strub JR, Pontius O, Koutayas S (2001) Survival rate and fracture strength of incisors restored with different post and core systems after exposure in the artificial mouth. J Oral Rehabil 28:120–124
Xible AA, Tavarez RR, Araujo Cdos R, Conti PC, Bonachella WC (2006) Effect of cyclic loading on fracture strength of endodontically treated teeth restored with conventional and esthetic posts. J Appl Oral Sci 14:297–303
Akkayan B (2004) An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowel systems. J Prosthet Dent 92:155–162
Akkayan B, Gulmez T (2002) Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent 87:431–437
Kern M, Simon M, Strub JR (1998) Initial clinical experiences with zirconium-dioxide ceramic posts. Dtsch Zahnartztl Z 53:266–268
Kern M (2009) Resin bonding to oxide ceramics for dental restorations. J Adhes Sci Technol 23:1097–1111
Kern M, Wegner SM (1998) Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater 14:64–71
Christel P, Meunier A, Heller M, Torre JP, Peille CN (1989) Mechanical properties and short-term in-vivo evaluation of yttrium-oxide-partially-stabilized zirconia. J Biomed Mater Res 23:45–61
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25
Heydecke G, Peters MC (2002) The restoration of endodontically treated, single-rooted teeth with cast or direct posts and cores: a systematic review. J Prosthet Dent 87:380–386
Aquilino SA, Caplan DJ (2002) Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 87:256–263
Dammaschke T, Steven D, Kaup M, Ott KH (2003) Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod 29:638–643
Ellner S, Bergendal T, Bergman B (2003) Four post-and-core combinations as abutments for fixed single crowns: a prospective up to 10-year study. Int J Prosthodont 16:249–254
Linde LA (1984) The use of composites as core material in root-filled teeth. II. Clinical investigation. Swed Dent J 8:209–216
Weine FS, Wax AH, Wenckus CS (1991) Retrospective study of tapered, smooth post systems in place for 10 years or more. J Endod 17:293–297
Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH (2007) Up to 17-year controlled clinical study on post-and-cores and covering crowns. J Dent 35:778–786
Creugers NH, Mentink AG, Kayser AF (1993) An analysis of durability data on post and core restorations. J Dent 21:281–284
Toksavul S, Turkun M, Toman M (2004) Esthetic enhancement of ceramic crowns with zirconia dowels and cores: a clinical report. J Prosthet Dent 92:116–119
Gernhardt CR, Bekes K, Schaller HG (2005) Short-term retentive values of zirconium oxide posts cemented with glass ionomer and resin cement: an in vitro study and a case report. Quintessence Int 36:593–601
Nothdurft FP, Pospiech PR (2006) Clinical evaluation of pulpless teeth restored with conventionally cemented zirconia posts: a pilot study. J Prosthet Dent 95:311–314
Segerstrom S, Astback J, Ekstrand KD (2006) A retrospective long term study of teeth restored with prefabricated carbon fiber reinforced epoxy resin posts. Swed Dent J 30:1–8
Ferrari M, Cagidiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, Tay F (2007) Long-term retrospective study of the clinical performance of fiber posts. Am J Dent 20:287–291
Qualtrough AJ, Mannocci F (2003) Tooth-colored post systems: a review. Oper Dent 28:86–91
King PA, Setchell DJ, Rees JS (2003) Clinical evaluation of a carbon fibre reinforced carbon endodontic post. J Oral Rehabil 30:785–789
Acknowledgments
The authors gratefully thank Dr. Stephanie Eschbach, former Assistant Professor at the University of Kiel for her help in data acquisition.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bateli, M., Kern, M., Wolkewitz, M. et al. A retrospective evaluation of teeth restored with zirconia ceramic posts: 10-year results. Clin Oral Invest 18, 1181–1187 (2014). https://doi.org/10.1007/s00784-013-1065-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1065-5