Abstract
Suspected unnatural or unexpected deaths in the Northern Territory of Australia are reportable to the coroner, and investigation of such cases typically includes a post-mortem examination with comprehensive toxicological screening. An autopsy case series of five Cumyl-PEGACLONE-related fatalities over a recent eighteen-month period is presented. Databases of the Northern Territory coroner’s office and the Royal Darwin Hospital Forensic Pathology Unit were searched to identify deaths related to synthetic cannabis use between July 1, 2018 and December 31, 2020. Toxicological analysis was performed at Forensic Science South Australia using a combination of liquid chromatography, gas chromatography and mass spectrometry. Cumyl-PEGACLONE, a synthetic cannabinoid receptor agonist (SCRA) with a gamma-carbolinone core, was detected in five cases (range in post-mortem blood 0.73—3.0 μg/L). Concurrent alcohol use and underlying cardiovascular disease were considered relevant factors in most cases. Toxicological Significance Scoring was carefully considered in all five cases, and in four cases, the presence of Cumyl-PEGACLONE was considered to be highly significant (TSS = 3). Synthetic cannabis use has not previously been identified in Northern Territory drug trends, and only one fatality related to the use of gamma-carbolines was identified in a recent Australia-wide study on synthetic cannabinoid-related fatalities. Deaths related to Cumyl-PEGACLONE use are emerging in the Northern Territory of Australia; this has public health implications. Although the exact mechanism(s) of death related to Cumyl-PEGACLONE are not fully established, this additional descriptive case series reaffirm an association with underlying cardiovascular disease, and suggest that concurrent use with alcohol may be relevant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Northern Territory (NT) is a federal territory in the central and northern regions of Australia. It is a sparsely populated region with a population of approximately 250,000, which is less than 1% of Australia’s population [1]. Suspected unnatural or unexpected deaths are reportable to the coroner, and medico-legal investigation of such cases typically includes a post-mortem examination with comprehensive toxicological screening. An autopsy case series of five Cumyl-PEGACLONE-related fatalities seen at Royal Darwin Hospital (RDH) Forensic Pathology Unit over a recent eighteen-month period is presented.
Methods
Databases of the NT Coroner’s Office and the RDH Forensic Pathology Unit were searched to identify all deaths where synthetic cannabinoids were detected over an eighteen-month period (July 1, 2018 – December 31, 2019). Copies of the coroner’s findings, post-mortem reports, contemporaneous notes, hospital records and collateral information filed in the archives at the NT coroner’s office and the RDH Forensic Pathology Unit, were retrieved and studied.
Toxicological analysis was performed at Forensic Science South Australia using a combination of liquid chromatography, gas chromatography and mass spectrometry [2], with quantitative validation of Cumyl-PEGACLONE as previously described [3].
Data-analysis was performed by the authors. All data was treated confidentially. Ethics approval was obtained from the Human Research Ethics Committee of the NT Department of Health and Menzies School of Health Research (Ref. no. HREC 2020–3718) and permission for this research was granted by the NT Coroner’s Office. The Toxicological Significance Score (TSS) for each case was first assessed by each of the authors individually (3 forensic pathologists and 1 toxicologist), with a consensus score then assigned.
Results
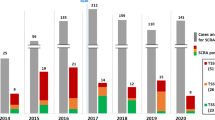
Over the eighteen-month period, 472 deaths were reported to the NT coroner. In five cases, Cumyl-PEGACLONE, a synthetic cannabinoid receptor agonist (SCRA) with a gamma-carbolinone core, was detected (range in post-mortem blood 0.73—3.0 μg/L). Toxicological Significance Scoring (TSS), a system developed by Elliott et al. to perform a health risk assessment of new psychoactive substances and to allow the clarification of the role of such substance(s) in deaths [4], was carefully considered in all five cases. A score from 1 (Low, alternative cause of death) to 3 (High, substance likely to have contributed to toxicity or death despite the detection of other drugs) is assigned. In this series, the presence of Cumyl-PEGACLONE was considered to be highly significant in four cases (TSS = 3).
The decedents in all five cases were male, with an age range of 31 years to 51 years (mean age = 41 years). Four deaths occurred at urban locations (one at a correctional facility) and one death at a remote location.
Case descriptions (summaries provided in Table 1)
Case 1
A 51-year-old male was found slumped and unresponsive at a bus stop in an urban location. A history of excessive alcohol use, bronchiectasis, hypertension, and hypercholesterolemia was known.
The main autopsy findings (post-mortem interval of 4 days) included an average body-build (body mass index = 25 kg/m2), slight cardiomegaly with four chamber dilation (heart weight = 392 g; predicted heart weight = 336 g [5]), coronary artery ectasia and left lung bronchiectasis. Histological examination confirmed concentric atherosclerotic fibrosis with extensive calcifications. No myocardial ischemia was evident. Toxicological analysis (post-mortem iliac vein blood) showed a blood alcohol concentration of 0.27%, and Cumyl-PEGACLONE at a concentration of 0.73 μg/L.
The cause of death was ascribed to the combined toxic effects of alcohol and Cumyl-PEGACLONE, in the context of coronary artery atherosclerosis (TSS = 3).
Case 2
A 50-year-old male was witnessed collapsing following a verbal altercation outside a shopping centre in an urban location; resuscitation was attempted. A hand-rolled cigarette butt was found in the decedent’s vicinity; subsequent testing indicated that it contained Cumyl-PEGACLONE. There was no available information on previous drug use, and the decedent did not have any known underlying medical conditions.
Main autopsy findings (post-mortem interval of 1 day) included an underweight body (body mass index of 17 kg/m2), macroscopically normal heart (heart weight = 252 g; predicted heart weight = 276 g [5]) and no overt macro- or microscopic pathology. Toxicological analysis (post-mortem iliac vein blood) showed a blood alcohol concentration of 0.24%, and Cumyl-PEGACLONE at a concentration of 3 μg/L.
The cause of death was acute drug toxicity resulting from alcohol and Cumyl-PEGACLONE use (TSS = 3).
Case 3
The body of a 31-year-old adult male was found inside his locked cell at a correctional facility. Herbal material was located inside the cell, and fellow inmates reported that the decedent was known to “pass out” on occasion when smoking “Kronic” (synthetic cannabis). No significant background medical history was known.
Autopsy (post-mortem interval of 1 day) showed the body of an obese male (body mass index = 37 kg/m2), macroscopically normal heart (heart weight = 395 g; predicted heart weight = 418 g [5]), and features of positional asphyxia, with intense congestion of the face and neck, numerous cutaneous petechiae over the face, chest, arms and legs, and intense scleral congestion and confluent scleral hemorrhages.
Toxicological analysis (post-mortem iliac vein blood) showed Cumyl-PEGACLONE at a concentration of 0.8 μg/L. Cumyl-PEGACLONE was also detected in a liver sample; 5F-Cumyl-P7AICA and 5F-Cumyl-PEGACLONE were detected in the pubic hair. Alcohol was not detected. The herbal material found in the cell was confirmed to contain Cumyl-PEGACLONE.
Death was attributed to positional asphyxia in the context of synthetic cannabis use and obesity (TSS = 3).
Case 4
A 33-year-old male was found “passed out” on the streets at an urban location, thought to be alcohol intoxicated. Resuscitation was unsuccessful. Past medical history comprised latent tuberculosis, dyslipidemia, chronic alcohol use, and cannabis smoking; the decedent had presented to the local emergency department on numerous occasions with chest pain following the smoking of cannabis.
Autopsy (post-mortem interval of 3 days) showed an average body build (body mass index = 23 kg/m2), macroscopically normal heart (heart weight = 317 g; predicted heart weight = 322g [5]), and a mild to moderate degree of coronary artery atherosclerosis. Extensive acute myocardial ischemic changes (pale, circumscribed areas ranging between 5 mm – 13 mm in diameter) were seen in an unusual, non-specific, patchy distribution involving the anterior, lateral and posterior walls of the left ventricle and the interventricular septum (See Figs. 1 and 2).
Toxicological analysis (post-mortem iliac vein blood) showed a blood alcohol concentration of 0.24%, and 2 μg Cumyl-PEGACLONE per L.
Death was attributed to acute myocardial ischaemia resulting from coronary artery atherosclerosis, Cumyl-PEGACLONE use, and alcohol use (TSS = 3).
Case 5
A 39-year-old male was witnessed collapsing in the street at a remote location (Bathurst Island); resuscitation was unsuccessful. The decedent was known to smoke synthetic cannabis, named “Cheeky One”, and reportedly intermittently smoked this substance in the days leading up to death. A non-specific history of “mental health issues” and “heart problems” was reported.
Autopsy findings (post-mortem interval of 3 days) included an average body build (body mass index = 24 kg/m2), cardiomegaly (heart weight = 454 g; predicted heart weight = 354g [5]), extensive left ventricular myocardial fibrosis, and advanced multi-vessel coronary artery atherosclerosis.
Toxicological analysis (post-mortem iliac vein blood) showed 1 μg Cumyl-PEGACLONE per L, 1.2 mg lignocaine per L, 8 μg Paliperidone per L, 14 μg delta-9-tetrahydrocannabinol per L, and 11-nor-9-carboxy-delta-9-tetrahydrocannabinol. No alcohol was present.
The cause of death was ischemic heart disease due to coronary artery atherosclerosis in the context of Cumyl-PEGACLONE use (TSS = 1).
Discussion
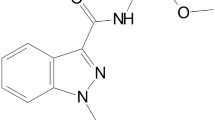
Cumyl-PEGACLONE is a synthetic cannabinoid receptor agonist (SCRA) with a gamma-carbolinone core structure that has dominated the German synthetic cannabinoid market since its first detection [6]. The laws surrounding the use and possession of new psychoactive substances in Australia are complex and vary between complete to specific banning in Australian jurisdictions [7]. In the Northern Territory, the use of some SCRAs is prohibited, with Cumyl-PEGACLONE only recently included in the Misuse of Drugs Act Amendment Regulations [8].
In this case series, five recent deaths related to Cumyl-PEGACLONE were identified in a small population, over eighteen months, including deaths at a correctional facility and at a remote location, indicating the availability of Cumyl-PEGACLONE in diverse populations, and associated public health implications.
A study of drug trends in the Northern Territory from 2014 – 2018 showed that morphine and methamphetamine were the most frequently reported drugs of choice, with an increase in the popularity of methamphetamine. Reported cannabis use was stable over this period, with hydroponic cannabis the form most commonly and most often used. Synthetic cannabis use was not identified as a trend [9]. Furthermore, in a recent Australia-wide study on synthetic cannabinoid-related fatalities, the use of gamma-carbolines (Cumyl-PEGACLONE) was only identified in one fatality [10], however no other information was provided for that case.
Cumyl-PEGACLONE has originally been reported to be a “comparatively safe new synthetic cannabinoid receptor agonist” [11]; however since then, deaths related to its fluorinated analogue, 5F-Cumyl-PEGACLONE, have been described [6, 10, 12], and more data is becoming available, suggesting that its use is not safe and death may result when a sufficient dose is taken, particularly in the context of underlying natural disease, or concurrent use of other drugs. A recent article by Janssens et al. demonstrated that Cumyl-PEGACLONE has the same CB1 receptor activation potential (in vitro) as its 5-fluorinated analogue [13]. There may, however, be other factors which influence toxicity in vivo and a consideration of the circumstances in each case is important.
The deaths described in this series share the most common characteristics of SCRA-related fatalities described by others [6, 10] of accidental drug toxicity, with a male preponderance, clinical presentation of sudden collapse, and association with underlying cardiovascular disease. The concurrent use of alcohol appeared to be relevant in three of our cases (range 0 – 0.27%), which corresponds with the findings of other authors investigating the characteristics and circumstances of synthetic cannabinoid related deaths [10], where alcohol was present in about a third of cases (range 0.014 – 0.271%).
In a case series on four deaths related to the use of 5F-Cumyl-PEGACLONE, the fluorinated analogue of Cumyl-PEGACLONE, also a potent CB1 receptor agonist, the decedents were reportedly found deceased at their residence(s), including a prison cell in one case, with no witness descriptions available of the decedents’ behavior prior to their collapse [6]. In two of our cases (cases 2 and 5), the involved individuals displayed noticeably agitated behavior prior to their collapse. Intense agitation prior to death related to synthetic cannabis use has also been described in other reports [10].
Little is known about either the toxicology or histopathology of Cumyl-PEGACLONE and other synthetic cannabinoids. Concentrations measured post-mortem may bear little relation to what they were at the time of death, as we have no way to distinguish whether the drug we are measuring is just drug stored in adipose tissue previously. It also makes the designation of “toxic” concentrations nearly impossible. The post-mortem interval ranged between 1 to 6 days in this case series which further complicates interpretation of “toxic” levels, with a lack of data on post-mortem redistribution.
Post-mortem Cumyl-PEGACLONE concentrations are not readily available in the literature. In this case series, Cumyl-PEGACLONE was detected in preserved post-mortem iliac vein blood at a range of 0.73 μg/L—3 μg/L. Halter et al. reported the concentrations of 27 cases of fatal and non-fatal intoxications associated with the consumption of Cumyl-PEGACLONE [11]. In their case series, Cumyl-PEGACLONE concentrations ranged between 0.12 ng/mL to 13 ng/mL for all cases (fatal and non-fatal intoxications), and between 0.12 ng/mL to 0.84 ng/mL for fatal intoxications. Very limited details about the cases and interpretation of the autopsy findings and toxicology results are provided in their report.
TSS was carefully considered by the authors in all five cases, and consensus scores were assigned. In four of the five cases, the presence of Cumyl-PEGACLONE was considered a likely contributor to the cause of death (TSS = 3), even in the presence of other conditions and/or drugs, however in no case was Cumyl-PEGACLONE toxicity considered the sole cause of death. It is recognized that death likely occurred where a sufficient dose has been taken in a specific context that renders the individual vulnerable, such as the presence of alcohol and/or underlying cardiovascular disease.
The history of chronic alcohol misuse in cases 1 and 4, and the high blood alcohol concentrations in cases 1, 2, and 4 complicated the speculation on the mechanism of death in these cases, and the exact contribution of the use of Cumyl-PEGACLONE in the mechanism of death. It is known that heavy alcohol consumption is linked to structural heart disease (alcohol-associated dilated cardiomyopathy and alcohol-associated atherosclerotic and hypertensive heart disease), functional heart disease (arrhythmogenesis associated with acute and chronic alcohol consumption and acute alcohol withdrawal), and sudden death [14].
Further complicating the diagnosis is the fact that underlying cardiovascular disease was present in three of the five decedents, and in two cases, the hearts were larger than predicted for normal individuals. Cardiac enlargement has been recognized for more than fifty years as an independent risk factor for the occurrence of sudden cardiac death.
We believe that the excessive use of alcohol with or without additional underlying cardiovascular disease predisposed the decedents to the reported cardiovascular effects associated with the use of SCRAs such as hypertension, tachycardia, and myocardial ischemia [15]. Unfortunately, in the total absence of histopathologic evidence about the effects of this drug, this can only remain a matter of speculation, and continued research is needed to elucidate the effects and toxicity of Cumyl-PEGACLONE.
The interpretation of deaths related to the use of new psychoactive substances is complex, and a comprehensive analysis and consideration of all the relevant factors is essential.
Conclusion
Deaths related to Cumyl-PEGACLONE use in the Northern Territory of Australia are emerging. Although the exact mechanism(s) of death related to Cumyl-PEGACLONE are not fully established, this additional descriptive case series reaffirm an association with underlying cardiovascular disease, and suggest that concurrent use with alcohol may be relevant.
Key points
-
1
Cumyl-PEGACLONE related deaths are emerging in the Northern Territory of Australia.
-
2
The use of Cumyl-PEGACLONE has only recently been regulated in the Northern Territory of Australia.
-
3
The concurrent use of Cumyl-PEGACLONE and alcohol in the context of underlying cardiovascular disease may be relevant in the mechanism of death.
-
4
Cumyl-PEGACLONE-related fatalities in the Northern Territory only involved middle-aged male decedents.
-
5
Cumyl-PEGACLONE-related fatalities in the Northern Territory occur at urban and remote locations, indicating its availability in diverse populations.
Availability of data and material (data transparency)
All relevant data has been included in the manuscript.
References
Australian Bureau of Statistics. 2016. https://www.abs.gov.au/ausstats/abs@.nsf/mediareleasesbyCatalogue/C73D7CC81CA1FD2FCA258148000A4067?OpenDocument. Accessed 18 May 2020.
Nash C, Butzbach D, Stockham P, et al. A fatality involving Furanylfentanyl and MMMP, with presumptive identification of three MMMP metabolites in urine. J Anal Toxicol. 2018;43:291–8.
Nash C, Glowacki L, Gerostamoulos D, et al. Identification of a thermal degradation product of CUMYL-PEGACLONE and its detection in biological samples. Drug Test Anal. 2019;11:1480–5.
Elliott S, Sedefov R, Evans-Brown M. Assessing the toxicological significance of new psychoactive substances in fatalities. Drug Test Anal. 2018;10:120–6.
Kitzman D, Scholz DG, Hagen PT, et al. Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity). A quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc. 1988;63:1237–46.
Giorgetti A, Mogler L, Halter SD, et al. Four cases of death involving the novel synthetic cannabinoid 5F-Cumyl-PEGACLONE. Forensic Toxicol. 2019;38:314–26.
Alcohol, tobacco & other drugs in Australia, New (and emerging) psychoactive substances - Australian Institute Of Health And Welfare. 2020. https://www.aihw.gov.au/reports/phe/221/alcohol-tobacco-other-drugs-australia/contents/drug-types/new-and-emerging-psychoactive-substances. Accessed 25 May 2020.
Misuse of Drugs (Act Amendment) Regulations 2020 (No.9) (NT) (Austl.) https://legislation.nt.gov.au/en/Subordinate-Legislation/Misuse-of-Drugs-Act-Amendment-Regulations-2020-SL-9. Accessed 28 May 2020.
Moon C. Northern Territory drug trends 2018: Key findings from the Illicit Drug Reporting System (IDRS) Interviews. Sydney: National Drug and Alcohol Research Centre, UNSW Australia; 2019.
Darke S, Duflou J, Farrel M, et al. Characteristics and circumstances of synthetic cannabinoid-related death. Clin Toxicol. 2020;58:368–74.
Halter S, Angerer V, Rohrich J, et al. Cumyl-PEGACLONE: A comparatively safe new synthetic cannabinoid receptor agonis entering the NPS market. Drug Test Anal. 2018;11:347–9.
Kraemer M, Boehmer A, Madea B, et al. Death cases involving certain new psychoactive substances: a review of the literature. Forensic Sci Int. 2019;298:186–267.
Janssens L, Cannaert A, Conolly MJ, et al. In vitro activity profiling of Cumyl-PEGACLONE variants at the CB1 receptor: Fluorination versus isomer exploration. Drug Test Anal. 2020;12:1336–43.
Cunningham KS. Alcohol and heart disease in the forensic setting. Acad Forensic Pathol. 2014;4:172–9.
Pacher P, Steffens S, Hasko G, et al. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol. 2018;15:151–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was granted by the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research and permission for this research was granted by the NT Coroner’s Office.
Consent to participate and consent for publication
The anonymized data used in the study was considered to be low risk, with no impact on the deceased study subjects or their relatives, and therefore a waiver of informed consent to the use of data applied.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tiemensma, M., Rutherford, J.D., Scott, T. et al. Emergence of Cumyl-PEGACLONE-related fatalities in the Northern Territory of Australia. Forensic Sci Med Pathol 17, 3–9 (2021). https://doi.org/10.1007/s12024-020-00334-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-020-00334-0