Abstract
Pediatric obesity is associated with negative health and psychosocial consequences. However, obesity may not uniformly affect all populations. Limited research has investigated the factors that contribute to the incidence and persistence of overweight and obesity among children with autism spectrum disorder (ASD). This review systematically examined the prevalence rate of overweight and obesity among children with ASD. The majority of studies suggest that children with ASD may be at a greater risk for excess weight gain compared to typically developing peers. Additionally, this review investigated potential contributing factors to the etiology and maintenance of obesity within this population. Research should continue to investigate excess weight gain in this population in order to adapt weight loss interventions for children with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the past several decades, rates of pediatric overweight and obesity rose drastically. Although there are many pathways that contribute to childhood obesity, individuals who are highly responsive to food and its rewarding properties may be at an increased risk for weight gain over time. In 2014, 17% of the children and adolescents in the USA met the criteria for obesity (Ogden et al. 2014). As opposed to adults, weight status in youth is categorized using age and sex-adjusted percentiles, such that the overweight category encompasses children in the 85th–95th body mass index (BMI) percentiles, whereas obesity is defined as a BMI equal to or greater than the 95th percentile. The health consequences associated with overweight and obesity have detrimental and long-lasting effects. Research has consistently shown that overweight children are at risk for a number of negative health outcomes, including Type 2 Diabetes Mellitus (Hannon et al. 2005), cardiovascular disease (Freedman et al. 2007), and fatty liver disease (Schwimmer et al. 2006). Overweight and obesity are also associated with psychosocial factors, including decreased quality of life (Fallon et al. 2005; Schwimmer et al. 2003), increased risk of depression (Boutelle et al. 2010), and disordered eating behaviors (Glasofer et al. 2007; Tanofsky-Kraff et al. 2004). Additionally, a neuropsychological review paper showed that children who are overweight and obese have poorer neurocognitive functioning across a variety of domains, including attention problems, executive functioning deficits, visuospatial difficulties, and impaired motor skills (Liang et al. 2014).
In addition to negative health consequences, it also appears that the course of obesity is relatively stable from childhood onward. Children who are overweight are more likely to be overweight in both adolescence and adulthood than children who are of normal weight (Reilly et al. 2003). Not only does weight trajectory appears relatively stable across time and development, research has also linked obesity in childhood to increases in both health risks and mortality rates in adulthood (Reilly and Kelly 2011). Yet, losing just 5–10% of the body weight can have a positive impact on many of the negative health outcomes related to overweight and obesity and in some cases may even reverse the harmful effects. Thus, given the persistent developmental trajectory, as well as the individual consequences and rising public health costs of pediatric obesity, prevention and early intervention efforts should be developed to target weight loss in children and adolescents.
However, overweight and obesity may not uniformly affect all populations the same way. Emerging evidence suggests that children with autism spectrum disorder (ASD) may fall into that category. Defined by impairments in social behavior, communication difficulties, and stereotyped behavioral patterns, ASDs are neurodevelopmental disorders that affect an estimated 1 in 88 children in the USA (DMNSY Developmental 2014). In research and clinical settings, the links between underweight and picky eating with ASD are often highlighted. However, the overweight end of the spectrum has been less researched, although it affects a large number of youth diagnosed with ASD. Research studies indicate that children with ASD have a 1.42 greater risk of developing obesity compared to children without ASD (Curtin et al. 2010). Among adults with ASD, rates of obesity may be as high as 34% (Croen et al. 2015), suggesting that the health and psychosocial problems associated with excess weight extend well beyond childhood. Given the pressing needs of children with ASD, weight loss may not be a primary target of intervention for families and researchers alike. Therefore, raising awareness about the obesity rates among this population, as well as undertaking research efforts to provide insight into the development and persistence of weight gain, is crucial.
What factors could be contributing to the increased prevalence of overweight and obesity among children and adolescents with ASD? In this review, a number of potential influences—ranging from genetics to environmental influences—will be considered in contributing to both the etiology and the maintenance of obesity within this population. First, this review will establish whether rates of overweight and obesity are higher among children with ASD by systematically examining the literature and analyzing reported prevalence rates. The remainder of the paper will then focus on potential factors that impact the etiology and maintenance of overweight and obesity among children with ASD. Given the multitude of negative health sequelae, as well as psychosocial and neurocognitive consequences associated with overweight and obesity, it is crucial to understand the mechanisms contributing to these increased rates, and develop interventions that specifically target associated factors. In particular, efforts should be specifically designed for children with ASD and targeted in ways that are adaptive and suit the specialized needs in order to be successful in this population.
Prior to discussing possible explanations for increased weight in children with ASD, it is important to first assess the potential relationship between ASD and obesity status by conducting a comprehensive review of published studies. While it appears that children with ASD have equal to or greater rates of overweight and obesity than the general population (Broder-Fingert et al. 2014; Curtin et al. 2010), prevalence rates are often not systematically reported across studies. Therefore, this review seeks to compile the available information regarding prevalence rates across studies in order to consolidate the literature to date.
Methods
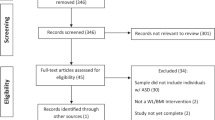
The authors conducted a comprehensive review of the literature examining obesity prevalence rates for children with ASD. This literature review used the following search terms: “Autism,” “Autism Spectrum Disorder,” “Obesity,” “Overweight,” and “Children.” The authors included PubMed (which encompasses MEDLINE) and PsychInfo as search engines. The search results initially returned 386 unique articles. Inclusion criteria for empirical studies included publication between 1995 and 2016 in a peer-reviewed journal; study population that met criteria for autism or ASD; reported prevalence rates of overweight, obesity, or both within the study sample; and sample including youth of at least 2 years old but not older than 20 years of age. The authors excluded studies from this review if the sample included only developmental or intellectual disabilities, or only included adults. This review also excluded single case study designs as well as studies that were exclusively within the context of a medication trial in order to better understand the prevalence of obesity apart from any potential medication side effect. A total of 31 articles met inclusion criteria for this review.
Results
Of the 31 articles that met criteria for this review, 21 studies reported prevalence rates of overweight and obesity for youth with ASD within the USA. Two of the studies (Evans et al. 2012; Must et al. 2013) reported on the same sample from the Children’s Activity and Meal Patterns Study, and thus, this sample was only counted once. In total, 16 out of 20 studies (80%) reported the prevalence of overweight and obesity in youth with ASD to be equal to or greater than typically developing children (see Table 1). The prevalence of overweight/obesity status in the overall US population of youth age 2–18 years was 31.80% for data collected between 2011 and 2012 (Ogden et al. 2014). Among American children ages 2.5 to 5 years old with ASD, an estimated 33% have a BMI over the 85th percentile (Egan et al. 2013), compared to only 22.80% in the same age range without ASD (Ogden et al. 2014). American adolescents with ASD also have higher rates of overweight and obesity compared to their peers (McCoy et al. 2016; Phillips et al. 2014; Rimmer et al. 2010). A chart review study with over 6500 individuals ages 2–20 years old found that participants with ASD were almost 5 times more likely to be obese compared to control participants without ASD (Broder-Fingert et al. 2014). The Autism Speaks Autism Treatment Network reported on overweight and obesity rates for approximately 5000 children with ASD, finding that 18% of the sample met criteria for obesity while another 33.60% were considered overweight based on BMI standards (Hill et al. 2015). Both small and large sample size studies consistently reported greater prevalence of overweight and obesity among youth with ASD compared to age-matched peers.
Only two studies reported overweight and obesity rates in ASD youth as lower than the general population, and the findings were mixed. In a study of children ages 2–11 years old, researchers reported that while children ages 2–5 with ASD did have significantly greater rates of overweight and obesity compared to age and gender-matched controls, children in the 6–11-year-old category with ASD did not differ in overweight and obesity rates compared to typically developing peers (Hyman et al. 2012). Another study reported combined overweight and obesity rates for children with ASD (28.10%) to be greater than the typically developing children in the sample (19.90%), although this difference was attenuated after accounting for other conditions (Corvey et al. 2016). Similarly, an additional study found no differences in overweight and obesity rates among 2–13 year olds with ASD and age-matched controls (Barnhill et al. 2017). Finally, although one study reported the rates of obesity among children with ASD to be lower than the national average (8.20%), this same study also found that children with ASD were almost twice as likely to be obese compared to typically developing children included in the study (Shedlock et al. 2016). However, this study only examined the rates of obesity within this sample, and thus, conclusions about the total combined obesity and overweight prevalence rates cannot be drawn.
This review also included ten studies conducted outside of the USA for comparison (see Table 2). Relatively high rates of overweight and obesity are documented internationally as well, with similar overweight and obesity rates for children with ASD reported in China (31.50–37.90%; Xia et al. 2010; Xiong et al. 2009), Canada (42.60%; Ho et al. 1997), Turkey (32.3%; Bicer and Alsaffar 2013), Australia (35%; Granich et al. 2016), and the United Arab Emirates (52.17%; Attlee et al. 2015). A study in Israel showed greater BMI-for-age scores among 3- to 6-year-old children with ASD diagnoses, even while noting nutritional deficits for this group (Shmaya et al. 2015). A study conducted in the United Arab Emirates reported the highest rates of overweight and obesity, with almost 74% of the sample meeting criteria for excess body weight (Attlee et al. 2015). Yet, it should be noted that only 23 participants were included in this small sample, and thus, only limited conclusions can be drawn from this study alone.
In contrast, a study in Oman among 3- to 5-year-old preschool children with ASD (n = 128) reported that no child in the study met criteria for overweight or obesity (Al-Farsi et al. 2011). Although prevalence data on obesity in typically developing preschool-age children in Oman is sparse (Abdul-Rasoul 2012), overweight rates for this age group are smaller (less than 2%) than other countries in the Eastern Mediterranean Region (Alasfoor and Mohammed 2009; Musaiger 2011); thus, it is not surprising that children with ASD in this sample did not differ in overweight status given these base rates. Studies should be replicated and compared against national averages for overweight and obesity in order to better understand the impact of excess weight gain for children living in countries outside of the USA.
It should be noted that different metrics and assessment techniques make it difficult to compare results across studies. Varying sample sizes may also unduly influence results; for instance, in this review, the sample size included varied from as few as eight individuals to over 6000. Additionally, sample sizes are generally gathered from academic studies, or ASD treatment networks, such as Autism Speaks. Therefore, it is possible that the study samples consist of families who are treatment seeking, and may be more actively involved in ASD care compared to other families. Future research should seek to apply meta-analytic techniques in order to provide common metrics and effect sizes for these findings.
Discussion
Research evidence indicates a consistent picture: children with ASD show similar or even an increased prevalence of overweight and obesity than typically developing children. These higher rates appear not only within the USA but internationally as well. The unanswered question as to why the rates of overweight and obesity are higher among children and adolescents with ASD compared to typically developing youth is a puzzling one, with multiple factors exerting influences alone and in complex interactions. Thus, there is a critical need to elucidate the factors that contribute to the incidence and persistence of overweight and obesity in this population, with an emphasis on targeting these maintaining factors in order to promote weight loss and improve overall health. The following discussion seeks to identify crucial factors that may be contributing to excess weight gain for youth with ASD, further highlighting the need for targeted weight loss intervention programs developed specifically for this population.
Etiology and Development of Overweight and Obesity in Children with ASD
While the etiology of obesity is multi-determined, this review will discuss relevant influences, such as the role of medication, the contribution of genetics, the impact of the obesogenic environment, and the relevance of parent feeding behaviors that may be related to excess weight gain in this population. Several key factors may be contributing to the rates of overweight and obesity in children with ASD, including physical limitations (Pan 2008), unusual dietary patterns (Curtin et al. 2005), sensory integration difficulties (Cermack et al. 2010), and challenging mealtime behaviors (Nadon et al. 2011). The potential impact of each factor on children with ASD will be discussed in the following sections.
Medication Hypothesis
Several different hypotheses from the research literature could help explain why children with ASD have equal to higher prevalence rates of obesity than typically developing children. An estimated 56% of the children with ASD are prescribed medication to help manage symptoms and behaviors related to the diagnosis (Pringle et al. 2012). The medication hypothesis focuses on the various different prescription medications that children with ASD are often prescribed—from stimulants to selective serotonin reuptake inhibitors (SSRIs) to atypical antipsychotics (Pringle et al. 2012)—and the side effects commonly associated with these medications, including weight gain, increased appetite, and metabolic changes.
In fact, the medication information sheet for risperidone (RISPERDAL®), an atypical antipsychotic approved by the Food and Drug Administration to target irritability and aggression in children with ASD, warns that “when treating pediatric patients with RISPERDAL® for any indication, weight gain should be assessed against that expected with normal growth” (Janssen Pharmaceuticals 2014). In addition to irritability and aggression, risperidone is also prescribed to target disruptive behaviors, such as self-injury, impulsivity, and the restricted, repetitive stereotype behaviors often seen in ASD (McCracken et al. 2002; McDougle et al. 1998; McDougle et al. 2005). Children with ASD and behavioral problems who took prescribed risperidone showed greater weight gain and increased appetite compared to a placebo in clinical trials (McCracken et al. 2002). One study showed an average increase of 7.5 kg (16.5 lb) over 12 months of risperidone among children and adults with ASD and other psychiatric disorders, with the majority of the weight gain occurring within the first 6 months of starting the antipsychotic (Janssen Pharmaceuticals 2014). After 1 year of use, children and adolescents gained comparable amounts of weight while taking this medication, with children ages 8–12 years old gaining 8.2 kg (18.08 lb) and adolescents ages 13–16 years old gaining 8.4 kg (18.52 lb) on average (Hellings et al. 2001). The Pediatric Psychopharmacology Autism Network reported an average 5.1 kg (11.24 lb) increase in weight over a 6-month trial of risperidone in children 5–17 years old with autism (Research Units on Pediatric Psychopharmacology Autism Network 2005). Among youth treated with risperidone for a variety of psychiatric conditions, individuals who started the medication treatment at a lower BMI gained more weight at the end of a 3-year study period (Calarge et al. 2009).
Double-blind placebo-controlled clinical trials produced mixed results as to the efficacy of SSRIs in targeting behavioral problems in children with ASD, with one study finding a reduction in repetitive behaviors but not overall global behavior symptoms for the medication group (Hollander et al. 2005), whereas another study did not report any treatment benefits for children taking an SSRI compared to a placebo control (McDougle et al. 2000). A review paper investigating the use of SSRIs for children with ASD found an overall moderate impact on behavioral symptoms and global functioning; however, the authors cautioned that these improvements were often accompanied by side effects related to the medication (West et al. 2009). In fact, the evidence suggests that children with ASD may experience a greater number of side effects than typically developing children, even at small medication doses (West et al. 2009). Documented side effects of SSRIs include trouble sleeping, gastrointestinal disturbances, appetite and weight changes, and suicidal ideation (Ferguson 2001; Jerrell 2010; Safer and Zito 2006). However, the atypical antipsychotics are more known for increasing appetite and weight gain across a variety of psychiatric disorders (Almandil et al. 2013; Bak et al. 2014; Tschoner et al. 2007), with a more clearly defined relationship with weight gain in children among this class of drugs, compared to SSRIs (Reekie et al. 2015; Yoon et al. 2016). It is important to acknowledge that children with ASD may be taking a combination of medications, and thus, it can be difficult without methodically rigorous randomized controlled clinical trials to fully evaluate the efficacy of each drug in isolation, and to separate out potential side effects, such as weight gain, for each medication uniquely.
However, a growing body of research literature suggests mixed effects in terms of weight gain from these medications. One study found that risperidone did not relate to a significant weight change from baseline to a 12-month follow-up, though the authors recommend interpreting these results cautiously, as only 18 individuals were included in the longitudinal analyses (Demb et al. 2011). Additionally, studies that have controlled for psychotropic medication use found no impact on weight in children with ASD across medication categories (Broder-Fingert et al. 2014; Egan et al. 2013). Further, stimulant use is thought to decrease, not increase, appetite, and weight, particularly for children with ADHD (American Academy of Pediatrics 2001; Charach et al. 2004; Cormier 2008; Zachor et al. 2006). Thus, given the recent inconsistent findings, it appears that while medication use might play a role in increasing weight among children with ASD, it is unlikely that medication alone contributes solely to the observed rates of overweight and obesity in this population.
Genetic Predispositions
Obesity has a highly genetic and heritable component, with estimates regarding BMI and obesity ranging from 0.60–0.74 in children (Haworth et al. 2008). Thus, genetic predispositions account for one of many independent contributors to childhood obesity (Farooqi 2005; Silventoinen et al. 2010; Wardle et al. 2008). Researchers found a much smaller influence of shared environmental factors (0.12–0.22; Haworth et al. 2008), though gene × environment interactions should also be considered. Similarly, ASDs have also been shown to have a high degree of genetic influence, with a moderate genetic heritability found in twin and family studies, ranging from 37 (Hallmayer et al. 2011) to 54% (Gaugler et al. 2014). Researchers established interactive databases to examine clinical, genetic, and neurobiological data to better understand the risks associated with ASD (Fischbach and Lord 2010).
Researchers identified 36 common genes involved in both obesity and ASD (Sharma et al. 2012). One particular area of interest involves the microdeletion 11p14.1, which has been implicated in both autism and obesity (Shinawi et al. 2011). The 16p11.2 copy number variant, deletion is implicated both in ASD and in increased BMI (Bochukova et al. 2010; Walters et al. 2010). Another area of research interest involves brain-derived neurotrophic factor (BDNF). BDNF deletion is found in 76.50% of the patients with autism compared to 42.30% of the patients without in a sample of individuals with WAGR syndrome (a genetic syndrome also known as WAGR complex or Wilms tumor-aniridia syndrome), which suggests a potential role for BDNF in understanding the increased risk of autism for these patients (Fischbach et al. 2005; Xu et al. 2008). While novel technology and updated scientific methods may continue to advance the understanding of the human genome, it is important to consider that the majority of genetic predispositions are merely probabilistic, as opposed to deterministic. Future research is needed to better understand what genetic link, if any, connects ASD and obesity.
Obesogenic Environment
The current obesogenic environment—replete with abundant food cues plus limited opportunities for physical activity—is established as one of the leading contributors to excessive weight gain occurring among today’s children and youth (Kirk et al. 2010; Swinburn et al. 1999). Individuals are thought to be more responsive to these highly palatable food cues and, given the ease at which these foods can be accessed, are thought to overeat and thus gain weight (Jansen 1998; Polivy et al. 2008). Of note, this explanation for the increasing rates of overweight and obesity among youth in the USA does not apply exclusively to typically developing children. Newly developed treatments are targeting food cue responsivity and overeating in children (Boutelle et al. 2015b), which emphasize the difference between cravings (“head hunger”) and physiological hunger states (“stomach hunger”). However, children with ASD may have a harder time distinguishing between these two internal states, and may not be able to think flexibly enough to grasp abstract, metaphoric concepts such as “head” versus “stomach” hunger. Strategies targeted at circumventing the obesogenic environment might work well for typically developing children, but differences in cognition and information processing may prohibit success in these treatment programs for children with ASD. Thus, children with ASD may be more susceptible to food cues around them and have less opportunities to understand how to modify their environments or practice skills that would allow them to limit excess weight gain.
Parent Feeding Practices
Restrictive parent feeding practices show a relationship with disordered eating (Matheson et al. 2015) and greater BMI in typically developing children (Faith et al. 2004). Higher levels of eating in the absence of hunger are related to greater maternal use of psychological control and parent monitoring of feeding behaviors (Liang et al. 2016). Compared to typically developing children, mothers report greater emotional response and behavioral control practices, but less control of their child’s feeding situation, for children with ASD (Martins et al. 2008). Parent control of child feeding is inversely related to ASD severity (Martins et al. 2008). Restrictive and controlling feeding practices may have unintentional effects on weight gain and growth trajectories. Providing parents with psychoeducation as to which strategies to implement in feeding their children may serve to decrease rates of overweight or obesity or, at the very least, to limit excess weight gain.
Physical Limitations
Children with ASD frequently have physical limitations, such as low muscle tone and postural instability, which limit mobility. Additionally, children with ASD often have coordination and motor control deficits (Fournier et al. 2010; Green et al. 2009), which also contribute to decreased physical activity and increased sedentary behaviors. Coupled with difficulties in interpersonal interactions, children with ASD may be less likely to engage in active play during recess or to join an afterschool recreational sports league, with more limited opportunities to burn calories and receive health benefits associated with regular physical activity. A research study in which children with ASD wore accelerometers over 7 days to track physical activity found that children ages 9–11 spend on average 17 min per day in moderate to vigorous physical activity, whereas adolescents ages 12–18 spend only 10 min per day (MacDonald et al. 2011). The totals for these age groups are much less than the recommended 60 min per day guidelines established by the American Academy of Pediatrics. In fact, across age categories, this study showed that children with ASD were engaged in vigorous physical activity for an average of only 1 min per day (MacDonald et al. 2011).
Increased sedentary behaviors and decreased physical activities are documented among children with ASD, particularly for older children who were found to be significantly more inactive than younger children in a recent study (MacDonald et al. 2011). The amount of time that children with ASD spend on computers and screens also contributes to increased sedentary behaviors. Studies indicate that high percentages of youth with ASD (60.30% in one sample) reported spending most of their time watching television or videos, and nearly half of the sample (41.40%) endorsed playing video games with most of their free time outside of school (Mazurek et al. 2012). Compared to only 18% of the youth without ASD reporting high levels of video game time, children with ASD spend substantially greater periods of time interfacing with screens (Mazurek et al. 2012). One study reported that 94% of the participants (14 children ages 8–14 years old with ASD) cited use of technology and screens as the most frequent reason for not participating in physical activity after school, and that children in this study with low levels of physical activity rated technology-interfaced activities as more exciting than exercise (Obrusnikova and Cavalier 2011). Perhaps children with ASD may prefer to use screens as a less intimidating interaction platform, or that parents often employ screens as a method to decrease disruptive behaviors, or likely a combination of both. Regardless the reason, the increased screen and technology use could be contributing to physical activity deficits and excess weight gain over time for these youth.
Unusual Dietary Patterns
Children with ASD also have unusual dietary patterns that could be contributing to the increased prevalence of overweight and obesity within this population. Compared to typically developing children, children with ASD show increased consumption of sugar-sweetened beverages and snack foods (Evans et al. 2012). A recent meta-analysis reports that one serving of a sugar-sweetened beverage per day was associated with a 0.06 increase in BMI unit for children (Malik et al. 2013). Consuming an excess of 200 to 250 cal per day in any form—whether from a sugar-sweetened beverage, a snack food, or excess portion sizes—can equate to an extra 20 to 25 lb per year. Moreover, research also indicates that children with ASD tend to eat less fruits and vegetables than their typically developing peers (Evans et al. 2012). Both behavioral observations and parent-reported measures identify vegetables as the most commonly rejected food group among children with ASD (Sharp et al. 2013), and are rejected more by children with ASD compared to typically developing peers (Bandini et al. 2010). The preference towards calorically dense foods and away from foods low in energy density may be contributing to excess adiposity and weight gain among children with ASD who also engage in these dietary patterns.
Sensory Integration Difficulties and Food Selectivity
In addition to dietary preferences that promote weight gain, children with ASD also experience sensory integration difficulties related to food (Cermak et al. 2010). Children with ASD may experience restricted preferences related to texture, taste, color, and shape (Kodak and Piazza 2008; Schreck and Williams 2006; Schreck et al. 2004), consistent with the restricted interests and repeated behaviors characteristic of the disorder. As such, preferences related to sameness and selectively around food may in turn impact food choices for children with ASD. Children with ASD show increased rates of food refusal compared to typically developing children (Bandini et al. 2008). Compared to age and sex-matched typically developing children, children with ASD engage in more food neophobia and food avoidance behaviors (Martins et al. 2008). Children with ASD may be more hesitant to try fruits and vegetables that have different shapes or textures, or their preference for sameness may limit the food choices parents present. Parents of children with ASD report a less varied diet than parents of children without ASDs, in that children with ASD only eat about half of the foods consumed by typically developing children across most food categories, with the exception of consuming about two thirds of the starches group (Schreck et al. 2004). Researchers hypothesize that the food selectivity demonstrated in children with ASD may be due to overresponsivity to the sensory components of foods, including textures, smells, and tastes that manifest in a largely unknown brain-gut connection (Cermack et al. 2010; Horvath and Perman 2002). These taste preferences may be influencing parent feeding behavior and child consumption in ways that contribute to excess weight gain.
Mealtime Behaviors
Various mealtime behaviors also present a unique challenge in ensuring adequate nutrition while limiting highly caloric foods for children with ASDs. Children with ASD that have difficulty staying seated during a meal (Nadon et al. 2011; Provost et al. 2010) or tend to eat rapidly (Anglesea et al. 2008) may be at an increased risk for overeating. Parent-reported rapid eating is associated with higher BMI percentile scores among children with ASD and other feeding disorders (Seiverling et al. 2011). If hunger and satiety cues are impaired, children may report feeling hungry all the time, which may behaviorally manifest through constantly asking others for food. Over time, if individuals consistently respond to these requests by providing food, a child’s overall level of food consumption would then increase, which could contribute to excess weight gain. Interventions that focus on providing support to parents and caretakers, while teaching about behavioral principles such as extinction bursts, may help manage these behaviors and lead to healthier eating and food choices.
Maintaining Factors of Overweight and Obesity in Children with ASD
Given that high rates of overweight and obesity among individuals with ASD persist from childhood to adulthood (Croen et al. 2015), it is also imperative to better understand what factors might be maintaining overweight and obesity in this population. Several facets related to both the disorder and treatment may provide clues as to important mechanisms to consider in the maintenance of excess weight for these individuals. The reinforcing value of food, and its use within treatment frameworks, may play a critical role. Additionally, a host of both interpersonal and intra-personal factors may account for the persistence in weight gain not only within childhood but also across the life span.
Reinforcing Value of Food
Food is inherently reinforcing, and is needed to sustain everyday activities of daily living. Yet, food is often viewed apart from this simplistic nutritional requirement. As food takes on learned and conditioned meanings, the relationship between eating and survival can become more distant, influencing eating behaviors that occur outside of times in which the individual is responding to a biological need. Once this relationship with food begins to change, the propensity to overeat and thus gain excess weight can more readily occur. For instance, food is a common reinforcer used in behavioral management and training. In particular, providers tend to use food often high in caloric content to influence behavior change (Center for Autism Research 2014). Thus, food becomes a therapeutic tool, and is associated with times outside of those driven by the physiological need for food. Parents are often taught to mimic the skills demonstrated by the therapeutic providers. It is not uncommon for parents of children with developmental disabilities to reward children with calorically dense foods for achieving behavioral targets (Simpson et al. 2006). Although older research suggests that sensory reinforcers produce more correct responses than edible ones (Rincover and Newson 1985), the heavy reliance on using food as a motivator in therapeutic treatments continues to persist (ABA Therapists 2003; Kelly 2008). Using highly palatable, calorically dense foods as a reinforcer to influence behavior change could have serious long-term health consequences, particularly among children that are already at risk for obesity and weight gain. Instead, therapists and parents alike should strive to find non-food reinforcers for children with ASD. Reliance on other behavioral reinforcement systems, such as token economies (Matson and Boisjoli 2009), that do not utilize food as a reinforcer or reward may help children achieve behavioral targets while limiting excess caloric intake.
Interpersonal Factors
Interpersonal factors also play a role in weight gain and obesity. For children with ASD, the social interaction difficulties and communication barriers that define the disorder may have important implications for food intake and could lead to overeating. In a society in which celebration and gatherings are often centered around food, children with ASD may have limited options and could engage in overeating behaviors if socializing and interacting with others are the only choices offered at such events. Parents, grandparents, and caregivers may also seek to communicate love and acceptance through food, as a means of relating to a child that often struggles in the interpersonal domain. Research has shown that family food preference predicts child food preference (Schreck and Williams 2006), and could be impacted by the modeling of eating behaviors or the foods that families choose to offer. Often seen as the “gate-keepers,” parents are often held responsible for the types and amounts of foods given to their child. While parents should not be blamed for their child’s weight status, parents should be viewed as the “agents of change” in influencing their child’s eating behaviors. Parents play such a crucial role that studies have found that parent-only behavioral weight loss treatments perform just as well as parent-child treatment, in terms of child weight outcomes (Boutelle et al. 2011). However, weight loss studies typically exclude children with ASD and other developmental disabilities, and thus, less is known about the role of parents in influencing weight loss for children with ASD.
Socially, children with ASD may have a difficult time connecting with loved ones and peers. These children may be less likely to join a community or recreational sports league or structured physical activity program, and thus, may have less opportunity to engage in physical activity. Motor deficits may present limitations to children participating in physical education classes or recess at school (Pan 2008). Children with ASD may prefer to not play with the neighbors or peers after school and on the weekends, and thus, may require additional intervention to engage in social and physically active outlets. While social interaction difficulties likely do not fully explain the lower observed physical activity levels among children with ASD (Pan 2008), it may contribute in important ways that perhaps are less of a barrier for children without ASD.
Hunger and Satiety Cues
Intra-individual differences in one’s ability to regulate hunger and satiety cues may also impact eating behaviors and weight gain. Several brain regions, including the insula and reward networks, are implicated in eating behavior and interoceptive awareness (Volkow et al. 2011). Research shows that the insula is hypoactive in individuals with autism (Uddin and Menon 2009). Thus, it is possible that hunger signals may be altered in children with ASD. Children with ASD may also have difficulty in identifying and labeling hunger states. Whereas children without ASD might experience difficulty in distinguishing internal hunger and satiety, children with ASD may not have the ability to communicate or express these bodily sensations. Perhaps children with ASD have more impulse control deficits (Hill 2004; Rajendran and Mitchell 2007), and these differences in regulatory control may make it harder for children to stop eating, particularly in situations in which high-calorie, highly rewarding food is readily available. Altered reward networks and brain functioning among children with ASD may also explain differences in eating behavior and weight gain. Neuroimaging studies suggest that, when hungry, children with ASD show increased responding to food cues in the insula and anterior cingulate cortex compared to children without ASD (Cascio et al. 2012). This finding suggests that these children may find food more rewarding, which could be one factor that contributes to overeating for children with ASD.
Potential Moderating Processes
Family History of Obesity
Several potential moderating processes may also be impacting weight and eating behavior for children with ASD. In particular, a family history of overweight and obesity is a risk factor for children regardless of autism status (Kral and Faith 2009). Children with one obese parent are twice as likely to be overweight, and children with two obese parents are 2.4 times more likely to be overweight, than children of normal weight parents (Manios et al. 2007). Parent overweight and obesity is an independent risk factor for childhood obesity (Agras et al. 2004), with both genetic and shared environmental risk factors at play. In children ages 6–13 years old, maternal BMI predicts child BMI z-scores (Gibson et al. 2007). Longitudinal studies show that obese children have a 50% chance of becoming an obese adult—compared to only a 10% chance for non-obese children—and that the risk of obesity in adulthood is higher if at least one parent is obese, more than doubling the risk for children under 10 years old (Whitaker et al. 1997).
Parent obesity is also associated with an increased prevalence of ASD. Studies indicate that prepregnancy obesity in mothers relates to a greater increased risk in having children with ASD (67% increase; Krakowiak et al. 2012), though this finding is not consistent across all studies (Brion et al. 2011; Suren et al. 2014). The population-based Norwegian Mother and Child Cohort Study reports that while maternal obesity was weakly associated with increased ASD risk, paternal obesity conveyed a stronger risk, with children of obese fathers having a 1.73 greater times likelihood of developing autistic disorder and a 2.01 greater odds for Asperger’s disorder (Suren et al. 2014). The authors suggest that pleiotropic gene variants, such as the 16p11.2 deletion mentioned earlier, may play a role in understanding the connection between obesity and ASD (Suren et al. 2014). These findings led the authors to conclude that paternal obesity should be considered an independent risk factor for ASDs in children (Suren et al. 2014). It is less well known whether parent weight status serves as a moderator of the relationship between child obesity and ASD, such that only children of overweight or obese parents are impacted, or if another overlapping mechanism may be accounting for this observed relationship. Given the link between parent weight status and child ASD diagnosis, it may also be possible that children with ASD are more likely to have an obese parent, and thus, more likely to be susceptible to genetic predispositions to gain weight and develop childhood obesity that persist into adolescence and adulthood.
Demographic Characteristics
It is also important to consider demographic characteristics that might be influencing the relationship between obesity and ASD, including age, ethnicity, sex, and autism severity. There appear to be differential relationships among obesity and ASD based on age. Among a clinical sample of children with autism, older children and adolescents (12–20 years) had higher odds of obesity compared to younger children (6–11 years; Broder-Fingert et al. 2014). Studies suggest that ethnicity is not a factor in moderating the observed relationship between obesity and ASD (Broder-Fingert et al. 2014). Autism severity and overall adaptive functioning also do not appear to be related to weight status in children with ASD (Egan et al. 2013). Given the limited research evidence examining these factors, studies should continue to assess and correlate demographic variables of interest with both ASD diagnosis and weight.
Interestingly, research studies find differences in sex ratios, with female children with ASD having reduced odds of obesity compared to male children with ASD (Broder-Fingert et al. 2014). Future research studies should continue to consider sex as a moderating factor in the relationship between obesity and autism, particularly given that no sex differences have been reported for obesity prevalence among children without ASD (Ogden et al. 2012). Despite largely equal prevalence rates, research shows an increase in obesity prevalence for males, but not females, from 1999 to 2010, with a significant increase in BMI for adolescent males ages 12–19 years old (Ogden et al. 2012). Given the strong sexual dimorphism associated with ASD diagnoses (four males to one female ratio), studies investigating the overlap between obesity and autism should continue to examine and account for potential sex differences as important explanatory moderators and covariates.
Weight-loss Treatment for Children with ASD
Despite the individual consequences and rising public health costs associated with pediatric obesity, very few studies target weight loss in children with ASD. Behavioral-based weight-loss treatments for obesity produce modest weight loss results in typically developing children (Epstein et al. 1994; Young et al. 2007) as well as adults (Butryn et al. 2011; Foster et al. 2005; Wadden et al. 2014). These behaviorally based weight-loss treatments focus on lifestyle modification through topics related to calorie reduction, self-monitoring, stimulus control, portion control, physical activity, and problem-solving skills (Boutelle et al. 2015a). It is currently unknown whether evidence-based treatments that work for typically developing children will also be acceptable, feasible, or effective for families with a child on the spectrum. Of note, no study has examined the feasibility and acceptability of the gold standard family-based behavioral treatment (FBT; Epstein et al. 2007) for weight loss within this population of children with ASD. A pilot project funded by the Healthy Weight Research Network for Children with Autism Spectrum Disorder and Developmental Disabilities is currently underway at the University of California, San Diego, to specifically adapt FBT to be suited for these families.
Parents may be more directly involved in weight loss efforts for children on the spectrum that require additional monitoring around food and eating behaviors. Parent-only treatments designed to promote weight loss in the target child may be especially useful to consider, given the physical and cognitive limitations of many children with ASD. Providing parents with psychoeducation about increased prevalence rates of overweight and obesity as well as strategies they can employ to limit excess weight gain for their children—such as switching to non-food reinforcers and promoting physical activity among children with ASD— will be crucial. Therapists and community service providers should also be educated on the effects of providing children with food as a reinforcer, and training should be offered to assist clinicians in using non-food reinforcers in their behavioral treatments instead.
However, it may be challenging for families to prioritize weight-loss treatment for a child that is already receiving specialized behavioral services for many other domains of functioning. Parent burnout and motivation will be important factors to consider when designing feasible and acceptable weight loss interventions for children with ASD. Empowering parents to promote weight change can be difficult, as behavioral weight loss strategies are time consuming and challenging to implement. Nevertheless, the health and psychosocial consequences associated with overweight and obesity have serious, negative outcomes that can last from childhood to adulthood, and even influence mortality rates. A greater understanding of the mediating and moderating processes related to the increased rates of overweight and obesity in children with ASD will provide invaluable targets for treatment and intervention. Researchers and clinicians alike should strive to develop effective prevention and intervention programs that uniquely account for the needs of families and children with ASD in order to promote weight change and healthier lifestyles.
Conclusions
This review investigating the factors related to the etiology, development, and maintenance of overweight and obesity in children and adolescents with ASD attempted to highlight this relationship and reveal the paucity of research that currently exists. Many factors seem to influence the relationship between weight and autism in children, including genetics, environmental components, parenting behaviors, and both inter- and intra-individual factors. It is also important to not simply think about these factors in isolation, but rather to consider the complex interactions that are likely occurring to impact weight status among these individuals.
The present study has several important limitations to consider. This study relies upon the research literature to determine the rates and potential contributors to obesity in ASD youth. However, many of the studies surveyed provide little or no information regarding important areas of interest, including the socioeconomic and ethno-racial minority status of families with children with ASD as well as an in-depth assessment of the effects of gender on study outcomes. The obesity literature consistently shows the relationship between socioeconomic status, ethno-racial minority status, and obesity (Ogden et al. 2010; Ogden et al. 2012; Wang and Lim 2012). Furthermore, the authors acknowledge that this study does not include an in-depth analysis of the relationship between cognitive functioning level and obesity in ASD youth. Ideally, this study would contain all of the necessary information to form a more nuanced analysis of obesity distribution across these relevant demographic factors. As the literature on ASD and obesity remains somewhat limited, this type of synthesis is not provided and remains a limitation of this study.
Clearly, future research is needed to better understand the cascading trajectory that weight gain in childhood might have on eating behaviors and weight status in later adolescence and adulthood. The information reviewed previously likely generates more questions than answers, which could be considered an adequate reflection of the field’s current state. Researchers should continue to investigate mediators and moderators that may impact weight gain in children with ASD in order to more accurately inform interventions designed specifically for this population.
References
ABA Therapists. (2003). Reinforcement and ABA therapy. Applied Behavior Analysis Training Guide. Retrieved May 10, 2016 from http://abatherapists.com/reinforcement-and-aba-therapy/.
Abdul-Rasoul, M. M. (2012). Obesity in children and adolescents in Gulf countries: facts and solutions. Avances en Diabetologia, 28(3), 64–69.
Agras, W. S., Hammer, L. D., McNicholas, F., & Kraemer, H. C. (2004). Risk factors for childhood overweight: a prospective study from birth to 9.5 years. The Journal of Pediatrics, 145(1), 20–25.
Alasfoor, D., & Mohammed, A. J. (2009). Implications of the use of the new WHO growth charts on the interpretation of malnutrition and obesity in infants and young children in Oman. Eastern Mediterranean Health Journal, 15(4), 890–898.
Al-Farsi, Y. M., Al-Sharbati, M. M., Waly, M. I., Al-Farsi, O. A., Al Shafaee, M. A., & Deth, R. C. (2011). Malnutrition among preschool-aged autistic children in Oman. Research in Autism Spectrum Disorders, 5(4), 1549–1552.
Almandil, N. B., Liu, Y., Murray, M. L., Besag, F. M., Aitchison, K. J., & Wong, I. C. (2013). Weight gain and other metabolic adverse effects associated with atypical antipsychotic treatment of children and adolescents: a systematic review and meta-analysis. Pediatric Drugs, 15(2), 139–150.
American Academy of Pediatrics. (2001). Clinical practice guideline: treatment of the school- aged child with attention-deficit/hyperactivity disorder. Pediatrics, 108(4), 1033–1044.
Anglesea, M. M., Hoch, H., & Taylor, B. A. (2008). Reducing rapid eating in teenagers with autism: use of a pager prompt. Journal of Applied Behavior Analysis, 41(1), 107–111.
Attlee, A., Kassem, H., Hashim, M., & Obaid, R. S. (2015). Physical status and feeding behavior of children with autism. The Indian Journal of Pediatrics, 82(8), 682–687.
Bak, M., Fransen, A., Janssen, J., van Os, J., & Drukker, M. (2014). Almost all antipsychotics result in weight gain: a meta-analysis. PloS One, 9(4), e94112.
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., Scampini, R., et al. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157(2), 259–264.
Barnhill, K., Gutierrez, A., Ghossainy, M., Marediya, Z., Marti, C. N., & Hewitson, L. (2017). Growth status of children with autism spectrum disorder: a case–control study. Journal of Human Nutrition and Dietetics, 30(1), 59–65.
Bicer, A. H., & Alsaffar, A. A. (2013). Body mass index, dietary intake and feeding problems of Turkish children with autism spectrum disorder (ASD). Research in Developmental Disabilities, 34(11), 3978–3987.
Bochukova, E. G., Huang, N. I., Keogh, J., Henning, E., Purmann, C., Blaszczyk, K., Saeed, S., Hamilton-Shield, J., Clayton-Smith, J., O’Rahilly, S., & Hurles, M. E. (2010). Large, rare chromosomal deletions associated with severe early-onset obesity. Nature, 463(7281), 666–670.
Boutelle, K. N., Hannan, P., Fulkerson, J. A., Crow, S. J., & Stice, E. (2010). Obesity as a prospective predictor of depression in adolescent females. Health Psychology, 29(3), 293–298.
Boutelle, K. N., Cafri, G., & Crow, S. J. (2011). Parent-only treatment for childhood obesity: a randomized controlled trial. Obesity, 19(3), 574–580.
Boutelle, K. N., Braden, A., Douglas, J. M., Rhee, K. E., Strong, D., Rock, C. L., Wilfley, D. E., Epstein, L., & Crow, S. J. (2015a). Design of the FRESH study: a randomized controlled trial of a parent-only and parent–child family-based treatment for childhood obesity. Contemporary Clinical Trials, 45, 364–370.
Boutelle, K. N., Liang, J., Knatz, S., Matheson, B., Risbrough, V., Strong, D., Rhee, K. E., Craske, M. G., Zucker, N., & Bouton, M. E. (2015b). Design and implementation of a study evaluating extinction processes to food cues in obese children: the Intervention for Regulations of Cues Trial (iROC). Contemporary Clinical Trials, 40, 95–104.
Brion, M. J., Zeegers, M., Jaddoe, V., Verhulst, F., Tiemeier, H., Lawlor, D. A., & Smith, G. D. (2011). Maternal pre-pregnancy overweight and child cognition and behavior: exploring intrauterine effects in two pregnancy cohorts. Pediatrics, 127(1), e202.
Broder-Fingert, S., Brazauskas, K., Lindgren, K., Iannuzzi, D., & Van Cleave, J. (2014). Prevalence of overweight and obesity in a large clinical sample of children with autism. Academic Pediatrics, 14(4), 408–414.
Butryn, M. L., Webb, V., & Wadden, T. A. (2011). Behavioral treatment of obesity. The Psychiatric Clinics of North America, 34(4), 841–859.
Calarge, C. A., Acion, L., Kuperman, S., Tansey, M., & Schlechte, J. A. (2009). Weight gain and metabolic abnormalities during extended risperidone treatment in children and adolescents. Journal of Child and Adolescent Psychopharmacology, 19(2), 101–109.
Cascio, C. J., Foss-Feig, J. H., Heacock, J. L., Newsom, C. R., Cowan, R. L., Benningfield, M. M., Rogers, B. P., & Cao, A. (2012). Response of neural reward regions to food cues in autism spectrum disorders. Journal of Neurodevelopmental Disorders, 4(1), 9–19.
Center for Autism Research. (2014). Applied behavioral analysis (ABA). CAR Autism Roadmap. Retrieved June 26, 2016 from https://www.carautismroadmap.org/applied- behavior-analysis-aba/.
Cermak, S. A., Curtin, C., & Bandini, L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110(2), 238–246.
Charach, A., Ickowicz, A., & Schachar, R. (2004). Stimulant treatment over five years: adherence, effectiveness, and adverse effects. Journal of the American Academy of Child & Adolescent Psychiatry, 43(5), 559–567.
Chen, A. Y., Kim, S. E., Houtrow, A. J., & Newacheck, P. W. (2010). Prevalence of obesity among children with chronic conditions. Obesity, 18(1), 210–213.
Cormier, E. (2008). Attention deficit/hyperactivity disorder: a review and update. Journal of Pediatric Nursing, 23(5), 345–357.
Corvey, K., Menear, K. S., Preskitt, J., Goldfarb, S., & Menachemi, N. (2016). Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Maternal and Child Health Journal, 20(2), 466–476.
Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823.
Curtin, C., Bandini, L. G., Perrin, E. C., Tybor, D. J., & Must, A. (2005). Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: a chart review. BioMed Central Pediatrics, 5(1), 48–54.
Curtin, C., Anderson, S. E., Must, A., & Bandini, L. (2010). The prevalence of obesity in children with autism: a secondary data analysis using nationally representative data from the National Survey of Children’s Health. BioMed Central Pediatrics, 10(1), 11–15.
Demb, H., Valicenti-McDermott, M., Navarro, A., & Ayoob, K. E. (2011). The effect of long-term use of risperidone on body weight of children with an autism spectrum disorder. Journal of Clinical Psychopharmacology, 31, 669–670.
DMNSY Developmental. (2014). Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report. Surveillance summaries (Washington, DC: 2002), 63(2), 1.
Egan, A. M., Dreyer, M. L., Odar, C. C., Beckwith, M., & Garrison, C. B. (2013). Obesity in young children with autism spectrum disorders: prevalence and associated factors. Childhood Obesity, 9(2), 125–131.
Epstein, L. H., Valoski, A., Wing, R. R., & McCurley, J. (1994). Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychology, 13(5), 373–383.
Epstein, L. H., Paluch, R. A., Roemmich, J. N., & Beecher, M. D. (2007). Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychology, 26(4), 381–391.
Evans, E. W., Must, A., Anderson, S. E., Curtin, C., Scampini, R., Maslin, M., & Bandini, L. (2012). Dietary patterns and body mass index in children with autism and typically developing children. Research in Autism Spectrum Disorders, 6(1), 399–405.
Faith, M. S., Scanlon, K. S., Birch, L. L., Francis, L. A., & Sherry, B. (2004). Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Research, 12(11), 1711–1722.
Fallon, E. M., Tanofsky-Kraff, M., Norman, A. C., McDuffie, J. R., Taylor, E. D., Cohen, M. L., Young-Hyman, D., Keil, M., Kolotkin, R. L., & Yanovski, J. A. (2005). Health-related quality of life in overweight and nonoverweight black and white adolescents. The Journal of Pediatrics, 147(4), 443–450.
Farooqi, I. S. (2005). Genetic and hereditary aspects of childhood obesity. Best Practice & Research Clinical Endocrinology & Metabolism, 19(3), 359–374.
Ferguson, J. M. (2001). SSRI antidepressant medications: adverse effects and tolerability. Primary Care Companion Journal Clinical Psychiatry, 3(1), 22–27.
Fischbach, G. D., & Lord, C. (2010). The Simons Simplex Collection: a resource for identification of autism genetic risk factors. Neuron, 68(2), 192–195.
Fischbach, B. V., Trout, K. L., Lewis, J., Luis, C. A., & Sika, M. (2005). WAGR syndrome: a clinical review of 54 cases. Pediatrics, 116(4), 984–988.
Foster, G. D., Makris, A. P., & Bailer, B. A. (2005). Behavioral treatment of obesity. The American Journal of Clinical Nutrition, 82(1), 230S–235S.
Fournier, K. A., Hass, C. J., Naik, S. K., Lodha, N., & Cauraugh, J. H. (2010). Motor coordination in autism spectrum disorders: a synthesis and meta-analysis. Journal of Autism and Developmental Disorders, 40(10), 1227–1240.
Freedman, D. S., Mei, Z., Srinivasan, S. R., Berenson, G. S., & Dietz, W. H. (2007). Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. The Journal of Pediatrics, 150(1), 12–17.
Gaugler, T., Klei, L., Sanders, S. J., Bodea, C. A., Goldberg, A. P., Lee, A. B., & Ripke, S. (2014). Most genetic risk for autism resides with common variation. Nature Genetics, 46(8), 881–885.
Gibson, L. Y., Byrne, S. M., Davis, E. A., & Blair, E. (2007). The role of family and maternal factors in childhood obesity. Medical Journal of Australia, 186(11), 591–595.
Gillette, M. L. D., Borner, K. B., Nadler, C. B., Poppert, K. M., Stough, C. O., Romine, R. S., & Davis, A. M. (2015). Prevalence and health correlates of overweight and obesity in children with autism spectrum disorder. Journal of Developmental & Behavioral Pediatrics, 36(7), 489–496.
Glasofer, D. R., Tanofsky-Kraff, M., Eddy, K. T., Yanovski, S. Z., Theim, K. R., Mirch, M. C., Ghorbani, S., & Yanovski, J. A. (2007). Binge eating in overweight treatment-seeking adolescents. Journal of Pediatric Psychology, 32(1), 95–105.
Granich, J., Lin, A., Hunt, A., Wray, J., Dass, A., & Whitehouse, A. J. (2016). Obesity and associated factors in youth with an autism spectrum disorder. Autism, 20(8), 916–926.
Green, D., Charman, T., Pickles, A., Chandler, S., Loucas, T., Simonoff, E., & Baird, G. (2009). Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine & Child Neurology, 51(4), 311–316.
Hallmayer, J., Cleveland, S., Torres, A., Phillips, J., Cohen, B., Torigoe, T., & Lotspeich, L. (2011). Genetic heritability and shared environmental factors among twin pairs with autism. Archives of General Psychiatry, 68(11), 1095–1102.
Hannon, T. S., Rao, G., & Arslanian, S. A. (2005). Childhood obesity and type 2 diabetes mellitus. Pediatrics, 116(2), 473–480.
Haworth, C., Plomin, R., Carnell, S., & Wardle, J. (2008). Childhood obesity: genetic and environmental overlap with normal-range BMI. Obesity, 16(7), 1585–1590.
Hellings, J. A., Zarcone, J. R., Crandall, K., Wallace, D., & Schroeder, S. R. (2001). Weight gain in a controlled study of risperidone in children, adolescents and adults with mental retardation and autism. Journal of Child and Adolescent Psychopharmacology, 11(3), 229–238.
Hill, E. L. (2004). Evaluating the theory of executive dysfunction in autism. Developmental Review, 24(2), 189–233.
Hill, A. P., Zuckerman, K. E., & Fombonne, E. (2015). Obesity and autism. Pediatrics, 136(6), 1051–1061.
Ho, H. H., Eaves, L. C., & Peabody, D. (1997). Nutrient intake and obesity in children with autism. Focus on Autism and Other Developmental Disabilities, 12(3), 187–192.
Hollander, E., Phillips, A., Chaplin, W., Zagursky, K., Novotny, S., Wasserman, S., & Iyengar, R. (2005). A placebo controlled crossover trial of liquid fluoxetine on repetitive behaviors in childhood and adolescent autism. Neuropsychopharmacology, 30(3), 582–589.
Horvath, K., & Perman, J. A. (2002). Autism and gastrointestinal symptoms. Current Gastroenterology Reports, 4(3), 251–258.
Hyman, S. L., Stewart, P. A., Schmidt, B., Lemcke, N., Foley, J. T., Peck, R., & James, S. J. (2012). Nutrient intake from food in children with autism. Pediatrics, 130(Supplement 2), S145–S153.
Jansen, A. (1998). A learning model of binge eating: cue reactivity and cue exposure. Behaviour Research and Therapy, 36(3), 257–272.
Janssen Pharmaceuticals. (2014). Risperdal® (risperidone). Retrieved May 8, 2016 from http://www.janssen.com/us/sites/www_janssen_com_usa/files/products-documents/risperdal.pdf
Jerrell, J. M. (2010). Neuroendocrine-related adverse events associated with antidepressant treatment in children and adolescents. CNS Neuroscience & Therapeutics, 16(2), 83–90.
Kelly, A.N. (2008). Common misconceptions about applied behavior analysis. Behaviorbabe. Retrieved May 10, 2016 from http://www.behaviorbabe.com/commonmisconceptions.htm.
Kirk, S. F., Penney, T. L., & McHugh, T. L. (2010). Characterizing the obesogenic environment: the state of the evidence with directions for future research. Obesity Reviews, 11(2), 109–117.
Kodak, T., & Piazza, C. C. (2008). Assessment and behavioral treatment of feeding and sleeping disorders in children with autism spectrum disorders. Child and Adolescent Psychiatric Clinics of North America, 17(4), 887-905.
Krakowiak, P., Walker, C. K., Bremer, A. A., Baker, A. S., Ozonoff, S., Hansen, R. L., & Hertz-Picciotto, I. (2012). Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics, 129(5), e1121–e1128.
Kral, T. V., & Faith, M. S. (2009). Influences on child eating and weight development from a behavioral genetics perspective. Journal of Pediatric Psychology, 34(6), 596–605.
Kral, T. V., Souders, M. C., Tompkins, V. H., Remiker, A. M., Eriksen, W. T., & Pinto-Martin, J. A. (2015). Child eating behaviors and caregiver feeding practices in children with autism spectrum disorders. Public Health Nursing, 32(5), 488–497.
Kummer, A., Barbosa, I. G., Rodrigues, D. H., Rocha, N. P., da Silva Rafael, M., Pfeilsticker, L., et al. (2016). Frequency of overweight and obesity in children and adolescents with autism and attention deficit/hyperactivity disorder. Revista Paulista de Pediatria (English Edition), 34(1), 71–77.
Lawson, L. M., & Foster, L. (2016). Sensory patterns, obesity, and physical activity participation of children with autism spectrum disorder. American Journal of Occupational Therapy, 70(5), 1–8.
Liang, J., Matheson, B. E., Kaye, W. H., & Boutelle, K. N. (2014). Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. International Journal of Obesity, 38(4), 494–506.
MacDonald, M., Esposito, P., & Ulrich, D. (2011). The physical activity patterns of children with autism. BioMed Central Research Notes, 4(1), 422–426.
Malik, V. S., Pan, A., Willett, W. C., & Hu, F. B. (2013). Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. The American Journal of Clinical Nutrition, 98(4), 1084–1102.
Manios, Y., Costarelli, V., Kolotourou, M., Kondakis, K., Tzavara, C., & Moschonis, G. (2007). Prevalence of obesity in preschool Greek children, in relation to parental characteristics and region of residence. BioMed Central Public Health, 7(1), 178–185.
Martins, Y., Young, R. L., & Robson, D. C. (2008). Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism and Developmental Disorders, 38(10), 1878–1887.
Matheson, B. E., Camacho, C., Peterson, C. B., Rhee, K. E., Rydell, S. A., Zucker, N. L., & Boutelle, K. N. (2015). The relationship between parent feeding styles and general parenting with loss of control eating in treatment-seeking overweight and obese children. International Journal of Eating Disorders, 48(7), 1047–1055.
Matson, J. L., & Boisjoli, J. A. (2009). The token economy for children with intellectual disability and/or autism: A review. Research in Developmental Disabilities, 30(2), 240–248.
Mazurek, M. O., Shattuck, P. T., Wagner, M., & Cooper, B. P. (2012). Prevalence and correlates of screen-based media use among youths with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(8), 1757–1767.
McCoy, S. M., Jakicic, J. M., & Gibbs, B. B. (2016). Comparison of obesity, physical activity, and sedentary behaviors between adolescents with autism spectrum disorders and without. Journal of Autism and Developmental Disorders, 46(7), 2317–2326.
McCracken, J. T., McGough, J., Shah, B., Cronin, P., Hong, D., Aman, M. G., Arnold, L. E., Lindsay, R., Nash, P., Hollway, J., & McDougle, C. J. (2002). Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine, 347(5), 314–321.
McDougle, C. J., Holmes, J. P., Carlson, D. C., Pelton, G. H., Cohen, D. J., & Price, L. H. (1998). A double-blind, placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Archives of General Psychiatry, 55(7), 633–641.
McDougle, C. J., Kresch, L. E., & Posey, D. J. (2000). Repetitive thoughts and behavior in pervasive developmental disorders: Treatment with serotonin reuptake inhibitors. Journal of Autism and Developmental Disorders, 30(5), 427–435.
McDougle, C. J., Scahill, L., Aman, M. G., McCracken, J. T., Tierney, E., Davies, M., Arnold, L. E., & Shah, B. (2005). Risperidone for the core symptom domains of autism: results from the study by the autism network of the research units on pediatric psychopharmacology. American Journal of Psychiatry, 162(6), 1142–1148.
Memari, A. H., Kordi, R., Ziaee, V., Mirfazeli, F. S., & Setoodeh, M. S. (2012). Weight status in Iranian children with autism spectrum disorders: Investigation of underweight, overweight and obesity. Research in Autism Spectrum Disorders, 6(1), 234–239.
Musaiger, A. O. (2011). Overweight and obesity in eastern mediterranean region: prevalence and possible causes. Journal of Obesity, 2011, 1–17.
Must, A., Phillips, S. M., Curtin, C., Anderson, S. E., Maslin, M., Lividini, K., & Bandini, L. G. (2014). Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism, 18(4), 376–384.
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011). Mealtime problems in children with autism spectrum disorder and their typically developing siblings: a comparison study. Autism, 15(1), 98–113.
Obrusnikova, I., & Cavalier, A. R. (2011). Perceived barriers and facilitators of participation in after-school physical activity by children with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 23(3), 195–211.
Ogden, C. L., Lamb, M. M., Carroll, M. D., & Flegal, K. M. (2010). Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS Data Brief, Number 51. Hyattsville, MD: National Center for Health Statistics.
Ogden, C. L., Carroll, M. D., Kit, B. K., & Flegal, K. M. (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. The Journal of the American Medical Association, 307(5), 483–490.
Ogden, C. L., Carroll, M. D., Kit, B. K., & Flegal, K. M. (2014). Prevalence of childhood and adult obesity in the United States, 2011–2012. The Journal of the American Medical Association, 311(8), 806–814.
Pan, C. Y. (2008). Objectively measured physical activity between children with autism spectrum disorders and children without disabilities during inclusive recess settings in Taiwan. Journal of Autism and Developmental Disorders, 38, 1292–1301.
Phillips, K. L., Schieve, L. A., Visser, S., Boulet, S., Sharma, A. J., Kogan, M. D., & Yeargin-Allsopp, M. (2014). Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Maternal and Child Health Journal, 18(8), 1964–1975.
Polfuss, M., Johnson, N., Bonis, S. A., Hovis, S. L., Apollon, F., & Sawin, K. J. (2016). Autism spectrum disorder and the child’s weight-related behaviors: a parent’ perspective. Journal of Pediatric Nursing, 31(6), 598–607.
Polivy, J., Herman, C. P., & Coelho, J. S. (2008). Caloric restriction in the presence of attractive food cues: external cues, eating, and weight. Physiology & Behavior, 94(5), 729–733.
Pringle B. A., Colpe L. J., Blumberg S. J., Avila R. M., & Kogan M. D. (2012). Diagnostic history and treatment of school-aged children with autism spectrum disorder and special health care needs. NCHS Data Brief, Number 97. Hyattsville, MD: National Center for Health Statistics.
Provost, B., Crowe, T. K., Osbourn, P. L., McClain, C., & Skipper, B. J. (2010). Mealtime behaviors of preschool children: comparison of children with autism spectrum disorder and children with typical development. Physical & Occupational Therapy in Pediatrics, 30(3), 220–233.
Rajendran, G., & Mitchell, P. (2007). Cognitive theories of autism. Developmental Review, 27(2), 224–260.
Reekie, J., Hosking, S. P. M., Prakash, C., Kao, K. T., Juonala, M., & Sabin, M. A. (2015). The effect of antidepressants and antipsychotics on weight gain in children and adolescents. Obesity Reviews, 16(7), 566–580.
Reilly, J. J., & Kelly, J. (2011). Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. International Journal of Obesity, 35(7), 891–898.
Reilly, J. J., Methven, E., McDowell, Z. C., Hacking, B., Alexander, D., Stewart, L., & Kelnar, C. J. (2003). Health consequences of obesity. Archives of Disease in Childhood, 88(9), 748–752.
Research Units on Pediatric Psychopharmacology Autism Network. (2005). Risperidone treatment of autistic disorder: longer-term benefits and blinded discontinuation after 6 months. American Journal of Psychiatry, 162, 1361–1369.
Rimmer, J. H., Yamaki, K., Lowry, B. M., Wang, E., & Vogel, L. C. (2010). Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities. Journal of Intellectual Disability Research, 54(9), 787–794.
Rincover, A., & Newsom, C. D. (1985). The relative motivational properties of sensory and edible reinforcers in teaching autistic children. Journal of Applied Behavior Analysis, 18(3), 237–248.
Safer, D. J., & Zito, J. M. (2006). Treatment-emergent adverse events from selective serotonin reuptake inhibitors by age group: children versus adolescents. Journal of Child & Adolescent Psychopharmacology, 16(1–2), 159–169.
Schreck, K. A., & Williams, K. (2006). Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Research in Developmental Disabilities, 27(4), 353–363.
Schreck, K. A., Williams, K., & Smith, A. F. (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34(4), 433–438.
Schwimmer, J. B., Burwinkle, T. M., & Varni, J. W. (2003). Health-related quality of life of severely obese children and adolescents. The Journal of the American Medical Association, 289(14), 1813–1819.
Schwimmer, J. B., Deutsch, R., Kahen, T., Lavine, J. E., Stanley, C., & Behling, C. (2006). Prevalence of fatty liver in children and adolescents. Pediatrics, 118(4), 1388–1393.
Seiverling, L., Hendy, H. M., & Williams, K. (2011). The screening tool of feeding problems applied to children (STEP-CHILD): psychometric characteristics and associations with child and parent variables. Research in Developmental Disabilities, 32(3), 1122–1129.
Sharma, J. R., Arieff, Z., Sagar, S., & Kaur, M. (2012). Autism and obesity: prevalence, molecular basis and potential therapies. Autism Insights, 4, 1–13.
Sharp, W. G., Jaquess, D. L., & Lukens, C. T. (2013). Multi-method assessment of feeding problems among children with autism spectrum disorders. Research in Autism Spectrum Disorders, 7(1), 56–65.
Shedlock, K., Susi, A., Gorman, G. H., Hisle-Gorman, E., Erdie-Lalena, C. R., & Nylund, C. M. (2016). Autism spectrum disorders and metabolic complications of obesity. The Journal of Pediatrics, 178, 183–187.
Shinawi, M., Sahoo, T., Maranda, B., Skinner, S. A., Skinner, C., Chinault, C., et al. (2011). 11p14. 1 microdeletions associated with ADHD, autism, developmental delay, and obesity. American Journal of Medical Genetics Part A, 155(6), 1272–1280.
Shmaya, Y., Eilat-Adar, S., Leitner, Y., Reif, S., & Gabis, L. (2015). Nutritional deficiencies and overweight prevalence among children with autism spectrum disorder. Research in Developmental Disabilities, 38, 1–6.
Silventoinen, K., Rokholm, B., Kaprio, J., & Sørensen, T. I. A. (2010). The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. International Journal of Obesity, 34(1), 29–40.
Simpson, C. G., Swicegood, P. R., & Gaus, M. D. (2006). Nutrition and fitness curriculum: designing instructional interventions for children with developmental disabilities. Teaching Exceptional Children, 38(6), 50–53.
Surén, P., Gunnes, N., Roth, C., Bresnahan, M., Hornig, M., Hirtz, D., & Schjølberg, S. (2014). Parental obesity and risk of autism spectrum disorder. Pediatrics, 133, 1–11.
Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: The development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29(6), 563–570.
Tanofsky-Kraff, M., Yanovski, S. Z., Wilfley, D. E., Marmarosh, C., Morgan, C. M., & Yanovski, J. A. (2004). Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology, 72(1), 53–61.
Tschoner, A., Engl, J., Laimer, M., Kaser, S., Rettenbacher, M., Fleischhacker, W. W., & Ebenbichler, C. F. (2007). Metabolic side effects of antipsychotic medication. International Journal of Clinical Practice, 61(8), 1356–1370.
Uddin, L. Q., & Menon, V. (2009). The anterior insula in autism: under-connected and under-examined. Neuroscience & Biobehavioral Reviews, 33(8), 1198–1203.
de Vinck-Baroody, O., Shui, A., Macklin, E. A., Hyman, S. L., Leventhal, J. M., & Weitzman, C. (2015). Overweight and obesity in a sample of children with autism spectrum disorder. Academic Pediatrics, 15(4), 396–404.
Volkow, N. D., Wang, G. J., & Baler, R. D. (2011). Reward, dopamine and the control of food intake: implications for obesity. Trends in Cognitive Sciences, 15(1), 37–46.
Wadden, T. A., Butryn, M. L., Hong, P. S., & Tsai, A. G. (2014). Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. The Journal of the American Medical Association, 312(17), 1779–1791.
Walters, R. G., Jacquemont, S., Valsesia, A., De Smith, A. J., Martinet, D., Andersson, J., Falchi, M., Chen, F., Andrieux, J., Lobbens, S., & Delobel, B. (2010). A new highly penetrant form of obesity due to deletions on chromosome 16p11. 2. Nature, 463(7281), 671–675.
Wang, Y., & Lim, H. (2012). The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. International Review of Psychiatry, 24(3), 176–188.
Wardle, J., Carnell, S., Haworth, C. M., & Plomin, R. (2008). Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. The American Journal of Clinical Nutrition, 87(2), 398–404.
West, L., Brunssen, S. H., & Waldrop, J. (2009). Review of the evidence for treatment of children with autism with selective serotonin reuptake inhibitors. Journal for Specialists in Pediatric Nursing, 14(3), 183–191.
Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D., & Dietz, W. H. (1997). Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine, 337(13), 869–873.
Xia, W., Zhou, Y., Sun, C., Wang, J., & Wu, L. (2010). A preliminary study on nutritional status and intake in Chinese children with autism. European Journal of Pediatrics, 169(10), 1201–1206.
Xiong, N., Ji, C., Li, Y., He, Z., Bo, H., & Zhao, Y. (2009). The physical status of children with autism in China. Research in Developmental Disabilities, 30(1), 70–76.
Xu, S., Han, J. C., Morales, A., Menzie, C. M., Williams, K., & Fan, Y. S. (2008). Characterization of 11p14-p12 deletion in WAGR syndrome by array CGH for identifying genes contributing to mental retardation and autism. Cytogenetic and Genome Research, 122(2), 181–187.
Yoon, Y., Wink, L. K., Pedapati, E. V., Horn, P. S., & Erickson, C. A. (2016). Weight gain effects of second-generation antipsychotic treatment in autism spectrum disorder. Journal of Child and Adolescent Psychopharmacology, 26(9), 822–827.
Young, K. M., Northern, J. J., Lister, K. M., Drummond, J. A., & O’Brien, W. H. (2007). A meta-analysis of family-behavioral weight-loss treatments for children. Clinical Psychology Review, 27(2), 240–249.
Zachor, D. A., Roberts, A. W., Hodgens, J. B., Isaacs, J. S., & Merrick, J. (2006). Effects of long-term psychostimulant medication on growth of children with ADHD. Research in Developmental Disabilities, 27(2), 162–174.
Zuckerman, K. E., Hill, A. P., Guion, K., Voltolina, L., & Fombonne, E. (2014). Overweight and obesity: Prevalence and correlates in a large clinical sample of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(7), 1708–1719.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors have no funding sources to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Matheson, B.E., Douglas, J.M. Overweight and Obesity in Children with Autism Spectrum Disorder (ASD): a Critical Review Investigating the Etiology, Development, and Maintenance of this Relationship. Rev J Autism Dev Disord 4, 142–156 (2017). https://doi.org/10.1007/s40489-017-0103-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40489-017-0103-7