Abstract
Introduction
Kratom is derived from the plant Mitragyna speciosa which is indigenous to Southeast Asia. Active compounds, mitragynine and 7-hydroxymitragynine, cause mild stimulant and opioid agonist effects. Although reported to have potential benefits in the treatment of opioid use disorder, efficacy remains uncertain while adverse health effects have been reported. A compounding concern is the presence of adulterants given that this is an unregulated product.
Case Details
A 54-year-old fitness instructor who used an online purchased kratom product regularly for one year developed stimulatory effects and suffered a large hemorrhagic stroke with a close temporal relationship to ingestion of a different kratom product from the one he regularly used. A collaborative investigation by medical toxicologists, a regional poison center, the state public health laboratory, and public health officials determined that his new kratom product was adulterated with phenylethylamine (PEA).
Discussion
We report a case of PEA adulterated kratom purchased and used with resultant adverse effects. PEA is structurally similar to amphetamine and is known to produce sympathomimetic effects. It is possible the stimulatory effect of PEA resulted in a marked and transient increase in blood pressure resulting in hemorrhagic stroke.
Conclusion
Medical toxicologists should form working relationships with laboratories and public health officials to aid in early identification of adulterated products that carry risk to the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
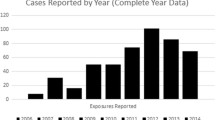
Kratom is an unregulated herbal supplement in the United States (US) prepared from the leaves of the Southeast Asian plant, Mitragyna speciosa. It has been used for centuries in Southeast Asia for its stimulant and opioid properties [1]. Kratom is posited as a safe and effective alternative for treatment of opioid use disorder (OUD), a use which has raised concerns by the US FDA and others [2, 3]. Its use has been increasing in the US [4]. Efficacy and potential adverse effects remain largely unknown [5, 6]. We report a case of hemorrhagic stroke associated with phenylethylamine (PEA)-adulterated kratom.
Case Details
A 54-year-old male, with a past medical history of hepatitis C with curative treatment, alcohol use disorder, and OUD, presented to the hospital with his partner due to altered mental status. It was reported that he obtained a kratom product online, “Kratom Crazy®,” and ingested 2–3 teaspoons daily for about 1 year. The patient worked as a fitness instructor and used the supplement for purported general health benefits, denying knowledge of any opioid properties. He purchased a different product, “Vivazen Botanicals Maeng Da Kratom®,” and mixed one teaspoon of powder with water and noticed an unusually bitter taste. Approximately 15 minutes after his first dose, he complained of headache and vomited. He went to sleep and awoke after several hours with incomprehensible speech.
On arrival to the hospital, physical examination revealed blood pressure 120/70 mmHg, heart rate 70 beats/minute, respiratory rate 18 breaths/minute, temperature 36.8 °C, and oxygen saturation 98% on room air. He appeared uncomfortable and provided nonsensical answers to questions without other neurological deficits. Electrocardiogram was unremarkable. Serum chemistry was unremarkable including glucose 124 mg/dL. He had a leukocytosis of 15.0 Th/mm3. Assays for alcohol, acetaminophen, and salicylates were negative. A high-sensitivity troponin T was slightly elevated at 91 ng/L (reference range 0–22 ng/L). Computed tomography of the head revealed a large right frontal intraparenchymal hemorrhage with intraventricular extension into the lateral and fourth ventricles measuring 40 cm3 with mass effect. The patient was transferred to an academic medical facility.
On arrival, the patient became increasingly encephalopathic and was intubated. A comprehensive urine drug screening for 289 pharmaceutical and recreational drugs utilizing immunoassay and liquid chromatography-mass spectrometry did not reveal positive results other than medications administered for his care. This assay does not detect mitragynine or phenylethylamine. Magnetic resonance imaging revealed stable intraparenchymal hemorrhage with 7-mm midline shift and subfalcine herniation (Fig. 1). Emergent craniotomy and evacuation of intraparenchymal clot with intraventricular drain placement were completed on hospital day (HD) 2. The serum concentration of mitragynine measured by liquid chromatography/tandem mass spectrometry at a reference laboratory was 340 ng/mL on HD 3. The patient was extubated on HD 8 and discharged neurologically intact on HD 12. Prior to discharge, the patient underwent buprenorphine induction with referral to outpatient chemical dependency treatment for underlying OUD. He remained neurologically intact on follow-up 2 months after discharge.
In conjunction with the regional poison center, the state laboratory (Wadsworth Center) and public health officials were contacted at the time of toxicology consultation to coordinate retrieval and analysis of the samples. A weeklong field investigation revealed that the retailer received customer feedback that the Vivazen Kratom® product was “very strong” prompting the corporate retailer to voluntarily remove it from stores.
The family provided samples of Vivazen Kratom® and Kratom Crazy® products. An unopened sample of Vivazen Kratom® was also obtained. Solvent extracts of the three samples were analyzed by liquid chromatography-tandem high-resolution mass spectrometry (LC-HRMS/MS) using a Shimadzu HPLC interfaced with a Sciex 6600 TripleTOF tandem mass spectrometer. The full-scan high-resolution data obtained were used to query databases. This led to the identification of PEA in Vivizen Kratom®.
An early-eluting HPLC peak that was present in Vivazen Kratom® but not in Kratom Crazy® showed an apparent [M + H]+ ion at m/z 122.0962, which is in agreement with the theoretical m/z of the [M + H]+ ion of PEA, 122.0964. The m/z value of the major fragment ion, [M + H-NH3]+, was 105.0700, which is likewise in agreement with that of the theoretical value of 105.0699. Upon procurement of a PEA standard (Sigma), the presence of PEA was confirmed by analysis of accurate mass, isotopic abundance, fragmentation, and HPLC retention time. A quantitative LC-HRMS/MS method was developed and utilized to measure PEA in the products. Vivazen Kratom® used by the patient was contained 16.3% PEA by mass and the unopened Vivazen Kratom® contained 15.1% PEA. The Vivazen Kratom® label did not list PEA as an ingredient. PEA was not detected in Kratom Crazy® (< 0.01%). Consent for publication of this case was obtained and provided to the journal in accordance with JMT policy.
Discussion
We report a case of hemorrhagic stroke associated with PEA-adulterated kratom. Although the stimulatory effects of kratom are reported, hemorrhagic stroke has not been associated with kratom use alone [4, 5]. PEA causes rapid and transient stimulatory effects including hypertension [7, 8] and intracranial hemorrhage after exposure to PEA or its derivatives are reported [9,10,11,12]. PEA remains an unscheduled substance without restrictions on its inclusion in supplements. The patient had a measurable mitragynine concentration; however, the range of toxicity has not been well established, with deaths having been reported in association with postmortem concentrations of 1060 ng/mL and 2500 ng/mL [13].
Our case highlights the importance of collaborative relationships among medical toxicologists, regional poison centers, public health laboratories, and health department officials that were critical to this adulterant identification. The regional poison center played a pivotal role in linking clinical toxicologists with the state laboratory and public health officials. Clinical teams often have limited laboratory resources to obtain an extensive analysis of unregulated herbal products and their potential adulterants. While capabilities may vary, public health laboratories may assist in these instances.
In this case, emergency physicians consulted medical toxicologists who suspected adulteration based on atypical findings of intracranial hemorrhage with kratom use. The regional poison center was contacted by the consulting toxicologists to inquire about the existence of other similar cases reported to the poison center. After a discussion with the poison center, the state Department of Health (DOH) was contacted due to concern of a larger public health issue. This resulted in numerous communications with the DOH, treating providers and poison center and the Wadsworth lab. These communications prompted further investigation and transfer of the consumed product and additional samples from store shelves to the state laboratory for analysis. In addition to the identification of the adulterant, the poison center created a case-based definition to identify any calls in real-time, and a notification was sent to the toxicologists at the poison center. If an anomaly were to arise based on this surveillance, the poison center would be able to alert the DOH for further investigation. The state department of health collected additional samples and evidence in order to determine if a market withdrawal of a potentially contaminated product was necessary. During the investigation, it was identified that the retailer had removed the product from sale due to other customer complaints. This retailer’s action obviated the need for an emergency order to be issued by the department of health to retailers prohibiting the sale and prompt removal. Such an order was issued for synthetic marijuana products in response to a 2011–2012 outbreak which resulted in acute illness and hospitalization of many patients.
The report is not without limitations in that the “comprehensive” urine drug screening assay available does not detect a great many xenobiotics of potential interest. The adulterant PEA was only detected in the product sample after the time of patient care; therefore, biological samples were not assayed for the adulterant. There is the possibility that the adulteration is an anomaly; however, three additional independently obtained samples were acquired from the manufacturer and all were found to contain the adulterant.
Conclusion
We report an intracranial hemorrhage temporally associated with ingestion of a publicly sold kratom product adulterated with PEA. The case progression highlights the importance of medical toxicologists working closely with the state laboratory and public health officials to identify commercial products that may be dangerous to the public. This type of collaboration may facilitate early identification of contamination and adulteration, and allow for a prompt and robust public health response.
Abbreviations
- US:
-
United States
- ICU:
-
Intensive care unit
- OUD:
-
Opioid use disorder
- PEA:
-
Phenylethylamine
References
Cinosi E, Martinotti G, Simonato P, et al. Following “the Roots” of kratom (Mitragyna speciosa): the evolution of an enhancer from a traditional use to increase work and productivity in Southeast Asia to a recreational psychoactive drug in Western countries. Biomed Res Int. 2015;2015:968786.
USFDA 2018: FDA objects to kratom compound intended for use as an alternative to prescription opioids and promoted with unproven claims to treat addiction. Available at: https://www.fda.gov/NewsEvents/Newsroom/FDAInBrief/ucm598389.htm.
Smid MC, Charles JE, Gordon AJ, Wright TE. Use of kratom, an opioid-like traditional herb, in pregnancy. Obstet Gynecol. 2018;132(4):926–8.
Post S, Spiller HA, Chounthirath T, Smith GA. Kratom exposures reported to United States poison control centers: 2011-2017. Clin Toxicol. 2019.
White CM. Pharmacologic and clinical assessment of kratom. Am J Health Syst Pharm. 2018;75:261–7.
Tayabali K, Bolzon C, Foster P, Patel J, Kalim MO. Kratom: a dangerous player in the opioid crisis. J Community Hosp Intern Med Perspect. 2018;8:107–10.
Liang CS, Sprecher D. Cardiovascular actions of beta-phenylethylamine. Am J Phys. 1979;236(4):H592–5.
Broadley KJ. The vascular effects of trace amines and amphetamines. Pharmacol Ther. 2010;125:363–75.
Cohen PA, Zeijlon R, Nardin R, Keizers PH, Venhuis B. Hemorrhagic stroke probably caused by exercise combined with a sports supplement containing β-methylphenyl-ethylamine (BMPEA): a case report. Ann Intern Med. 2015;162:879–80.
Wijers CHW, Visser MC, van Litsenburg RTH, Niesink RJM, Willemse RB, Croes EA. Haemorrhagic stroke related to the use of 4-fluoroamphetamine. J Neurol. 2018;265:1607–11.
Harris BF, Winn C, Ableman TB. Hemorrhagic stroke in a young healthy male following use of pre-workout supplement Animal Rage XL. Mil Med. 2017;182(10):e2030–3.
Lappin JM, Darke S, Farrell M. Stroke and methamphetamine use in young adults: a review. J Neurol Neurosurg Psychiatry. 2017;88:1079–91.
Wang C, Walker AE. Fatal mitragynine-associated toxicity in Canada. Acad For Pathol. 2018;8(2):340–6. https://doi.org/10.1177/1925362118782076.
Sources of Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent for publication of this case was obtained from the patient and family and provided to the journal in accordance with JMT policy.
Conflicts of Interest
None.
Additional information
Supervising Editor: Andis Graudins, MB BS, PhD
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nacca, N., Schult, R.F., Li, L. et al. Kratom Adulterated with Phenylethylamine and Associated Intracerebral Hemorrhage: Linking Toxicologists and Public Health Officials to Identify Dangerous Adulterants. J. Med. Toxicol. 16, 71–74 (2020). https://doi.org/10.1007/s13181-019-00741-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-019-00741-y