Abstract
Previous literature suggests children with autism spectrum disorder (ASD) have a higher prevalence of excess weight than typically developing (TD) children, but information addressing risk factor concordance between those with ASD and TD children is lacking. We used a retrospective analysis of children (N = 2610) who visited an Autism Speaks Autism Treatment Network (AS-ATN) center in the United States or Canada. This analysis occurred concurrently with two other research teams within AS-ATN. We found substantial agreement between predictors of weight in children with ASD and known correlates of obesity in typical children. These included Asian and Hispanic ethnicities, four medication groups, and psychopathological comorbidities such as aggression, anxiety, depression, and ADHD symptoms. The similarities of risk factors for weight between TD and ASD children will allow for use of existing protocols for weight interventions with minimal modification, saving resources otherwise spent pursuing new risk factors or treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Overweight (body mass index [BMI] or weight in kilograms divided by height in meters squared >85th percentile) and obesity (BMI > 95th percentile) are considered nutritional disorders (Ito 2006). They contribute to chronic health conditions that have medical and psychological implications, including greater risk for diabetes mellitus, metabolic syndrome, cardiovascular problems, depression, low self-esteem, and cancer (Deckelbaum and Williams 2001; Lobstein et al. 2004). This makes childhood overweight and obesity potentially serious issues that can have significant effects on quality of life, morbidity, and mortality (e.g., Daniels 2006; Deckelbaum and Williams 2001; Freedman et al. 2001). In this manuscript, references to excessive weight (e.g., overweight, obesity) are derived from BMI percentiles that fall into the overweight or obese ranges, unless indicated otherwise.
Youth with intellectual and developmental disabilities (IDD) have been affected by the increase in weight status. Some research suggests that children with IDD are impacted to a greater extent than what is experienced by those who are typically developing (TD; Allison et al. 1998). Differences between youth with IDD and those who are TD may be due to disability-specific risk factors (e.g., increased medication use, syndrome specific symptoms) and by increased behavioral, cognitive, or social difficulties (Chen et al. 2010; Grondhuis and Aman 2013).
Literature on the prevalence of obesity in children and adolescents with autism spectrum disorder (ASD) is available from multiple sources. Curtin et al. (2010) reported that 30.4 % of their sample with autism were obese compared to 23.6 % of children without autism, although the finding was not statistically significant. De Vinck-Baroody et al. (2015) made a compelling contrast to a national comparison sample demonstrating that children with ASD were more likely to be obese than the general population. Hill et al. (2015) used similar analyses and found that only young children (ages 2–5 years) with ASD had greater prevalence of overweight and obesity when compared to the same general population comparison sample used by de Vinck-Baroody et al. (2015).
Many other studies (e.g., Curtin et al. 2005; Memari et al. 2012; Phillips et al. 2014; Sharp et al. 2014; Xiong et al. 2009) have also found that overweight and obesity are common problems for children with ASD, although sometimes with limited information about risk factors and correlates that may cause altered weight. More information appears to be needed about whether correlates of obesity in children with ASD are similar to those commonly found in TD children.
Substantial effort has been dedicated to combatting the rise of childhood overweight and obesity all over the globe. This “epidemic” has been recognized as one of the biggest health concerns that humans currently face (World Health Organization 2000). Since experts the world over are working to identify risk factors for childhood obesity for children in general, we should follow suit with children having ASD. Understanding what correlates are the same for children with ASD and identifying points of divergence will allow researchers to customize existing treatment protocols and establish areas where new directions should be pursued.
Children with ASD could be influenced by known risk factors for overweight in TD children in many ways. For example, youngsters with ASD are often impacted with co-occurring psychopathology (Simonoff et al. 2008), such as anxiety disorders, attention deficit hyperactivity disorder (ADHD), and mood disorders, and each disorder may affect rates of obesity and overweight. Many children with ASD are medicated to address behavioral or emotional problems or to treat comorbid medical issues (Grondhuis and Aman 2013). Medications are often accompanied by drug-specific side-effect profiles; they can diminish or increase appetite, alter metabolic functioning, or change food preferences (Bernstein 1987).
Disordered sleep occurs at a greater rate in children with ASD than in TD children (Hollway and Aman 2011), and overweight adolescents tend to have more disrupted sleep associated with wakefulness multiple times throughout the night and shorter sleep duration (Beebe et al. 2007). Overweight children were also at higher risk for sleep-disordered breathing, such as apnea (Beebe et al. 2007; Flint et al. 2007).
Socioeconomic status (SES) has been identified as a major contributor to obesity. Children from families in lower income brackets or with less education tend to be more overweight. Lower income families typically purchase lower quality foods that are relatively inexpensive (but highly caloric), have fewer recreation areas for physical activities near home, and engage in more sedentary behaviors (Ebbeling et al. 2002).
Ethnicity also has a link with SES (Freedman et al. 2007). Freedman et al. (2007) compared ethnicity, BMI, and family income in TD children and found that body mass dropped with higher SES for Caucasians and Mexican Americans, but that BMI percentile increased for African American children as familial income rose. Alternatively, people of Asian descent have historically been lighter than peers from other ethnicities (Lauderdale and Rathouz 2000).
Some recent papers on the issue of risk for overweight (including this one) used clinical samples from the Autism Speaks Autism Treatment Network, or AS-ATN. Two research teams (de Vinck-Baroody et al. 2015 and Hill et al. 2015) used data from all AS-ATN sites and compared prevalence of overweight and obesity in children with ASD and in TD children and each noted significantly higher rates of overweight in those with ASD. Both groups studied a variety of demographic, clinical, sleep, and psychological risk factors by various logistic regression analyses that classified the children with ASD as having obesity/overweight or not. We conducted our analyses concurrently with de Vinck-Baroody et al. and Hill et al.; whereas they used discrete outcomes, we were interested in the full range of weight, measured continuously. Hill et al. used continuous scores for only a total score reflecting quality of sleep, Vineland Adaptive Behavior Scales (VABS) Adaptive Behavior Composite Score, and autism symptom severity, measured by the Autism Diagnostic Observation Schedule (Lord et al. 2000). All other variables used by Hill and colleagues and deVinck-Baroody et al. were forced into discrete categories that were generally dichotomous, usually a suboptimal data analytic strategy (Royston, Altman, & Sauerbrei 2006; Streiner 2002). For example, both studies used an IQ cut-off of 70 to classify participants as ID vs. non-ID, whereas we used the full IQ continuum. They used the clinical cutoff scores (t scores ≥70) on the Child Behavior Checklist (CBCL), whereas we used the full range on all subscales of the CBCL for examining associations with weight.
Participants in our AS-ATN sample were seen between June 2007 and June 2012. The children in de Vinck-Baroody et al. (2015) were enrolled between December 2007 and September 2012, whereas Hill and colleagues’ (2015) participants were from 2008 to 2013. As such, sample overlap and similarities between potential risk factors under investigation were unavoidable. Our studies differed in terms of statistical approaches employed, the use of different variables such as ASD subtype, choice and breadth of variables used, and the actual sample captured. Additionally, in the current study, medication class was broken out far more exhaustively than in the reports of de Vinck-Baroody et al. and Hill et al.
Objectives
Our goal was to identify risk factors (measured continuously) related to excess BMI (also measured continuously) in youth with ASD and to compare those findings to known correlates of obesity in TD children from previously published literature. Our hypothesis was that the risk variables for overweight in TD children would hold true for our large sample of children with ASD. If similar risk factors were confirmed for both children with ASD and TD children, this could open avenues for preventative treatment and interventions in youth with ASD that previously were thought to be specific to TD children.
Methods
Our analyses used deidentified data from the AS-ATN, and were approved by both an institutional review board and by the AS-ATN Scientific Review Committee. The AS-ATN is a network of medical centers in the United States and Canada that provide initial diagnoses and follow-up care to children with ASD and their families. The AS-ATN uses an interdisciplinary team approach that includes psychologists, pediatricians, neurologists, and psychiatrists. Each AS-ATN site obtained informed consent and collected physical assessments, IQ, autism-specific testing, and parent-completed forms to assess health, adaptive behavior, and psychopathology.
Instruments
The AS-ATN gathered a standard array of measures, and the following were included in our analyses.
Child Behavior Checklist (CBCL)
The CBCL (Achenbach and Rescorla 2001) is a behavior rating scale used to assess psychopathology in children ages 1.5–18 years, inclusive. It exists in two age categories, one for ages 1.5–5 years, and another for 6–18 years of age. The empirically derived questions align to criteria that are divided into (a) problem scales (Internalizing, Externalizing, and Total Problems), (b) syndrome scales (Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Social Problems, Thought Problems, Attention Problems, Rule-Breaking Behavior, Aggressive Behavior, Emotional Symptoms, and Pervasive Developmental Problems), and (c) DSM-oriented scales (Affective Problems, Anxiety Problems, Somatic Problems, Attention Deficits/ Hyperactivity Problems, Oppositional Defiant Problems, and Conduct Problems). Subscale alpha reliabilities reported for the 1.5–5 year rating form ranged from .66 (Anxious/Depressed) to .92 (for both Aggression and Externalizing) in a sample of TD children, and were found to be comparable for an ASD sample, with the exception of the Somatic Complaints subscale (Pandolfi et al. 2009).
Vineland Adaptive Behavior Scales-II (VABS)
The VABS (Sparrow et al. 2005) is an individually administered adaptive behavior scale designed to examine functional skills and normed from birth to 90 years of age. In order to minimize caregiver burden, the Survey Interview Form, the shortest of the interview formats, was used. Analyses used the Adaptive Behavior Composite Score, which was found to be significantly and negatively correlated (−.49, indicating higher levels of adaptive behavior were associated with fewer symptoms of autism; de Bildt et al. 2005) with scores received on the Autism Diagnostic Observation Schedule (Lord et al. 2000).
Intelligence Assessments
A variety of intelligence tests were administered at the discretion of site personnel, due to the heterogeneous presentation of children. The choice of what test to administer could be based on multiple factors, including language ability, time available for testing, and/or child cooperativeness. IQ assessments included the Stanford-Binet Intelligence Scales (Roid 2003), the Wechsler Intelligence Scales for Children-IV (Wechsler 2004), the Wechsler Preschool and Primary School (Wechsler 2002), and the Leiter International Performance Scale-Revised (Roid and Miller 1997).
Children’s Sleep Habits Questionnaire (CSHQ)
The CSHQ is a retrospective parent-completed questionnaire to characterize sleep behavior (Owens et al. 2000). The CSHQ data were assigned to subscales, which included Bedtime Resistance, Sleep Onset Delay, Sleep Duration, Sleep Anxiety, Night Waking, Parasomnias, Sleep Disordered Breathing, and Daytime Sleepiness. The CSHQ has decent internal consistency (.78), and is comparable to other sleep instruments (Spruyt and Gozal 2011).
Height, Weight, and BMI
AS-ATN staff members recorded (a) height, (b) weight, (c) age, and (d) sex. We used an Excel macro from the Centers for Disease Control to calculate child BMI and BMI percentile for later analyses (Children’s BMI Group Calculator – Metric Version 2010).
Medication
Common medications were listed by name in the AS-ATN data base. An “Other” option was also available if an agent was not listed in the choices given. We recoded medications into their drug classes as (a) stimulants, (b) atomoxetine, (c) SSRIs, (d) anticonvulsants, (e) antihistamines, (f) melatonin, (g) atypical antipsychotics, (h) alpha-2 agonists, and (i) other.
Diagnosis
The ASD diagnosis was based on the Autism Diagnostic Observation Schedule (Lord et al. 2000), and DSM-IV-TR diagnostic criteria (America Psychiatric Association 2000). Based on available information, the interdisciplinary team diagnosed each child as having autistic disorder, Asperger’s disorder, or pervasive developmental disorder – not otherwise specified (PDD-NOS). All data were collected through June 2012, prior to DSM-5 (American Psychiatric Association 2013) release and the new ASD criteria.
Analyses
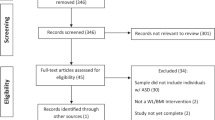
We conducted analyses using IBM SPSS Statistics 19 (IBM Corp 2010). Although the data set started with 6684 individual entries, this number included multiple entries from many participants. The data were reduced due to multiple patient visits, and only data from the first recorded visit were retained. While this typically resulted in use of data from the earliest visit being used, there were times when the IQ testing, for example, was not completed until a subsequent visit, in which case IQ data from the later visit were used.
There were substantial data missing from the CSHQ. A MCAR (Missing Completely at Random) test was run to determine whether the data were missing in a systematic way or by chance (Little 1988). The statistic, χ2 (2807, N = 2864) = 3668.71, p < .001, suggested that the data were missing in a consistent fashion, and could have confounded these analyses. We excluded participants with missing data, resulting in the final sample size of 2610. There were occasionally missing data for the CBCL scores (roughly 10 cases per subscale for the entire sample). Because data were missing at random and affected so few participants, the subscale average was used for missing values. Multicollinearity was investigated due to the size of the sample, and was found not to be a concern. A hierarchical regression model was used for this retrospective chart review to assess the individual contributions of several variables while keeping data continuous (including BMI percentile), whenever possible, to allow for the full range of variability to be expressed. Hierarchical regression models have variables entered in a series of blocks, which allows one to see if each new group of variables adds variance to the prediction produced by the previous blocks. This method avoided the use of logistic regression and odds ratios (used by both de Vinck-Baroody et al. 2015 and Hill et al. 2015), as interpretation of odds ratios becomes more difficult as the event under investigation (e.g., overweight/obesity) occurs in more than 10 % of the sample (Katz 2006), which was the case for excess weight. This analytic approach allowed us to use the full range of available scores by employing as many continuous variables as possible. Unnecessarily splitting data into discrete categories can reduce power of statistical tests and cause nuances in the data to be lost (Streiner 2002; Suissa 1991). Furthermore, analyses with discrete outcomes often produce odds ratios to denote the relationship strength between risk factors and the dependent variable. This is considered ill-advised when the outcome prevalence is higher than 10 %, as is the case with obesity, as it can lead to effect size misinterpretation (Katz 2006; Tajeu et al. 2012).
Participants
Participants were 2610 children and adolescents with ASD seen at the AS-ATN sites who completed the assessments of interest for this study. Table 1 lists demographic characteristics of the total sample. The participants ranged in age from 1.8 years to 18.1 years; average age was 6.4 years, with a standard deviation of 3.3 years. There were 2204 males (84.4 %), 1963 children (75.2 %) were Caucasian, and 1685 participants (64.6 %) had autistic disorder based on DSM-IV-TR. A plurality of mothers had completed some college (n = 817, 31.3 %), while fathers were most likely to have bachelor’s degrees (n = 644, 24.7 %). Table 2 presents the frequency of medication use; medicines were taken by 1123 participants (43 %). In all, 1487 received no medication, 605 received one, and the remainder (518, 19.8 %) received two or more medicines. The catch-all category of Other was used most (n = 663, 24.3 %) and included an array of agents (e.g., aspirin, complementary and alternative medicines, diabetes treatments) not listed on standardized medication forms. Table 3 shows mean subscale scores for CBCL and CSHQ, mean full-scale IQ score, and mean Adaptive Behavior Composite score for the VABS.
Results
For the sample of 2610 subjects, 118 (4.5 %) children were underweight, 859 (32.9 %) were overweight, and 452 (17.3 %) were obese based on BMI percentile. Thus, 1633 (62.6 %) children in the sample had normal weight for height. BMI percentile scores for participants in this study ranged from 0.00–99.99 %, with a mean BMI percentile of 63.53 % and standard deviation of 30.45 %. Please see Table 1 for additional BMI percentile information for sex, ethnicity, diagnosis, and maternal/paternal education.
Selected results from our hierarchical analyses can be seen in Table 4. Significant findings are in bold and include Hispanic ethnicity, SSRIs, alpha-2 agonists, high scores on the Withdrawn/Depressed or Aggressive Behavior CBCL subscale and Sleep Disordered Breathing CSHQ subscale being associated with greater weight. Being of Asian descent, higher levels of parental education, stimulants or atomoxetine use, and high scores on the Anxious/Depressed CBCL subscale were negatively associated with weight. Participants diagnosed with autistic disorder were heavier on average than participants with PDD-NOS. Table 5 is a statistical summary of this analysis and includes measures of model significance, block significance, amount of variance (a measure of effect size) associated with each block, and change in variance as blocks were added.
CBCL Version
In the first model tested, the CBCL subscales were limited to only those common to the 1.5–5 year form and the 6–18 year form. We could not include Emotional Symptoms, Pervasive Developmental Problems, Rule-Breaking Behavior, Social Problems, and Thought Problems in the previous models because they were only assessed on one version of the CBCL (preschool vs. school age). We also thought it prudent to investigate the preschool and school-age groups separately to determine whether the age-specific subscales were associated with excess weight.
For the younger 1.5–5 years CBCL group (see Tables 6 and 7), there were 1464 participants. In this model, age, use of stimulants, Withdrawn/Depressed scores, and ASD subtype were all significant predictors of BMI. Interestingly, other variables that were previously significant, such as ethnicity, paternal education, other medications (e.g., SSRIs), and sleep disturbances failed to emerge in this model.
There were 1084 older youth evaluated using the 6–18 year version of the CBCL (see Tables 8 and 9). African American ethnicity, Hispanic ethnicity, stimulants, atomoxetine, alpha-2 agonists, Aggressive Problems, Anxious/Depressed, ADHD Problems, Somatic Complaints, IQ, Adaptive Behavior Composite Score, Sleep Disordered Breathing, and ASD subtype were all significant predictors of BMI centile. Whereas there were fewer youth in the older CBCL category, more variables were significantly associated with BMI centile than the younger group.
In addition, we probed for interactions to evaluate whether age truly affected the relationship between weight and variables that could be measured in both age groups. We found that this appeared to be true for CBCL Somatic Complaints (F = 10.332, Δr 2 = .0039, p = .0013) and CSHQ Sleep Disordered Breathing (F = 3.732, Δr 2 = .0014, p = .05). This implies, for example, that the somatic complaints of young children impacted their weight at a lower level than the somatic complaints of older children.
Discussion
Predictors of Overweight and ASD in General
These analyses help to identify variables that contribute to abnormal weight in these children with ASD. Most were consistent with previously published literature in TD children; similarities will be addressed in the order that we reported them.
Age was significant in the model that looked at CBCL scores for younger children (1.5–5 years). In the first CBCL analysis, age was associated with greater BMI percentile, indicating that preschoolers’ age was positively but weakly associated with greater weight. This could be due to the fact that as children age, cumulative life style has greater opportunity to affect weight. They were also likely to have higher rates of medication use with age, a consistent finding in the literature (Aman et al. 2005).
The analyses demonstrated that Hispanic children were more likely to have elevated BMI percentile. Deckelbaum and Williams (2001) reported that Mexican-American children were more likely to be overweight than peers of other ethnicities. Children who were Asian generally had low body weight in relation to height, consistent with findings that identified Asian participants as lighter on average (Lauderdale and Rathouz 2000). African American heritage was only significantly associated with greater BMI percentile in the CBCL analysis for older children. Speculatively, the AS-ATN may have drawn participants, including African Americans, who were not typical of the general population (with higher education, SES, etc.). Therefore, the results may not have followed the usual ethnic expectations (de Vinck-Baroody et al. 2015).
Father’s educational level was negatively associated with BMI centile and could be reflective of two possible phenomena. First, more advanced education generally leads to greater prosperity (Beaton 1975). These individuals may be able to provide higher quality foods to their children. The lowest rating on the demographics form was assigned when there was no father present. This designation on the “education” continuum was likely associated with children from single-parent homes being heavier than those with two parents present, as was found in previous literature (Costello et al. 2001). This was likely due to possible income constraints associated with single parenting linked to food purchased or effects of stress.
The variable that was most associated with weight in these analyses was stimulant medication use, as it predicted lower BMI percentile in all analyses. It is well established that stimulant use can suppress appetite, leading to reduction in weight (Cortese et al. 2008; Faraone et al. 2008). Use of SSRIs was positively associated with BMI, indicating that children who took SSRIs were heavier than their peers. This is consistent with existing literature and suggests that SSRIs increase appetite and weight (Ferguson 2001). Children who took atomoxetine were more likely to be lighter than peers (e.g., Wernicke and Kratochvil 2002), while children who were prescribed alpha-2 agonists were heavier. Both observations are in line with some of the literature. One open-label study of guanfacine in children and adolescents with traumatic stress-related symptoms (Conner et al. 2013) found a small, but statistically significant, increase in weight from baseline to the sixth week of treatment. Several other studies (e.g., Jain et al. 2011; Kollins et al. 2011; Palumbo et al. 2008) did not report weight changes, so the association of alpha-2 agonists in TD children is somewhat uncertain.
Another variable that was consistently associated with BMI percentile was Sleep Disordered Breathing. There is a well-established relationship between weight and some sleep problems such as sleep apnea and snoring. There is a strong likelihood that disordered breathing during sleep did not actually cause participants to have higher levels of body mass. Instead, it is likely that there was a reciprocal relationship, in which people develop these respiratory conditions because of their excess weight. If this is the case, Sleep Disordered Breathing should not be treated as a risk factor for excess weight but rather as a result.
The Aggressive Behavior subscale of the CBCL reached significance in two analyses. Although we know that aggression is a common feature in children with ASD (Farmer and Aman 2011), it is not often associated with obesity and overweight. Farmer and Aman (2011) reported that children with ASD are frequently aggressive, but in a way that does not imply malicious intent. Instead, such children appear to have rather limited awareness of behavioral norms, and they tend to engage in impulsive (reactive) aggression. This study’s finding of aggression associated with BMI centile could be an aberration, or it could be due to larger children attempting to reach their goals through physical intimidation.
Interestingly, the results indicated that higher scores on the Anxious/Depressed subscale were associated with lower overall weight status. This negative relationship is in contrast to previous literature showing individuals with anxiety or depression were more likely to be overweight (Dockray et al. 2009). Since individual CBCL items were not available to enhance interpretation (i.e., anxiety and depression are intermixed in the subscale), future research may help to determine if this finding is attributed more to the anxiety or the depression elements of this subscale or whether they are necessarily intertwined at this developmental stage.
The CBCL Withdrawn/Depressed subscale was also associated with higher weight percentiles in all analyses. This is consistent with literature documenting the pattern in both TD adults and adolescents (Blaine 2008). However, it is difficult to say whether depression precedes weight gain, whether weight gain occurs first and depression follows, or if the process is dynamically interrelated. Both the ADHD problems subscale and the Somatic Complaints subscales were significant in one analysis, and for both it was within the older CBCL version. This finding may suggest that age plays a meaningful role. Our sample had more young children (n = 1464) than older children (n = 1084) and, in the case of ADHD symptoms, it may have been difficult to disentangle true ADHD symptoms from the normal exuberance of preschoolers.
The last variable to be associated with BMI centile was ASD subtype. Children with autistic disorder were more likely to have elevated body mass than youngsters with PDD-NOS. Thus, children with more severe ASD symptoms were more likely to be overweight. Many autistic symptoms (including most restricted interests, impairments in social interaction, being withdrawn) may be associated with sedentary behavior. Indeed, some literature has shown that children with autism appear to engage in more sedentary than active behavior, as recorded by accelerometers (MacDonald et al. 2011). In the future it will be useful to investigate specific ASD symptoms and their association with correlates of weight.
The following were variables that failed to predict increases in weight: sex, antihistamines, anticonvulsants, atypical antipsychotics, other medications, Bedtime Resistance, Sleep Onset Delay, Sleep Duration, Sleep Anxiety, Parasomnias, Daytime Sleepiness, Affective Problems, Anxiety Problems, and Conduct Disorder/Oppositional Defiant Disorder. Of these, the biggest surprise was that of atypical antipsychotics. Considerable literature reported significant positive associations between antipsychotics and weight (Correll 2007; Wetterling 2001). Our null finding became less surprising given the small but positive correlation between BMI percentile and atypical antipsychotics was highly correlated with other pharmacotherapies taken by participants. Additionally, it is intriguing that the Conduct Disorder/Oppositional Defiant Disorder subscale also did not predict weight. This is in contrast to literature that found TD children with oppositional defiant disorder were more likely to be obese (Mustillo et al. 2003). Whereas variables necessarily linked to autism (such as ASD subtype) were untestable in TD children, the majority of our findings were highly consistent with previous studies of TD children.
Predictors of Weight in AS-ATN Participants
Given that the studies by de Vinck-Baroody et al. (2015) and Hill et al. (2015) used partially overlapping data as this investigation, one may expect substantial agreement on variables evaluated by more than one research team; for instance, we all found that increased weight was associated with Hispanic ethnicity and lower levels of parental education. These two variables were measured in similar ways across all three studies. Older child age likewise appeared to demonstrate an increase in overweight and obesity when compared to younger children (found in all three studies), although we evaluated this within the confines of the CBCL versions (1.5–5 years vs. 6–18 years) while the other two studies divided age into three categories (2–5 years, 6–11 years, and 12–17 years).
Hill and associates’ (2015) measure of ASD severity failed to be significantly linked to excess weight, whereas our similar variable of ASD subtype was correlated with weight in our analyses. De Vinck-Baroody et al. (2015) found that higher scores on the VABS Composite were associated with lower rates of overweight and obesity; conversely, Hill and colleagues and this study found no such association. Additionally, de Vinck-Baroody’s group found a connection between weight and atypical antipsychotics, which we did not find. They used less specific medication categories (only stimulant, atypical antipsychotics, medication use in general, and more than one medication) than this study, which could have limited the dispersions of variance to other medication classes; Hill and colleagues collapsed their medication categories irrespective of clinical indication, so further comparisons cannot be drawn.
A final difference in our findings relates to the CBCL. De Vinck-Baroody and associates (2015) identified high scores (in their case, above the cut-off for clinical significance; t ≥ 70) on the Somatic Complaints subscale as being a risk factor for excess weight, as we did (while treating the variable as continuous) on the analysis for children ages 6–18, but the similarities end there. De Vinck-Baroody et al. also found children at or above the clinical cut-off for Total Problems more likely to be overweight or obese and children at or above the clinical cut-off for Internalizing Problems as less likely to be overweight. Hill et al. (2015), also using clinical cut-off criteria (t ≥ 70), found an association between Affective Problems and excess weight. In addition to the Somatic Complaints listed earlier, we found significant weight-related risk linked to the following subscales: Anxious/Depressed, Withdrawn/Depressed, ADHD Problems, and Aggressive Behaviors. The other researchers did not identify these risk relationships either because they did not investigate the subscales or used different analytic strategies (often involving lumping scores dichotomously into normal vs. abnormal). Our belief is that using the full continuum of scores yielded greater statistical power overall (Streiner 2002).
To sum up, this study shared some common data with de Vinck-Baroody et al. (2015) and Hill et al. (2015), but our analyses and results differed in several important aspects. These included (a) the use of continuous over discrete data, (b) the use of CBCL subscales (e.g., Emotion Problems, Social Problems, Thought Problems, Withdrawn/Depressed) not contained in the other reports, (c) inclusion of CSHQ subscales not covered elsewhere, (d) breakdown of psychotropic drugs, classified by drug action, (e) continuous IQ scores not reduced to above or below 70 points, and (f) presentation of the incremental variance accounted for by each variable in our tables (Tables 5, 7, and 9). We believe that this helps to “flesh out” aspects not covered in other reports.
Study Strengths
Much of the literature relating to children with ASD and overweight has been limited in terms of sample size and suboptimal measurement procedures (e.g., parental reporting of height, weight, diagnosis). This project addressed both of these issues. The sample comprised 2610 children, and participants’ height and weight were measured by professionals. Data bases comprising different geographic locations and maintained by clinicians are desirable for epidemiological weight-related research (Ogden et al. 2007). Having a broad network from which to evaluate data was a strength because the sample was large, based on multiple sites, and was fairly representative of children with ASD in the US and Canada. Our statistical analyses were novel for this data set and did not reduce weight or the variables under investigation to discrete categories as in some studies, which allowed for the full expression of the variables. These analyses that could potentially be more powerful given the increased range of these data, and we did not use odds ratios because the outcome variable was prevalent in more than 10 % of the population, which increases the chance for misinterpretation. Further, we made direct comparisons to previously published child weight literature to highlight the array of similarities that exist between TD children and those with ASD that have real-world application for clinicians, physicians, and researchers.
Study Limitations
This data set was not created for studying weight, resulting in some limitations of our variables. Although BMI is the usual standard for human weight research, it has shortcomings as well. These include inability to differentiate between different masses within the body and the problematic nature of child growth, which necessitates use of percentiles. Also, not all variables were available on all participants, which reduced our sample size, and the majority of measures collected (medications, CBCL, CSHQ, etc.) were derived by parent-report, which could detract from the quality of some variables. We were only able to account for a small amount of variance in these analyses (see Tables 5, 7, and 9), although that amount is consistent with other previous child weight research (e.g., Beebe et al. 2007; Memari et al. 2012). This limited explained variance indicates that there is much more work to be done in identifying risk factors for overweight. This investigation would have been stronger had the project included a group of TD children that could have been directly compared to our sample with ASD, a standardized measure of physical activity, and a standardized diet log.
Conclusions and Future Directions
It is well established that overweight children are more likely than others to become adults with similar weight problems (Dietz 1997; Freedman et al. 2004). It seems especially important to identify risk factors for obesity within children with ASD, as these children are already significantly disadvantaged. The study was able to confirm many of the findings that we were aware of from the existing literature with TD children. This similarity between children and adolescents with ASD and TD youth is important, in and of itself, since these groups tend to have great differences in how they react to life in general.
The substantial agreement found here for risk factors for overweight suggests that existing intervention programs for children with weight problems can be used for children with ASD since the intervention should target problem areas that apply to both groups. Early identification of children with ASD with comorbid psychopathologies or who are prescribed medications associated with weight gain, for example, should be monitored by medical personnel to ensure that problematic changes to weight are not overlooked. While outside the scope of this study, intervention programs that focus on increasing physical activity while decreasing sedentary behaviors have shown promise in reducing BMI for both TD children and those with ASD, although long-term maintenance of those reductions still needs to be investigated (Atlantis et al. 2006; Pitetti et al. 2007). Similarly, diet modifications to increase nutritional quality and reduce calorie or fat intake should be investigated, as such changes have been useful (Memari and Ziaee 2014). Though alterations will likely need to be made for comprehension and to proactively address transitions, aversive stimuli, etc., the benefits of being able to integrate existing protocols that have previously been researched and found successful are considerable.
References
Achenbach, T. M. & Rescorla, L. (2001). Ratings of relations between DSM-IV diagnostic categories and items of the CBCL/11/2–5 and C-TRF.
Allison, D. B., Packer-Munter, W., Pietrobelli, A., Alfonso, V. C., & Faith, M. S. (1998). Obesity and developmental disabilities: pathogenesis and treatment. Journal of Developmental and Physical Disabilities, 10(3), 215–255 Retrieved from http://springerlink.bibliotecabuap.elogim.com/article/10.1023/A:1022888323684.
Aman, M. G., Lam, K. S. L., & Van Bourhandien, M. E. (2005). Medication patterns in patients with autism: temporal, regional, and demographic influences. Journal of Child and Adolescent Psychopharmacology, 15, 116–126. doi:10.1089/cap.2005.15.116.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5.). American Psychiatric Pub.
Atlantis, E., Barnes, E. H., & Sign, M. F. (2006). Efficacy of exercise for treating overweight in children and adolescents: a systematic review. International Journal of Obesity, 30(7), 1027–1040. doi:10.1038/sj.ijo.0803286.
Beaton, A.E. (1975). The influence of education and ability on salary and attitudes. In Education, income, and human behavior (pp. 365–396). NBER.
Beebe, D. W., Lewin, D., Zeller, M., McCabe, M., MacLeod, K., Daniels, S. R., & Amin, R. (2007). Sleep in overweight adolescents: shorter sleep, poorer sleep quality, sleepiness, and sleep-disordered breathing. Journal of Pediatric Psychology, 32(1), 69–79. doi:10.1093/jpepsy/jsj104.
Bernstein, J. G. (1987). Induction of obesity by psychotropic drugs. Annals of the New York Academy of Sciences, 203–215. doi:10.1111/j.1749-6632.1987.tb36212.x.
Blaine, B. (2008). Does depression cause obesity? A meta-analysis of longitudinal studies of depression and weight control. Journal of Health Psychology, 13(8), 1190–1197. doi:10.1177/1359105308095977.
Chen, A. Y., Kim, S. E., Houtrow, A. J., & Newacheck, P. W. (2010). Prevalence of obesity among children with chronic conditions. Obesity, 18(1), 210–213. doi:10.1038/oby.2009.185.
Children’s BMI Group calculator – metric version 2010. Retrieved from http://www.cdc.gov/healthyweight/assessing/bmi/childrens_BMI/tool_for_schools.html.
Conner, D. F., Grasso, D. J., Slivinsky, M. D., Pearson, G. S., PMH-CNS, F. A. A. N., & Banga, A. (2013). An open-label study of guanfacine extended release for treatment of stress related symptoms. Journal of Child and Adolescent Psychopharmacology, 23(4), 244–251. doi:10.1089/cap.2012.0119.
Correll, C. U. (2007). Weight gain and metabolic effects of mood stabilizers and antipsychotics in pediatric bipolar disorder: a systematic review and pooled analysis of short-term trials. Journal of the American Academy of Child and Adolescent Psychiatry, 46(6), 687–700. doi:10.1097/chi.0b013e318040b25f.
Cortese, S., Angriman, M., Maffeis, C., Isnard, P., Konofal, E., Lecendreux, M., Purper-Ouakil, D., Vincenzi, B., Bernardina, B. D., & Mouren, M. C. (2008). Attention deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Critical Reviews in Food Science and Nutrition, 48, 524–537. doi:10.1080/10408390701540124.
Costello, E. J., Keeler, G. P., & Angold, A. (2001). Poverty, race/ethnicity and psychiatric disorder: a study of rural children. American Journal of Public Health, 91, 1494–1498. doi:10.2105/AJPH.91.9.1494.
Curtin, C., Bandini, L. G., Perrin, E. C., Tybor, D. J., & Must, A. (2005). Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: a chart review. BMC Pediatrics, 5, 48. doi:10.1186/1471-2431-5-48.
Curtin, C., Anderson, S. E., Must, A., & Bandini, L. (2010). The prevalence of obesity in children with autism: a secondary data analysis using nationally representative data from the nation survey of Children’s health. BMC Pediatrics, 10, 11. doi:10.1186/1471-2431-10-11.
Daniels, S. R. (2006). The consequences of childhood overweight and obesity. The Future of Children, 16(1), 47–67 Retrieved from http://www.jstor.org/stable/3556550.
de Bildt, A., Kraijer, D., Sytema, S., & Minderaa, R. (2005). The psychometric properties of the Vineland adaptive behavior scales in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders, 35(1), 53–62. doi:10.1007/s10803-004-1033-7.
de Vinck-Baroody, O., Shui, A., Macklin, E. A., Hyman, S. L., Leventhal, J. M., & Weitzman, C. (2015). Overweight and obesity in a sample of children with autism spectrum disorder. Academic Pediatrics, 15(4), 396–404. doi:10.1016/j.acap.2015.03.008.
Deckelbaum, R. J., & Williams, C. L. (2001). Childhood obesity: the health issue. Obesity Research, 9(S4), 239S–243S. doi:10.1038/oby.2001.125.
Dietz, W. H. (1997). Periods of risk in childhood for the development of adult obesity—what do we need to learn? The Journal of Nutrition, 127(9), 1884S–1886S Retrieved from http://jn.nutrition.org/content/127/9/1884S.long.
Dockray, S., Susman, E. J., & Dorn, L. D. (2009). Depression, cortisol reactivity, and obesity in childhood and adolescence. Journal of Adolescent Health, 45, 344–350. doi:10.1016/j.jadohealth.2009.06.014.
Ebbeling, C. B., Pawlak, D. B., & Ludwig, D. S. (2002). Childhood obesity: public-health crisis, common sense cure. The Lancet, 360, 473–482. doi:10.1016/S0140-6736(02)09678-2.
Faraone, S. V., Biederman, J., Morley, C. P., & Spencer, T. J. (2008). Effect of stimulants on height and weight: a review of the literature. Journal of the American Academy of Child and Adolescent Psychiatry, 47(9), 994–1009. doi:10.1097/CHI.ObO13e31817eOea7.
Farmer, C. A., & Aman, M. G. (2011). Aggressive behavior in a sample of children with autism spectrum disorders. Research in Autism Spectrum Disorders, 5, 317–323. doi:10.1016/j.rasd.2010.04.014.
Ferguson, J. M. (2001). SSRI antidepressant medications: adverse effects and tolerability. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 22–27. doi:10.4088/PCC.v03n0105.
Flint, J., Kothare, S. V., Zihlif, M., Suarez, E., Adams, R., Legido, A., & DeLuca, F. (2007). Associations of inadequate sleep and insulin resistance in obese children. Journal of Pediatrics, 150(4), 364–369. doi:10.1016/j.jpeds.2006.08.063.
Freedman, D. S., Khan, L. K., Dietz, W. H., Srinivasan, S. R., & Berenson, G. S. (2001). Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa heart study. Pediatrics, 108(3), 712–718. doi:10.1542/peds.108.3.712.
Freedman, D. S., Khan, L. K., Serdula, M. K., Dietz, W. H., Srinivasan, S. R., & Berenson, G. S. (2004). Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa heart study. International Journal of Obesity, 28, 10–16. doi:10.1038/sj.ito.0802544.
Freedman, D. S., Mei, Z., Srinivasan, S. R., Berenson, G. S., & Dietz, W. H. (2007). Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa heart study. The Journal of Pediatrics, 150(1), 12–17. doi:10.1016/j.jpeds.2006.08.042.
Grondhuis, S. N., & Aman, M. G. (2013). Overweight and obesity in youth with developmental disabilities: a call to action. Journal of Intellectual Disability Research. doi:10.1111/jir.12090.
Hill, A. P., Zuckerman, K. E., & Fombonne, E. (2015). Obesity and autism. Pediatrics, 136(6) peds-2015. doi:10.1542/peds.2015-1437.
Hollway, J. A., & Aman, M. G. (2011). Sleep correlates of pervasive developmental disorders: a review of the literature. Research in Developmental Disabilities, 32, 1399–1421. doi:10.1016/j.ridd.2011.04.001.
IBM Corp (2010). IBM SPSS statistics for windows, version 19.0. Armonk, NY: IBM Corp.
Ito, J. (2006). Brief research report: obesity and its related health problems in people with intellectual disabilities. Journal of Poly and Practice in Intellectual Disabilities, 3(2), 129–132. doi:10.1111/j.1741-1130.2006.00064.x.
Jain, R., Segal, S., Kollins, S. H., & Khayrallah, M. (2011). Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50(2), 171–179. doi:10.1016/j.jaac.2010.11.005.
Katz, K. A. (2006). The (relative) risks of using odds ratios. Archives of Dermatology, 142, 761–764. doi:10.1001/archderm.142.6.
Kollins, S. H., Jain, R., Brams, M., Segal, S., Findling, R. L., Wigal, S. B., & Khayrallah, M. (2011). Clonidine extended-release tablets as add-on therapy to psychostimulants in children and adolescents with ADHD. Pediatrics, 127(6), e1406–e1413. doi:10.1542/peds.2010-1260.
Lauderdale, D. S., & Rathouz, P. J. (2000). Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. International Journal of Obesity, 24(9), 1188–1194. doi:10.1038/sj.ijo.0801365.
Little, R. J. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202 Retrieved from http://medrescon.tripod.com/docs/little_paper.pdf.
Lobstein, T., Baur, L., & Uauy, R. (2004). Obesity in children and young people: a crisis in public health. Obesity Reviews, 5(s1), 4–85. doi:10.1111/j.1467-789X.2004.00133x.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., et al. (2000). The autism diagnostic observation schedule—generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. doi:10.1023/A:1005592401947.
MacDonald, M., Esposito, P., & Ulrich, D. (2011). The physical activity patterns of children with autism. BMC Research Notes, 4(1), 422. doi:10.1186/1756-0500-4-422.
Memari, A.H. & Ziaee, V. (2014). Overweight and obesity epidemic: Weight status in individuals with autism. In Comprehensive Guide to Autism (pp. 1955–1971). New York: Springer.
Memari, A. H., Kordi, R., Ziaee, V., Mirfazeli, F. S., & Setoodeh, M. S. (2012). Weight status in Iranian children with autism spectrum disorders: investigation of underweight, overweight and obesity. Research in Autism Spectrum Disorders, 6(1), 234–239. doi:10.1016/j.rasd.2011.05.004.
Mustillo, S., Worthman, C., Erkanli, A., Keeler, G., Angold, A., & Costello, E. J. (2003). Obesity and psychiatric disorders: developmental trajectories. Pediatrics, 111(4), 851–859. doi:10.1542/peds.111.4.851.
Ogden, C. L., Yanovski, S. Z., Carroll, M. D., & Flegal, K. M. (2007). The epidemiology of obesity. Gastroenterology, 132, 2087–2102. doi:10.1053/j.gastro.2007.03.052.
Owens, J. A., Spirito, A., & McGuinn, M. (2000). The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep, 23(8), 1043–1052 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11145319.
Palumbo, D. R., Sallee, F. R., Pelham, W. E., Bukstein, O. G., Daviss, W. B., McDermott, M. P., & CAT Study Team (2008). Clonidine for attention-deficit/hyperactivity disorder: I. Efficacy and tolerability outcomes. Journal of the American Academy of Child and Adolescent Psychiatry, 47(2), 180–188. doi:10.1097/chi.0b013e31815d9af7.
Pandolfi, V., Magyar, C. I., & Dill, C. A. (2009). Confirmatory factor analysis of the child behavior checklist 1.5-5 in a sample of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 986–995. doi:10.1007/s10803-009-0716-5.
Phillips, K. L., Schieve, L. A., Visser, S., Boulet, S., Sharma, A. J., Kogan, M. D., Boyle, C. A., & Yeargin-Allsopp, M. (2014). Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Maternal and Child Health Journal, 18(8), 1964–1975. doi:10.1007/s10995-014-1442-y.
Pitetti, K. H., Rendoff, A. D., Grover, T., & Beets, M. W. (2007). The efficacy of a 9-month treadmill walking program on the exercise capacity and weight reduction for adolescents with severe autism. Journal of Autism and Developmental Disorders, 37(6), 997–1006. doi:10.1007/s10803-006-0238-3.
Roid, G. H. (2003). Stanford Binet Intelligence Scales (5th ed.). Itasca, IL: Riverside Publishing.
Roid, G. H., & Miller, L. J. (1997). Leiter international performance scale-revised. Wood Dale, IL: Stoelting Col.
Royston, P., Altman, D. G., & Sauerbrei, W. (2006). Dichotomizing continuous predictors in multiple regression: a bad idea. Statistics in Medicine, 25(1), 127–141. doi:10.1002/sim.2331.
Sharp, A. M., Pawlak, R., & Ding, Q. (2014). Weight status and growth patterns among children with autism living in North Carolina. Topics in Clinical Nutrition, 29(1), 10–14. doi:10.1097/01.TIN.0000443022.75534.3b.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. doi:10.1097/CHI.0b013e318179964f.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland adaptive behavior scales, second Ed. In Survey forms manual. Bloomington, MN: NCS Pearson, Inc..
Spruyt, K., & Gozal, D. (2011). Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Medicine Reviews, 15(1), 19–32. doi:10.1016/j.smrv.2010.07.005.
Streiner, D. L. (2002). Breaking up is hard to do: the heartbreak of dichotomizing continuous data. Canadian Journal of Pcyhiatry, 47(3), 262–265. doi:10.1177/070674370204700307.
Suissa, S. (1991). Binary methods for continuous outcomes: a parametric alternative. Journal of Clinical Epidemiology, 44(3), 241–248 Retrieved from http://www.sciencedirect.com/science/article/pii/0895435691900358.
Tajeu, G. S., Sen, B., Allison, D. B., & Menachemi, N. (2012). Misuse of odds ratios in obesity literature: an empirical analysis of published studies. Obesity, 20(8), 1726–1731. doi:10.1038/oby.2012.71.
Wechsler, D. (2002). WPPSI-III: administration and scoring manual. San Antonio, TX: The Psychological Corporation.
Wechsler, D. (2004). WISC-IV: administration and scoring manual. San Antonio, TX: Harcourt Assessment, Inc..
Wernicke, J. F., & Kratochvil, C. J. (2002). Safety profile of atomoxetine in the treatment of children and adolescents with ADHD. Journal of Clinical Psychiatry, 63(S12), 50–55 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12562062.
Wetterling, T. (2001). Bodyweight gain with atypical antipsychotics: a comparative review. Drug Safety, 24(1), 59–73. doi:10.2165/00002018-200124010-00005.
World Health Organization (2000). Obesity: preventing and managing the global epidemic. (No. 894). World Health Organization.
Xiong, N., Ji, C., Li, Y., He, Z., Bo, H., & Zhao, Y. (2009). The physical status of children with autism in China. Research in Developmental Disabilities, 30(1), 70–76. doi:10.1016/j.ridd.2007.11.001.
Acknowledgment
This Network activity was supported by Autism Speaks and cooperative agreement UA3 MC11054 through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program to the Massachusetts General Hospital. This work was conducted through the Autism Speaks Autism Treatment Network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No research funding was obtained by the authors for this manuscript. The Autism Speaks Autism Treatment Network generously provided us with use of their database to make these analyses possible.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in this study at the assessment site per AS-ATN protocol.
Conflicts of Interest
The authors declare that they have no additional conflicts of interest.
Rights and permissions
About this article
Cite this article
Grondhuis, S.N., Aman, M.G. Risk Factors for Overweight in Children with Autism Spectrum Disorder. J Dev Phys Disabil 29, 241–263 (2017). https://doi.org/10.1007/s10882-016-9522-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-016-9522-0