Abstract
Background
Olaparib is a first-in-class potent oral poly(ADP-ribose) polymerase inhibitor.
Objectives
The aims of this analysis were to establish an integrated population pharmacokinetic (PK) model of olaparib in patients with solid tumors and to bridge the PK of olaparib between capsule and tablet formulations.
Methods
The population PK model was developed using plasma concentration data from 659 patients in 11 phase I, II, and III studies of olaparib tablets/capsules monotherapy. Relative bioavailability between the tablet and capsule formulations was estimated and the relative exposure between olaparib tablet and capsule therapeutic doses was further assessed.
Results
The concentration–time profile was described using a two-compartment model with sequential zero- and first-order absorption and first-order elimination for both capsules and tablets with different absorption parameters. Multiple-dose clearance compared with single-dose clearance was reduced by approximately 15% (auto-inhibition). Disease severity had an impact on olaparib clearance, and tablet strength had an impact on Ka. The olaparib geometric mean area under the curve (AUC) and maximal concentration (Cmax) following a single 300 mg tablet were 42.1 μg h/mL and 5.8 μg/mL, respectively, and the steady-state geometric mean AUC and Cmax following a 300 mg tablet twice daily were 49.0 μg h/mL and 7.7 μg/mL, respectively. The relative exposure (AUC) of the 300 mg tablet formulation is 13% higher than the 400 mg capsule formulation.
Conclusion
This analysis bridged the olaparib capsule and tablet formulation PK and provided key assessment to support the approval of the olaparib tablet formulation in patients with ovarian cancer, regardless of their BRCA mutation status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The olaparib capsule formulation was approved based on significant efficacy in a platinum-sensitive relapsed ovarian cancer population regardless of BRCA mutation status. |
The SOLO2 study also demonstrated significant efficacy of olaparib using the tablet formulation, but the study was conducted in gBRCA-mutated ovarian cancer patients. |
This analysis bridged the olaparib capsule (400 mg twice daily) and tablet formulation (300 mg twice daily) pharmacokinetics (PK) and provided key assessment to support the approval of the olaparib tablet formulation in patients with ovarian cancer, regardless of their BRCA mutation status. |
The oral bioavailability of the tablet formulation is higher than the capsule formulation. The population PK analysis results were included in olaparib labeling (US package insert). |
1 Introduction
Olaparib (Lynparza™) is a first-in-class potent oral poly(ADP-ribose) polymerase (PARP) inhibitor [1]. PARP inhibition leads to the accumulation of DNA single-strand breaks, which can lead to the development of more deleterious double-strand breaks. In tumors with deficiencies in the homologous recombination repair pathway (such as mutations in BRCA1 and BRCA2), double-strand breaks lead to an increase in genomic instability and result in tumor cell death [1].
Olaparib was first developed in a capsule formulation and was first approved as monotherapy in the USA and EU for the treatment of adult patients with deleterious or suspected deleterious germline BRCA-mutated advanced ovarian cancer previously treated with three or more lines of chemotherapy, or who are in response (complete or partial) to platinum-based chemotherapy, respectively [2, 3].
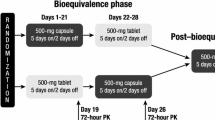
The approved capsule formulation of olaparib requires patients to receive eight 50 mg capsules twice daily for the approved daily dose (2 × 400 mg). The capsule formulation increases olaparib solubility by combining 10% crystalline olaparib in lauroyl macrogolglycerides. To improve patient convenience, a melt-extrusion tablet formulation was developed for phase III clinical trials to deliver the therapeutic dose in fewer dose units: 300 mg twice daily (2 × 150 mg tablets) equivalent to a total daily dose of 600 mg. The tablet formulation stabilizes the amorphous form of olaparib, which has higher solubility than the crystalline form used in the capsule formulation, in a melt-extruded solid dispersion that dissolves via an erosion mechanism. Given the different drug delivery technologies in the capsule and tablet, the formulations are not considered to be bioequivalent. An adaptive open-label phase I study showed that a tablet formulation of 300 mg twice daily matched or exceeded the steady-state exposure of 400 mg twice daily capsules and provided similar tolerability and efficacy in terms of tumor shrinkage in patients with germline BRCA-mutated ovarian cancer [4]. The olaparib tablet formulation has been approved in multiple countries for ovarian and breast cancer and is being investigated in other cancer types (e.g. prostate, pancreatic cancer) [2, 4, 5].
A mass balance study in humans indicated olaparib was the major component present in plasma, and drug-related materials were eliminated via the renal (approximately 44% of the dose) and fecal (approximately 42% of the dose) routes [6]. In vitro and in vivo studies showed that olaparib metabolism is mediated mainly by cytochrome P450 (CYP) 3A4/5 [7, 8]. Olaparib is not recommended to be administered with moderate or potent CYP3A4 inhibitors or inducers; [7] however, if a moderate or potent CYP3A inhibitor must be administered, then the olaparib dose should be reduced [4]. In vitro studies also indicated that olaparib was an inducer of CYP3A4 and a time-dependent inhibitor of CYP3A4/5; however, the net effect of olaparib on CYP3A in vivo is weak time-dependent inhibition [8].
Following administration of a 300 mg (2 × 150 mg tablets) single dose of olaparib tablets, peak plasma concentrations were reached after approximately 1.5 h, after which olaparib concentrations decreased in a biphasic fashion, with a terminal half-life (t½) of approximately 15 h [7, 9]. Food slows the rate of olaparib absorption but has no effect on the extent of absorption; therefore, this effect is not considered clinically significant and patients are allowed to take olaparib tablets with or without food.
Expanding on these prior assessments, the objective of the current analyses was to develop a population pharmacokinetic (PK) model for olaparib to derive PK parameters describing concentration–time data following administration of either capsules or tablets in patients with advanced solid tumors (i.e. breast or ovarian cancer). These analyses also sought to describe potential differences in the absorption kinetics profile of the two formulations, estimate relative bioavailability, determine the influence of covariates on the PK of olaparib, and generate individual post hoc exposure estimates for subsequent exposure–response analysis.
2 Methods
2.1 Study Design and Population
This analysis utilized pooled plasma concentration data obtained from 11 phase I, II, and III clinical studies with olaparib monotherapy in patients with cancer, including five studies using capsule formulations only, five studies using tablet formulations only, and one study using both capsule and tablet formulations. Some studies were not included in the analysis due to availability at the time of analysis, e.g. hepatic and renal impairment studies. Within the included studies, the period of fed state in the food effect part of study 04, as well as patients with gastric surgery, vomiting, erroneous PK sampling date, and unknown dosing history, were excluded. The effects of strong CYP3A inhibitors or inducers on the PK of olaparib had been well-characterized in a formal drug–drug interaction study [7]. In patients, coadministration with itraconazole (a strong CYP3A inhibitor) increased olaparib area under the plasma concentration–time curve (AUC) by 170% (n = 57) and coadministration with rifampicin (a strong CYP3A inducer) decreased olaparib AUC by 87%. Therefore, data from patients who received coadministration of CYP3A inducers or inhibitors were excluded from the analysis. Patients received once- or twice-daily oral doses of 10–600 mg olaparib capsule formulation or 100–450 mg once- or twice-daily oral tablet formulations. A summarized description of all the studies included in this analysis can be found in Table 1.
Blood samples after single and/or multiple doses for determination of olaparib concentrations were taken from all patients in phase I/II studies and selected patients in the phase III study. The determination of olaparib drug concentrations was performed by liquid chromatography mass spectrometry using a deuterated internal standard as previously reported [10]. The lower limits of quantification for olaparib were 0.5 and 20 ng/mL in the high- and low-sensitive methods, respectively. Either the high- or low-sensitive method was used depending on the expected plasma concentration of olaparib.
The Institutional Review Boards or independent Ethics Committees of all investigational sites approved all clinical studies, and the studies were performed in accordance with the Declaration of Helsinki, Good Clinical Practice, and the AstraZeneca Policy on Bioethics.
2.2 Population Pharmacokinetic (PK) Analysis
2.2.1 Base Model Development
Three population PK analyses of olaparib have been previously conducted. The first was developed for the olaparib capsule formulation, the second for the tablet formulation in patients with advanced solid tumors [12] and the third for the tablet formulation using data from a phase III study that supported the proposed maintenance indication in patients with ovarian cancer [13]. As the current analysis combined data from all three previous analyses, the initial exploratory graphical analysis as well as results from previous analysis were used to guide the base model selection. A two-compartment model with a sequential zero- and first-order absorption model was selected as the base structural model for olaparib. Given the difference in release mechanisms, different absorption parameters of capsule and tablet formulations were estimated in the base model. As preclinical and in vivo studies indicated, olaparib is a time-dependent inhibitor of CYP3A4/5, [8] and because olaparib is also a substrate of the CYP3A4/5 enzyme, [7] auto-inhibition is possible after multiple doses. Therefore, a potential change in olaparib apparent clearance (CL/F) after multiple-dose administrations was estimated. As non-compartmental analyses indicated a less than dose proportional increase in olaparib exposure for a capsule dose ≥ 100 mg, an empirical linear model was used for the relative bioavailability (F1) for these formulations, and the < 100 mg capsule dose was included as reference (F1 = 1) in the base model using the following equation:
where THETA is a parameter estimate for the relationship between capsule doses ≥ 100 and < 100 mg, and TVF1 is the typical value of relative bioavailability for capsule doses ≥ 100 mg. In addition, a separate F1 was applied for the tablet formulation. Between-subject variability (BSV) was examined for each of the typical PK parameters and included in the base model if supported by data.
2.2.2 Covariate Analysis
The potential covariate effect on olaparib PK was evaluated by a stepwise forward selection and backward elimination procedure using the stepwise covariate model (SCM) implemented in the PsN toolkit [11]. The p-values for forward selection and backward elimination were set at 0.01 and 0.001, respectively, corresponding to a decrease in the NONMEM objective function value (OFV) of 6.68 and 10.83 units, respectively. The effect of demographic factors (body weight, age, sex, and race), renal function (creatinine clearance [CrCl]), hepatic function [National Cancer Institute criteria]), as well as line of treatment, Eastern Cooperative Oncology Group (ECOG) performance status, tumor type (ovarian cancer, breast cancer, and other types) were tested to explain intersubject variability in the CL/F and central volume of distribution of olaparib. In addition, the effect of age and tablet strength were also explored as fixed effects on absorption of olaparib (Ka). Continuous covariates were evaluated as a power model centered on a median value, while categorical covariates were incorporated into the base model as a linear proportional model, with a coding variable equal to 1 when the covariate is present and 0 when it is absent.
2.2.3 Model Evaluation
Model evaluation was guided by several assessment methods, including visual inspection of diagnostic plots, successful convergence, changes in the OFV, precision of parameter estimates, covariance estimation, and plausibility of parameter estimates. The predictive performance of the final model was assessed with a prediction-corrected visual predictive check (pcVPC) [14] using simulation of 1000 new data sets. The final model outcomes were also evaluated using a nonparametric bootstrap approach using 1000 replicate bootstrap data sets [11, 15].
2.2.4 Empirical Bayes Estimation
Individual empirical Bayes estimates of olaparib PK parameters from the final population PK model were used to simulate the olaparib concentration–time profile after single doses and at steady-state using the individual nominal dose at the beginning of study. The AUC and maximal concentration (Cmax) values after single doses and at steady-state were calculated for different dose levels and the relative exposure between the 300 mg tablet and 400 mg capsule were estimated. The estimated individual exposure was also applied in the subsequent exposure–response analysis.
2.2.5 Modeling Methodology and Software
The software packages NONMEM version 7.3 (ICON Development Solutions, Hanover, MD, USA) and R version 3.2.4 (The R Foundation for Statistical Computing, Vienna, Austria) were used for modeling and simulation. R was also used for data preparation, graphical analysis, model diagnostics, and statistical summaries. Perl-speaks-NONMEM (PsN) [11] was used to implement all the NONMEM runs for the population PK modeling and diagnostic check. The first-order conditional estimation with interaction between the interindividual and residual random effects (FOCEI) method in NONMEM was employed for all model runs.
3 Results
3.1 Patient Population and Characteristics
Patients who had at least one measurable value (greater than the lower limit of quantification) for the plasma olaparib concentration were included in the population PK analysis dataset. Any patients with a history of gastric surgery, or coadministered strong CYP3A4 inducers or inhibitors, were excluded from the analysis. The final pooled data set for the population PK analysis included 659 patients with a total of 10,092 olaparib plasma concentrations from 11 studies. Of the 659 patients analyzed, the majority were female (588; 89%), White (589; 90%), and with normal hepatic function (571; 87%), normal renal function (317; 48.1%), and ovarian cancer (427; 65%). The ECOG performance status (score of 0 [normal activity], 1 [restricted activity], and 2 [in bed ≤ 50% of the time]) was used to define disease severity; no patient had an ECOG performance status score > 2. The majority of patients were able to carry on normal activity (52.6%) or restricted activity (43.9%). The number of prior lines of chemotherapy treatment was not available for study NCT00572364 (n = 12, 1.8%), and 3 of 659 (0.4%) patients were missing ECOG performance status or race information. The missing line of treatment covariate was assigned as a line of treatment > 5, while missing ECOG performance status and race were assigned as the most common within the category. The summary of covariates for the pooled data set are shown in Table 2.
3.2 Population PK Model
The olaparib PK concentration–time profile was adequately described using a two-compartment model with sequential zero- and first-order absorption and first-order elimination for both capsule and tablet formulations. A proportional residual error model and BSV for the absorption rate constant (Ka), duration of absorption (D1), CL/F, central and peripheral volume of distribution (V2/F and V3/F, respectively), and intercompartmental clearance (Q/F) were estimated. The final parameter estimates for olaparib are summarized in Table 3. Although the same zero- and first-order absorption structure model was supported by plasma concentration data from either capsule or tablet formulations, the absorption between capsule and tablet formulations was distinguished by approximately a twice longer zero-order release rate constant for the capsule (0.90 h) compared with the tablet formulation (0.47 h). With the bioavailability (F1) of the capsule formulation doses < 100 mg being used as reference of 1, the estimated population mean relative F1 for the capsule formulation 400 mg and tablet formulation (all doses) were 26.6% and 62.7%, respectively. Thus, the model–derived relative F1 of all the tablet doses relative to the capsule formulation dose of 400 mg and above was 236% (62.7%/26.6%). The relative exposure between the 300 mg tablet formulation and the 400 mg capsule formulation was 177% after taking dose into account. The CL/F of olaparib after a single dose was 4.22 L/h, and clearance was reduced by approximately 15% after multiple doses due to auto-inhibition, regardless of formulation.
The effect of demographic factors, renal function, hepatic function, as well as line of treatment, ECOG performance status, and tumor types were tested as covariates on the CL/F and V2/F of olaparib. ECOG performance status was identified as a significant covariate on overall clearance. Patients with an ECOG performance status score of 1 and 2 were estimated to exhibit decreased olaparib clearance by 24.0% and 58.5%, respectively, when compared with patients with an ECOG performance status score of 0. In addition, the tablet strength was found to be influential on the absorption rate; olaparib Ka increased by 86% with a 100 mg strength tablet compared with a 150 mg strength tablet. Other tablet strengths (200, 300, 125, and 225 mg) had less impact (32.6% increase compared with 150 mg strength) on the Ka of olaparib (Table 3). None of the other demographic covariates or laboratory observations had a significant effect on olaparib PK parameters. More specifically, prior lines of chemotherapy treatment or patient tumor type had no impact on olaparib PK. The shrinkage values were all below 30% for interindividual variability of all PK parameters, except for Ka and V2/F, which were 31.5% and 36.7%, respectively. The reasonable shrinkage values suggested the model could be used for further exposure–response analysis using empirical Bayes estimates [16].
3.3 Model Evaluation
The standard goodness-of-fit plots of the final model are shown in Fig. 1. Individual predicted values agreed well with observed values across the range of observations. The weighted residuals were evenly scattered across the range of predicted concentrations and time. The stability of the final population PK model was evaluated by bootstrapping. The median values of parameter estimates from the bootstrap analysis were in close agreement with the population estimates in the final model, suggesting that the parameter estimates of the model were unbiased (Table 3). The pcVPC plot of the full dataset (Fig. 2) suggested the model could adequately represent the distribution of observed olaparib concentrations. Most of the observed concentrations were within the 95% prediction interval, indicating that the predicted variability did not exceed the observed variability. The pcVPC in capsule and tablet formulations from study D0810C00024 (Fig. 3) further demonstrated the final model could reasonably describe observed olaparib concentrations in both capsule and tablet formulations.
Visual predictive check for the final covariate model. The pink-shaded areas represent the 90% CI around the median, and the light-blue-shading at the bottom and top areas represents the 90% CI around the predicted 5th and 95th percentiles. The red solid line represents the observed median, and the dotted lines represent the observed 5th and 95th percentiles of the data. The circles represent individual observations. CI confidence interval
Visual predictive check for the final covariate model for Study D0810C00024 with olaparib capsule (a) and tablet (b) formulation dose administration. The pink-shaded areas represent the 90% CI around the median, and the light-blue-shading at the bottom and top areas represents the 90% CI around the predicted 5th and 95th percentiles. The red solid line represents the observed median, and the dotted lines represent the observed 5th and 95th percentiles of the data. The circles represent individual observations. CI confidence interval
3.4 Empirical Bayes Estimation
The final olaparib population PK model was used to obtain individual empirical Bayes estimates of PK parameters and exposure of AUC, Cmax, and minimal plasma concentration (Cmin) for patients administered 100, 200, and 400 mg olaparib single or multiple (twice daily) capsule formulations, and for subjects administered 200, 250, and 300 mg olaparib single or multiple (twice daily) tablet formulations. The summary of model-predicted AUC and Cmax after single- or multiple-dose administrations of olaparib is presented in Fig. 4 and Electronic Supplementary Table S1. The olaparib geometric mean AUC and Cmax following a single 300 mg tablet dose (n = 204) were 42.1 μg h/mL and 5.8 μg/mL, respectively, and the steady-state geometric mean AUC and Cmax following a 300 mg tablet twice daily (n = 227) were 49.0 μg h/mL and 7.7 μg/mL, respectively. The steady-state geometric mean AUC and Cmax following a 200 mg tablet twice daily (n = 30) were 39.0 μg h/mL and 7.0 μg/mL, respectively. The steady-state geometric mean AUC and Cmax following a 400 mg commercial capsule twice daily (n = 48) were 43.5 μg h/mL and 6.2 μg/mL, respectively. Finally, the geometric mean steady-state exposure of the 300 mg tablet formulation was 13% higher than the 400 mg capsule formulation (Electronic Supplementary Table S1).
4 Discussion
Study 19 [19] and SOLO2 [18] were the pivotal studies that led to the approval of olaparib in patients with ovarian cancer for capsule and tablet formulations, respectively. Study 19 (capsule) was conducted in ovarian cancer patients regardless of BRCA mutation, but SOLO2 (tablet) was conducted in gBRCA-mutated patients only. To gain approval for the tablet formulation in a broader population (regardless of BRCA mutation), bridging olaparib PK between tablet and capsule was raised as a key question from multiple regulatory agencies, including the FDA, European Medicines Agency (EMA) and Health Canada. The current analysis integrated PK data from different patient populations to evaluate the impact of formulations, patient demographics, ECOG performance status, lines of treatment, and tumor types on the PK of olaparib. This analysis provided key assessment to support approval of the olaparib tablet formulation in patients with ovarian cancer, regardless of their BRCA mutation status.
In this population PK model, the same two-compartment disposition model was applied to describe drug distribution and elimination for both capsule and tablet formulations. Although the same zero- and first-order absorption model was used to describe the absorption process of both formulations, different magnitudes of absorption parameter estimates were applied to distinguish different absorption processes between the two formulations. In addition, the empirically selected parameter model characterized well the less than dose-proportional increase in olaparib ≥ 100 mg in capsule formulation. The estimated CL/F and apparent total volume of distribution for the tablet formulation in this analysis were approximately 6.7 L/h and 35.5 L, respectively. These values are similar to those previously reported (6.83 L/h and 32.4 L, respectively) using a single phase I study [17]. Based on model Bayesian estimates, the geometric mean steady-state exposure of the 300 mg tablet formulation was 13% higher than the 400 mg capsule formulation, which is in agreement with the value (31%) reported in a non-compartmental analysis from a tablet–capsule formulation crossover study (D0810C00024) [4]. Olaparib showed time-dependent PK that the steady-state clearance decreased by 15% after multiple dosing. These results of the population PK model were included as part of the prescribing information [4].
Among the covariates evaluated for potential impact on olaparib PK, the demographic factors and hepatic or renal function did not significantly influence olaparib clearance or volume of distribution, which is similar to the previously reported population PK analysis [17]. In addition, the line of treatment and tumor type (ovarian cancer vs. breast cancer vs. other cancer types) were not identified to have significant impact on the overall olaparib PK; however, the ECOG performance status score was found to have a statistically significant impact on olaparib clearance. The observed decrease in olaparib clearance in patients with an ECOG performance status score of 2 was based on 23 patients, representing only 3.5% of the total patients included in the analysis, only 5 of whom were administered 300 mg tablets twice daily, which is considered insufficient to derive a definitive conclusion. Furthermore, in an attempt to further understand this finding, the potential contribution of reduced renal or hepatic function in these patients with poor performance status (ECOG = 2) was examined, and neither was found to be responsible for the elevated exposure observed in these patients. There is no obvious biological explanation for olaparib exposure being higher in patients with an ECOG performance status score of 2. A similar effect was observed for sunitinib, where patients with an ECOG score of 2 have decreased sunitinib metabolite clearance; [20] however, the mechanism was not clear either. Additionally, it should be noted that the ECOG performance status is subjectively defined and is therefore imprecise. Given the limitations of this analysis and the expectation that clinical impact with such exposure differences is minimal, cautious interpretation should be exercised regarding ECOG performance status.
The 300 and 400 mg twice-daily doses were the approved starting doses for the tablet and capsule formulations, respectively. Although the 300 mg tablet formulation exhibited higher exposure than the exposure observed after the 400 mg capsule formulation, the safety data from SOLO2 (300 mg tablet formulation) [18] was consistent with that from Study 19 (400 mg capsule formulation), [19] with only leukopenia identified as a new adverse drug reaction. Similarly, the safety profile of olaparib from the larger 300 mg twice-daily tablet pool was consistent with that from the larger 400 mg twice-daily capsule pool (data on file). Hematologic toxicity (primarily anemia) was reported at an increased frequency with the tablet formulation compared with the capsule formulation; however, anemia remained manageable by interrupting or reducing olaparib dose or administering blood transfusions when indicated, and treatment discontinuation was rarely required. Reports of neutropenia and thrombocytopenia remained at low frequency with the tablet formulation; these events remained primarily low grade and rarely required treatment discontinuation. Nausea and vomiting, as well as grouped events of fatigue and asthenia, were reported, with a similar frequency and severity for both the tablet and capsule formulations. Since the safety and efficacy profiles for both formulations are similar, no impact on the benefit–risk profile is expected should patients switch from capsule to tablet formulation.
5 Conclusions
An integrated population PK model of two-compartment disposition with consecutive zero- and first-order absorption described olaparib PK and its variability well in both tablet and capsule formulations. The relative exposure (AUC) of the 300 mg tablet formulation is 13% higher than the 400 mg capsule formulation. This analysis bridged the olaparib capsule and tablet formulation PK and provided key assessment to support the approval of the olaparib tablet formulation in patients with ovarian cancer, regardless of their BRCA mutation status. The model can be applied for further exposure–response analyses to support and inform clinical decisions.
References
O’Connor MJ. Targeting the DNA damage response in cancer. Mol Cell. 2015;60:547–60.
FDA. Lynparza prescribing information. 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/208558s001lbl.pdf. Accessed 11 June 2018.
European Medicines Agency. Lynparza (olaparib); EPAR. 2015. http://www.ema.europa.eu/ema/index.jsp?curl=/pages/medicines/human/medicines/003726/human_med_001831.jsp. Accessed 11 June 2018.
Mateo J, et al. An adaptive study to determine the optimal dose of the tablet formulation of the PARP inhibitor olaparib. Target Oncol. 2016;11:401–15.
Mateo J, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373:1697–708.
Ang JE, et al. A mass balance study to investigate the metabolism, excretion and pharmacokinetics of [14C]-olaparib (AZD2281) in patients with advanced solid tumours refractory to standard treatments. Eur J Cancer Suppl. 2010;8:128–9.
Dirix L, et al. Effect of itraconazole and rifampin on the pharmacokinetics of olaparib in patients with advanced solid tumors: results of two phase I open-label studies. Clin Ther. 2016;38:2286–99.
McCormick A, Swaisland H, Reddy VP, Learoyd M, Scarfe G. In vitro evaluation of the inhibition and induction potential of olaparib, a potent poly(ADP-ribose) polymerase inhibitor, on cytochrome P450. Xenobiotica. 2018;48(6):555–64.
Plummer R, et al. Olaparib tablet formulation: effect of food on the pharmacokinetics after oral dosing in patients with advanced solid tumours. Cancer Chemother Pharmacol. 2015;76:723–9.
Rolfo C, et al. Effect of food on the pharmacokinetics of olaparib after oral dosing of the capsule formulation in patients with advanced solid tumors. Adv Ther. 2015;32:510–22.
Lindbom L, Pihlgren P, Jonsson EN, Jonsson N. PsN-Toolkit—a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79:241–57.
Xu H, Li J, Learoyd M, Bui K, Tomkinson H, Al-Huniti N. Population pharmacokinetic (PK) and exposure haemoglobin response analysis for olaparib tablet formulation. Clin Pharmacol Ther. 2017;101(Suppl 1):S92.
Li J, Xu H, Learoyd M, Bui K, Tomkinson H, Al-Huniti N. Population pharmacokinetic (PopPK) and exposure response (E-R) analyses for olaparib tablet formulation in a Phase III study (SOLO2) in patients with ovarian cancer. J Pharmacokinet Pharmacodyn. 2017;44(Suppl 1):133.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 2011;13:143–51.
Xu H, et al. Evaluation of aztreonam dosing regimens in patients with normal and impaired renal function: a population pharmacokinetic modeling and Monte Carlo simulation analysis. J Clin Pharmacol. 2017;57:336–44.
Savic RM, Karlsson MO. Importance of shrinkage in empirical Bayes estimates for diagnostics: problems and solutions. AAPS J. 2009;11:558–69.
Peer CJ, et al. Population pharmacokinetic analyses of the effect of carboplatin pretreatment on olaparib in recurrent or refractory women’s cancers. Cancer Chemother Pharmacol. 2017;80:165–75.
Pujade-Lauraine E, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84.
Ledermann J, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012;366:1382–92.
Houk BE, et al. A population pharmacokinetic meta-analysis of sunitinib malate (SU11248) and its primary metabolite (SU12662) in healthy volunteers and oncology patients. Clin Cancer Res. 2009;15:2497–506.
Yamamoto N, et al. A phase I, dose-finding and pharmacokinetic study of olaparib (AZD2281) in Japanese patients with advanced solid tumors. Cancer Sci. 2012;103:504–9.
Fong PC, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361:123–34.
Tutt A, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376:235–44.
Audeh MW, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trial. Lancet. 2010;376:245–51.
Kaye SB, et al. Phase II, open-label, randomized, multicenter study comparing the efficacy and safety of olaparib, a poly(ADP-ribose) polymerase inhibitor, and pegylated liposomal doxorubicin in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer. J Clin Oncol. 2012;30:372–9.
Yonemori K, et al. Safety and tolerability of the olaparib tablet formulation in Japanese patients with advanced solid tumours. Cancer Chemother Pharmacol. 2016;78:525–31.
Acknowledgements
The authors would like to thank the patients, their families, and all investigators and study personnel involved. They would also like to acknowledge the programmers who supported the compilation of the dataset, Mihai Surducan of Mudskipper Ltd for medical writing assistance funded by AstraZeneca, and the FDA pharmacometric reviewers Chao Liu, Jingyu Yu, and Yaning Wang for their comments. This study was sponsored by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by AstraZeneca.
Conflict of interest
Diansong Zhou, Maria Learoyd, Alienor Berges, Tsveta Milenkova, Nidal Al-Huniti, Helen Tomkinson, and Hongmei Xu are employees of and shareholders in AstraZeneca. Jianguo Li and Khanh Bui are former employees of AstraZeneca.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, D., Li, J., Bui, K. et al. Bridging Olaparib Capsule and Tablet Formulations Using Population Pharmacokinetic Meta-analysis in Oncology Patients. Clin Pharmacokinet 58, 615–625 (2019). https://doi.org/10.1007/s40262-018-0714-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-018-0714-x