Abstract
Purpose of Review
Anemia is a frequent complication in patients suffering from traumatic brain injury (TBI) or subarachnoid hemorrhage (SAH) and has been associated with poor outcome. Interestingly, red blood cell transfusion (RBCT), which is the most common therapeutic intervention in anemic brain-injured patients, was also reported as an independent predictor of mortality in several studies. The aim of this review was to summarize the current literature on the use of RBCT in brain-injured patients and to provide some insights on how to optimize their use in this setting.
Recent Findings
In moderately anemic TBI/SAH patients, RBCT could increase hemoglobin (Hb) levels while the effects on cerebral oxygenation were modest and inconsistent, raising serious concerns about the effectiveness and the risk/benefit ratio of this intervention. The optimal Hb level to trigger RBCT in TBI and SAH patients has not been defined yet. Thus, in those patients who are awake and without any further neurological deterioration, RBCT should be initiated as in other critically ill patients, e.g., for Hb levels below 7 g/dL. In case of poor-grade clinical status, the use of indicators of inadequate systemic oxygen delivery (e.g., low venous hemoglobin saturation or high lactate levels) or of brain hypoxia (e.g., low regional hemoglobin saturation or brain oxygen pressure) may be helpful to guide RBCT. Nevertheless, there is no evidence to provide strong recommendations based on this strategy to initiate transfusions in this patients’ population.
Summary
Few good quality data exist about the effects of RBCT on the outcome of TBI and SAH patients. While randomized trials will be initiated, the optimal Hb level to trigger RBCT in these patients may be related to the clinical status or on systemic and/or cerebral monitoring values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute brain injury, which is mainly represented by traumatic brain injury (TBI), subarachnoid hemorrhage (SAH), and ischemic/hemorrhagic stroke, is a frequent condition among patients admitted to the intensive care unit (ICU) [1–3]. Patients suffering from acute brain injury are vulnerable to secondary brain damages following the primary injury, such as hyperthermia, arterial hypotension, hypoglycemia, or hypoxemia, which will contribute to neuronal death and poor functional recovery [4]. Given the increased susceptibility of the injured brain to secondary insults, avoiding ischemia is of major concern when dealing with neurocritically ill patients. Hemoglobin concentration is one of the determinants of brain oxygen delivery according to the following equation:
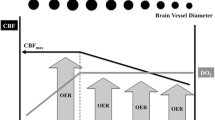
where DO2 is the oxygen delivery to brain, [Hb] is the concentration of hemoglobin, SaO2 is the oxygen saturation of hemoglobin, PaO2 is the oxygen partial pressure, and CBF is the cerebral blood flow. Hence, according to this equation, a significant reduction of Hb concentrations may lead to decreased brain DO2 and eventually tissue hypoxia, if the compensatory mechanisms aiming to keep a constant tissue oxygenation fail [5].
About two-thirds of patients admitted to a general ICU are anemic on admission; almost one-third of them have hemoglobin level below 10 g/dL [6, 7]. In this setting, many factors can contribute to the development of anemia, such as frequent blood sampling, blood losses (clinically apparent or occult) (10), hemodilution, shortened red blood cells survival, and impaired erythropoiesis [8]. Anemia has been shown to be an independent predictor of poor outcome in many ICU populations [9]. Nevertheless, blood transfusions, which is the most common therapy given to correct anemia to increase Hb levels and is required in almost half of critically ill patients [6], are also associated with several complications and have been associated with poor outcome in several studies, including neurocritically ill patients [10]. Reasons for this “paradox” are complex and may include, among all, the association of red blood cells transfusions (RBCT) with the occurrence of oxidative injuries, arterial hypoxemia due to transfusion-associated circulatory overload (TACO), or transfusion-related acute lung injury (TRALI) or the so-called “TRIM” (transfusion-related immune modulation) effects, which increase the risk of hospital-acquired infections [10–12]. In this review, we summarized current knowledge about transfusion practices in patients with acute brain injury, with particular attention to TBI and SAH. A practical approach to transfusion therapy in those patients has also been suggested.
The Effects of Red Blood Cells Transfusions on Critically Ill Patients
Transfusion practices in the critically ill patients are based on a number of prospective and retrospective studies conducted in the last 15 years in different patient settings. In the landmark “TRICC” (Transfusion Requirements In Critical Care) trial, ICU patients assigned to a restrictive transfusion strategy (transfusion if Hb level was below 7 g/dL) had similar 30-day mortality rates (and even lower mortality in subgroups with APACHE II <20 and patients younger than age 55 years) than patients transfused according to a more liberal strategy (if Hb level <10 g/dL) [13]. The safety of a “restrictive” transfusion policy was confirmed in other studies evaluating septic shock, gastrointestinal bleeding, or elderly patients with cardiovascular disease undergoing hip surgery [14–16]. Even in stable pediatric critically ill patients, an Hb threshold of 7 g/dL to initiate RBCT could decrease transfusion requirements without increasing adverse outcomes [17]. Results are more conflicting in cardiac surgery patients; as such, a recent randomized trial showed that the occurrence of infection (primary outcome) was similar between patients in the “restrictive-threshold group” (e.g., transfusion if Hb < 7.5 g/dL) and those in the “liberal-threshold group” (e.g., transfusion if Hb < 10.0 g/dL); however, mortality was higher in the “restrictive” group (4.2 vs. 2.6 %; p = 0.045) [18].
The Effects of Red Blood Cells Transfusions on Brain-Injured Patients
In the case of brain injury, the adaptive mechanisms (e.g., cerebral vasodilation, decreased viscosity, increased cardiac output, and oxygen extraction) to maintain an adequate DO2 during anemia are altered and may result in cerebral hypoxia at higher Hb thresholds than in other ICU populations [5]. In a retrospective study on TBI patients, patients with Hb < 10 g/dL during their ICU stay (anemic group—2 % on admission and 48 % during the first week) had a higher in-hospital mortality than nonanemic patients (25 % vs. 6 %, p = 0.01); nevertheless, only RBCT, and not anemia, was an independent predictor of poor outcome [19]. Similarly, mean 7-day Hb levels below 9 g/dL were independently associated with an increased risk of hospital mortality in a retrospective cohort of 273 TBI patients [20•]. In another retrospective study on TBI patients (n = 116), an increased time during which Hb levels exceeded the threshold of 9 g/dL was associated with improved neurological outcome [21•]. On the opposite, Salim et al. showed that anemia (Hb ≤ 9 g/dL on 3 consecutive blood draws) was associated with poor outcome after TBI; however, in a multivariable analysis, only RBCT independently predicted mortality and an increased risk of complications [22]. Finally, Okoye et al. showed that anemia (Hb ≤ 8 g/dL) was not associated with an increase in mortality or other complications in isolated TBI [23].
In patients suffering from SAH, the occurrence of symptomatic vasospasm was significantly associated with Hb levels below 11 g/dL in the postoperative period [24•]. These findings were confirmed in another retrospective study on 130 patients suffering from aneurysmal SAH, where lower mean Hb levels were found in patients with cerebral vasospasm and was an independent predictor of poor outcome [25]. In another study, low mean Hb levels were associated with unfavorable outcome after SAH (n = 702), with the best Hb cut-off to predict outcome at 11.1 g/dL [26]. In a retrospective study, Naidech et al. showed that Hb levels remained significantly lower in nonsurvivors when compared to survivors during the first week after SAH (n = 103); also, low Hb levels remained associated with poor outcome even after adjustment for several confounders, including Hunt and Hess grade and the occurrence of vasospasm [27]. These results suggest that the impact of anemia may be dependent on the underlying brain disease; if in TBI patients, data suggest a controversial association of poor outcome with Hb concentrations below 9 g/dL, in SAH patients, in particular in case of vasospasm, the cut-off of Hb independently associated with mortality appeared much higher, around 11 g/dL. However, most of clinical studies were retrospective and potentially presented significant selection biases. Furthermore, the impact of length of exposition to anemia, timing of anemia development (early vs. late), and the relationship of anemia with RBCT needs to be clarified yet.
Importantly, taken these considerations all together, one may argue that current recommendations on the use of a restrictive transfusion strategy in ICU patients (e.g., when Hb levels are below 7 g/dL in the absence of significant heart disease) [28] may not apply to patients with TBI or SAH. Nevertheless, it remains unclear whether increasing Hb levels to 9–10 g/dL using RBCT would be a logical therapeutic decision to improve cerebral oxygenation and neurological recovery. In patients with TBI, the increase in brain oxygen pressure (PbtO2) after RBCT was generally limited. In one study, an increase in PbtO2 was observed in 26/35 (74 %) patients; the mean increase in PbtO2 was around 3 mmHg from baseline at 1 h after RBCT administration [29•]. In another study (n = 30), 57 % of them experienced an increase in PbtO2 after RBCT, with change in Hb levels being significantly associated with change in PbtO2 [30]. More recently, Yamal et al. showed brain tissue hypoxia (e.g., PbtO2 < 20 mmHg) events were not significantly different between patients receiving RBCT at two Hb thresholds (7 g/dL vs. 10 g/dL) [31•]. Moreover, in these studies, there were no clear factors predicting “responders” and “nonresponders” (on the basis of PbtO2 changes) to RBCT. Few studies evaluated the impact of RBCT on brain oxygenation in poor-grade SAH; Kurtz et al. showed that each 1.0 g/dL increase in Hb levels after RBCT in such patients was associated with an increase in PbtO2 of 1.39 mmHg, without significant effects on cerebral metabolism (e.g., the lactate to pyruvate ratio—LPR—as a marker of anaerobic metabolism) [32•]. In a prospective study on anemic (Hb < 9 g/dL) SAH patients, the administration of one RBCT pack resulted in a significant improvement in cerebral DO2, which was assessed using positron emission tomography (PET) imaging [33]. Interestingly, these effects resulted in a reduction of oxygen extraction in those cerebral territories with the lowest baseline DO2. In a second study, the same authors compared the effects of 3 different interventions (e.g., fluid expansion, vasopressors, or RBCT) on brain DO2 in three different subgroups of poor-grade SAH patients [34••]; regional DO2 significantly increased in the three groups, but the effects were more important in patients receiving RBCT.
Studies evaluating RBCT as a predictor of outcome after TBI or SAH have also found conflicting results. In a large retrospective study in TBI patients (n = 1150), Salim et al. found that RBCT were given in almost half of them during the ICU stay and that RBCT were associated with increased hospital mortality in a multivariable analysis [22]. In another retrospective study in the same population, RBCT were also found as an independent risk factor for poor long-term neurological outcome [35]. On the opposite, in a smaller cohort (n = 82), there was no association between RBCT and poor neurological outcome after TBI [36]. In SAH patients, several studies on patients found an association between RBCT and worse neurological outcome, the occurrence of delayed cerebral ischemia or even increased mortality [37, 38]. However, these findings were not confirmed in all studies; Broessner et al. found no association between RBCT and neurological recovery in a multivariate analysis conducted on 292 SAH patients [39].
Optimal Hemoglobin Concentrations in TBI and SAH: Results from Randomized Trials and Common Practice
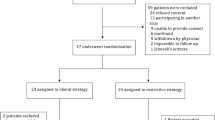
Only few studies compared the effects of a restrictive or a liberal transfusions strategy on the outcome of patients with TBI or SAH. In a post hoc analysis performed in the 67 TBI patients included in the TRICC trial, patients randomized to the “restrictive” RBCT policy (e.g., transfusion if Hb < 7.0 g/dL; n = 29) received less RBC units than those included in the “liberal” strategy (e.g., transfusion if Hb < 10.0 g/dL; n = 38), with a similar 30-day mortality (17 % vs. 13 %, p = 0.64), hospital length of stay, and the occurrence of organ dysfunction [13]. In a prospective randomized trial including 44 SAH patients, Naidech et al. evaluated the effects of RBCT initiated at Hb of 10 or 11.5 g/dL in those subjects at high risk of developing cerebral vasospasm [40••]; patients randomized to the higher Hb threshold received more transfusions than others but safety endpoints (e.g., infections and thromboembolic events) were not different between groups. The number of cerebral infarctions on brain imaging (6/20 vs. 9/22) and of patients showing a poor neurological recovery was lower, although not statistically significant, in the higher Hb threshold group. In a more recent study, Robertson et al. investigated the effects of two different thresholds of Hb to guide RBCT (7 vs. 10 g/dL) in TBI patients [41••]. On a total of 200 patients, favorable outcome was similar between patients included in the 7 g/dL (37/87) or in the 10 g/dL group (31/94); moreover, thromboembolic events were significantly more frequent in the group transfused at 10 g/dL than others (22/101 [22 %] vs. 8/99 [8 %]; p = 0.009). These studies, although underpowered and with significant methodological issues, showed no particular benefit in maintaining high Hb levels in patients suffering from severe TBI or SAH. Two surveys, evaluating either TBI or SAH patients, were conducted in North America and evaluated the factors that could influence transfusion threshold in this setting. In the first study, two clinical scenarios (a TBI comatose patients either with or without intracranial hypertension) were proposed to trauma surgeons, neurosurgeons, and ICU physicians from the US trauma centers (n = 187) [42•]. Interestingly, neurosurgeons used a greater mean Hb threshold to initiate RBCT than trauma surgeons and ICU physicians, independently from the presence of intracranial hypertension. Moreover, neurosurgeons used less indicators of poor anemia tolerance, such as increased lactate, low mixed venous saturation, or PbtO2, than others to decide for RBCT. In a second study conducted in North America, physicians taking care of SAH patients in academic hospitals were inquired on the common triggers to initiate RBCT in SAH patients [43•]. Mean Hb concentrations at which clinicians administered RBCT progressively increased from an uncomplicated case to a poor-grade patient (7.8 vs. 8.2 g/dL), in particular in case of cerebral vasospasm and delayed cerebral ischemia. Again, neurosurgeons expressed the highest minimum Hb to initiate RBCT among all responders. The presence of low PbtO2 (<15 mmHg) and high LPR (>40) were also important triggers to administer RBCT in this setting.
How to Optimize Blood Transfusion
Currently, there are few alternatives to RBCT for anemic brain-injured patients. Although recent studies suggested some benefits from erythropoiesis-stimulating agents in TBI patients [44], there is an urgent need to optimize the use of RBCT in such patients and physicians should consider the potential benefits on avoiding secondary brain hypoxia as well as the detrimental effects on the development of complications when correcting anemia in this setting. If patients are awake and could be repeatedly examined, Hb levels could be titrated according to the occurrence of neuroworsening (NW) and only when NW is suspected to be secondary to tissue hypoxia. In all comatose or poor-grade patients, the use of advanced systemic and cerebral monitoring could help to better titrate the decision to administer RBCT (Fig. 1).
A practical approach to guide red blood cells transfusion (RBCT) in patients suffering from traumatic brain injury (TBI) or subarachnoid hemorrhage (SAH). In awake patients without any deterioration of their neurological status, a restrictive strategy (e.g., RBCT for hemoglobin—Hb—levels below 7 g/dL) should be considered. In case of comatose patients, indicators of low systemic oxygen delivery (DO2), such as low venous Hb saturation (SvO2/SvcO2), impaired microcirculation or high lactate levels, or of cerebral hypoxia, such as low jugular venous saturation (SvjO2), cerebral regional oxygen saturation (rSO2), or brain oxygen pressure (PbtO2), could be used to guide RBCT
Systemic indicators of poorly tolerated anemia could be used in clinical practice to decide for RBCT administration. As such, in case of inadequate oxygen delivery, as suggested by a mixed (SvO2) or superior vena cava (ScvO2) oxygen saturation <65–70 %, RBCT could be useful to improve tissue oxygenation, if hypovolemia has been previously excluded, as shown in patients with sepsis [45]. Although there are no studies showing that this approach would provide some benefits in patients with TBI or SAH, two retrospective studies have shown that early hemodynamic optimization (EHO) using a target ScvO2 of ≥65 % was associated with a trend toward reduced mortality and better neurological outcome in patients suffering from postanoxic brain injury [46, 47]. Importantly, the amount of RBCT and mean Hb levels were similar between patients receiving EHO when compared to controls, suggesting that the role of blood transfusion in this therapeutic strategy remains to be further clarified. Other indicators of impaired oxygen delivery may be lactate levels and altered peripheral microcirculation. In one study, Mazza et al. showed that, in septic patients receiving RBCT for an Hb threshold of 7 g/dL, blood transfusions could improve ScvO2 and concomitantly reduce lactate (from 2.4 to 2.2 mmol/L, p = 0.005) [48]. Similarly, Sakr et al. showed that, in septic patients with a critical reduction of capillary density in the sublingual area, RBCT could significantly improve microvascular flow [49]. Unfortunately, no data are available on the effects of RBCT on lactate levels and microcirculation in TBI and SAH patients. Thus, further studies are needed to validate such approach based on biomarkers of impaired DO2 to guide RBCT in this setting.
Monitoring of cerebral oxygenation and metabolism could also be helpful to titrate RBCT in TBI and SAH patients. Cerebral regional oxygen saturation (rSO2) assessed using near-infrared spectrometry (NIRS) devices is effective to evaluate the brain effects of anemia during elective heart surgery [50]. In preterms infants with symptomatic anemia (n = 23), RBCT improved cerebral oxygenation independently from the transfusion duration [51]. Similar results were found in patients suffering from sickle-cells disease or undergoing major abdominal surgery when RBCT was given [52, 53]. Venous saturation in the jugular vein (SvjO2) can also provide relevant information on the adequacy of CBF in patients with SAH or TBI [54, 55]. In one study, hemodilutional anemia (Hb between 5 and 7 g/dL) accentuated hypoxic cerebral injury following TBI in rats, although SvjO2 remained unaffected [56]. Furthermore, we lack of clinical studies evaluating the impact of RBCT on rSO2 and SvjO2 in TBI and SAH patients. Moreover, these two techniques present several pitfalls, in particular, the contamination from extracranial blood for the rSO2 measurement and the poor sensitivity of SvjO2 desaturation to detect regional brain hypoxia in these patients [57, 58].
Direct monitoring of tissue hypoxia via PbtO2 catheters has shown that only patients with anemia (Hb < 9 g/dL) and concomitant tissue hypoxia (e.g., PbtO2 < 20 mmHg) were at high risk of poor outcome after TBI [59•] and should be potentially considered as candidate for RBCT. The main limitation of such approach is that PbtO2 catheters are not available in all centers and give information only for a very limited area of the brain. Also, other possible causes for cerebral hypoxia, such as increased intracranial hypertension, severe hypocapnia, seizures, hyperthermia, and arterial hypoxemia, should be excluded before considering RBCT in the management of such patients.
Conclusions
Optimizing RBCT in TBI and SAH patients remains a significant challenge for clinicians. According to recommendations for other critically ill patients, a “restrictive” transfusion practice (e.g., RBCT for Hb < 7 g/dL) should be considered safe for brain-injured patients, at least for those who are awake and do not present worsening of their clinical status during repeated neurological examination. For those with poor-grade clinical status, the use of “systemic” (low SvO2/ScvO2, high lactate levels or impaired microcirculation) or “cerebral” (low rSO2, SvjO2 and PbtO2) indicators of cerebral hypoxia may be helpful to guide RBCT in this setting. However, this approach needs to be validated in large prospective studies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Phelan HA, Richter AA, Scott WW, Pruitt JH, Madden CJ, Rickert KL, Wolf SE. Does isolated traumatic subarachnoid hemorrhage merit a lower intensity level of observation than other traumatic brain injury? J Neurotrauma. 2014;31(20):1733–6.
Drazin D, Rosner J, Nuño M, Alexander MJ, Schievink WI, Palestrant D, Lyden PD, Miller C. Type of admission is associated with outcome of spontaneous subarachnoid hemorrhage. Int J Stroke. 2015;10(4):529–33.
Alonso A, Ebert AD, Kern R, Rapp S, Hennerici MG, Fatar M. Outcome predictors of acute stroke patients in need of intensive care treatment. Cerebrovasc Dis. 2015;40(1–2):10–7.
Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34(2):216–22.
Hare GM, Tsui AK, McLaren AT, Ragoonanan TE, Yu J, Mazer CD. Anemia and cerebral outcomes: many questions, fewer answers. Anesth Analg. 2008;107(4):1356–70.
Benson AB, Moss M, Silliman CC. Transfusion-related acute lung injury (TRALI): a clinical review with emphasis on the critically ill. Br J Haematol. 2009;147(4):431–43.
Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, Nollet G, Peres-Bota D. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288(12):1499–507.
Walsh TS, Saleh EE. Anaemia during critical illness. Br J Anaesth. 2006;97(3):278–91.
Raghavan M, Marik PE. Anemia, allogenic blood transfusion, and immunomodulation in the critically ill. Chest. 2005;127(1):295–307.
Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008;36(9):2667–74.
Vamvakas EC, Blajchman MA. Transfusion-related immunomodulation (TRIM): an update. Blood Rev. 2007;21(6):327–48.
Li G, Rachmale S, Kojicic M, Shahjehan K, Malinchoc M, Kor DJ, Gajic O. Incidence and transfusion risk factors for transfusion-associated circulatory overload among medical intensive care unit patients. Transfusion. 2011;51(2):338–43.
Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian critical care trials group. N Engl J Med. 1999;340(6):409–17.
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K, Macaulay W, Lewis C, Cook DR, Dobbin G, Zakriya KJ, Apple FS, Horney RA, Magaziner J. FOCUS investigators. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453–62.
Holst LB, Haase N, Wetterslev J, Wernerman J, Guttormsen AB, Karlsson S, Johansson PI, Aneman A, Vang ML, Winding R, Nebrich L, Nibro HL, Rasmussen BS, Lauridsen JR, Nielsen JS, Oldner A, Pettilä V, Cronhjort MB, Andersen LH, Pedersen UG, Reiter N, Wiis J, White JO, Russell L, Thornberg KJ, Hjortrup PB, Müller RG, Møller MH, Steensen M, Tjäder I, Kilsand K, Odeberg-Wernerman S, Sjøbø B, Bundgaard H, Thyø MA, Lodahl D, Mærkedahl R, Albeck C, Illum D, Kruse M, Winkel P, Perner A. TRISS trial group; Scandinavian critical care trials group. lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014;371(15):1381–91.
Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11–21.
Lacroix J, Hébert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, Gauvin F, Collet JP, Toledano BJ, Robillard P, Joffe A, Biarent D, Meert K, Peters MJ. TRIPICU investigators; Canadian critical care trials group; pediatric acute lung injury and sepsis investigators network. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356(16):1609–19.
Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, Reeves BC. TITRe2 investigators. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med. 2015;372(11):997–1008.
Al-Dorzi HM, Al-Humaid W, Tamim HM, Haddad S, Aljabbary A, Arifi A, Arabi YM. Anemia and blood transfusion in patients with isolated traumatic brain injury. Crit Care Res Pract. 2015;2015:672639.
• Sekhon MS, McLean N, Henderson WR, Chittock DR, Griesdale DE. Association of hemoglobin concentration and mortality in critically ill patients with severe traumatic brain injury. Crit Care. 2012;16(4):R128. One recent study evaluating the impact of anemia and red blood cells transfusion in a large cohort of TBI patients.
• Griesdale DE, Sekhon MS, Menon DK, Lavinio A, Donnelly J, Robba C, Sekhon IS, Taylor A, Henderson WR, Turgeon AF, Gupta AK. hemoglobin area and time index above 90 g/L are associated with improved 6-month functional outcomes in patients with severe traumatic brain injury. Neurocrit Care. 2015;23(1):78–84. This study evaluated the time exposure of TBI patients to low (<9 g/dL) haemoglobin levels and found that this variable was significantly associated with poor outcome.
Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L, Margulies DR. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207(3):398–406.
Okoye O, Inaba K, Kennedy M, Salim A, Talving P, Plurad D, Lam L, Demetriades D. The impact of anemia in moderate to severe traumatic brain injury. Eur J Trauma Emerg Surg. 2013;39(6):627–33.
• Sun J, Tan G, Xing W, He Z. Optimal hemoglobin concentration in patients with aneurysmal subarachnoid hemorrhage after surgical treatment to prevent symptomatic cerebral vasospasm. Neuroreport. 2015;26(5):263–6. In this study, the authors yielded that low haemoglobin levels were an independent predictor of poor outcome in SAH patients developing cerebral vasospasm.
Bell DL, Kimberly WT, Yoo AJ, Leslie-Mazwi TM, Rabinov JD, Bell JE, Mehta BP, Hirsch JA. Low neurologic intensive care unit hemoglobin as a predictor for intra-arterial vasospasm therapy and poor discharge modified Rankin scale in aneurysmal subarachnoid haemorrhage-induced cerebral vasospasm. J Neurointerv Surg. 2015;7(6):438–42.
Stein M, Brokmeier L, Herrmann J, Scharbrodt W, Schreiber V, Bender M, Oertel MF. Mean hemoglobin concentration after acute subarachnoid hemorrhage and the relation to outcome, mortality, vasospasm, and brain infarction. J Clin Neurosci. 2015;22(3):530–4.
Naidech AM, Drescher J, Ault ML, Shaibani A, Batjer HH, Alberts MJ. Higher hemoglobin is associated with less cerebral infarction, poor outcome, and death after subarachnoid hemorrhage. Neurosurgery. 2006;59(4):775–9.
Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, Holcomb JB, Illoh O, Kaplan LJ, Katz LM, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157(1):49–58.
• Smith MJ, Stiefel MF, Magge S, Frangos S, Bloom S, Gracias V, Le Roux PD. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med. 2005;33(5):1104–8. This is one of the first studies evaluating the effects of red blood cells transfusion on cerebral oxygenation in TBI patients. The results showed an increase in tissue oxygen pressure after transfusion, however the change was modest and not reported in all patients.
Zygun DA, Nortje J, Hutchinson PJ, Timofeev I, Menon DK, Gupta AK. The effect of red blood cell transfusion on cerebral oxygenation and metabolism after severe traumatic brain injury. Crit Care Med. 2009;37(3):1074–8.
• Yamal JM, Rubin ML, Benoit JS, Tilley BC, Gopinath S, Hannay HJ, Doshi P, Aisiku IP, Robertson CS. Effect of hemoglobin transfusion threshold on cerebral hemodynamics and oxygenation. J Neurotrauma. 2015;32(16):1239–45. The authors of this study showed that older blood transfusions had no adverse effect in severe traumatic brain injury.
• Kurtz P, Helbok R, Claassen J, Schmidt JM, Fernandez L, Stuart RM, Connolly ES, Lee K, Mayer SA, Badjatia N. The effect of packed red blood cell transfusion on cerebral oxygenation and metabolism after subarachnoid hemorrhage. Neurocrit Care 2016;24(1):118–21. In this study, red blood cells transfusions resulted in an improvement of cerebral oxygenation without a clear effect on cerebral metabolism among SAH patients.
Dhar R, Zazulia AR, Videen TO, Zipfel GJ, Derdeyn CP, Diringer MN. Red blood cell transfusion increases cerebral oxygen delivery in anemic patients with subarachnoid hemorrhage. Stroke. 2009;40(9):3039–44.
•• Dhar R, Scalfani MT, Zazulia AR, Videen TO, Derdeyn CP, Diringer MN: Comparison of induced hypertension, fluid bolus, and blood transfusion to augment cerebral oxygen delivery after subarachnoid hemorrhage. J Neurosurg. 2012;116(3):648–56. In this study, blood transfusions had a more significant impact on the improvement of oxygen delivery to vulnerable brain regions at risk for ischemia after SAH than intravenous fluids or vasopressor therapy.
Warner MA, O’Keeffe T, Bhavsar P, Shringer R, Moore C, Harper C, Madden CJ, Sarode R, Gentilello LM, Diaz-Arrastia R. Transfusions and long-term functional outcomes in traumatic brain injury. J Neurosurg. 2010;113(3):539–46.
George ME, Skarda DE, Watts CR, Pham HD, Beilman GJ. Aggressive red blood cell transfusion: no association with improved outcomes for victims of isolated traumatic brain injury. Neurocrit Care. 2008;8(3):337–43.
Tseng MY, Hutchinson PJ, Kirkpatrick PJ. Effects of fluid therapy following aneurysmal subarachnoid haemorrhage: a prospective clinical study. Br J Neurosurg. 2008;22(2):257–68.
Kramer AH, Gurka MJ, Nathan B, Dumont AS, Kassell NF, Bleck TP. Complications associated with anemia and blood transfusion in patients with aneurysmal subarachnoid hemorrhage. Crit Care Med. 2008;36(7):2070–5.
Broessner G, Lackner P, Hoefer C, Beer R, Helbok R, Grabmer C, Ulmer H, Pfausler B, Brenneis C, Schmutzhard E. Influence of red blood cell transfusion on mortality and long-term functional outcome in 292 patients with spontaneous subarachnoid hemorrhage. Crit Care Med. 2009;37(6):1886–92.
•• Naidech AM, Shaibani A, Garg RK, Duran IM, Liebling SM, Bassin SL, Bendok BR, Bernstein RA, Batjer HH, Alberts MJ. Prospective, randomized trial of higher goal hemoglobin after subarachnoid hemorrhage. Neurocrit Care. 2010;13(3):313–20. This is the only randomized clinical trial evaluating the effects of two different haemoglobin thresholds to initiate transfusions in SAH patients and their impact on outcome.
•• Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, Baldwin A, Rivera Lara L, Saucedo-Crespo H, Ahmed O et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47. This is the only randomized clinical trial evaluating the effects of two different haemoglobin thresholds to initiate transfusions in TBI patients and their impact on outcome.
• Sena MJ, Rivers RM, Muizelaar JP, Battistella FD, Utter GH: Transfusion practices for acute traumatic brain injury: a survey of physicians at US trauma centers. Intensive Care Med 2009;35(3):480–8. The only survey conducted in North America to evaluate the transfusion policy of different physicians to treat TBI patients.
• Kramer AH, Diringer MN, Suarez JI, Naidech AM, Macdonald LR, Le Roux PD: Red blood cell transfusion in patients with subarachnoid hemorrhage: a multidisciplinary North American survey. Crit Care. 2011;15(1):R30. The only survey conducted in North America to evaluate the transfusion policy of different physicians to treat SAH patients.
Nichol A, French C, Little L, Haddad S, Presneill J, Arabi Y, Bailey M, Cooper DJ, Duranteau J, Huet O, Mak A, McArthur C, Pettilä V, Skrifvars M, Vallance S, Varma D, Wills J, Bellomo R. EPO-TBI investigators; ANZICS clinical trials group. Erythropoietin in traumatic brain injury (EPO-TBI): a double-blind randomised controlled trial. Lancet. 2015;386(10012):2499–506.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Gaieski DF, Band RA, Abella BS, Neumar RW, Fuchs BD, Kolansky DM, Merchant RM, Carr BG, Becker LB, Maguire C, et al. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009;80(4):418–24.
Walters EL, Morawski K, Dorotta I, Ramsingh D, Lumen K, Bland D, Clem K, Nguyen HB. Implementation of a post-cardiac arrest care bundle including therapeutic hypothermia and hemodynamic optimization in comatose patients with return of spontaneous circulation after out-of-hospital cardiac arrest: a feasibility study. Shock. 2011;35(4):360–6.
Mazza BF, Freitas FG, Barros MM, Azevedo LC, Machado FR. Blood transfusions in septic shock: is 7.0 g/dL really the appropriate threshold? Rev Bras Ter Intensiva. 2015;27(1):36–43.
Sakr Y, Chierego M, Piagnerelli M, Verdant C, Dubois MJ, Koch M, Creteur J, Gullo A, Vincent JL, De Backer D. Microvascular response to red blood cell transfusion in patients with severe sepsis. Crit Care Med. 2007;35(7):1639–44.
Cem A, Serpil UO, Fevzi T, Murat O, Umit G, Esin E, Pinar U, Sahin S, Hasan K, Cem A. Efficacy of near-infrared spectrometry for monitoring the cerebral effects of severe dilutional anemia. Heart Surg Forum. 2014;17(3):E154–259.
Dani C, Pratesi S, Fontanelli G, Barp J, Bertini G. Blood transfusions increase cerebral, splanchnic, and renal oxygenation in anemic preterm infants. Transfusion. 2010;50(6):1220–6.
Quinn CT, Dowling MM. Cerebral tissue hemoglobin saturation in children with sickle cell disease. Pediatr Blood Cancer. 2012;59(5):881–7.
Green DW. A retrospective study of changes in cerebral oxygenation using a cerebral oximeter in older patients undergoing prolonged major abdominal surgery. Eur J Anaesthesiol. 2007;24(3):230–4.
Citerio G, Cormio M, Portella G, Vascotto E, Galli D, Gaini SM. Jugular saturation (SjvO2) monitoring in subarachnoid hemorrhage (SAH). Acta Neurochir Suppl. 1998;71:316–9.
Schoon P, Benito Mori L, Orlandi G, Larralde C, Radrizzani M. Incidence of intracranial hypertension related to jugular bulb oxygen saturation disturbances in severe traumatic brain injury patients. Acta Neurochir Suppl. 2002;81:285–7.
Hare GM, Mazer CD, Hutchison JS, McLaren AT, Liu E, Rassouli A, Ai J, Shaye RE, Lockwood JA, Hawkins CE, Sikich N, To K, Baker AJ. Severe hemodilutional anemia increases cerebral tissue injury following acute neurotrauma. J Appl Physiol. 2007;103(3):1021–9 (1985).
Davie SN, Grocott HP. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology. 2012;116(4):834–40.
Gopinath SP, Valadka AB, Uzura M, Robertson CS. Comparison of jugular venous oxygen saturation and brain tissue PO2 as monitors of cerebral ischemia after head injury. Crit Care Med. 1999;27(11):2337–45.
• Oddo M, Levine JM, Kumar M, Iglesias K, Frangos S, Maloney-Wilensky E, Le Roux PD. Anemia and brain oxygen after severe traumatic brain injury. Intensive Care Med 2012;38(9):1497–504. This is the first study showing that only when anemia (haemoglobin <9 g/dL) was associated with tissue hypoxia (low cerebral oxygen pressure), this was an independent predictor of poor outcome.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None to declare.
Additional information
This article is part of the Topical collection on Neuroanesthesia.
Rights and permissions
About this article
Cite this article
Crippa, I.A., Lelubre, C., Lozano-Roig, A. et al. Optimizing Blood Transfusion Practices in Traumatic Brain Injury and Subarachnoid Hemorrhage. Curr Anesthesiol Rep 6, 250–256 (2016). https://doi.org/10.1007/s40140-016-0169-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-016-0169-2