Abstract
Purpose of Review
In this review, we discuss the roles of the gut microbiota and dietary phytochemicals in improving human health. Recent studies have reported that the human gut microbiota can be altered by dietary phytochemicals, including phenolics, carotenoids, and dietary fibers. In addition, both pathogenic and nonpathogenic bacteria show regulatory effects with phytochemicals, suggesting potential synergistic effects in the improvement of human gut health and prevention of chronic diseases.
Recent Findings
Numerous studies have been conducted on gut microbial alterations induced by phytochemicals, such as phenolics and carotenoids. Butyrate, a short-chain fatty acid produced via bacterial fermentation in the colon, also shows a significantly beneficial effect in the maintenance of gut microbial homeostasis. However, the molecular mechanisms underlying the effects of diets and the interactions of the gut microorganisms remain poorly understood. The gut microbiome profile changes have been observed in chronic inflammation-induced diseases, including colitis, Crohn’s disease, immune dysfunction, colon cancer, obesity, and diabetes. The anti-inflammatory effects of dietary phytochemicals against these diseases may be partially mediated by the regulation of microbial profiles. The latest advances in biomedical technology, such as next-generation sequencing (NGS), and continuous cost reduction associated with these technologies have enabled researchers to perform an ever-increasing number of large-scale, high-throughput computational analyses to elucidate the potential mechanism of phytochemical–microbiome interactions.
Summary
Information obtained from these studies may provide valuable insights to guide future clinical research for the development of therapeutics, botanicals, and drug efficacy testing, many of which will be discussed in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term ‘microbiota’ refers to microbial communities [1]. The human gastrointestinal (GI) tract harbors more than 100 trillion total microbes, including bacteria, archaea, microbial eukaryotes, and viruses [2, 3]. Although this number varies in individual studies, it remains clear that microbial biological functions are important [4]. The gut microbiota has several beneficial effects on human health, including promoting innate and adaptive immunity [5, 6], maintaining the intestinal epithelial integrity [7, 8], helping the metabolism and synthesis of essential nutrients such as vitamins and carbohydrate [9, 10], and resisting pathogens [11, 12]. Currently, scientists can explore the characteristics of the human microbiota from low to high resolution by collecting and analyzing high-throughput sequencing data with computational methods and algorithms [13, 14]. The National Institutes of Health (NIH) common fund-supported Human Microbiome Project initiated the profiling of the signature of the human microbiota and interpreted the high-throughput data obtained from 16S rRNA sequencing (relative abundance and diversity) and shotgun sequencing (functions and pathways) [3]. Subsequently, the gut microbiota of healthy subjects and patients with specific diseases has been explored dynamically in the last decade [15,16,17,18]. Phytochemicals are bioactive compounds that are abundantly distributed in fruits and vegetables [19,20,21,22]. A strong correlation between specific classes of phytochemicals and modification of the responding microbiota was observed [23,24,25]. However, comprehensive understanding of the interactions among phytochemicals and the gut microbiota remains in the early phase.
In this review, we will cover the roles of several classes of phytochemicals in the modification of the human gut microbiota. We will explore the relationship between the human gut microbiota and chronic diseases, including inflammatory bowel disease (IBD), colorectal cancer (CRC), and obesity. We will also discuss the potential mechanism underlying the triangular regulation of phytochemicals, the gut microbiota, and human diseases, along with other significant factors, including dietary patterns, lifestyles, and environmental exposure. The purpose of this review is to highlight the importance of interactions between phytochemicals and the gut microbiota, and demonstrate the strong potential for the development of multiple platforms of diagnosis and therapies using this information, which will guide future clinical studies.
Phytochemicals in the Modification of the Gut Microbiota
Flavonoids
Flavonoids are a major subgroup of phenolics that contain two phenyl rings and one heterocyclic ring, and are widely distributed in fruits and vegetables, such as blueberry and cranberry [26,27,28]. Evidence suggests that flavonoids and their derivatives influence the profile of the gut microbiota for improvement of host immune function and metabolism [29,30,31], and the metabolic process reveals that flavonoids have both prebiotic and antibacterial effects [32]. Possible growth enhancement of Bifidobacterium, Lactobacillus, and Enterococcus species and inhibition of Clostridium and Bacteroides species were observed during the coculture with flavonoids, and the changes in the human gut microflora were assessed by fluorescence in situ hybridization [33]. The bacterial species Eubacterium ramulus and Clostridium orbiscindens were also involved in flavonoid metabolism [34, 35]. Quercetin and its glycoside derivatives are abundant flavonols (subcategorized as flavonoids [36]) that are consumed via regular diets [37, 38]. A study showed that quercetin, not its glycoside derivatives, inhibited the growth of the bacteria Bacteroides galacturonicus, Lactobacillus, Escherichia coli, Enterococcus caccae, and Ruminococcus gauvreauii in a dose-dependent manner [29]. Other flavonoids also showed antimicrobial properties against food-borne pathogens and are widely applied in the food industry [39]. Naringin (a flavanone) and rutin (a flavonol) metabolism have been determined to be microbiota-dependent, based on results obtained for mixed cultures with the human microflora [40]. All evidence suggest that flavonoid metabolism and the gut microbiota influence each other, and the gut microbiota has a strong impact on flavonoids and the associated metabolites, leading to strong health benefits.
Anthocyanins
Anthocyanins represent a major subgroup of flavonoids that are distributed in the common vegetables and fruits consumed in the US market, such as blueberry, raspberry, purple cauliflower, and lettuces [41,42,43,44]. Raspberry anthocyanins (glycosides) have been significantly degraded in the presence of the active human microflora during coincubation [45]. Anthocyanins from potato, black rice, and malvidin 3-glucoside also exhibited significant impacts on the growth of the gut microbiota, including on the growth of Bifidobacterium spp., Lactobacillus spp., Staphylococcus aureus, and Salmonella typhimurium, during in vitro fermentation [33, 46, 47]. This bidirectional effect between anthocyanins and the gut microbiota was also observed in vivo. The catalytic gut bacteria Eubacterium ramulus and Clostridium saccbarogumia were involved in the deglycosylation of cyanidin-3-glucoside, a major derivative of cyaniding [48]. Black raspberry anthocyanins restored the growth of Eubacterium rectale, Faecalibacterium prausnitzii, and Lactobacillus spp., and inhibited the growth of Desulfovibrio spp. and Enterococcus spp. in C57BL/6J mice [49]. The luminal abundances of Firmicutes (Clostridium spp.) and Bacteroidetes (Barnesiella spp.) were significantly altered by raspberry anthocyanins [50]. The relative abundances of Bacteroides, Prevotella, Porphyromonas, and Lactobacillus significantly increased and those of Bifidobacterium and Clostridium decreased in rats fed with blackcurrant anthocyanins [51]. Berry anthocyanins suppressed the growth of the proinflammatory bacterium Bilophila wadsworthia and increased the abundance of Gammaproteobacteria in the high-fat-diet group [52, 53]. In human clinical trials, subjects fed anthocyanin-rich red wine exhibited increased relative abundances of Eggerthella lenta, Bifidobacterium, and Enterococcus at the genus level in feces [54]. An 8-week study with 51 subjects fed anthocyanins and prebiotic fibers showed increased phylum levels of Bacteroidetes and reduced levels of Firmicutes and Actinobacteria [55]. A majority of anthocyanins undergo metabolism in the lower small intestine and colon, which was mediated by the colonic microbiota [29]. Even through a large amount of studies and results have been reported, further research of specific bacteria and anthocyanins interactions and their molecular mechanisms are needed to be elucidated.
Hydrolyzable Tannins
Tannins are polyphenolic compounds and are subcategorized into ellagitannins, gallotannins, complex tannins, and condensed tannins [56]. Ellagitannins are hydrolyzable tannins that are present in berries, walnuts, plant seeds, and herbs [57,58,59,60]. Ellagitannins were hydrolyzed to ellagic acid, and ellagic acid was then gradually metabolized by the colon microbiota to produce urolithin A and urolithin B [60]. In addition, it has been demonstrated that the antioxidants urolithin C and urolithin D were also present at significantly high concentrations in the intestines [61]. Evidently, urolithin metabolites production and tannins metabolism occurs primarily in the human lower GI tract and are microbiota-dependent. To identify specific microbes that are involved in ellagitannin metabolism, human clinical studies have reported that species belonging to the genera Bacteroides, Prevotella, and Ruminococcus are the dominant gut microbes in subjects that consumed urolithin-enriched walnut and pomegranate extracts, and the family Coriobacteriaceae is associated with urolithin metabolites and blood cholesterol levels [62]. Other studies have suggested that the genera Clostridium, Bifidobacterium, Lactobacillus, and Bacteroides are involved in the production of urolithins [63, 64]. Bifidobacterium and Clostridium were also involved in pomegranate ellagitannin metabolism in a bacteria-species-dependent manner, as determined by measuring the optical density of culture media [65]. Gallotannin is another type of hydrolyzable tannin [66, 67]. A human clinical trial revealed that gallotannins underwent microbe-mediated metabolism and released free gallic acid in the GI tract [68]. Although many studies have suggested that hydrolyzable tannin metabolism is microbiota-related, the mechanisms underlying the antioxidant and anti-inflammatory activities of tannin metabolites and urolithins in the improvement of human health remain poorly understood [60].
Carotenoids
Carotenoids are tetraterpenoids, colored pigments that are present in fruits and vegetables [69]. The subgroups include xanthophylls (lutein, zeaxanthin) and carotenes (alpha-carotene, beta-carotene, and astaxanthin), and these compounds exhibit high antioxidant activity in the maintenance of human health [70,71,72,73]. Astaxanthin is an oxycarotenoid that is abundant in certain microalgae and marine animals [73,74,75]. Dietary astaxanthin (50 mg/kg) altered the relative abundances of the phyla Bacteroidetes and Proteobacteria; genera Butyricimonas, Bilophila, and Parabacteroides; and species from Verrucomicrobia and Akkermansia in C57BL/6J mice [76]. Astaxanthin (200 mg per kg body weight per day) reduced the bacterial load of gram-negative pathogen Helicobacter pylori 119/95p on Helicobacter pylori-infected BALB/cA mice, and reduced the gastric inflammation and Helicobacter pylori-specific T cell cytokine release [77]. A pilot study showed that dietary astaxanthin (0.04%, w/w) modified cecal microbiota at the phylum by both gender and genotype in vivo [23]. Astaxanthin application selectively reduced the abundance of cecal Proteobacteria and Bacteroides in female wide-type and BCO2 knockout mice C57BL/6J mice. In addition, astaxanthin significantly increased the abundance of Actinobacteria and Bifidobacterium in male wide-type mice only.
Fibers and Butyrates
Whole-plant foods include vegetables, whole grains, and fruits and contain high amounts of fibers. Digestible fibers are among the major bioactive components of whole-food dietary interventions and significantly change the profile of the human gut microbiota [78,79,80]. Butyrate is a short-chain fatty acid that is commonly produced by bacterial fermentation of dietary fibers in the colon [81, 82]. This fatty acid plays several important biological roles, including as an inhibitor of histone deacetylase, an energy metabolite for the production of ATP, an activator of G protein-coupled receptors, an antioxidant, an anti-inflammatory agent, and a promoter of brain health [83,84,85,86,87,88,89]. Human clinical trials determined that dietary fiber intake was strongly associated with the abundances of specific gut microbes, including those of the bacterial class Clostridia, phylum Actinobacteria, and order Bifidobacteriales [90]. Soluble corn fibers (21 g per day) significantly altered the bacterial phyla Firmicutes and Bacteroidetes and families Ruminococcaceae, Lachnospiraceae, Eubacteriaceae, and Porphyromonadaceae in a randomized human clinical study [91]. Furthermore, metabolic pathways, including metabolism of carbohydrates, nucleotides, vitamins, and amino acids, were also induced by dietary fiber consumption. Studies have reported that a high-fiber diet influences the composition of the intestinal microbiome, indicating that the process of fiber fermentation is highly microbiota-dependent [92, 93]. Thus, to fully appreciate the benefits to human health and understand the potential underlying mechanisms to guide the improvement of dietary requirements in the future, further research is needed.
From the above discussion, one could see that there are significant interactions between dietary phytochemicals and gut microbiota (summarized in Table 1) that could impact human health, to be discussed below.
Gut Microbiota and Phytochemical Interactions in Chronic Diseases
The human gut microbiome and chronic diseases have been extensively studied in recent years [94,95,96]. An increasing number of studies have reported that microbial profiles systematically represent the interactions between the gut microbiota and microbiota-derived metabolites. The signature profiles are variable and highly dependent on the chronic diseases exhibited by the subject. In this review, the microbiota signatures of IBD, colorectal inflammation/CRC, and obesity/metabolic syndrome are discussed.
IBD and Gut Microbiota
IBD is induced by severely dysregulated and excessive immune response to commensal microbes, especially pathogens [97, 98]. IBD has been subcategorized into two major types: ulcerative colitis (UC) and Crohn’s disease (CD) [99]. With the development of gene sequencing technologies, especially 16S ribosome RNA and metagenomic sequencing and powerful bioinformatics tools, the reliability and accuracy of the description of gut microbial profiles and bacterial functions during intestinal inflammation in IBD have increased [13, 100]. UC is characterized as a continuous inflammation in the colon [99]. Compared with the ‘normal’ gut microbiota, patients with UC suffer from a reduction in bacterial diversity, microbiota instability (over- or under-expression of certain species), and adverse effects of therapies and drugs [97]. Some signature changes have been observed in human clinical trials, where UC patients exhibited abnormalities of the gut microbiota, such as total depletion of the phyla Firmicutes and Bacteroidetes [101]. Other clinical reports have shown that UC patients exhibited increased abundances of the phyla Actinobacteria and Proteobacteria, with decreased bacterial diversity. In vitro, Fusobacterium varium, Fusobacterium nucleatum, and Escherichia coli were isolated from patients with UC and were possibly responsible for the induction of chronic inflammation in the colon [102,103,104,105,106]. Unlike UC, CD occurs in the entire GI tract, with mixed healthy and inflamed areas [97]. A systematic review and meta-analysis revealed that the abundance of Mycobacterium avium subspecies paratuberculosis was positively correlated with CD [107]. Reduced abundances of the genera Faecalibacterium and Roseburia, as well as increased levels of Escherichia coli and Ruminococcus gnavus, were also observed in patients with CD [108]. Currently, the gut microbiota–host interaction-induced mucosal immune response dysfunctions and intestinal chronic inflammation are the major causes of IBD, leading to reduced gut bacterial diversity and microbial dysregulation. To restore the gut microbiota homeostasis and prevent IBD, dietary intervention has become a critical and promising approach.
Phytochemicals show strong anti-inflammatory activity in vivo and in vitro, and might have potential applications in the treatment of IBD [109,110,111,112]. In human clinical trials, 40 patients with IBD were tested on an anti-inflammatory diet (IBD-AID) treatment [113,114,115]. The IBD-AID diet contained fish, egg, and various fruits and vegetables to improve IBD patients’ carbohydrate modification, ingestion of pre- and probiotics, balance of the fatty acids intake, and overall dietary pattern. The results showed that over 60% of IBD patients had good or very good response to dietary treatment in the clinical assessment. The symptom reduction and life quality improvement was effective. Unfortunately, the underlying mechanism of efficiency was not elucidated. For other phytochemicals, flavonoids and polyphenols played anti-inflammatory roles against IBD through increasing intestinal bacterial diversity, reducing the relative abundance of Escherichia coli and Fusobacteria, and increasing the abundance of Bacteroidetes [116, 117]. Flavanols EGCG from green tea and tannic acids from gelatin tannate also showed strong anti-inflammatory activity in vitro by modulating gut microbiota, yet the accurate interaction was not fully understood [118, 119]. With accumulated evidence of gut microbiota interaction with phytochemicals, future human clinical trials of selected dietary supplementation would help to develop effective and less toxic botanical therapies against IBD.
Gut Microbiota in Colorectal Inflammation and CRC
The human colonic mucosa is populated with a wide range of microorganisms, usually in a symbiotic relationship with the host [120]. The imbalance of colon microbiota raises the risk of the colon exposed to metabolic and inflammatory stimuli [101, 121]. This imbalance, or dysbiosis, is a multifactorial issue that has been found to be associated with lifestyle (indicative of dietary habits and sedentary behaviors), DNA mutations, inflammation, and, most recently, changes in microbiota [122,123,124,125]. Recent studies have attempted to identify microbial changes that may enhance the process [126,127,128,129,130]. For example, Proteobacteria is a phylum that houses more than 200 genera of gram-negative bacteria, including several well-known pathogens, such as Escherichia coli, Salmonella, and Helicobacter pylori [131]. Several preclinical and clinical studies have demonstrated that these pathogens were found to be associated with human colon inflammation and CRC [132,133,134,135,136]. Meta-analyses of human clinical studies revealed that Helicobacter pylori infection was associated with a nearly 50% significant higher risk of CRC [137, 138]. A case–control study from Germany in 2003–2007 showed slightly higher levels of Helicobacter pylori (around 46.1%) in CRC cases than in healthy controls (40.1%). Firmicutes comprises mostly gram-positive phyla in human colon [130, 139]. The overall gut mucosa Firmicutes accounted for 43.46% and 63.46% in healthy individuals and CRC patients, respectively [140]. Staphylococcaceae, a family class of Firmicutes, was found to be more abundant in human CRC patients than in healthy controls [141]. In contrast, another human clinical study showed that Firmicutes at the mucosal tissue of tumors was lower at 37.12% compared to normal mucosa at 44.72% of total mucosal bacteria [142]. Fusobacterium is a gram-negative bacteria and has been shown to be more prevalent in individuals with CRC than in healthy rats and humans [141, 143]. Furthermore, among individuals, those with a high abundance of Fusobacterium were apparently more likely to have adenomas than those with a low abundance of this genus [144]. A significant increase of Fusobacteria occurred on the gut microbiota of CRC patients from 0.03% to 10.58% compared with healthy individuals [140]. These findings suggest that such microbiota may accumulate during the colorectal carcinogenesis. Meanwhile, by transplanting fecal microbiota from both CRC patients and healthy individuals into germ-free mice, the tumor burden increase was strongly associated with the abundance of the genus Bacteroides in the mice gut [143]. Evidence suggests that inflammatory and metabolic stimuli, along with the microbial community, are important for the prognosis of colon carcinogenesis. Investigation of the colon microbiota and the associated modulatory cellular pathways is an area with great potential for research.
Phytochemicals show anticancer and anti-inflammatory activities on various human cancers [20, 145, 146]. Phytochemicals also modulate the intestinal microbial ecology, especially the gut microbiota, as early as a few days after switching between carefully controlled diets [147,148,149]. Evidence suggested that dietary polyphenols stimulated the growth of certain Lactobacillus strains [150]. Berry phenolics inhibited the growth of both gram-positive and gram-negative pathogenic bacterial strains, but, interestingly, the lactic acid bacteria group was hardly affected [151]. Lactobacillus acidophilus CECT 362 was resistant to tea phenolic extracts containing caffeine, (−)-epicatechin, (−)-epicatechin gallate, (−)- epigallocatechin, (−)-epigallocatechin gallate, and gallic acid, whereas food-borne bacteria were inhibited [152]. Polyphenolic extracts from green tea, honey, peppers, blackcurrants, raspberries, cinnamon, and peppermint also exhibited inhibitory activity against Helicobacter pylori [153,154,155]. Polyphenols in olive oil diffused into the gastric juice and exerted a potent bactericidal effect against eight strains of Helicobacter pylori at very low concentrations (1.3 μg/mL) [156]. Tea-extracted phenolics (epicatechin, catechin, 3-O-Me gallic acid, gallic acid, and caffeic acid), aromatics, and metabolites (3-(4-OH phenyl)propionic acid, 3-phenylpropionic acid, 4-OH phenylacetic acid) showed selective growth effects on human gut microflora and reduced the growth of pathogenic bacteria, including Clostridium perfringens, Clostridium difficile, and Bacteroides spp., significantly [157]. Despite systemic similarities between rodents and humans, it is important to understand the complexity, exposure-related differences, and mechanisms of action of phytochemicals in gut microbial modulation [158]. Phytochemicals contribute to the maintenance of human GI health, largely via modulation of the gut microbial balance with simultaneous inhibition of pathogens and stimulation of beneficial bacteria. Hence, regular consumption of a diet rich in phytochemical contents may beneficially balance the gut microbial ecology, helping prevent GI disorders and, thus, enhancing host health.
Gut Microbiota, Obesity, and Metabolic Syndrome
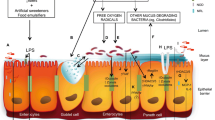
Obesity is commonly defined as body mass index (BMI) values greater than 30 kg/m2 [159, 160] and widely characterized by the pathophysiology of lipid accumulation in body compartments and excessive secretion of pro-inflammatory adipokines by adipocytes and macrophages [161, 162]. Obesity and insulin resistance can lead to the development of metabolic syndromes, including high blood glucose levels, high blood pressure, high serum triglyceride levels, low high-density lipoprotein levels, and large waist circumferences, which increase the risk of heart disease, diabetes mellitus, and stroke [163, 164]. Genetic changes in the body may not fully explain the dramatic increase in the occurrence of obesity in the past few decades [165, 166]; instead, environmental factors, such as high-caloric diet and sedentary lifestyle, are among the major driving forces [167]. An increasing number of studies have shown that the gut microbiome diversity and composition are associated with both diet and human diseases such as obesity, metabolic syndromes, and type 2 diabetes [168,169,170,171,172,173,174]. The gut microbiota transplantation from conventional mice to lean and insulin-sensitive germ-free mice (a process called conventionalization) led to a 60% increase in adiposity and caused insulin resistance [175]. Subsequently, the same laboratory reported that the gut microbial composition in obese (ob/ob) mice showed a 50% reduction in the abundance of Bacteroidetes and an increase in the abundance of Firmicutes compared to the abundances in lean (ob/+) and wild-type (+/+) mice [176]. To understand the causative role of the gut microbiome in obesity, a landmark study was conducted showing that germ-free mice transplanted with the gut microbiota from obese (ob/ob) mice exhibited substantially increased adiposity compared to mice transplanted with the gut microbiota from lean (ob/+) mice [177]. The mechanism was interpreted based on increased capacity for energy harvest, as demonstrated by the increased acetate and butyrate levels. Similar results were also reported on Western-diet-induced obesity C57BL/6J mice, and the microbiota profile was shifted to an increased abundance of Firmicutes and a decreased abundance of Bacteroidetes [178]. Meanwhile, one bacterial class, Mollicutes, in the phylum Firmicutes was found to be significantly up-regulated by diet-induced obesity, which increased host energy harvest, as indicated by the enrichment of microbial genes and KEGG pathways involved in the import and anaerobic fermentation of dietary carbohydrates. The lipopolysaccharides (LPS) are an endotoxin produced at the outer membrane of all gram-negative microbes [179] and cause systemic inflammation to initiate insulin resistance and obesity (a phenomenon called metabolic endotoxemia) [180, 181]. LPS-producing pathogens, including the families Enterobacteriaceae and Desulfovibrionaceae (phylum of Proteobacteria), were found to be enriched in high-fat-diet-induced obesity mice and rats [182, 183]. A significant decrease in fecal Enterobacteriaceae was observed in obese adolescent humans who lost 4–7 kg following a 3-month energy-restricted diet and a physical exercise program [184]. In addition, diurnal oscillations of the microbiota were linked to obesity and metabolic syndromes [185, 186]. Mice fed a high-fat diet with disturbance in circadian rhythm exhibited altered microbial compositions and presented higher weight gains and glucose intolerance than mice fed the same diet with a normal circadian rhythm [185]. Moreover, germ-free mice transplanted with feces from jet-lagged human subjects exhibited dysbiosis, which caused weight gain and glucose intolerance [185].
Cranberry extracts, composed of phenolic acid, flavonols, anthocyanins, and proanthocyanidins, reduced weight gain, visceral adiposity, and insulin resistance by reinforcement of antioxidative defense and prevention of intestinal inflammation in obese mice fed a high-fat/high-sucrose diet [187]. In this study, cranberry extracts restored the metabolic homeostasis in a positive correlation with the abundance of Akkermansia [187]. Strikingly consistent results were observed in mice fed 1% concord grape polyphenols (high in anthocyanins, flavan-3-ols, and flavonols). Grape polyphenols substantially increased the abundance of Akkermansia muciniphila, leading to altered intestinal gene expression. This effect, in turn, regulated intestinal epithelial integrity and inflammatory marker levels, finally resulting in improved lipid deposition (reduced adiposity and weight gain) and glucose tolerance (decreased glucose absorption and increased insulin secretion) [188]. In cafeteria-diet-induced obese rats, a negative correlation was observed between weight gain and enrichment of microbial pathways involved in flavonoid biosynthesis [189]. The results indicated that dysbiosis caused by obesogenic diets could disrupt the biosynthesis of flavonoids, which may lead to decreased host utilization of flavonoids, resulting in an obesity phenotype [189]. The gut microbiota exhibited conversion of flavonoids, which were mainly distributed in the phyla Actinobacteria, Firmicutes, and the families Clostridiaceae, Enterococcaceae, Eubacteriaceae, Erysipelotrichaceae, Lactobacillaceae, Lachnospiraceae, Ruminococcaceae, and Streptococcaceae [32]. In addition, glucoraphanin (which can be metabolized to isothiocyanates), which is abundant in cruciferous vegetables such as broccoli, cauliflower, and mustard, could mitigate obesity, insulin resistance, and related metabolic disorders by browning white fat, inhibiting metabolic endotoxemia-related chronic inflammation, and decreasing oxidative stress in mice fed a high-fat diet [190]. Glucoraphanin exerted its anti-obesity effect via a decrease in the abundances of the phylum Proteobacteria, many bacteria from which can produce endotoxins [182, 190]. Moreover, Ganoderma lucidum, a medicinal mushroom that is used in traditional Chinese medicine, reduced obesity and insulin resistance by suppressing metabolic endotoxemia-related chronic inflammation in mice fed a high-fat diet by decreasing the endotoxin-bearing Proteobacteria and Firmicutes to Bacteroidetes ratios [191]. Fecal transplantation from mice treated with the Ganoderma lucidum extracts to mice fed a high-fat diet could effectively reverse obesity and fat accumulation, as well as the dysregulation of proinflammatory cytokines and intestinal tight junctions. These findings indicate that modulation of the gut microbiota is the mechanism underlying the treatment of obesity.
Current Challenges in and Applications of Human Microbiota Studies
Some of the challenges of the human microbiota studies are associated with interpretation of the metagenomic data with a lack of standard parameters and references and with the potential biases of technicians and methods during sample preparation. These challenges include, but are not limited to, the following: (1) variations in data processing and analysis using different computational tools; (2) difficulty in sample collection of the mucosal and cecal microbes, as well as GI tract tissue under inflammation and oxidative stress; (3) microbiota composition changes during fermentation and degradation and during passage from the rectum to lumen; (4) DNA extraction efficiency for gram-positive and gram-negative bacteria are different, and the results also vary in different chemical isolation kits.
Conclusion
There is solid evidence that gut microbes play key roles in the reduction of the risk of chronic diseases, and phytochemicals are interactive with them. Currently, comprehensive preclinical and clinical studies reveal the gut microbial profiles of both healthy subjects and those suffering from chronic diseases such as inflammatory bowel disease (IBD), colorectal cancer (CRC), and obesity. Dietary intervention seems to be a less aggressive, low risk, and effective approach to prevent and treat such diseases. In the future, we will understand the biological functions of the gut microbiota and the interactions with phytochemicals, which will contribute to the improvement of health benefits for humans.
References
Allaband C, McDonald D, Vázquez-Baeza Y, Minich JJ, Tripathi A, Brenner DA, et al. Microbiome 101: studying, analyzing, and interpreting gut microbiome data for clinicians. Clin Gastroenterol Hepatol. 2019;17(2):218–30. https://doi.org/10.1016/j.cgh.2018.09.017.
Ley RE, Peterson DA, Gordon JI. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell. 2006;124(4):837–48. https://doi.org/10.1016/j.cell.2006.02.017.
Dave M, Higgins PD, Middha S, Rioux KP. The human gut microbiome: current knowledge, challenges, and future directions. Transl Res. 2012;160(4):246–57. https://doi.org/10.1016/j.trsl.2012.05.003.
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14(8):e1002533. https://doi.org/10.1371/journal.pbio.1002533.
Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336(6086):1268–73. https://doi.org/10.1126/science.1223490.
Jarchum I, Pamer EG. Regulation of innate and adaptive immunity by the commensal microbiota. Curr Opin Immunol. 2011;23(3):353–60. https://doi.org/10.1016/j.coi.2011.03.001.
Ashida H, Ogawa M, Kim M, Mimuro H, Sasakawa C. Bacteria and host interactions in the gut epithelial barrier. Nat Chem Biol. 2012;8(1):36–45. https://doi.org/10.1038/nchembio.741.
Ismail AS, Hooper LV. Epithelial cells and their neighbors. IV. Bacterial contributions to intestinal epithelial barrier integrity. Am J Physiol Gastrointest Liver Physiol. 2005;289(5):G779–84. https://doi.org/10.1152/ajpgi.00203.2005.
Ramakrishna BS. Role of the gut microbiota in human nutrition and metabolism. J Gastroenterol Hepatol. 2013;28:9–17. https://doi.org/10.1111/jgh.12294.
El Kaoutari A, Armougom F, Gordon JI, Raoult D, Henrissat B. The abundance and variety of carbohydrate-active enzymes in the human gut microbiota. Nat Rev Microbiol. 2013;11(7):497–504. https://doi.org/10.1038/nrmicro3050.
Kamada N, Chen GY, Inohara N, Núñez G. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol. 2013;14(7):685–90. https://doi.org/10.1038/ni.2608.
Bäumler AJ, Sperandio V. Interactions between the microbiota and pathogenic bacteria in the gut. Nature. 2016;535(7610):85–93. https://doi.org/10.1038/nature18849.
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5):335–6. https://doi.org/10.1038/nmeth.f.303.
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP. DADA2: High-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–3. https://doi.org/10.1038/Nmeth.3869.
Bäckhed F, Fraser CM, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe. 2012;12(5):611–22. https://doi.org/10.1016/j.chom.2012.10.012.
Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146(6):1489–99. https://doi.org/10.1053/j.gastro.2014.02.009.
Morgan XC, Tickle TL, Sokol H, Gevers D, Devaney KL, Ward DV, et al. Dysfunction of the intestinal microbiome in inflammatory bowel disease and treatment. Genome Biol. 2012;13(9):R79. https://doi.org/10.1186/gb-2012-13-9-r79.
Greenblum S, Turnbaugh PJ, Borenstein E. Metagenomic systems biology of the human gut microbiome reveals topological shifts associated with obesity and inflammatory bowel disease. Proc Natl Acad Sci U S A. 2012;109(2):594–9. https://doi.org/10.1073/pnas.1116053109.
Lu B, Li M, Yin R. Phytochemical content, health benefits, and toxicology of common edible flowers: a review (2000–2015). Crit Rev Food Sci Nutr. 2016;56(Suppl 1):S130–48. https://doi.org/10.1080/10408398.2015.1078276.
Yin R, Li T, Tian JX, Xi P, Liu RH. Ursolic acid, a potential anticancer compound for breast cancer therapy. Crit Rev Food Sci Nutr. 2018;58(4):568–74. https://doi.org/10.1080/10408398.2016.1203755.
Liu RH. Health benefits of fruit and vegetables are from additive and synergistic combinations of phytochemicals. Am J Clin Nutr. 2003;78(3 Suppl):517S–20S. https://doi.org/10.1093/ajcn/78.3.517S.
Sun J, Chu YF, Wu X, Liu RH. Antioxidant and antiproliferative activities of common fruits. J Agric Food Chem. 2002;50(25):7449–54.
Lyu Y, Wu L, Wang F, Shen X, Lin D. Carotenoid supplementation and retinoic acid in immunoglobulin A regulation of the gut microbiota dysbiosis. Exp Biol Med (Maywood). 2018;243(7):613–20. https://doi.org/10.1177/1535370218763760.
Gomez A, Petrzelkova K, Yeoman CJ, Vlckova K, Mrázek J, Koppova I, et al. Gut microbiome composition and metabolomic profiles of wild western lowland gorillas (Gorilla gorilla gorilla) reflect host ecology. Mol Ecol. 2015;24(10):2551–65. https://doi.org/10.1111/mec.13181.
Russell W, Duthie G. Plant secondary metabolites and gut health: the case for phenolic acids. Proc Nutr Soc. 2011;70(3):389–96. https://doi.org/10.1017/S0029665111000152.
Wang SY, Chen CT, Sciarappa W, Wang CY, Camp MJ. Fruit quality, antioxidant capacity, and flavonoid content of organically and conventionally grown blueberries. J Agric Food Chem. 2008;56(14):5788–94. https://doi.org/10.1021/jf703775r.
Ferguson PJ, Kurowska EM, Freeman DJ, Chambers AF, Koropatnick J. In vivo inhibition of growth of human tumor lines by flavonoid fractions from cranberry extract. Nutr Cancer. 2006;56(1):86–94. https://doi.org/10.1207/s15327914nc5601_12.
Rice-Evans CA, Miller NJ, Bolwell PG, Bramley PM, Pridham JB. The relative antioxidant activities of plant-derived polyphenolic flavonoids. Free Radic Res. 1995;22(4):375–83.
Duda-Chodak A. The inhibitory effect of polyphenols on human gut microbiota. J Physiol Pharmacol. 2012;63(5):497–503.
Etxeberria U, Fernández-Quintela A, Milagro FI, Aguirre L, Martínez JA, Portillo MP. Impact of polyphenols and polyphenol-rich dietary sources on gut microbiota composition. J Agric Food Chem. 2013;61(40):9517–33. https://doi.org/10.1021/jf402506c.
Wu GD, Chen J, Hoffmann C, Bittinger K, Chen YY, Keilbaugh SA, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334(6052):105–8. https://doi.org/10.1126/science.1208344.
Braune A, Blaut M. Bacterial species involved in the conversion of dietary flavonoids in the human gut. Gut Microbes. 2016;7(3):216–34. https://doi.org/10.1080/19490976.2016.1158395.
Hidalgo M, Oruna-Concha MJ, Kolida S, Walton GE, Kallithraka S, Spencer JP, et al. Metabolism of anthocyanins by human gut microflora and their influence on gut bacterial growth. J Agric Food Chem. 2012;60(15):3882–90. https://doi.org/10.1021/jf3002153.
Braune A, Gütschow M, Engst W, Blaut M. Degradation of quercetin and luteolin by Eubacterium ramulus. Appl Environ Microbiol. 2001;67(12):5558–67. https://doi.org/10.1128/AEM.67.12.5558-5567.2001.
Schoefer L, Mohan R, Schwiertz A, Braune A, Blaut M. Anaerobic degradation of flavonoids by Clostridium orbiscindens. Appl Environ Microbiol. 2003;69(10):5849–54.
Liu RH. Potential synergy of phytochemicals in cancer prevention: mechanism of action. J Nutr. 2004;134(12 Suppl):3479S–85S. https://doi.org/10.1093/jn/134.12.3479S.
de Vries JH, Janssen PL, Hollman PC, van Staveren WA, Katan MB. Consumption of quercetin and kaempferol in free-living subjects eating a variety of diets. Cancer Lett. 1997;114(1–2):141–4.
Miean KH, Mohamed S. Flavonoid (myricetin, quercetin, kaempferol, luteolin, and apigenin) content of edible tropical plants. J Agric Food Chem. 2001;49(6):3106–12.
Selma MV, Espin JC, Tomas-Barberan FA. Interaction between phenolics and gut microbiota: role in human health. J Agr Food Chem. 2009;57(15):6485–501. https://doi.org/10.1021/jf902107d.
Rechner AR, Smith MA, Kuhnle G, Gibson GR, Debnam ES, Srai SK, et al. Colonic metabolism of dietary polyphenols: influence of structure on microbial fermentation products. Free Radic Biol Med. 2004;36(2):212–25.
Wu X, Cao G, Prior RL. Absorption and metabolism of anthocyanins in elderly women after consumption of elderberry or blueberry. J Nutr. 2002;132(7):1865–71. https://doi.org/10.1093/jn/132.7.1865.
Pantelidis GE, Vasilakakis M, Manganaris GA, Diamantidis G. Antioxidant capacity, phenol, anthocyanin and ascorbic acid contents in raspberries, blackberries, red currants, gooseberries and Cornelian cherries. Food Chem. 2007;102(3):777–83. https://doi.org/10.1016/j.foodchem.2006.06.021.
Volden J, Bengtsson GB, Wicklund T. Glucosinolates, L-ascorbic acid, total phenols, anthocyanins, antioxidant capacities and colour in cauliflower (Brassica oleracea L. ssp. botrytis); effects of long-term freezer storage. Food Chem. 2009;112(4):967–76. https://doi.org/10.1016/j.foodchem.2008.07.018.
Llorach R, Martínez-Sánchez A, Tomás-Barberán FA, Gil MI, Ferreres F. Characterisation of polyphenols and antioxidant properties of five lettuce varieties and escarole. Food Chem. 2008;108(3):1028–38. https://doi.org/10.1016/j.foodchem.2007.11.032.
González-Barrio R, Edwards CA, Crozier A. Colonic catabolism of ellagitannins, ellagic acid, and raspberry anthocyanins: in vivo and in vitro studies. Drug Metab Dispos. 2011;39(9):1680–8. https://doi.org/10.1124/dmd.111.039651.
Sun H, Zhang P, Zhu Y, Lou Q, He S. Antioxidant and prebiotic activity of five peonidin-based anthocyanins extracted from purple sweet potato (Ipomoea batatas (L.) Lam.). Sci Rep. 2018;8(1):5018. https://doi.org/10.1038/s41598-018-23397-0.
Zhu Y, Sun H, He S, Lou Q, Yu M, Tang M, et al. Metabolism and prebiotics activity of anthocyanins from black rice (Oryza sativa L.) in vitro. PLoS One. 2018;13(4):e0195754. https://doi.org/10.1371/journal.pone.0195754.
Hanske L, Engst W, Loh G, Sczesny S, Blaut M, Braune A. Contribution of gut bacteria to the metabolism of cyanidin 3-glucoside in human microbiota-associated rats. Brit J Nutr. 2013;109(8):1433–41. https://doi.org/10.1017/S0007114512003376.
Chen L, Jiang B, Zhong C, Guo J, Zhang L, Mu T, et al. Chemoprevention of colorectal cancer by black raspberry anthocyanins involved the modulation of gut microbiota and SFRP2 demethylation. Carcinogenesis. 2018;39(3):471–81. https://doi.org/10.1093/carcin/bgy009.
Gu J, Thomas-Ahner JM, Riedl KM, Bailey MT, Vodovotz Y, Schwartz SJ, et al. Dietary black raspberries impact the colonic microbiome and phytochemical metabolites in mice. Mol Nutr Food Res. 2019;63(8):e1800636. https://doi.org/10.1002/mnfr.201800636.
Paturi G, Butts CA, Monro JA, Hedderley D. Effects of blackcurrant and dietary fibers on large intestinal health biomarkers in rats. Plant Foods Hum Nutr. 2018;73(1):54–60.
Fernández J, García L, Monte J, Villar CJ, Lombó F. Functional anthocyanin-rich sausages diminish colorectal cancer in an animal model and reduce pro-inflammatory bacteria in the intestinal microbiota. Genes (Basel). 2018;9(3):133. https://doi.org/10.3390/genes9030133.
Lee S, Keirsey KI, Kirkland R, Grunewald ZI, Fischer JG, de La Serre CB. Blueberry supplementation influences the gut microbiota, inflammation, and insulin resistance in high-fat-diet-fed rats. J Nutr. 2018;148(2):209–19. https://doi.org/10.1093/jn/nxx027.
Boto-Ordóñez M, Urpi-Sarda M, Queipo-Ortuño MI, Tulipani S, Tinahones FJ, Andres-Lacueva C. High levels of Bifidobacteria are associated with increased levels of anthocyanin microbial metabolites: a randomized clinical trial. Food Funct. 2014;5(8):1932–8. https://doi.org/10.1039/c4fo00029c.
Hester SN, Mastaloudis A, Gray R, Antony JM, Evans M, Wood SM. Efficacy of an anthocyanin and prebiotic blend on intestinal environment in obese male and female subjects. J Nutr Metab. 2018;2018:7497260. https://doi.org/10.1155/2018/7497260.
Khanbabaee K, van Ree T. Tannins: classification and definition. Nat Prod Rep. 2001;18(6):641–9.
Moilanen J, Koskinen P, Salminen JP. Distribution and content of ellagitannins in Finnish plant species. Phytochemistry. 2015;116:188–97. https://doi.org/10.1016/j.phytochem.2015.03.002.
Okuda T, Yoshida T, Hatano T. Ellagitannins as active constituents of medicinal plants. Planta Med. 1989;55(2):117–22. https://doi.org/10.1055/s-2006-961902.
Fecka I. Qualitative and quantitative determination of hydrolysable tannins and other polyphenols in herbal products from meadowsweet and dog rose. Phytochem Anal. 2009;20(3):177–90. https://doi.org/10.1002/pca.1113.
Landete JM. Ellagitannins, ellagic acid and their derived metabolites: a review about source, metabolism, functions and health. Food Res Int. 2011;44(5):1150–60. https://doi.org/10.1016/j.foodres.2011.04.027.
Bialonska D, Kasimsetty SG, Khan SI, Ferreira D. Urolithins, intestinal microbial metabolites of pomegranate ellagitannins, exhibit potent antioxidant activity in a cell-based assay. J Agric Food Chem. 2009;57(21):10181–6.
Romo-Vaquero M, Cortés-Martín A, Loria-Kohen V, Ramírez-de-Molina A, García-Mantrana I, Collado MC, et al. Deciphering the human gut microbiome of urolithin metabotypes: association with enterotypes and potential cardiometabolic health implications. Mol Nutr Food Res. 2019;63(4):e1800958. https://doi.org/10.1002/mnfr.201800958.
García-Villalba R, Beltrán D, Espín JC, Selma MV, Tomás-Barberán FA. Time course production of urolithins from ellagic acid by human gut microbiota. J Agric Food Chem. 2013;61(37):8797–806. https://doi.org/10.1021/jf402498b.
Bialonska D, Ramnani P, Kasimsetty SG, Muntha KR, Gibson GR, Ferreira D. The influence of pomegranate by-product and punicalagins on selected groups of human intestinal microbiota. Int J Food Microbiol. 2010;140(2–3):175–82. https://doi.org/10.1016/j.ijfoodmicro.2010.03.038.
Bialonska D, Kasimsetty SG, Schrader KK, Ferreira D. The effect of pomegranate (Punica granatum L.) byproducts and ellagitannins on the growth of human gut bacteria. J Agric Food Chem. 2009;57(18):8344–9.
Marín L, Miguélez EM, Villar CJ, Lombó F. Bioavailability of dietary polyphenols and gut microbiota metabolism: antimicrobial properties. Biomed Res Int. 2015;2015:905215. https://doi.org/10.1155/2015/905215.
Kawabata K, Yoshioka Y, Terao J. Role of intestinal microbiota in the bioavailability and physiological functions of dietary polyphenols. Molecules. 2019;24(2):370. https://doi.org/10.3390/molecules24020370.
Barnes RC, Krenek KA, Meibohm B, Mertens-Talcott SU, Talcott ST. Urinary metabolites from mango (Mangifera indica L. cv. Keitt) galloyl derivatives and in vitro hydrolysis of gallotannins in physiological conditions. Mol Nutr Food Res. 2016;60(3):542–50. https://doi.org/10.1002/mnfr.201500706.
Burns J, Fraser PD, Bramley PM. Identification and quantification of carotenoids, tocopherols and chlorophylls in commonly consumed fruits and vegetables. Phytochemistry. 2003;62(6):939–47.
Rinninella E, Mele M, Merendino N, Cintoni M, Anselmi G, Caporossi A, et al. The role of diet, micronutrients and the gut microbiota in age-related macular degeneration: new perspectives from the gut–retina axis. Nutrients. 2018;10(11):1677.
Rao AV, Rao LG. Carotenoids and human health. Pharmacol Res. 2007;55(3):207–16.
Fiedor J, Burda K. Potential role of carotenoids as antioxidants in human health and disease. Nutrients. 2014;6(2):466–88.
Magnuson AD, Sun T, Yin R, Liu G, Tolba S, Shinde S, et al. Supplemental microalgal astaxanthin produced coordinated changes in intrinsic antioxidant systems of layer hens exposed to heat stress. Algal Res. 2018;33:84–90. https://doi.org/10.1016/j.algal.2018.04.031.
Ambati R, Phang S-M, Ravi S, Aswathanarayana RG. Astaxanthin: sources, extraction, stability, biological activities and its commercial applications—a review. Mar Drugs. 2014;12(1):128–52.
Sun T, Yin R, Magnuson AD, Tolba SA, Liu GC, Lei XG. Dose-dependent enrichments and improved redox status in tissues of broiler chicks under heat stress by dietary supplemental microalgal astaxanthin. J Agr Food Chem. 2018;66(22):5521–30. https://doi.org/10.1021/acs.jafc.8b00860.
Liu H, Liu M, Fu X, Zhang Z, Zhu L, Zheng X, et al. Astaxanthin prevents alcoholic fatty liver disease by modulating mouse gut microbiota. Nutrients. 2018;10(9):1298.
Bennedsen M, Wang X, Willén R, Wadström T, Andersen LP. Treatment of H. pylori infected mice with antioxidant astaxanthin reduces gastric inflammation, bacterial load and modulates cytokine release by splenocytes. Immunol Lett. 1999;70(3):185–9.
Tuohy KM, Conterno L, Gasperotti M, Viola R. Up-regulating the human intestinal microbiome using whole plant foods, polyphenols, and/or fiber. J Agr Food Chem. 2012;60(36):8776–82. https://doi.org/10.1021/jf2053959.
De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107(33):14691–6. https://doi.org/10.1073/pnas.1005963107.
Tasse L, Bercovici J, Pizzut-Serin S, Robe P, Tap J, Klopp C, et al. Functional metagenomics to mine the human gut microbiome for dietary fiber catabolic enzymes. Genome Res. 2010;20(11):1605–12. https://doi.org/10.1101/gr.108332.110.
Cummings JH, Macfarlane GT. The control and consequences of bacterial fermentation in the human colon. J Appl Bacteriol. 1991;70(6):443–59. https://doi.org/10.1111/j.1365-2672.1991.tb02739.x.
Pryde SE, Duncan SH, Hold GL, Stewart CS, Flint HJ. The microbiology of butyrate formation in the human colon. FEMS Microbiol Lett. 2002;217(2):133–9. https://doi.org/10.1111/j.1574-6968.2002.tb11467.x.
Sealy L, Chalkley R. The effect of sodium butyrate on histone modification. Cell. 1978;14(1):115–21.
Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: can a high fiber diet improve brain health? Neurosci Lett. 2016;625:56–63. https://doi.org/10.1016/j.neulet.2016.02.009.
Candido EP, Reeves R, Davie JR. Sodium butyrate inhibits histone deacetylation in cultured cells. Cell. 1978;14(1):105–13.
Gardian G, Browne SE, Choi DK, Klivenyi P, Gregorio J, Kubilus JK, et al. Neuroprotective effects of phenylbutyrate in the N171-82Q transgenic mouse model of Huntington’s disease. J Biol Chem. 2005;280(1):556–63. https://doi.org/10.1074/jbc.M410210200.
Säemann MD, Böhmig GA, Osterreicher CH, Burtscher H, Parolini O, Diakos C, et al. Anti-inflammatory effects of sodium butyrate on human monocytes: potent inhibition of IL-12 and up-regulation of IL-10 production. FASEB J. 2000;14(15):2380–2. https://doi.org/10.1096/fj.00-0359fje.
Andoh A, Bamba T, Sasaki M. Physiological and anti-inflammatory roles of dietary fiber and butyrate in intestinal functions. JPEN J Parenter Enteral Nutr. 1999;23(5 Suppl):S70–3. https://doi.org/10.1177/014860719902300518.
Leonel AJ, Alvarez-Leite JI. Butyrate: implications for intestinal function. Curr Opin Clin Nutr Metab Care. 2012;15(5):474–9. https://doi.org/10.1097/MCO.0b013e32835665fa.
Dominianni C, Sinha R, Goedert JJ, Pei Z, Yang L, Hayes RB, et al. Sex, body mass index, and dietary fiber intake influence the human gut microbiome. PLoS One. 2015;10(4):e0124599. https://doi.org/10.1371/journal.pone.0124599.
Holscher HD, Caporaso JG, Hooda S, Brulc JM, Fahey GC Jr, Swanson KS. Fiber supplementation influences phylogenetic structure and functional capacity of the human intestinal microbiome: follow-up of a randomized controlled trial. Am J Clin Nutr. 2015;101(1):55–64. https://doi.org/10.3945/ajcn.114.092064.
Vernazza CL, Gibson GR, Rastall RA. Carbohydrate preference, acid tolerance and bile tolerance in five strains of Bifidobacterium. J Appl Microbiol. 2006;100(4):846–53. https://doi.org/10.1111/j.1365-2672.2006.02832.x.
Serino M, Luche E, Gres S, Baylac A, Bergé M, Cenac C, et al. Metabolic adaptation to a high-fat diet is associated with a change in the gut microbiota. Gut. 2012;61(4):543–53. https://doi.org/10.1136/gutjnl-2011-301012.
Guinane CM, Cotter PD. Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therap Adv Gastroenterol. 2013;6(4):295–308. https://doi.org/10.1177/1756283x13482996.
Caussy C, Tripathi A, Humphrey G, Bassirian S, Singh S, Faulkner C, et al. A gut microbiome signature for cirrhosis due to nonalcoholic fatty liver disease. Nat Commun. 2019;10(1):1406. https://doi.org/10.1038/s41467-019-09455-9.
Aron-Wisnewsky J, Clément K. The gut microbiome, diet, and links to cardiometabolic and chronic disorders. Nat Rev Nephrol. 2016;12(3):169–81. https://doi.org/10.1038/nrneph.2015.191.
Manichanh C, Borruel N, Casellas F, Guarner F. The gut microbiota in IBD. Nat Rev Gastroenterol Hepatol. 2012;9(10):599–608. https://doi.org/10.1038/nrgastro.2012.152.
Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14(10):573–84. https://doi.org/10.1038/nrgastro.2017.88.
Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6; discussion 16–9.
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–3. https://doi.org/10.1038/nmeth.3869.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780–5. https://doi.org/10.1073/pnas.0706625104.
Ohkusa T, Sato N, Ogihara T, Morita K, Ogawa M, Okayasu I. Fusobacterium varium localized in the colonic mucosa of patients with ulcerative colitis stimulates species-specific antibody. J Gastroenterol Hepatol. 2002;17(8):849–53.
Ohkusa T, Okayasu I, Ogihara T, Morita K, Ogawa M, Sato N. Induction of experimental ulcerative colitis by fusobacterium varium isolated from colonic mucosa of patients with ulcerative colitis. Gut. 2003;52(1):79–83. https://doi.org/10.1136/gut.52.1.79.
Strauss J, Kaplan GG, Beck PL, Rioux K, Panaccione R, Devinney R, et al. Invasive potential of gut mucosa-derived Fusobacterium nucleatum positively correlates with IBD status of the host. Inflamm Bowel Dis. 2011;17(9):1971–8. https://doi.org/10.1002/ibd.21606.
Sokol H, Lepage P, Seksik P, Dore J, Marteau P. Temperature gradient gel electrophoresis of fecal 16S rRNA reveals active Escherichia coli in the microbiota of patients with ulcerative colitis. J Clin Microbiol. 2006;44(9):3172–7. https://doi.org/10.1128/JCM.02600-05.
Chassaing B, Darfeuille-Michaud A. The commensal microbiota and enteropathogens in the pathogenesis of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1720–8. https://doi.org/10.1053/j.gastro.2011.01.054.
Feller M, Huwiler K, Stephan R, Altpeter E, Shang A, Furrer H, et al. Mycobacterium avium subspecies paratuberculosis and Crohn’s disease: a systematic review and meta-analysis. Lancet Infect Dis. 2007;7(9):607–13. https://doi.org/10.1016/S1473-3099(07)70211-6.
Willing BP, Dicksved J, Halfvarson J, Andersson AF, Lucio M, Zheng Z, et al. A pyrosequencing study in twins shows that gastrointestinal microbial profiles vary with inflammatory bowel disease phenotypes. Gastroenterology. 2010;139(6):1844–54.e1. https://doi.org/10.1053/j.gastro.2010.08.049.
Li WJ, Guo Y, Zhang CY, Wu RY, Yang AY, Gaspar J, et al. Dietary phytochemicals and Cancer chemoprevention: a perspective on oxidative stress, inflammation, and epigenetics. Chem Res Toxicol. 2016;29(12):2071–95. https://doi.org/10.1021/acs.chemrestox.6b00413.
Khor TO, Kong ANT. Curcumin from turmeric spice, anti-inflammatory and antioxidant phytochemical, and cancer prevention. In: Kong ANT, editor. Inflammation, oxidative stress, and cancer: dietary approaches for cancer prevention. Boca Raton, FL: CRC Press; 2014. p. 343–54.
Tsai SJ, Yin MC. Antioxidative and anti-inflammatory protection of oleanolic acid and ursolic acid in PC12 cells. J Food Sci. 2008;73(7):H174–8. https://doi.org/10.1111/j.1750-3841.2008.00864.x.
Ou BX, Bosak KN, Brickner PR, Iezzoni DG, Seymour EM. Processed tart cherry products—comparative phytochemical content, in vitro antioxidant capacity and in vitro anti-inflammatory activity. J Food Sci. 2012;77(5):H105–12. https://doi.org/10.1111/j.1750-3841.2012.02681.x.
Olendzki BC, Silverstein TD, Persuitte GM, Ma YS, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report. Nutr J. 2014;13:5. https://doi.org/10.1186/1475-2891-13-5.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96. https://doi.org/10.1017/S1368980013002115.
Cavicchia PP, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J Nutr. 2009;139(12):2365–72. https://doi.org/10.3945/jn.109.114025.
D’Argenio G, Mazzone G, Tuccillo C, Ribecco MT, Graziani G, Gravina AG, et al. Apple polyphenols extract (APE) improves colon damage in a rat model of colitis. Dig Liver Dis. 2012;44(7):555–62. https://doi.org/10.1016/j.dld.2012.01.009.
Sommer F, Rühlemann MC, Bang C, Höppner M, Rehman A, Kaleta C, et al. Microbiomarkers in inflammatory bowel diseases: caveats come with caviar. Gut. 2017;66(10):1734–8. https://doi.org/10.1136/gutjnl-2016-313678.
Axling U, Olsson C, Xu J, Fernandez C, Larsson S, Ström K, et al. Green tea powder and Lactobacillus plantarum affect gut microbiota, lipid metabolism and inflammation in high-fat fed C57BL/6J mice. Nutr Metab (Lond). 2012;9(1):105. https://doi.org/10.1186/1743-7075-9-105.
Scaldaferri F, Lopetuso LR, Petito V, Cufino V, Bilotta M, Arena V, et al. Gelatin tannate ameliorates acute colitis in mice by reinforcing mucus layer and modulating gut microbiota composition: emerging role for ‘gut barrier protectors’ in IBD? United European Gastroenterol J. 2014;2(2):113–22. https://doi.org/10.1177/2050640614520867.
Lepage P, Häsler R, Spehlmann ME, Rehman A, Zvirbliene A, Begun A, et al. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology. 2011;141(1):227–36. https://doi.org/10.1053/j.gastro.2011.04.011.
Knights D, Silverberg MS, Weersma RK, Gevers D, Dijkstra G, Huang HL, et al. Complex host genetics influence the microbiome in inflammatory bowel disease. Genome Med. 2014;6:107. https://doi.org/10.1186/s13073-014-0107-1.
Davis CD. Nutrigenomics and the prevention of colon cancer. Pharmacogenomics. 2007;8(2):121–4. https://doi.org/10.2217/14622416.8.2.121.
Riscuta G, Dumitrescu RG. Nutrigenomics: implications for breast and colon cancer prevention. Methods Mol Biol. 2012;863:343–58. https://doi.org/10.1007/978-1-61779-612-8_22.
Rustgi AK. The genetics of hereditary colon cancer. Genes Dev. 2007;21(20):2525–38. https://doi.org/10.1101/gad.1593107.
Watson AJ, Collins PD. Colon cancer: a civilization disorder. Dig Dis. 2011;29(2):222–8. https://doi.org/10.1159/000323926.
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–6. https://doi.org/10.1038/nature12506.
Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci U S A. 2008;105(43):16731–6. https://doi.org/10.1073/pnas.0804812105.
Devillard E, McIntosh FM, Duncan SH, Wallace RJ. Metabolism of linoleic acid by human gut bacteria: different routes for biosynthesis of conjugated linoleic acid. J Bacteriol. 2007;189(6):2566–70. https://doi.org/10.1128/JB.01359-06.
Sears CL, Garrett WS. Microbes, microbiota, and colon cancer. Cell Host Microbe. 2014;15(3):317–28. https://doi.org/10.1016/j.chom.2014.02.007.
Wang TT, Cai GX, Qiu YP, Fei N, Zhang MH, Pang XY, et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2012;6(2):320–9. https://doi.org/10.1038/ismej.2011.109.
Kundu P, Blacher E, Elinav E, Pettersson S. Our gut microbiome: the evolving inner self. Cell. 2017;171(7):1481–93. https://doi.org/10.1016/j.cell.2017.11.024.
Martin HM, Campbell BJ, Hart CA, Mpofu C, Nayar M, Singh R, et al. Enhanced Escherichia coli adherence and invasion in Crohn’s disease and colon cancer. Gastroenterology. 2004;127(1):80–93. https://doi.org/10.1053/j.gastro.2004.03.054.
Lu R, Wu SP, Zhang YG, Xia YL, Zhou ZR, Kato I, et al. Salmonella protein AvrA activates the STAT3 signaling pathway in colon cancer. Neoplasia. 2016;18(5):307–16. https://doi.org/10.1016/j.neo.2016.04.001.
Ye ZD, Petrof EO, Boone D, Claud EC, Sun J. Salmonella effector AvrA regulation of colonic epithelial cell inflammation by deubiquitination. Am J Pathol. 2007;171(3):882–92. https://doi.org/10.2353/ajpath.2007.070220.
Shmuely H, Passaro D, Figer A, Niv Y, Pitlik S, Samra Z, et al. Relationship between Helicobacter pylori CagA status and colorectal cancer. Am J Gastroenterol. 2001;96(12):3406–10.
Breuer-Katschinski B, Nemes K, Marr A, Rump B, Leiendecker B, Breuer N, et al. Helicobacter pylori and the risk of colonic adenomas. Digestion. 1999;60(3):210–5. https://doi.org/10.1159/000007661.
Zumkeller N, Brenner H, Zwahlen M, Rothenbacher D. Helicobacter pylori infection and colorectal cancer risk: a meta-analysis. Helicobacter. 2006;11(2):75–80. https://doi.org/10.1111/j.1523-5378.2006.00381.x.
Njei BM, Ditah IC, Appiah J, Jinjuvadia R, Birk JW. Helicobacter pylori infection and the risk of colorectal cancer: a meta-analysis of epidemiologic evidence. J Clin Oncol. 2012;30(4_suppl):408. https://doi.org/10.1200/jco.2012.30.4_suppl.408.
Fierer N, Bradford MA, Jackson RB. Toward an ecological classification of soil bacteria. Ecology. 2007;88(6):1354–64.
Gao ZG, Guo BM, Gao RY, Zhu QC, Qin HL. Microbiota disbiosis is associated with colorectal cancer. Front Microbiol. 2015;6:20. https://doi.org/10.3389/fmicb.2015.00020.
Wu N, Yang X, Zhang R, Li J, Xiao X, Hu Y, et al. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb Ecol. 2013;66(2):462–70. https://doi.org/10.1007/s00248-013-0245-9.
Gao R, Kong C, Huang L, Li H, Qu X, Liu Z, et al. Mucosa-associated microbiota signature in colorectal cancer. Eur J Clin Microbiol. 2017;36(11):2073–83. https://doi.org/10.1007/s10096-017-3026-4.
Zhu Q, Jin Z, Wu W, Gao R, Guo B, Gao Z, et al. Analysis of the intestinal lumen microbiota in an animal model of colorectal cancer. PLoS One. 2014;9(3):e90849. https://doi.org/10.1371/journal.pone.0090849.
McCoy AN, Araujo-Perez F, Azcarate-Peril A, Yeh JJ, Sandler RS, Keku TO. Fusobacterium is associated with colorectal adenomas. PLoS One. 2013;8(1):e53653. https://doi.org/10.1371/journal.pone.0053653.
Ramirez CN, Li WJ, Zhang CY, Wu RY, Su S, Wang C, et al. In vitro-in vivo dose response of ursolic acid, sulforaphane, PEITC, and curcumin in cancer prevention. AAPS J. 2018;20(1):19. https://doi.org/10.1208/s12248-017-0177-2.
Wang L, Li YL, Zhu LD, Yin R, Wang R, Luo XH, et al. Antitumor activities and immunomodulatory of rice bran polysaccharides and its sulfates in vitro. Int J Biol Macromol. 2016;88:424–32. https://doi.org/10.1016/j.ijbiomac.2016.04.016.
Florowska A, Krygier K, Florowski T, Dłużewska E. Prebiotics as functional food ingredients preventing diet-related diseases. Food Funct. 2016;7(5):2147–55. https://doi.org/10.1039/c5fo01459j.
Walker AW, Ince J, Duncan SH, Webster LM, Holtrop G, Ze X, et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J. 2011;5(2):220–30. https://doi.org/10.1038/ismej.2010.118.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63. https://doi.org/10.1038/nature12820.
Hervert-Hernández D, Pintado C, Rotger R, Goñi I. Stimulatory role of grape pomace polyphenols on Lactobacillus acidophilus growth. Int J Food Microbiol. 2009;136(1):119–22. https://doi.org/10.1016/j.ijfoodmicro.2009.09.016.
Puupponen-Pimiä R, Nohynek L, Hartmann-Schmidlin S, Kähkönen M, Heinonen M, Määttä-Riihinen K, et al. Berry phenolics selectively inhibit the growth of intestinal pathogens. J Appl Microbiol. 2005;98(4):991–1000. https://doi.org/10.1111/j.1365-2672.2005.02547.x.
Liu Z, Chen Z, Guo H, He D, Zhao H, Wang Z, et al. The modulatory effect of infusions of green tea, oolong tea, and black tea on gut microbiota in high-fat-induced obese mice. Food Funct. 2016;7(12):4869–79. https://doi.org/10.1039/c6fo01439a.
Tombola F, Campello S, De Luca L, Ruggiero P, Del Giudice G, Papini E, et al. Plant polyphenols inhibit VacA, a toxin secreted by the gastric pathogen Helicobacter pylori. FEBS Lett. 2003;543(1–3):184–9.
Burger O, Ofek I, Tabak M, Weiss EI, Sharon N, Neeman I. A high molecular mass constituent of cranberry juice inhibits Helicobacter pylori adhesion to human gastric mucus. FEMS Immunol Med Microbiol. 2000;29(4):295–301. https://doi.org/10.1111/j.1574-695X.2000.tb01537.x.
Chatterjee A, Yasmin T, Bagchi D, Stohs SJ. Inhibition of Helicobacter pylori in vitro by various berry extracts, with enhanced susceptibility to clarithromycin. Mol Cell Biochem. 2004;265(1–2):19–26.
Romero C, Medina E, Vargas J, Brenes M, De Castro A. In vitro activity of olive oil polyphenols against Helicobacter pylori. J Agric Food Chem. 2007;55(3):680–6. https://doi.org/10.1021/jf0630217.
Lee HC, Jenner AM, Low CS, Lee YK. Effect of tea phenolics and their aromatic fecal bacterial metabolites on intestinal microbiota. Res Microbiol. 2006;157(9):876–84. https://doi.org/10.1016/j.resmic.2006.07.004.
Maru GB, Hudlikar RR, Kumar G, Gandhi K, Mahimkar MB. Understanding the molecular mechanisms of cancer prevention by dietary phytochemicals: from experimental models to clinical trials. World J Biol Chem. 2016;7(1):88–99. https://doi.org/10.4331/wjbc.v7.i1.88.
Poskitt EME. Defining childhood obesity: the relative body mass index (BMI). Acta Paediatr. 1995;84(8):961–3. https://doi.org/10.1111/j.1651-2227.1995.tb13806.x.
Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115(16):2111–8. https://doi.org/10.1161/Circulationaha.106.635011.
AMA adopts new policies on second day of voting at annual meeting. Press release of the American Medical Association. 2013. http://www.npr.org/documents/2013/jun/ama-resolution-obesity.pdf.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66.
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–8. https://doi.org/10.1161/01.CIR.0000111245.75752.C6.
American Heart Association. What Is metabolic syndrome? 2015. https://www.heart.org/-/media/files/health-topics/answers-by-heart/what-is-metabolic-syndrome-300322.pdf?la=en&hash=3B60478685B71C2CD6CEB93782DAE8B7EAD33445.
Xia Q, Grant SFA. The genetics of human obesity. Ann N Y Acad Sci. 2013;1281(1):178–90.
Conterno L, Fava F, Viola R, Tuohy KM. Obesity and the gut microbiota: does up-regulating colonic fermentation protect against obesity and metabolic disease? Genes Nutr. 2011;6(3):241–60.
Rothschild D, Weissbrod O, Barkan E, Kurilshikov A, Korem T, Zeevi D, et al. Environment dominates over host genetics in shaping human gut microbiota. Nature. 2018;555(7695):210–5. https://doi.org/10.1038/nature25973.
Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol. 2009;9(5):313–23. https://doi.org/10.1038/nri2515.
Gentile CL, Weir TL. The gut microbiota at the intersection of diet and human health. Science. 2018;362(6416):776–80. https://doi.org/10.1126/science.aau5812.
Chen X, Devaraj S. Gut microbiome in obesity, metabolic syndrome, and diabetes. Curr Diab Rep. 2018;18(12):129.
Kovatcheva-Datchary P, Arora T. Nutrition, the gut microbiome and the metabolic syndrome. Best Pract Res Clin Gastroenterol. 2013;27(1):59–72. https://doi.org/10.1016/j.bpg.2013.03.017.
Parekh PJ, Balart LA, Johnson DA. The influence of the gut microbiome on obesity, metabolic syndrome and gastrointestinal disease. Clin Transl Gastroenterol. 2015;6:e91. https://doi.org/10.1038/ctg.2015.16.
Mazidi M, Rezaie P, Kengne AP, Mobarhan MG, Ferns GA. Gut microbiome and metabolic syndrome. Diabetes Metab Syndr. 2016;10(2 Suppl 1):S150–7. https://doi.org/10.1016/j.dsx.2016.01.024.
Ussar S, Fujisaka S, Kahn CR. Interactions between host genetics and gut microbiome in diabetes and metabolic syndrome. Mol Metab. 2016;5(9):795–803. https://doi.org/10.1016/j.molmet.2016.07.004.
Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101(44):15718–23.
Ley RE, Bäckhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102(31):11070–5. https://doi.org/10.1073/pnas.0504978102.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. https://doi.org/10.1038/nature05414.
Turnbaugh PJ, Bäckhed F, Fulton L, Gordon JI. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3(4):213–23.
Erridge C, Bennett-Guerrero E, Poxton IR. Structure and function of lipopolysaccharides. Microbes Infect. 2002;4(8):837–51. https://doi.org/10.1016/S1286-4579(02)01604-0.
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56(7):1761–72. https://doi.org/10.2337/db06-1491.
Beutler B, Rietschel ET. Innate immune sensing and its roots: the story of endotoxin. Nat Rev Immunol. 2003;3(2):169–76. https://doi.org/10.1038/nri1004.
Zhang C, Zhang M, Wang S, Han R, Cao Y, Hua W, et al. Interactions between gut microbiota, host genetics and diet relevant to development of metabolic syndromes in mice. ISME J. 2010;4(2):232–41. https://doi.org/10.1038/ismej.2009.112.
de La Serre CB, Ellis CL, Lee J, Hartman AL, Rutledge JC, Raybould HE. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am J Physiol Gastrointest Liver Physiol. 2010;299(2):G440–8. https://doi.org/10.1152/ajpgi.00098.2010.
Sotos M, Nadal I, Marti A, Martínez A, Martin-Matillas M, Campoy C, et al. Gut microbes and obesity in adolescents. In: Proceedings of the 1st international immunonutrition workshop, Valencia, Spain, 3–5 October 2007. Cambridge: Cambridge University Press; 2008.
Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159(3):514–29. https://doi.org/10.1016/j.cell.2014.09.048.
Thaiss CA, Levy M, Korem T, Dohnalová L, Shapiro H, Jaitin DA, et al. Microbiota diurnal rhythmicity programs host transcriptome oscillations. Cell. 2016;167(6):1495–510.e12.
Anhê FF, Roy D, Pilon G, Dudonné S, Matamoros S, Varin TV, et al. A polyphenol-rich cranberry extract protects from diet-induced obesity, insulin resistance and intestinal inflammation in association with increased Akkermansia spp. population in the gut microbiota of mice. Gut. 2015;64(6):872–83. https://doi.org/10.1136/gutjnl-2014-307142.
Roopchand DE, Carmody RN, Kuhn P, Moskal K, Rojas-Silva P, Turnbaugh PJ, et al. Dietary polyphenols promote growth of the gut bacterium Akkermansia muciniphila and attenuate high-fat diet-induced metabolic syndrome. Diabetes. 2015;64(8):2847–58. https://doi.org/10.2337/db14-1916.
Kaakoush NO, Martire SI, Raipuria M, Mitchell HM, Nielsen S, Westbrook RF, et al. Alternating or continuous exposure to cafeteria diet leads to similar shifts in gut microbiota compared to chow diet. Mol Nutr Food Res. 2017;61(1):1500815. https://doi.org/10.1002/mnfr.201500815.
Nagata N, Xu L, Kohno S, Ushida Y, Aoki Y, Umeda R, et al. Glucoraphanin ameliorates obesity and insulin resistance through adipose tissue browning and reduction of metabolic endotoxemia in mice. Diabetes. 2017;66(5):1222–36. https://doi.org/10.2337/db16-0662.
Chang CJ, Lin CS, Lu CC, Martel J, Ko YF, Ojcius DM, et al. Ganoderma lucidum reduces obesity in mice by modulating the composition of the gut microbiota. Nat Commun. 2015;6:7489. https://doi.org/10.1038/ncomms8489.
Acknowledgements
We thank all members of Dr. Ah-Ng Kong’s lab for the helpful discussions and preparation of the manuscript.
Funding
This review was supported by R01 CA200129 from the National Cancer Institute (NCI) and R01 AT009152 from the National Center for Complementary and Integrative Health (NCCIH) of the National Institutes of Health (NIH) to Dr. Ah-Ng Tony Kong.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Microbiome
Rights and permissions
About this article
Cite this article
Yin, R., Kuo, HC., Hudlikar, R. et al. Gut Microbiota, Dietary Phytochemicals, and Benefits to Human Health. Curr Pharmacol Rep 5, 332–344 (2019). https://doi.org/10.1007/s40495-019-00196-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-019-00196-3