Abstract
Purpose of Review
Kratom, a preparation of the leaves collected from the Southeast Asian plant Mitragyna speciosa, has increased in use within the United States (US) predominantly due to its stimulant and opioid-like effects. It contains many active alkaloids, most notably mitragynine. Clinical pharmacological research and toxicological information are limited, hindering forensic interpretation and an understanding of the role kratom use may play in death. Despite arguments from some vocal proponents and vendors that kratom poses no risk to users, there is a growing body of evidence that kratom use can result in significant adverse events, including death.
Recent Findings
Toxicological data for blood specimens analyzed between January 2018 and September 2022 in postmortem and driving under the influence of drugs cases were reviewed for the presence of mitragynine, the primary alkaloid of Mitragyna speciosa. Reported blood mitragynine concentrations, compound positivity, and concomitant findings were evaluated.
Summary
The forensic interpretation of mitragynine continues to be challenging. Kratom has been implicated in an increasing number of overdoses and deaths, and its significance is difficult to ascertain due to a substantial number of confounding variables, including a limited scope of toxicological testing and frequent co-positivity with drugs of abuse. Mitragynine has been listed as the primary toxicological finding in several overdose deaths albeit at a lower frequency compared to overall positivity, particularly when present at elevated concentrations (> 1000 ng/mL); these cases provide forensic confirmation of harms due to kratom use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kratom is the herbal substance derived from the leaves of Mitragyna speciosa, a large evergreen tree of the same name native to Southeast Asia, that has centuries of ethnobotanical use [1•]. Common preparations of dried or fresh leaves, either chewed or made into a tea, provide mild stimulation to ward off fatigue, akin to traditional South American use of coca leaf [2]. Larger doses may cause anxiolytic and opioid-like effects and is often used for managing pain and opioid dependence [3, 4]. These potentially beneficial aspects of kratom use are complicated by its legal status in Southeast Asian countries. In Malaysia, it is illegal to possess or use kratom, despite the tree growing freely throughout the country. In Thailand, kratom was fully legalized in 2021 after having been banned for nearly 80 years.
Over the last two decades, kratom use has grown in popularity in western countries, particularly the US, where kratom is legal at the federal level and banned in only a few states. Kratom is widely available as an herbal supplement online and in smoke shops, with ground leaves sold as powders and in capsules, and concentrated extracts sold as tinctures and drinks. Its popularity, however, has also seen kratom products expand into seltzers, sodas, and ready-portioned drink sachets. Reasons for use varies, but online surveys suggest that kratom is used most frequently for self-treating anxiety, depression, and pain, and for relieving withdrawal symptoms of other opioids [5, 6]. But while kratom may be beneficial, some self-report “kratom use disorder,” with approximately 30% of respondents in a US online survey describing tolerance, cravings, and moderate withdrawal symptoms such as restlessness, anxiety, and fatigue [7].
Kratom’s analgesic activity and use in self-treatment of opioid use disorders (OUD) results largely from mitragynine, the predominant alkaloid present in the leaves. Although alkaloid content varies with kratom chemotypes and environmental conditions, mitragynine comprises approximately 66% of the alkaloids in crude kratom extract, with other notable alkaloids including the mitragynine diastereomers speciogynine, speciociliatine, and mitraciliatine [8]. Kratom extract also contains a small amount of psychoactive 7-hydroxymitragynine which is not present in the plant itself, but generated post-harvest by the oxidation of mitragynine, which accounts for its wide variability in kratom products [9]. 7-Hydroxymitragynine is also an active metabolite of mitragynine, formed primarily via hepatic CYP3A4 metabolism [10••].
Pharmacologically, mitragynine and 7-hydroxymitragynine are the primary bioactive compounds, and thought to be responsible in part for kratom’s psychoactive and analgesic effects. Binding affinities (Ki) for mitragynine alkaloids at the human mu-opioid receptor (hMOR) using radioligand displacement assays were calculated to be 223 nM and 47 nM for mitragynine and 7-hydroxymitragynine, respectively [11]. Functional assays at hMOR using bioluminescence resonance energy transfer (BRET) showed mitragynine and 7-hydroxymitragynine to be partial agonists, with EC50 concentrations of 339 nM and 35 nM, respectively [11]. In comparison, morphine is a full MOR agonist in the same assay, with an EC50 of 3 nM, making mitragynine and 7-hydroxymitragynine between 100- and 10-times less potent respectively than morphine [11]. Both compounds are weak antagonists at human kappa-opioid and delta-opioid receptors [11]. In addition to opioid receptor activity, various kratom alkaloids have demonstrated serotonergic and adrenergic activity in vitro and in vivo, perhaps adding to kratom’s mood altering and analgesic activity [12, 13].
Despite modest MOR activity, the reported effects of kratom are not completely explained by its pharmacological profile. It is likely that kratom’s activity is a complex interaction of the various alkaloids’ agonist and antagonist effects.
Kratom’s psychoactive effects may also be affected by another biochemical mechanism. While 7-hydroxymitragynine is a major metabolite of mitragynine, it is also a degradation product in stored whole blood, and in preliminary in vitro research in human plasma, it has demonstrated conversion to mitragynine pseudoindoxyl [14••]. Mitragynine pseudoindoxyl has a greater binding affinity for hMOR (Ki 0.8 nM), and in GTPγS functional assays, is a full MOR agonist (EC50 1.7 nM) [15•], and may also contribute to the pharmacological effects, effectively making mitragynine a pro-drug for mitragynine pseudoindoxyl.
The increased activity of 7-hydroxymitragynine and mitragynine pseudoindoxyl is not lost to online retailers. Offerings of “Bentuangie Kratom” claim a fermentation process increases the concentration of 7-hydroxymitragyine, while converting some of it to mitragynine pseudoindoxyl, potentially making it one of the most potent kratom products available [16]. Because kratom products are unregulated and not monitored or approved by the US Food and Drug Administration (FDA), products such as these often offer little guidance or scientific perspective on safe use, potentially resulting in adverse events.
In a review of 935 self-reported kratom-only exposures between 2011 and 2018 in the National Poison Data System, the most common adverse events were agitation (18.6%), tachycardia (16.9%), and drowsiness (13.6%) [17]. Severe adverse effects included seizures (6.1%), respiratory depression (2.8%), and coma (2.3%); a limitation of this work is the lack of toxicology testing, both to confirm the use of kratom and rule out presence of other substances, although self-reported exposures to multiple substances (including kratom) were excluded from the dataset [17]. Though kratom intoxications do not always present like opioid overdoses, its cardiotoxicity should not be overlooked. Recent studies suggest kratom can cause a prolonged QTc interval and torsade de pointes in a dose-dependent manner [18], much like methadone [19]. An additional concern is the potential for dependence and addiction resulting from long-term use. While a large proportion of users report using kratom to reduce or replace prescription or illicit opioid use [5, 20], long-term kratom use can lead to withdrawal symptoms, some of which have been attenuated with the opioid partial-agonist buprenorphine [21, 22]. The use of buprenorphine, however, is complicated, and care should be used when patients are naïve to traditional opioids [23].
Mitragynine is also increasingly found in postmortem toxicological casework. In one dataset, looking at 583 postmortem cases that were tested within 35 days of specimen collection, the mean and median blood concentrations were 372 ng/mL and 140 ng/mL, respectively [24••]. Nearly all of these fatalities were polydrug overdose deaths, with the most frequent concomitant findings being opioids and benzodiazepines. With the increased usage and ease of obtaining kratom products, some of which may be fortified with kratom alkaloids or adulterated with other drugs, it is advisable that toxicology laboratories include at least mitragynine, and if feasible, other related alkaloids, in their screening techniques.
To increase our understanding of mitragynine and its significance in forensic casework, we completed a review of recently published postmortem cases in the literature that included toxicological confirmation of mitragynine, with an emphasis on cases in which mitragynine was ruled and/or likely to have played a significant role in the cause of death; cause of death (COD) was provided in six of the cases and listed as acute mitragynine intoxication (Table 1). These reports typically include cases in which mitragynine was the only finding, in addition to cases in which mitragynine was likely the primary cause of toxicity relative to the other drugs present. In addition, we report blood mitragynine concentrations, drug co-positivity, and temporal trends of positivity in cases from our own laboratory from data reported between 2018 and September 2022.
Methods
Searches were conducted in PubMed using the terms “mitragynine”, “postmortem”, “kratom”, overdose”, and “toxicity”. Articles identified were screened by the authors to identify those that specifically reported deaths related to mitragynine use.
Mitragynine positivity was assessed in casework reported from our own laboratory. Cases were identified as postmortem based on the ordering of a postmortem test panel or impaired driving based on ordering of a panel specified for driving under the influence of drugs (DUID) cases; these results were searched after the inclusion of quantitative mitragynine confirmation within the scope of testing. Analysis for mitragynine was previously described by Papsun et al. [24••], with screening performed using high-performance liquid chromatography time-of-flight mass spectrometry (LC-TOF/MS) and quantitative confirmation testing performed by liquid chromatography tandem mass spectrometry (LC-MS/MS). Toxicology data reported between January 2018 and September 2022 were queried for the reporting of mitragynine and concentrations in blood specimens. Blood concentrations, trend information, and concomitant findings were compiled.
Results
Mitragynine was reported in 6860 blood specimens submitted for forensic toxicology analysis between January 2018 and September 2022. The number of blood specimens positive for mitragynine each year, blood concentration statistics, and positivity rate are listed in Table 2. The blood positivity rate is reported from the frequency of detections in a routine postmortem panel.
Blood Concentrations
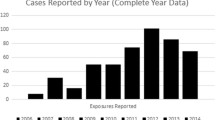
In this dataset from the reporting laboratory, specimens included antemortem blood collected from living individuals and postmortem blood collected during medico-legal death investigations. In Table 2, the blood statistics are calculated using the entirety of the dataset, without specifically delineating the entire population into human-performance, postmortem, hospitalizations, or other cases. Since directed testing is available for mitragynine, not all cases have additional details available to identify the case type. During the reporting period, blood concentrations ranged from 5.0 ng/mL (the reporting limit of the analytical method) to 11000 ng/mL. Of the 6860 blood specimens in this work, 78% were identified as postmortem based on the original panel ordered (n = 5413) and had mean and median blood mitragynine concentrations of 360 and 120 ng/mL, respectively, with a range of 5.4–11,000 ng/mL. Mitragynine reported from impaired driving investigations was a smaller population (n = 127), comprising less than 2% of the reported cases. Mean and median concentrations in these cases were 133 and 62 ng/mL, respectively, with a range of 8.8–1000 ng/mL, lower than that of the postmortem cases. Figure 1 shows a histogram of the percentage of cases per concentration bin pulled from specimens sent specifically for postmortem and impaired driving toxicology panels. The data shows that the majority of blood concentrations fall below 500 ng/mL, and that only postmortem specimens reported mitragynine greater than 1000 ng/mL. The remaining blood specimens were submitted for directed mitragynine analysis and could include postmortem specimens from death investigations or antemortem specimens from hospitalizations.
Percentage of positive blood mitragynine specimens from postmortem (PM) and driving under the influence of drugs (DUID) cases per concentration interval. Blood concentrations must be less than the listed concentration to count in that bin. During the reporting period, there were 5413 defined PM cases and 127 defined DUID cases
Additional Findings
In toxicology casework, mitragynine is most frequently detected together with other substances. Fentanyl was the most frequent finding with mitragynine, which is likely tied to the rise in its illicit manufacturing and distribution. In 2018, fentanyl was found in 33% of mitragynine-positive cases. This combination has steadily increased over time, with fentanyl reported in 62% of mitragynine-positive blood cases in 2022, slightly down from a peak of 63% in 2021. Co-positivity for the stimulant methamphetamine has also increased steadily over recent years. In 2018, methamphetamine was found in 9% of mitragynine-positive cases, and by 2022, it more than doubled to 19%. Cocaine co-positivity has increased over time as well, rising from 7.8% in 2018 to 10% in 2022. Concomitant reporting of mitragynine with Delta-9 THC has been consistent over the 5-year period, with positivity varying between 22 and 25%. Reporting of mitragynine in combination with other prescription opioids has also been steady over time, with hydrocodone, tramadol, and buprenorphine reporting averages of 5.3% ± 0.72, 3.9% ± 0.58, and 2.0% ± 0.58, respectively, in mitragynine-positive cases, in the reporting period. Benzodiazepines were also frequently reported with mitragynine in the studied time period. Alprazolam (Xanax®) and clonazepam and/or its metabolite 7-aminoclonazepam (Klonopin®), two of the most commonly prescribed FDA-approved benzodiazepines, are each being detected in approximately 13% of cases. Diazepam (Valium®) trailed slightly behind, at approximately 10% co-positivity. Etizolam, a non-FDA-approved benzodiazepine and a substance classified as a designer benzodiazepine, was detected in 3.1% of mitragynine cases.
Discussion
It is clear from the mitragynine positivity in toxicological casework that kratom is part of the current US drug landscape. Since 2019, mitragynine positivity detected through a comprehensive postmortem panel ranged between 1.67 and 1.88% of all cases tested within the specified timeframe (total N = 6075). Positive cases from this study have been reported in 47 different US states, Washington DC, the Virgin Islands, and 5 different Canadian provinces. Mitragynine’s steady appearance in forensic casework has resulted in much debate over the significance of its involvement in impaired driving and postmortem investigations [31•].
Blood Concentrations
In this study, blood concentrations varied widely from 5.0 to 11,000 ng/mL. There is limited information reflecting blood concentrations of mitragynine from pharmacokinetic or pharmacodynamic studies. One such study documented mitragynine blood concentrations up to 191 ng/mL after consumption of kratom tea prepared with mitragynine concentrations of 104, 166, and 192 g/mL, with no adverse effects noted by chronic users [32]. Another study looked at the pharmacokinetics of kratom alkaloids after drinking kratom tea prepared from 2 g of a dry leaf powder. The seven study participants had peak blood mitragynine concentrations ranging from 19.9 to 70.5 ng/mL, with no adverse events related to kratom ingestion [33•]. In a postmortem study, the average blood concentration in 15 decedents with non-pathological causes of death was 332 ± 495 ng/mL, which was compared to an average mitragynine blood concentration of 114 ± 145 ng/mL found in 12 traumatic accident victims [34•].
In the data from 6860 cases presented above, more than 90% of the reported blood concentrations fell below 1000 ng/mL, with approximately 9.5% of the cases greater than 1000 ng/mL, and 6.1% of the cases greater than 1500 ng/mL. In previous work, we cautioned that blood concentrations greater than 1000 ng/mL are becoming more frequent and increasingly associated with cause of death [29]. In 6 cases from the literature (Table 1) in which acute intoxication of mitragynine was listed as the cause of death, blood concentrations were 1900, 1590, 3390, 3430, 2325, and 3809 ng/mL [27, 28, 30•]. In 12 cases of mitragynine-only positive deaths, and mitragynine toxicity listed as the cause of death, blood concentrations ranged from 730 to 5900 ng/mL with a median concentration of 2000 ng/mL [35]. The highest blood concentration reported in the current analysis was 11,000 ng/mL, the highest blood concentration reported to date, and over 10 times higher than the highest blood concentration reported in any impaired driving investigation (1000 ng/mL). Concentrations of > 1000 ng/mL are well above documented concentrations from the pharmacokinetic studies after drinking kratom tea as well as the one postmortem study with non-pathological causes of death [32, 33, 34•].
Additional Findings
When attempting to determine the significance of a toxicological finding, it is important to consider concomitant findings. Each case needs to be evaluated on its own merit, because even in cases of polypharmacy, other findings may be deemed insignificant, such as the death of a 56 y/o female with a history of chronic obstructive pulmonary disease (COPD) with prescribed medications of oxycodone and lorazepam. In this case, positive findings included 2500 ng/mL of mitragynine, 190 ng/mL of oxycodone, and 62 ng/mL of lorazepam in femoral blood, with mitragynine listed as the primary cause of toxicity, as the oxycodone and lorazepam were to be expected [26•]. Another case reported 1060 ng/mL of mitragynine and 150 ng/mL of 7-hydroxymitragynine, along with 43 ng/mL zopiclone, 360 ng/mL citalopram, and 5.4 mg/L of lamotrigine in a death of a middle-aged man with a history of substance use including “Kratom” purchased via the internet [36]. In two cases previously reported by the authors, mitragynine was primarily implicated at high concentrations and with low concentrations of other findings, although the COD was listed as mixed drug toxicity: one case involved 3300 ng/mL of mitragynine with 450 ng/mL of sertraline and 930 ng/mL of norsertraline reported in femoral blood and the other reported 2900 ng/mL of mitragynine with 31 ng/mL of alprazolam in iliac blood [24••]. Many of the other findings in these cases were those within expected levels of prescriptions and some, such as citalopram, lamotrigine, and sertraline, are not substances that are typically implicated in deaths.
Frequently, drugs co-ingested with mitragynine have central nervous system (CNS) activity, complicating the interpretation and specific contribution of kratom. In the data presented here, mitragynine was commonly found in conjunction with opioids such as fentanyl, heroin, and prescription opioids, and since opioids can cause respiratory depression that spans hypoventilation to death, it is difficult to establish a causal link specifically from kratom in cases where elevated concentrations of opioids are also detected. In cases with combined stimulant and mitragynine use, it is equally difficult to delineate the specific contribution of mitragynine, as it has biphasic action with stimulant effects at low doses, and illicit stimulants such as methamphetamine and cocaine are cardiotoxic. Overall, the high rate of mitragynine found in combination with other substances speaks to the polydrug problem that is pervasive in the US [28, 37, 38••].
Pre-analytical Variables
Interpretation of mitragynine blood concentrations in forensic cases is further complicated by pre-analytical variables, such as stability. In one study, mitragynine was found to be relatively stable for 30 days with refrigeration, but a loss of greater than 20% was recorded between 30 and 90 days, so in cases analyzed outside a 30-day window, reported blood concentrations may be artificially low [24••]. Metabolite and oxidative by-product 7-hydroxymitragynine is even more unstable, so much so that it is often omitted from toxicological analysis. Further study has demonstrated that stability of mitragynine and related alkaloids are highly dependent on pH and temperature, even in aqueous specimens [39]. Together, this advocates for caution when interpreting low mitragynine concentrations and evaluation of the specimen collection to testing interval is important.
In the data presented here, only mitragynine was included in the scope of analysis, but Mitragyna speciosa includes a number of alkaloids that can present analytical challenges. The testing described herein does appropriately identify mitragynine and resolve it from its diastereomers [24••], but it does not identify or report other alkaloids present in kratom. Other work expands the scope of toxicology testing to include mitragynine, 7-hydroxymitragynine, speciociliatine, paynantheine, and speciogynine [40] and others also included the kratom alkaloids mitraciliatine and isopaynantheine [33•]. The narrowness in scope of current available toxicological testing is a significant limitation with analytical testing, since identifying and reporting only one target alkaloid does not provide a comprehensive understanding, particularly in light of kratom’s complex pharmacology. Toxicology testing for mitragynine is largely routine in a forensic laboratory setting, but analysis of related kratom alkaloids is limited by the availability of certified reference standards and appropriate analytical methods that chromatographically separate and identify isomers and diastereomers, in addition to their metabolites, after kratom use.
Conclusions
Current Limitations
The pharmacology of kratom is incredibly complex and woefully understudied. With such large gaps in scientific knowledge, coupled with a lack of incorporating kratom alkaloids into routine toxicology testing, it is difficult to make connections to forensic importance. While kratom has demonstrated the potential for therapeutic use to manage pain, OUD, and related withdrawal symptoms, human clinical studies linking detailed use and dosing with comprehensive analytical toxicology testing are lacking. These studies would help forensic toxicological interpretations in cases such as impaired driving or overdose deaths. Current interpretation of mitragynine in a forensic case is subject to a number of confounding factors, including limited chemical stability, appropriate chemical analysis that ensures separation and identification of pertinent alkaloids, the lack of regulation with commercial kratom products and risks of contamination and adulteration, underlying medical conditions, and frequent detection with other substances [37, 39, 41, 42].
Improving the State of the Science
Comprehensive toxicology testing would not only benefit forensic laboratories, but would also benefit clinical investigation of kratom’s potential therapeutic use. Research into specific kratom alkaloid receptor binding is underway, but there is a need to include additional active kratom alkaloids and metabolites [43,44,45]. There have been clinical studies on the pharmacokinetics of kratom use, but they are limited because they do not necessarily account for the ways in which an individual can use kratom products and/or all the different target alkaloids that may exert effects [32, 33•]. Clinical studies would need to focus on the different types of kratom products available, with controlled dosing of teas, tinctures, pills, powders, and other available formulations and with appropriate product regulation and testing. The clinical effects of kratom would also need to document doses that result in stimulant vs opioid effects. Toxicology testing on blood specimens after controlled dosing studies would also be a significant step forward in advancing the interpretation of mitragynine findings in forensic cases, as a blood concentration could be compared against known “therapeutic” concentrations after assessing potential for pre-analytical variables.
Forensic Interpretation of Kratom
Kratom alkaloids are of forensic interest, but the data collected has been mostly limited to mitragynine. Kratom, and the role mitragynine plays in death investigation and impaired driving cases, still needs to be elucidated. The work described herein supports the authors’ initial conclusions that blood mitragynine concentrations of > 1000 ng/mL are more often associated with severe adverse events, up to and including death [24••]. Though kratom-related deaths are low when compared to its widespread use, the denial that kratom use does not result in fatalities is false and misleading. Mitragynine has been confirmed as the sole toxicological finding in overdose deaths and has played a role in other adverse effects, including hepatic injury, seizures, and coma [46,47,48,49,50,51,52]. In addition, there are reports of kratom use leading to dependence and/or addiction resulting in withdrawal symptoms, as well as documented reports of naloxone use for reversal of respiratory depression [53,54,55,56,57].
However, it is worthwhile to note that the majority of reported blood mitragynine concentrations were less than 500 ng/mL, with average and median blood concentrations consistently falling below this concentration. Although there may be an underreporting of kratom-related fatalities with a documented toxicological finding of mitragynine with no other competent cause of death ruled out by autopsy, these cases do appear to be infrequent when compared to cases in which mitragynine is listed in a polysubstance case. In other words, individuals may often not be dying solely due to kratom, but are likely more often dying with kratom in their system, with the caveat that kratom use may be contributory to death.
Kratom clearly has some therapeutic utility, but like all drugs, it is not without harm and the toxicology adage “the dose makes the poison” certainly applies. Though kratom does not appear to be a substance used commonly by itself, users should be better informed regarding its risk profile. This would include informed guidance of dosing of specific products, product regulation and quality standards, and warnings regarding use with other CNS acting drugs. More research is also needed for proper characterization of adverse events, including emergency room admissions and fatalities linked to kratom use, followed by dissemination of that data to health professionals, death investigators, and medical examiners/coroners [17, 29, 38, 58, 59, 60••]. An important recommendation would be specifically linking adverse events after kratom use to “kratom” and not one specific toxicologically confirmed alkaloid. Currently, adverse events are often linked predominantly to mitragynine due to the current state of toxicology testing, but this may be obfuscating the true role of kratom with its significant number of ill-characterized alkaloids and their actions within the human body. The question is really not if kratom can result in toxicity, but rather at what dose and what are the corresponding blood concentrations of target alkaloids. Debate over kratom’s toxicity may continue, but there is certainty that kratom use will persist and maintain a presence in forensic toxicology.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Han C, Schmitt J, Gilliland KM. DARK classics in chemical neuroscience: kratom. ACS Chem Neurosci. 2020;11(23):3870. https://doi.org/10.1021/acschemneuro.9b00535. This article is a good review on the chemical properties, pharmacology, and use of kratom.
Cinosi E, Martinotti G, Simonato P, Singh D, Demetrovics Z, Roman-Urrestarazu A, Bersani FS, Vicknasingam B, Piazzon G, Li JH, Yu WJ, Kapitány-Fövény M, Farkas J, Di Giannantonio M, Corazza O. Following “the roots” of kratom (Mitragyna speciosa): the evolution of an enhancer from a traditional use to increase work and productivity in Southeast Asia to a recreational psychoactive drug in Western countries. Biomed Res Int. 2015;2015:968786. https://doi.org/10.1155/2015/968786.
Eastlack SC, Cornett EM, Kaye AD. Kratom-pharmacology, clinical implications, and outlook: a comprehensive review. Pain Ther. 2020;9(1):55–69. https://doi.org/10.1007/s40122-020-00151-x.
Prozialeck WC, Lamar PC, Krupp M 2nd, Moon M, Phelps LE, Grundmann O. Kratom use within the context of the evolving opioid crisis and the COVID-19 pandemic in the United States. Front Pharmacol. 2021;26(12):729220. https://doi.org/10.3389/fphar.2021.729220.
Grundmann O. Patterns of kratom use and health impact in the US-results from an online survey. Drug Alcohol Depend. 2017;1(176):63–70. https://doi.org/10.1016/j.drugalcdep.2017.03.007.
Garcia-Romeu A, Cox DJ, Smith KE, Dunn KE, Griffiths RR. Kratom (Mitragyna speciosa): user demographics, use patterns, and implications for the opioid epidemic. Drug Alcohol Depend. 2020;1(208):107849.
Smith KE, Dunn KE, Rogers JM, Garcia-Romeu A, Strickland JC, Epstein DH. Assessment of kratom use disorder and withdrawal among an online convenience sample of US adults. J Addict Med. 2022;16(6):666–70.
Brown PN, Lund JA, Murch SJ. A botanical, phytochemical and ethnomedicinal review of the genus Mitragyna korth: implications for products sold as kratom. J Ethnopharmacol. 2017;18(202):302–25. https://doi.org/10.1016/j.jep.2017.03.020.
Sharma A, McCurdy CR. Assessing the therapeutic potential and toxicity of Mitragyna speciosa in opioid use disorder. Expert Opin Drug Metab Toxicol. 2021;17(3):255–7. https://doi.org/10.1080/17425255.2021.1853706.
•• Kruegel AC, Uprety R, Grinnell SG, Langreck C, Pekarskaya EA, Le Rouzic V, Ansonoff M, Gassaway MM, Pintar JE, Pasternak GW, Javitch JA, Majumdar S, Sames D. 7-Hydroxymitragynine is an active metabolite of mitragynine and a key mediator of its analgesic effects. ACS Cent Sci. 2019;5(6):992–1001. https://doi.org/10.1021/acscentsci.9b00141. Demonstrating that 7-hydroxymitragynine is a metabolite of mitragynine and furthers our understanding of kratom’s effects.
Kruegel AC, Grundmann O. The medicinal chemistry and neuropharmacology of kratom: a preliminary discussion of a promising medicinal plant and analysis of its potential for abuse. Neuropharmacology. 2018;134(Pt A):108–20. https://doi.org/10.1016/j.neuropharm.2017.08.026.
León F, Obeng S, Mottinelli M, Chen Y, King TI, Berthold EC, Kamble SH, Restrepo LF, Patel A, Gamez-Jimenez LR, Lopera-Londoño C, Hiranita T, Sharma A, Hampson AJ, Canal CE, McMahon LR, McCurdy CR. Activity of Mitragyna speciosa (“kratom”) alkaloids at serotonin receptors. J Med Chem. 2021;64(18):13510–23.
Obeng S, Kamble SH, Reeves ME, Restrepo LF, Patel A, Behnke M, Chear NJ, Ramanathan S, Sharma A, León F, Hiranita T, Avery BA, McMahon LR, McCurdy CR. Investigation of the adrenergic and opioid binding affinities, metabolic stability, plasma protein binding properties, and functional effects of selected indole-based kratom alkaloids. J Med Chem. 2020;63(1):433–9.
•• Kamble SH, León F, King TI, Berthold EC, Lopera-Londoño C, Siva Rama Raju K, Hampson AJ, Sharma A, Avery BA, McMahon LR, McCurdy CR. Metabolism of a kratom alkaloid metabolite in human plasma increases its opioid potency and efficacy. ACS Pharmacol Transl Sci. 2020;3(6):1063–8. https://doi.org/10.1021/acsptsci.0c00075. This research of a mitragynine metabolite that is a potent MOR agonist could help explain kratom’s pharmacology and psychoactive properties.
• Váradi A, Marrone GF, Palmer TC, Narayan A, Szabó MR, Le Rouzic V, Grinnell SG, Subrath JJ, Warner E, Kalra S, Hunkele A, Pagirsky J, Eans SO, Medina JM, Xu J, Pan YX, Borics A, Pasternak GW, McLaughlin JP, Majumdar S. Mitragynine/corynantheidine pseudoindoxyls as opioid analgesics with Mu agonism and delta antagonism, which do not recruit β-arrestin-2. J Med Chem. 2016;59(18):8381–97. https://doi.org/10.1021/acs.jmedchem.6b00748. An important paper on the MOR pharmacology of Mitragyna alkaloids.
Wade P. Bentuangie Kratom Strains & Their Effects [Internet]. Kratom.org. 2022. [cited 29 November 2022] Available from: kratom.org/strains/bentuangie
Eggleston W, Stoppacher R, Suen K, Marraffa JM, Nelson LS. Kratom use and toxicities in the United States. Pharmacotherapy. 2019;39(7):775–7. https://doi.org/10.1002/phar.2280.
Leong Bin Abdullah MFI, Singh D. The adverse cardiovascular effects and cardiotoxicity of kratom (Mitragyna speciosa Korth.): a comprehensive review. Front Pharmacol. 2021;27(12):726003. https://doi.org/10.3389/fphar.2021.726003.
Stringer J, Welsh C, Tommasello A. Methadone-associated Q-T interval prolongation and torsades de pointes. Am J Health Syst Pharm. 2009;66(9):825–33. https://doi.org/10.2146/ajhp070392.
Smith KE, Lawson T. Prevalence and motivations for kratom use in a specimen of substance users enrolled in a residential treatment program. Drug Alcohol Depend. 2017 Nov;1(180):340–8. https://doi.org/10.1016/j.drugalcdep.2017.08.034.
Weiss ST, Douglas HE. Treatment of kratom withdrawal and dependence with buprenorphine/naloxone: a case series and systematic literature review. J Addict Med. 2021;15(2):167–72. https://doi.org/10.1097/ADM.0000000000000721.
Broyan VR, Brar JK, Allgaier Student T, Allgaier JT. Long-term buprenorphine treatment for kratom use disorder: a case series. Subst Abus. 2022;43(1):763–6.
Smith KE, Dunn KE, Epstein DH, Feldman JD, Garcia-Romeu A, Grundmann O, Henningfield JE, McCurdy CR, Rogers JM, Schriefer D, Singh D, Weiss ST. Need for clarity and context in case reports on kratom use, assessment, and intervention. Subst Abus. 2022;43(1):1221–4.
•• Papsun DM, Chan-Hosokawa A, Friederich L, Brower J, Graf K, Logan B. The trouble with kratom: analytical and interpretative issues involving mitragynine. J Anal Toxicol. 2019;43(8):615–29. https://doi.org/10.1093/jat/bkz064. This paper constitutes the largest dataset of mitragynine in forensic toxicology casework.
Bourgine J, Garnier-Jardin C, Chrétien B, Le Boisselier R, Loilier M, Lelong-Boulouard V, et al. Fatal intoxication with kratom: a case report. Toxicologie Analytique et Clin. 2019;31:S36–7.
• Wang C, Walker AE. Fatal mitragynine-associated toxicity in Canada: a case report and review of the literature. Acad Forensic Pathology. 2019;8:340–6. Case report with elevated mitragynine blood concentration and mitragynine is primarily implicated
• Matson M, Schenk N. Fatality of 33-year-old man involving kratom toxicity. J Forensic Sci. 2019;64:1933–5. Case report with elevated mitragynine blood concentration and mitragynine is primarily implicated
• Mata DC, Andera KM. Case series: mitragynine blood and tissue concentrations in fatalities from 2017 to 2018 in Orange County, CA, USA. Forensic. Chemistry. 2020;17:100205. Case series of cases involving mitragynine with more detail
•• Gershman K, Timm K, Frank M, Lampi L, Melamed J, Gerona R, et al. Deaths in Colorado attributed to kratom. New England J Med. 2019;380:97–8. Case series of cases involving mitragynine with more detail
• Behonick GS, Vu C, Czarnecki L, El-Ters M, Shanks KG. Two single-drug fatal intoxications by mitragynine. J Anal Toxicol. 2022;46(5):e110–4. https://doi.org/10.1093/jat/bkac016. Case report with elevated mitragynine blood concentration and mitragynine is listed in COD
• Trakulsrichai S, Sathirakul K, Auparakkitanon S, Krongvorakul J, Sueajai J, Noumjad N, et al. Pharmacokinetics of mitragynine in man. Drug Des, Dev Ther. 2015;9:2421–9. An important paper on one of the few pharmacokinetic studies of kratom use in humans
Grundmann O. Patterns of kratom use and health impact in the US-results from an online survey. Drug Alcohol Depend. 2017;1(176):63–70.
• Tanna RS, Nguyen JT, Hadi DL, Manwill PK, Flores-Bocanegra L, Layton ME, et al. Clinical pharmacokinetic assessment of Kratom (Mitragyna Speciosa), a botanical product with opioid-like effects, in healthy adult participants. Pharmaceutics. 2022;14:620. An important paper on one of the few pharmacokinetic studies of kratom use in humans
• Chadchoy P, Sinchai T. The relationship between Mitragynine blood concentrations and death in Thailand. Interdiscip Res Rev. 2020;15:18–21. An important paper reporting blood mitragynine concentrations in non-pathological causes of death
Brower J. Mitragynine-only deaths in North Carolina. In: Society of Forensic Toxicologists Annual Conference. Society of Forensic Toxicologists; 2022.
Karinen R, Fosen JT, Rodge S, Vindenes V. An accidental poisoning with mitragynine. Forensic Sci Int. 2014;245:e29–232.
O’Malley Olsen E, O’Donnell J, Mattson CL, Schier JG, Wilson N. Unintentional drug overdose deaths with kratom detected – 27 states, July 2016-December 2017. Morbid Mortal Weekly Rep. 2019;68(14):326–7.
•• Schmitt J, Bingham K, Knight L. Kratom-associated fatalities in northern Nevada – what mitragynine level is fatal? Am J Forensic Med Pathol. 2021;42(4):341–9. Case series of cases involving mitragynine with more detail
Basiliere S, Kerrigan S. Temperature and pH-dependent stability of mitragyna alkaloids. J Anal Toxicol. 2020;44:314–24. https://doi.org/10.1093/jat/bkz103.
Basiliere S, Brower J, Winecker R, Friederich L, Kerrigan S. Identification of five mitragyna alkaloids in blood and tissues using liquid chromatography-quadrupole/time-of-flight mass spectrometry. Forensic Toxicol. 2020;38:420–35. https://doi.org/10.1007/s11419-020-00537-8.
Nacca N, Schult RF, Li L, Spink DC, Ginsberg G, Navarette K, et al. Kratom adulterated with phenylethylamine and associated intracerebral hemorrhage: linking toxicologists and public health officials to identify dangerous adulterants. J Med Toxicol: Official J Am College Med Toxicol. 2020;16:71–4.
Hoonwijit U, Waithum K, Tansrisawad N. Comparison of mitragynine stability in human blood in common blood collection tubes. Chulalongkorn Med J. 2020;64:439447.
Takayama H. Chemistry and pharmacology of analgesic indole alkaloids from the rubiaceous plant, mitragyna speciosa. Chem Pharm Bull. 2004;52(8):916–28.
Hanapi NA, Chear NJY, Azizi J, Yusof SR. Kratom alkaloids: interactions with enzymes. Front Pharmacol. 2021;17(12):751656.
Henningfield JE, Rodricks JV, Manguson AM, Huestis MA. Respiratory effects of oral mitragynine and oxycodone in a rodent model. Psychopharmacology. 2022;239(12):3793–804.
Kapp F, Maurer H, Auwärter V, Winkemann M, Hermanns-Clausen M. Intrahepatic cholestasis following abuse of powdered kratom (mitragyna speciosa). J Med Toxicol. 2011;7:227–31.
Nelsen JL, Lapoint J, Hodgman MJ. Seizure and coma following kratom (mitragynine speciosa korth) exposure. J Med Toxicol. 2020;6:424–6.
Dorman C, Wong M, Khan A. Cholestatic hepatitis from prolonged kratom use: a case report. Hepatology. 2015;61(3):1086–7.
Tayabeli K, Bolzon C, Foster P, Patel J, Kalim MO. Kratom: a dangerous player in the opioid crisis. J Community Hosp Intern Med Perspect. 2018;8(3):107–10.
Afzal H, Esang M, Rahman S. A case of kratom-induced seizures. Cureus. 2020;12:e6588.
Ahmad J, Odin JA, Hayashi PH, Fontana RJ, Conjeevaram H, Avula B, et al. Liver injury associated with kratom, a popular opioid-like product: experience from the U.S. drug induced liver injury network and a review of the literature. Drug Alcohol Depend. 2021;1(218):108426. https://doi.org/10.1016/j.drugalcdep.2020.108426.
Schimmel J, Dart RC. Kratom (Mitragyna Speciosa) liver injury: a comprehensive review. Drugs. 2020;80:263–83.
Singh D, Narayanan S, Müller CP, Swogger MT, Rahim AA, Leong Bin Abdullah MFI, et al. Severity of kratom (Mitragyna speciosa Korth.) psychological withdrawal symptoms. J Psychoact Drugs. 2018;50:445–50.
Overbeek DL, Abraham J, Munzer BW. Kratom (Mitragynine) ingestion requiring naloxone reversal. Clin Pract Cases Emerg Med. 2019;3:24–6.
Stanciu CN, Gnanasegaram SA, Ahmed S, Penders T. Kratom withdrawal: a systematic review with case series. J Psychoact Drugs. 2019;51:12–8.
Assangkornchai S, Muekthong A, Sam-Angsri N, Pattanasttayawong U. The use of mitragynine speciosa (“krathom”), an addictive plant in Thailand. Subst Use Misuse. 2007;24(14):2145–57.
McWhirter L, Morris S. A case report of inpatient detoxification after kratom (mitragyna speciosa) dependence. Eur Addict Res. 2010;16(4):229–31.
Cumpston KL, Carter M, Wills BK. Clinical outcomes after Kratom exposures: a poison center case series. Am J Emerg Med. 2018;36:166–8.
Post S, Spiller HA, Chounthirath T, Smith GA. Kratom exposures reported to United States poison control centers: 2011-2017. Clin Toxicol (Phil). 2019;57:847–54.
•• Corkery JM, Streete P, Claridge H, Goodair C, Papanti D, Orsolini L, et al. Characteristics of deaths associated with kratom use. J Psychopharmacol (Oxford, England). 2019;33:1102–23. [High level review of mitragynine involvement in fatalities]
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papsun, D., Schroeder, W., Brower, J. et al. Forensic Implications of Kratom: Kratom Toxicity, Correlation with Mitragynine Concentrations, and Polypharmacy. Curr Addict Rep 10, 272–281 (2023). https://doi.org/10.1007/s40429-023-00477-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00477-4