Abstract
Vitiligo is an acquired immune disorder of the skin characterized by the presence of white depigmented macules. Its immunopathogenesis is not completely understood, but inflammatory alterations in the skin microenvironment, and particularly increased expression of the cytokine tumor necrosis factor-α (TNFα), are thought to be essential regulators of melanocyte dysfunction and death. In this article we review the evidence that implicates TNFα in the pathogenesis of vitiligo, including studies on serum and tissue levels of TNFα, TNFα gene polymorphisms, in vitro studies, and therapeutic trials using TNFα inhibitors. TNFα emerges as a complex mediator with apparently conflicting roles in vitiligo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
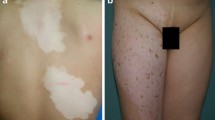
Vitiligo is an acquired cutaneous disorder of pigmentation, with a 0.5–2 % incidence worldwide that affects males and females alike [1]. It is characterized by progressive depigmentation and the appearance of white cutaneous macules, usually with no other clinical symptoms. Clinically, it can present as a non-segmental variant, with bilateral and generalized distribution (the most common form) or as a segmental variant, involving a single body region. Depigmentation is due to the loss of functioning melanocytes [1, 2]. Multiple studies have provided evidence of various candidate genes and loci associated with vitiligo, and no single gene has been singled out as determinant for the development of the disease [2].
The immunopathological mechanisms leading to melanocyte loss are not completely understood. Autoimmune, autocytotoxic/metabolic and neural dysfunctional mechanisms have been proposed [1, 2]. Common to all of these hypotheses is an inflammatory alteration of the epidermal and dermal microenvironments. Mononuclear cell inflammatory infiltrates, changes in cytokine and chemokine balance, increased oxidative stress and changes in cellular immunity across all the involved cell subtypes appear to be primary immunopathologic events in the development of vitiligo (see Guerra et al. [1, 3] and Sandoval-Cruz et al. [1, 3] for reviews).
Altered numbers and function of T cells are proposed as participants in the development of vitiligo [4]. Increased circulating numbers of CD8+ T lymphocytes and decreased levels of regulatory T cells have been correlated to disease severity in vitiligo patients [5], although other studies have not replicated these results [6]. Nevertheless, lymphocytic infiltrates in vitiliginous lesions are a common finding, and tend to show a predominantly T-helper-1 cell (Th1) response with the release of various cytokines, including tumor necrosis factor-α (TNFα) [2, 4]. In the Smyth line animal model of vitiligo, lymphocyte imbalance and a Th1-polarized response have been confirmed as central immune alterations associated with disease activity [7]. However, inflammatory cells are not the only sources of cytokine production. Keratinocytes are hypothesized to produce an excess of a variety of cytokines, including TNFα, in the vitiliginous microenvironment [8], and dermal cells such as fibroblasts could be another source of TNFα production under inflammatory conditions [9].
The prominent role of TNFα in regulating the inflammatory response, from leucocyte-cell interactions to cytotoxic activity, has led to it being proposed as a central effector in the immunopathological mechanisms involved in vitiligo. However, therapeutic trials using anti-TNFα agents in treating vitiligo have shown mostly negative results, calling into question the physiopathological relevance of TNFα. In this article, we will review the evidence linking TNFα to vitiligo, and discuss a possible explanation for the conflicting results so far obtained.
2 Peripheral Blood Cells and Plasma
The determination of cytokine levels in sera or blood cells taken from patients with a disease, and comparing it with samples taken from matched controls, can lead to associations between the cytokine and disease. Unfortunately, in the case of TNFα, its general role in the acute phase response of the inflammatory cascade makes it non-specific. Thus, TNFα elevations occur in a myriad of clinical conditions. In one of the earliest studies carried out on peripheral mononuclear cells derived from patients with vitiligo, the spontaneous production of the cytokines interleukin (IL)-6 and IL-8 was found to be increased, with no changes in TNFα production [10]. In fact, TNFα production was diminished when these cells were stimulated with anti-mononuclear cell immunoglobulin. This was thought to explain the reduced inflammatory reaction found in vitiliginous lesions.
Another study failed to show increased serum levels of TNFα in 50 patients with active vitiligo, although an IL-6 elevation was indeed confirmed [11]. Similar findings were reported in another study, where IL-6 and IL-2 were increased in sera from 80 patients with vitiligo compared with normal controls, but no difference was observed in TNFα concentrations [12]. Finally, in a study of 40 patients with non-segmental vitiligo, serum levels of soluble TNF receptor I were also similar to healthy controls [6]. However, at least two studies found positive results: increased production of TNFα by peripheral mononuclear cells derived from 32 patients with active vitiligo that were stimulated with lipopolysaccharide [13], and, in the largest study to date, elevated levels of serum TNFα in 214 vitiligo patients compared with 236 unaffected controls [14]. This last study also found increased levels of TNFα messenger RNA (mRNA) expression in a subset of the vitiligo patients. Severe disease activity, vitiligo subtype and different genotypes could be important in explaining these conflicting results. Taken together, the conflicting evidence derived from studies on peripheral blood cells or serum levels of TNFα do not suggest a precise role for this cytokine in the pathogenesis of vitiligo. However, they imply a systemic proinflammatory state that may not be representative of the spectrum of vitiligo presentations, and tissue studies would seem more pathophysiologically relevant.
3 Tissue Studies
Tissue studies showing increased TNFα activity in active vitiliginous lesions compared with unaffected skin would more strongly support the idea of an important role for TNFα in depigmentation, and this is precisely what some studies have found. Tissue samples from the affected epidermis of patients with active vitiligo have been found to have increased expression of IL-6 and TNFα, by immunohistochemical methods [8]. This suggested a relevant change in the production of cytokines in the epidermal microenvironment of vitiliginous lesions. In keeping with these results, increased mRNA expression for TNFα was found to be elevated in both involved and uninvolved skin in patients with vitiligo [15], and of both TNFα and IL-6 in the epidermis of affected skin [16]. These observations have been confirmed in other studies [17], and extended to cover other hypopigmented disorders such as tinea versicolor and mycosis fungoides [18]. Furthermore, in vitro studies of cloned CD4+ and CD8+ T cells obtained from vitiliginous lesions show a striking upregulation of TNFα and a predominantly type-1-like cytokine secretion profile [19].
However, other studies point toward significant variability in TNFα immunohistochemical staining in vitiliginous lesions. In a study of eight cases, five had strong TNFα staining, whereas three did not, although TNFα staining intensity did seem to correlate to disease activity [20]. In contrast to peripheral blood and sera studies, there is substantial evidence that TNFα is increased locally in vitiliginous lesions. Considering that vitiligo is not associated with a systemic inflammatory state, but with a localized (skin) immune reaction, these conflicting findings could be easily explained.
4 Genetic Studies
Vitiligo is an acquired disease that is genetically heterogeneous. However, a role for TNFα in its pathogenesis would be supported by findings on polymorphisms associated with TNFα genes. The TNFα-308 promoter polymorphism, which leads to higher rates of TNFα transcription, has been associated with autoimmune and inflammatory diseases. In a study of 61 patients with vitiligo, polymerase chain reaction amplification analysis of the promoter TNFα gene failed to show any difference in the G/A polymorphism at position −308 compared with age, sex, and ethnic matching controls [21]. This early negative study cast further doubts on an association between TNFα and vitiligo.
In a later study of 176 vitiligo patients, Namian et al. [22] found that the TNFα-308 G/A polymorphism was significantly more common in female vitiligo patients compared with controls, but no change in males or between vitiligo subtypes. This confirmed the heterogeneous genetic determinants of vitiligo, and suggested that genetic studies would have to control for variables other than sex and vitiligo subtype. In a recent study involving 198 vitiligo patients, the association between the TNFα-308 promoter G/A polymorphism and vitiligo was confirmed, but found only in patients with active vitiligo vulgaris: sex and age of onset were not important factors [23]. These results have been reconciled in the largest study to date. After analyzing 977 vitiligo patients, Laddha et al. [14] found that various polymorphisms (−238, −857, −863, −1031 as well as the −308 G/A polymorphism) in the promoter region of the TNFα gene were found to be significantly associated with vitiligo. That same study also showed higher TNFα transcript and protein levels in women, patients with active vitiligo, generalized vitiligo, and associations between some polymorphisms and early-age onset of disease, suggesting genotype-phenotype correlations. Laddha et al. [14] also described the association of different haplotypes with some phenotypic expressions: haplotypes AACCT, AGTCT, GATCT, and AGCCT with increased TNFα serum levels; AACCT, GATCT, GATCC, and AATCC with increased TNFα expression levels; and AACAT, AACCT, AATCC, and AATCT with early disease onset. Together, these studies support a role for TNFα promoter polymorphisms as genetic risk factors, and a role for TNFα itself in the autoimmune pathogenesis of vitiligo.
5 Mechanisms
TNFα is thought to participate in the immunopathogenesis of vitiligo by inducing melanocyte dysfunction and death through various mechanisms. TNFα has been demonstrated to be proapoptotic in various tissues and cell types. TNFα is also known to be induced by and act as an inducer for nuclear factor kappa-B (NF-κB), a transcription factor involved in inflammatory and pro-survival gene promotion. Death receptors belonging to the TNF receptor superfamily, such as TNF-related apoptosis-inducing ligand (TRAIL), participate in the induction of programmed cell death and play important roles in the immunopathogenesis of skin diseases [24]. TRAIL promotes apoptosis of primary human melanocytes in vitro by activation of caspases and cleavage of vital proteins [25], and melanocytes exposed to chemical stressors show increased TRAIL expression and promote dendritic cell-mediated melanocyte death [26].
Melanocyte function, including proliferation, differentiation and immunologic susceptibility to cytotoxicity can be altered by proinflammatory cytokines, including TNFα [27]. Adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1) are overexpressed in melanocytes from vitiligo lesions, and cytokines such as TNFα can induce their expression on the surface of epidermal melanocytes [28, 29]. Moreover, TNFα is a strong inducer of ICAM-1 in both normal and vitiliginous cultured melanocytes [30]. This pathway could influence melanocyte target recognition by T cells and mediate immunologic cytotoxic damage. TNFα can inhibit melanogenesis by decreasing the intracellular levels of tyrosinase and tyrosinase-related protein 1, an abundant melanosomal glycoprotein involved in both melanogenesis and prevention of melanocyte death [31, 32]. There is also evidence that TNFα-mediated inhibition of tyrosinase activity and melanogenesis is dependent on the activation of NF-κB [33]. TNFα-treated melanocytes show marked cellular shrinking and reduced melanin production in vitro, as well as downregulation of MITF, a transcription factor essential in the regulation of melanocyte development, proliferation, death, and melanogenesis [34]. TNFα leads to a dose-dependent inhibition of melanocyte proliferation, partly through increased expression of the CXC-chemokine receptor II [35]. TNFα also leads to reduced expression of the pigment-associated antigens HMB-45 and K.1.2 in normal cultured melanocytes [36] as well as to altered immunological phenotypes.
Other mechanisms of TNFα-induced alterations in melanogenesis have been uncovered. Melanocyte-stimulating hormone receptor (MSH-R) and melanocortin-1 receptor (MC1-R) are known inducers of melanogenesis, capable of inducing the expression of melanin synthase, modulating pigmentation and melanocyte survival in normal and pathological conditions (see Slominski et al. [37] for an excellent review). In vitro studies of normal human melanocytes have shown that TNFα downregulates MSH-R binding activity and reduces the expression of MC1-R mRNA [38]. TNFα also reduces the expression of gp87 in melanoma cells, a melanosomal protein involved in melanogenesis [39]. A recent study shed further light on the effects of TNFα in inflammation-associated pigmentation changes. Using normal human melanocytes, Wang et al. [40] showed that TNFα could stimulate the melanoma mitogens IL-8 and CXCL1, inhibit pigmentation-related signaling and melanin production, and increase the production of β-defensin 3, an antagonist for MC1-R.
A percentage of cultured normal melanocytes respond to TNFα with apoptosis, but melanocytes with high basic NF-κB binding activity do not show TNFα-induced NF-κB activation and are apoptosis resistant [41]. Apoptosis-sensitive melanocytes in turn show reduced melanogenesis. This suggests that melanocytes with impaired melanogenesis have altered NF-κB signaling that leads to susceptibility to TNFα-induced apoptosis. Impaired phosphatidylinositol 3-kinase/serine/threonine protein kinase activation followed by reduced NF-κB activation under increased TNFα levels was demonstrated as a mechanism for keratinocyte apoptosis in vitiligo as well [42]. Indeed, human vitiliginous keratinocytes treated with TNFα show increased apoptosis due to an impaired phosphatidylinositol 3-kinase/protein kinase B signaling pathway [43].
The participation of altered redox homeostasis in the pathogenesis of vitiligo has been reviewed by Laddha et al. [44] and Glassman [4]. The generation of a redox imbalance and overproduction of reactive oxygen species (ROS) such as nitric oxide (NO) and hydrogen peroxide (H2O2) could represent another possible mechanism of TNFα-induced melanocytotoxicity. The intracellular levels of H2O2 and other ROS increase in various cell systems in response to TNFα stimulation [45]. In studies of in vitro human primary keratinocytes, TNFα dose-dependently and rapidly induces ROS generation, and ROS further mediate TNFα-mediated production of inflammatory cytokines [46]. In human skin-derived cultured fibroblasts, incubation with TNFα led to increased production of H2O2 and other ROS [47]. H2O2 can also act as a messenger in the TNFα-dependent activation of NF-κB [48].
TNFα is known to induce NO production in cultured melanocytes through upregulation of inducible NO synthase [49]. A similar mechanism has been observed in cultured keratinocytes, which show TNFα-induced NO production leading to increased apoptosis [50]. A TNFα-mediated altered redox state in the skin could then lead to membrane lipid alterations and increased mitochondrial production of ROS, resulting in melanocyte apoptosis in vitiligo [1, 51]. The complex interplay between oxidative stress and immune mediators such as proinflammatory cytokines and T cells suggest a central role for oxidative stress—autoimmunity-mediated melanocyte loss in vitiligo as well [44].
The TNFα-associated alterations in melanocytes reviewed here (Fig. 1), coupled with evidence of increased TNFα levels in affected skin and TNFα gene polymorphism studies, point towards a causal role for TNFα in the immunopathogenesis of vitiligo. Studies involving modulating TNFα as a therapeutic strategy would seem warranted, and in fact some have been reported in the literature.
Mechanisms of TNFα-mediated alterations in melanocyte function in vitiligo. CXC-chemokine RII CXC-chemokine receptor II, H 2 O 2 hydrogen peroxide, ICAM-1 intercellular adhesion molecule-1, MC1-R melanocortin-1 receptor, MSH-R melanocyte-stimulating hormone receptor, NF-kappaB nuclear factor kappa B, NO nitric oxide, ROS reactive oxygen species, Th1 T-helper-1 cell, TNF-α tumor necrosis factor-α, TRAIL TNF-related apoptosis-inducing ligand, ↑ indicates increased, ↓indicates decreased
6 Treatment Studies
The expression of TNFα mRNA is decreased in lesions treated with topical tacrolimus, a finding associated with clinical improvement [15]. Although this could simply reflect a general anti-inflammatory effect induced by tacrolimus, a possible role for TNFα in the pathophysiology of vitiligo has led to the evaluation of anti-TNFα therapies as possible treatments [52]. A single case report of a patient with ankylosing spondylitis treated with infliximab (a monoclonal antibody against TNFα) described remarkable improvement in concomitant vitiligo lesions [53], and a patient with psoriasis and vitiligo treated with etanercept (TNFα receptor antibody) showed mild improvement in his concomitant vitiligo [54]. However, another study failed to show any clinical efficacy of etanercept in treating vitiligo in four patients [55], and a recent study involving six patients with vitiligo treated with infliximab, etanercept or adalimumab (humanized monoclonal antibody against TNFα), with the specific aim of treating their vitiligo, failed to show any efficacy [56]. Treatment individualization, as in using anti-TNFα agents in patients with known tissue overexpression of TNFα, could lead to better outcomes, as a recent study has shown [20].
The issue is further complicated by findings that anti-TNFα therapy can lead to the appearance of immune-mediated skin lesions, including vitiligo [57]. In fact, a case of a patient with vitiligo treated with infliximab who developed psoriasiform dermatitis and worsening vitiligo was reported recently [58]. Infliximab and adalimumab therapy have been associated with the appearance of de novo vitiligo in other clinical settings, such as rheumatoid arthritis, ulcerative colitis, and psoriatic arthritis [59–62]. Although the mechanism of anti-TNFα-induced vitiligo is unknown, some authors have speculated that paradoxical induction of autoimmunity against melanocytes might be involved [59]. Indeed, there is convincing evidence showing that anti-TNFα therapy can lead to development of auto-antibodies and new-onset of autoimmune disorders [57, 63]. Another study showed increased TNFα expression in involved skin, but after treatment with narrow-band ultraviolet B therapy in 20 patients with vitiligo [64]. There is little support of therapeutic efficacy for any type of anti-TNFα treatment in vitiligo, which is unexpected considering the tissue studies discussed above (summarized in Table 1).
7 A Dual Role for Tumor Necrosis Factor-α
Tissue and in vitro studies seem to suggest a role for TNFα in the immunopathogenesis of vitiligo. Serums studies, and to a lesser extent genetic studies, are conflicting. However, treatment studies do not support the use of TNFα inhibition as an effective therapeutic strategy. Insights on the dual function of TNFα could partly explain these discrepancies.
The inflammatory effects of TNFα and its role in tissue injury in diverse pathologies are well known. However, TNFα has also been shown to induce tissue repair and to promote cell survival, as in the case of central and peripheral nervous system injuries [65, 66]. In cancer biology, TNFα is well known to possess anti-cancer activity, but recent findings suggest that it may also promote cancer development and progression [67]. In wound repair studies, an initial inflammatory response mediated by cytokines such as TNFα ultimately leads the way towards adequate wound healing [68]. In the heart, TNF receptor activation can lead both to myocyte injury and to increased resistance to apoptosis, depending on the cellular microenvironment [69]. The complexity of TNFα signaling, and its dual effects in both injury and repair, could explain the clinical failure of TNFα inhibition in diseases where pre-clinical studies strongly suggested a role for TNFα in their pathogenesis, such as heart failure, multiple sclerosis, asthma, or dermatomyositis [70].
The transcription factor NF-κB could be important for explaining these observations. TNFα is able to induce NF-κB in a complex crosstalk of TNF-receptor signaling [71], and NF-κB is known to be a key regulator of the expression of cell survival and repair genes. In the case of vitiligo, reduced NF-κB activation is known to result in increased susceptibility to apoptosis in vitiliginous keratinocytes [43], and NF-κB can mediate the transcription of antiapoptotic factors which may block TNFα-induced apoptosis in melanocytes [36]. The finding of increased TNFα in affected skin of patients with vitiligo after treatment with ultraviolet B also suggests a role for TNFα in repigmentation [64].
Although TNFα-induced inhibition of melanogenesis is well established, TNFα could also have a dual role in the pigmentation process. TNFα is constitutively expressed in both normal and perturbed dermis and epidermis, which suggests it plays a role in skin homeostasis [72]. Endothelin-1 (ET-1) and stem cell factor (SCF) are melanogenic factors produced in response to various stimuli, capable of modulating inflammation-induced hyperpigmentation [37]. Both ET-1 and SCF mRNA has been found to be reduced in vitiliginous skin in correlation with increased levels of TNFα [16]. However, studies have shown that TNFα can stimulate the production of ET-1 in skin, leading to enhanced pigmentation in seborrhoeic keratosis [73]. Furthermore, TNFα is able to stimulate SCF production in normal human keratinocytes [74]. In discussing the role of an altered redox state in vitiligo we reviewed evidence showing that TNFα can induce NO production in melanocytes. NO is also melanogenic factor produced from cells surrounding melanocytes in response to ultraviolet irradiation, and also plays a role in intracellular signal transduction pathways regulating melanogenesis [37, 75]. Thus, TNFα could play a dual role in vitiligo as well, acting on different cell populations and at different timepoints, both in promoting melanocyte injury and inhibiting melanogenesis on one hand, and promoting their survival and function on the other (Fig. 1).
8 Conclusion
The immunopathogenesis of vitiligo is complex and not completely understood. Plasma and peripheral blood cell studies of TNFα levels in vitiligo have given conflicting results. Genetic and tissue studies do suggest that TNFα might play an important role in the development of vitiliginous lesions, although with some heterogeneity as to its precise relevance. Furthermore, molecular mechanisms of TNFα-mediated melanocyte dysfunction and death have been uncovered using in vitro methods. A dual role for TNFα could explain the lack of clinical effectiveness of TNFα inhibition therapy in vitiligo. However, abandoning this promising strategy would be premature. Treatment individualization, patient selection (possibly including genotypic or phenotypic variables) as well as taking into account different time periods in treatment (acute, subacute, or chronic), could lead to positive results, and further studies will be required to clarify these issues.
References
Guerra L, Dellambra E, Brescia S, Raskovic D. Vitiligo: pathogenetic hypotheses and targets for current therapies. Curr Drug Metab. 2010;11:451–67.
Passeron T, Ortonne JP. Physiopathology and genetics of vitiligo. J Autoimmun. 2005;25(Suppl):63–8.
Sandoval-Cruz M, García-Carrasco M, Sánchez-Porras R, Mendoza-Pinto C, Jiménez-Hernández M, Munguía-Realpozo P, Ruiz-Argüelles A. Immunopathogenesis of vitiligo. Autoimmun Rev. 2011;10:762–5.
Glassman SJ. Vitiligo, reactive oxygen species and T-cells. Clin Sci (Lond). 2011;120:99–120.
Dwivedi M, Laddha NC, Arora P, Marfatia YS, Begum R. Decreased regulatory T-cells and CD4+/CD8+ ratio correlate with disease onset and progression in patients with generalized vitiligo. Pigment Cell Melanoma Res. 2013 (in press). doi:10.1111/pcmr.12105.
Pichler R, Sfetsos K, Badics B, Gutenbrunner S, Berg J, Auböck J. Lymphocyte imbalance in vitiligo patients indicated by elevated CD4+/CD8+ T-cell ratio. Wien Med Wochenschr. 2009;159:337–41.
Shi F, Erf GF. IFN-γ, IL-21, and IL-10 co-expression in evolving autoimmune vitiligo lesions of Smyth line chickens. J Invest Dermatol. 2012;132:642–9.
Moretti S, Spallanzani A, Amato L, Hautmann G, Gallerani I, Fabiani M, Fabbri P. New insights into the pathogenesis of vitiligo: imbalance of epidermal cytokines at sites of lesions. Pigment Cell Res. 2002;15:87–92.
Bashir MM, Sharma MR, Werth VP. TNF-alpha production in the skin. Arch Dermatol Res. 2009;301:87–91.
Yu HS, Chang KL, Yu CL, Li HF, Wu MT, Wu CS, Wu CS. Alterations in IL-6, IL-8, GM-CSF, TNF-alpha, and IFN-gamma release by peripheral mononuclear cells in patients with active vitiligo. J Invest Dermatol. 1997;108:527–9.
Tu CX, Gu JS, Lin XR. Increased interleukin-6 and granulocyte-macrophage colony stimulating factor levels in the sera of patients with non-segmental vitiligo. J Dermatol Sci. 2003;31:73–8.
Singh S, Singh U, Pandey SS. Serum concentration of IL-6, IL-2, TNF-α, and IFNγ in Vitiligo patients. Indian J Dermatol. 2012;57:12–4.
Zailaie MZ. Decreased proinflammatory cytokine production by peripheral blood mononuclear cells from vitiligo patients following aspirin treatment. Saudi Med J. 2005;26:799–805.
Laddha NC, Dwivedi M, Begum R. Increased tumor necrosis factor (TNF)-α and its promoter polymorphisms correlate with disease progression and higher susceptibility towards vitiligo. PLoS ONE. 2012;7:e52298.
Grimes PE, Morris R, Avaniss-Aghajani E, Soriano T, Meraz M, Metzger A. Topical tacrolimus therapy for vitiligo: therapeutic responses and skin messenger RNA expression of proinflammatory cytokines. J Am Acad Dermatol. 2004;51:52–61.
Moretti S, Fabbri P, Baroni G, Berti S, Bani D, Berti E, Nassini R, Lotti T, Massi D. Keratinocyte dysfunction in vitiligo epidermis: cytokine microenvironment and correlation to keratinocyte apoptosis. Histol Histopathol. 2009;24:849–57.
Birol A, Kisa U, Kurtipek GS, Kara F, Kocak M, Erkek E, Caglayan O. Increased tumor necrosis factor alpha (TNF-alpha) and interleukin 1 alpha (IL1-alpha) levels in the lesional skin of patients with nonsegmental vitiligo. Int J Dermatol. 2006;45:992–3.
Seif El Nasr H, Shaker OG, Fawzi MM, El-Hanafi G. Basic fibroblast growth factor and tumour necrosis factor alpha in vitiligo and other hypopigmented disorders: suggestive possible therapeutic targets. J Eur Acad Dermatol Venereol. 2013;27:103–8.
Wańkowicz-Kalińska A, van den Wijngaard RM, Tigges BJ, Westerhof W, Ogg GS, Cerundolo V, Storkus WJ, Das PK. Immunopolarization of CD4+ and CD8+ T cells to Type-1-like is associated with melanocyte loss in human vitiligo. Lab Invest. 2003;83:683–95.
Kim NH, Torchia D, Rouhani P, Roberts B, Romanelli P. Tumor necrosis factor-α in vitiligo: direct correlation between tissue levels and clinical parameters. Cutan Ocul Toxicol. 2011;30:225–7.
Yazici AC, Erdal ME, Kaya TI, Ikizoglu G, Savasoglu K, Camdeviren H, Tursen U. Lack of association with TNF-alpha-308 promoter polymorphism in patients with vitiligo. Arch Dermatol Res. 2006;298:46–9.
Namian AM, Shahbaz S, Salmanpoor R, Namazi MR, Dehghani F, Kamali-Sarvestani E. Association of interferon-gamma and tumor necrosis factor alpha polymorphisms with susceptibility to vitiligo in Iranian patients. Arch Dermatol Res. 2009;301:21–5.
Salinas-Santander M, Díaz-García D, Rojas-Martínez A, Cantú-Salinas C, Sánchez-Domínguez C, Reyes-López M, Cerda-Flores RM, Ocampo-Candiani J, Ortiz-López R. Tumor necrosis factor-α −308G/A polymorphism is associated with active vitiligo vulgaris in a northeastern Mexican population. Exp Ther Med. 2012;3:893–7.
Smith KJ, Diwan H, Skelton H. Death receptors and their role in dermatology, with particular focus on tumor necrosis factor-related apoptosis-inducing ligand receptors. Int J Dermatol. 2003;42:3–17.
Larribere L, Khaled M, Tartare-Deckert S, Busca R, Luciano F, Bille K, Valony G, Eychene A, Auberger P, Ortonne JP, Ballotti R, Bertolotto C. PI3K mediates protection against TRAIL-induced apoptosis in primary human melanocytes. Cell Death Differ. 2004;11:1084–91.
Kroll TM, Bommiasamy H, Boissy RE, Hernandez C, Nickoloff BJ, Mestril R. Caroline Le Poole I. 4-Tertiary butyl phenol exposure sensitizes human melanocytes to dendritic cell-mediated killing: relevance to vitiligo. J Invest Dermatol. 2005;124:798–806.
Morelli JG, Norris DA. Influence of inflammatory mediators and cytokines on human melanocyte function. J Invest Dermatol. 1993;100:191S–5S.
Zhang S, Liu S, Yu N, Xiang L. RNA released from necrotic keratinocytes upregulates intercellular adhesion molecule-1 expression in melanocytes. Arch Dermatol Res. 2011;303:771–6.
Norris DA. Cytokine modulation of adhesion molecules in the regulation of immunologic cytotoxicity of epidermal targets. J Invest Dermatol. 1990;95:111S–20S.
Hedley SJ, Metcalfe R, Gawkrodger DJ, Weetman AP, Mac Neil S. Vitiligo melanocytes in long-term culture show normal constitutive and cytokine-induced expression of intercellular adhesion molecule-1 and major histocompatibility complex class I and class II molecules. Br J Dermatol. 1998;139:965–73.
Martínez-Esparza M, Jiménez-Cervantes C, Solano F, Lozano JA, García-Borrón JC. Mechanisms of melanogenesis inhibition by tumor necrosis factor-alpha in B16/F10 mouse melanoma cells. Eur J Biochem. 1998;255:139–46.
Swope VB, Abdel-Malek Z, Kassem LM, Nordlund JJ. Interleukins 1 alpha and 6 and tumor necrosis factor-alpha are paracrine inhibitors of human melanocyte proliferation and melanogenesis. J Invest Dermatol. 1991;96:180–5.
Englaro W, Bahadoran P, Bertolotto C, Buscà R, Dérijard B, Livolsi A, Peyron JF, Ortonne JP, Ballotti R. Tumor necrosis factor alpha-mediated inhibition of melanogenesis is dependent on nuclear factor kappa B activation. Oncogene. 1999;18:1553–9.
Kotobuki Y, Tanemura A, Yang L, Itoi S, Wataya-Kaneda M, Murota H, Fujimoto M, Serada S, Naka T, Katayama I. Dysregulation of melanocyte function by Th17-related cytokines: significance of Th17 cell infiltration in autoimmune vitiligo vulgaris. Pigment Cell Melanoma Res. 2012;25:219–30.
Lee KY, Jeon SY, Hong JW, Choi KW, Lee CY, Kim JH, Song KH, Kim KH. Endothelin-1 enhances the proliferation of normal human melanocytes in a paradoxical manner from the TNF-α-inhibited condition, but tacrolimus promotes exclusively the cellular migration without proliferation: a proposed action mechanism for combination therapy of phototherapy and topical tacrolimus in vitiligo treatment. J Eur Acad Dermatol Venereol. 2012;27:609–16.
Krasagakis K, Garbe C, Eberle J, Orfanos CE. Tumour necrosis factors and several interleukins inhibit the growth and modulate the antigen expression of normal human melanocytes in vitro. Arch Dermatol Res. 1995;287:259–65.
Slominski A, Tobin DJ, Shibahara S, Wortsman J. Melanin pigmentation in mammalian skin and its hormonal regulation. Physiol Rev. 2004;84:1155–228.
Funasaka Y, Chakraborty AK, Hayashi Y, Komoto M, Ohashi A, Nagahama M, Inoue Y, Pawelek J, Ichihashi M. Modulation of melanocyte-stimulating hormone receptor expression on normal human melanocytes: evidence for a regulatory role of ultraviolet B, interleukin-1alpha, interleukin-1beta, endothelin-1 and tumour necrosis factor-alpha. Br J Dermatol. 1998;139:216–24.
Martínez-Esparza M, Jiménez-Cervantes C, Solano F, Lozano JA, García-Borrón JC. Regulation of the murine silver locus product (gp87) by the hypopigmenting cytokines TGF-beta1 and TNF-alpha. Pigment Cell Res. 2000;13:120–6.
Wang CQ, Akalu YT, Suarez-Farinas M, Gonzalez J, Mitsui H, Lowes MA, Orlow SJ, Manga P, Krueger JG. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: potential relevance to psoriasis. J Invest Dermatol. 2013 (in press). doi:10.1038/jid.2013.237.
Shang J, Eberle J, Geilen CC, Hossini AM, Fecker LF, Orfanos CE, Tebbe B. The role of nuclear factor-kappa B and melanogenesis in tumor necrosis factor-alpha-induced apoptosis of normal human melanocytes. Skin Pharmacol Appl Skin Physiol. 2002;15:321–9.
Lee AY. Role of keratinocytes in the development of vitiligo. Ann Dermatol. 2012;24:115–25.
Kim NH, Jeon S, Lee HJ, Lee AY. Impaired PI3K/Akt activation-mediated NF-kappaB inactivation under elevated TNF-alpha is more vulnerable to apoptosis in vitiliginous keratinocytes. J Invest Dermatol. 2007;127:2612–7.
Laddha NC, Dwivedi M, Mansuri MS, Gani AR, Ansarullah M, Ramachandran AV, Dalai S, Begum R. Vitiligo: interplay between oxidative stress and immune system. Exp Dermatol. 2013;22:245–50.
Jiménez-Cervantes C, Martínez-Esparza M, Pérez C, Daum N, Solano F, García-Borrón JC. Inhibition of melanogenesis in response to oxidative stress: transient downregulation of melanocyte differentiation markers and possible involvement of microphthalmia transcription factor. J Cell Sci. 2001;114:2335–44.
Young CN, Koepke JI, Terlecky LJ, Borkin MS, Boyd Savoy L, Terlecky SR. Reactive oxygen species in tumor necrosis factor-alpha-activated primary human keratinocytes: implications for psoriasis and inflammatory skin disease. J Invest Dermatol. 2008;128:2606–14.
Meier B, Radeke HH, Selle S, Younes M, Sies H, Resch K, Habermehl GG. Human fibroblasts release reactive oxygen species in response to interleukin-1 or tumour necrosis factor-alpha. Biochem J. 1989;263:539–45.
Schmidt KN, Amstad P, Cerutti P, Baeuerle PA. The roles of hydrogen peroxide and superoxide as messengers in the activation of transcription factor NF-kappa B. Chem Biol. 1995;2:13–22.
Rocha IM, Guillo LA. Lipopolysaccharide and cytokines induce nitric oxide synthase and produce nitric oxide in cultured normal human melanocytes. Arch Dermatol Res. 2001;293:245–8.
Viard-Leveugle I, Gaide O, Jankovic D, Feldmeyer L, Kerl K, Pickard C, Roques S, Friedmann PS, Contassot E, French LE. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Invest Dermatol. 2013;133:489–98.
Kim JJ, Lee SB, Park JK, Yoo YD. TNF-alpha-induced ROS production triggering apoptosis is directly linked to Romo1 and Bcl-X(L). Cell Death Differ. 2010;17:1420–34.
Lv Y, Li Q, Wang L, Gao T. Use of anti-tumor necrosis factor agents: a possible therapy for vitiligo. Med Hypotheses. 2009;72:546–7.
Simón JA, Burgos-Vargas R. Vitiligo improvement in a patient with ankylosing spondylitis treated with infliximab. Dermatology. 2008;216:234–5.
Campanati A. Giuliodori K, Ganzetti G, Liberati G, Offidani AM. A patient with psoriasis and vitiligo treated with etanercept. Am J Clin Dermatol. 2010;11:46–8.
Rigopoulos D, Gregoriou S, Larios G, Moustou E, Belayeva-Karatza E, Kalogeromitros D. Etanercept in the treatment of vitiligo. Dermatology. 2007;215:84–5.
Alghamdi KM, Khurrum H, Taieb A, Ezzedine K. Treatment of generalized vitiligo with anti-TNF-α Agents. J Drugs Dermatol. 2012;11:534–9.
Exarchou SA, Voulgari PV, Markatseli TE, Zioga A, Drosos AA. Immune-mediated skin lesions in patients treated with anti-tumour necrosis factor alpha inhibitors. Scand J Rheumatol. 2009;38:328–31.
Alghamdi KM, Khurrum H, Rikabi A. Worsening of vitiligo and onset of new psoriasiform dermatitis following treatment with infliximab. J Cutan Med Surg. 2011;15:280–4.
Song R, Kim S, Lee S, Lee Y, Hong S, Cho H, Kim G, Yang H. A case of development of vitiligo followed by TNF-α antagonist treatment for rheumatoid arthritis. J Rheum Dis. 2012;19:216–9.
Ismail WA, Al-Enzy SA, Alsurayei SA, Ismail AE. Vitiligo in a patient receiving infliximab for refractory ulcerative colitis. Arab J Gastroenterol. 2011;12:109–11.
Lahita RG, Vernace MA. Vasculitis, vitiligo, thyroiditis, and altered hormone levels after anti-tumor necrosis factor therapy. J Rheumatol. 2011;38:579–80.
Smith DI, Heffernan MP. Vitiligo after the resolution of psoriatic plaques during treatment with adalimumab. J Am Acad Dermatol. 2008;58:S50–2.
Atzeni F, Talotta R, Salaffi F, Cassinotti A, Varisco V, Battellino M, Ardizzone S, Pace F, Sarzi-Puttini P. Immunogenicity and autoimmunity during anti-TNF therapy. Autoimmun Rev. 2013;12:703–8.
Attwa E, Gamil H, Assaf M, Ghonemy S. Over-expression of tumor necrosis factor-α in vitiligo lesions after narrow-band UVB therapy: an immunohistochemical study. Arch Dermatol Res. 2012;304:823–30.
Shohami E, Ginis I, Hallenbeck JM. Dual role of tumor necrosis factor alpha in brain injury. Cytokine Growth Factor Rev. 1999;10:119–30.
Cámara-Lemarroy CR, Guzmán-de la Garza FJ, Fernández-Garza NE. Molecular inflammatory mediators in peripheral nerve degeneration and regeneration. Neuroimmunomodulation. 2010;17:314–24.
Bertazza L, Mocellin S. The dual role of tumor necrosis factor (TNF) in cancer biology. Curr Med Chem. 2010;17:3337–52.
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601.
Jiang B, Liao R. The paradoxical role of inflammation in cardiac repair and regeneration. J Cardiovasc Transl Res. 2010;3:410–6.
Karampetsou MP, Liossis SN, Sfikakis PP. TNF-α antagonists beyond approved indications: stories of success and prospects for the future. QJM. 2010;103:917–28.
Heyninck K, Beyaert R. Crosstalk between NF-kappaB-activating and apoptosis-inducing proteins of the TNF-receptor complex. Mol Cell Biol Res Commun. 2001;4:259–65.
Kilgus O, Payer E, Schreiber S, Elbe A, Strohal R, Stingl G. In vivo cytokine expression in normal and perturbed murine skin—analysis by competitive quantitative polymerase chain reaction. J Invest Dermatol. 1993;100:674–80.
Manaka L, Kadono S, Kawashima M, Kobayashi T, Imokawa G. The mechanism of hyperpigmentation in seborrhoeic keratosis involves the high expression of endothelin-converting enzyme-1alpha and TNF-alpha, which stimulate secretion of endothelin 1. Br J Dermatol. 2001;145:895–903.
Takenaka Y, Hoshino Y, Nakajima H, Hayashi N, Kawashima M, Imokawa G. Paracrine cytokine mechanisms underlying the hyperpigmentation of seborrheic keratosis in covered skin areas. J Dermatol. 2013 (in press). doi:10.1111/1346-8138.12178.
Lassalle MW, Igarashi S, Sasaki M, Wakamatsu K, Ito S, Horikoshi T. Effects of melanogenesis-inducing nitric oxide and histamine on the production of eumelanin and pheomelanin in cultured human melanocytes. Pigment Cell Res. 2003;16:81–4.
Acknowledgments
No sources of funding were used to prepare this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camara-Lemarroy, C.R., Salas-Alanis, J.C. The Role of Tumor Necrosis Factor-α in the Pathogenesis of Vitiligo. Am J Clin Dermatol 14, 343–350 (2013). https://doi.org/10.1007/s40257-013-0039-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-013-0039-3