Abstract
Background
Clinical studies have caused blood transfusion practices in critically ill patients to become more conservative in the last decade. However, few studies have focused on trauma patients, particularly those with severe isolated traumatic brain injury.
Methods
We conducted a retrospective study to test the hypothesis that patients with severe brain injury would not benefit from aggressive red blood cell transfusion (RBCT). End points of the study were in-hospital mortality and morbidity (pneumonia, urinary tract infection, deep venous thrombosis, pulmonary embolus, decubitus ulcer, bacteremia, septic shock, myocardial infarction, and seizure). Included in our retrospective study were patients at two urban, level I trauma centers who were admitted with a diagnosis of isolated head injury and with a Glasgow Coma Scale (GCS) score of 8 or less. We recorded demographic, interventional, and outcome variables.
Results
In 289 patients, 24 of 25 (96%) were transfused if their lowest recorded intensive care unit (ICU) hemoglobin level was 8.0 g/dl or less. In contrast, only 9/182 (5%) of these 289 patients were transfused if the hemoglobin levels were 10.0 g/dl or greater. In the remaining 82 patients with lowest ICU hemoglobin levels of 8.0–10.0 g/dl, 52% were transfused. These 82 patients (43 underwent RBCT and 39 did not) were included in our analysis.
Discussion
The overall in-hospital mortality rate was 32%; rates were similar between the two groups (29%, non-RBCT; 35%, RBCT) (P = 0.64). Likewise, in-hospital morbidity was similar between groups. Logistic and proportional hazard regression analyses identified RBCT as one predictor of mortality.
Conclusions
Our results suggest that a restrictive transfusion practice is safe for severely head-injured patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impetus to limit red blood cell transfusion (RBCT) in the 1980s stemmed primarily from fears of rare but devastating infectious risks such as hepatitis and HIV. However, a growing body of recent evidence suggests that (i) RBCT is associated with additional immunomodulatory and inflammatory risks and (ii) a moderate degree of anemia (with minimum hemoglobin levels of 7–8 g/dl) is usually well tolerated, even in critically ill patients. Consequently, RBCT guidelines have been published; transfusion practices have shifted toward less transfusion, toward transfusion based on clinical need, and toward lower acceptable hemoglobin (7–8 g/dl) and hematocrit (21–24%) levels [1].
Less evidence is available detailing the risks and benefits of RBCT in trauma patients, especially those with severe traumatic brain injury. Only a few large studies have addressed RBCT in trauma patients, only one of which focused on patients with severe traumatic brain injury [2]. The non-profit, New York-based Brain Trauma Foundation has not published guidelines for RBCT, and traditional transfusion triggers as outlined in neurosurgery textbooks (“the 10/30 rule”: using RBCT to maintain hemoglobin levels of at least 10 g/dl or a hematocrit of at least 30%) seem to be more commonly used in brain-injured patients than in critical care patients in general [3, 4]. In our study, we tested the hypothesis that patients with severe isolated traumatic brain injury would not benefit from traditional aggressive RBCT.
Materials and Methods
The institutional review boards at Hennepin County Medical Center (HCMC, Minneapolis, MN) and North Memorial Medical Center (NMMC, Robbinsdale, MN) approved our study. These two level I urban trauma centers are separated by 4.5 miles. They both admit >85% blunt trauma and have similar numbers of traumatic brain-injured patients admitted annually. During the study period from January 1, 1998, through December 31, 2002, each institution averaged about 2,000 trauma admissions annually. Of these admissions, approximately 500 included traumatic brain-injured patients; 20% of these were severe with a Glasgow Coma Scale (GCS) score ≤8.
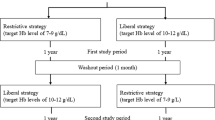
The clinical practices for treating head injury and management of intracranial pressure (ICP) are similar between institutions. These best evidence practices are based on guidelines first published by the Brain Trauma Foundation in 1996 and revised once during the study period in 2000 [5, 6]. The guidelines address the importance of organized trauma systems, early treatment of hypotension and hypoxia, antiseizure prophylaxis, indications for ICP monitoring, treatment of elevated ICP, and maintenance of cerebral perfusion pressure (CPP) to prevent secondary brain injury (using vasopressors, diuretics, hypoventilation, and barbiturates), and nutritional support. The 2000 revision discusses prognostic features of severe traumatic brain injury [computed tomography (CT) scan features, pupillary diameter and light reflex, age, and GCS score], and emphasizes the importance of ICP monitoring. Note that these guidelines do not address RBCT in the treatment of traumatic brain injury. Neither hospital has formal transfusion protocols; however, one institution has liberal indications for RBCT for trauma patients (minimum hemoglobin levels in ICU patients are usually maintained at 10 g/dl) while the other has adopted a more conservative RBCT practice (patients in the ICU tend not to be transfused until hemoglobin levels fall below 8 g/dl).
First, we queried the trauma registry at each hospital for patients who were admitted to an ICU from January 1, 1998, through December 31, 2002, who met the following criteria: (i) they had an isolated traumatic brain injury and (ii) their admission GCS score was 8 or less. Excluded from our study were patients who met any of the following criteria: (i) penetrating brain trauma, (ii) age under18 years, (iii) pregnancy at the time of their injury, (iv) history of chronic anemia, or (v) death within 72 h after admission. Data extracted from each trauma registry included patient age and gender, date of admission, admission GCS score, head and neck abbreviated injury scale score (AIS), injury severity score (ISS), Marshall head CT score, and admission blood alcohol level (BAL). Isolated traumatic brain injury was defined by excluding patients with any non-head and neck AIS of >2 or a sum non-head and neck AIS > 3. We calculated GCS score, ISS, and Marshall Head CT score as previously described [7–12].
After we identified our study patients from each trauma registry, we retrospectively reviewed their medical records with regard to the following additional variables: hospital length of stay (HLOS), ICU length of stay (ICULOS), lowest recorded hemoglobin and sodium levels while in the ICU, and type of intracranial injury (subdural hematoma, epidural hematoma, subarachnoid hemorrhage, or intraventricular hemorrhage). We recorded interventions, including transfusion of blood products, surgery, tracheostomy, and ICP management. We calculated total units of RBCT during their hospital admission. As detailed above, transfusion practices differed between institutions but neither hospital used transfusion protocols during the time period of this study. We reviewed the medical record for patient in-hospital mortality and morbidity. Specifically, we recorded the diagnosis of pneumonia, urinary tract infection (UTI), deep venous thrombosis (DVT), pulmonary embolus (PE), decubitus ulcer, bacteremia, septic shock, myocardial infarction (MI), and seizure. We noted any prophylactic measure administered for DVT. For our final analysis, we focused on patients with the greatest variability in RBCT patterns which corresponded to patients with a lowest recorded ICU blood hemoglobin level of ≥8.0 and <10.0 g/dl.
Data Analysis
We calculated and evaluated means, standard deviations, and normality for all continuous and discrete variables, which are presented as mean ± standard deviation. Categorical variables are presented as totals with percentage calculated. To compare continuous and discrete variables, we used a Wilcoxon Two Sample Test; categorical variables, a Fisher’s Exact Test. A P value of ≤0.05 defined significance. We created a univariate and multivariate regression analysis model to assess predictors of mortality. After examining correlations among variables, we incorporated into our model age, gender, motor GCS score, total GCS score, admission BAL, head and neck AIS score, ISS, presence of subarachnoid hemorrhage (SAH), minimum ICU sodium level, minimum ICU hemoglobin level, packed red blood cell (PRBC) transfusion, and development of any complication. Last, we performed a Cox proportional hazard regression using these same variables to assess predictors of mortality. All statistics were performed with SPSS 11 for Macintosh (SPSS, Chicago, IL).
Results
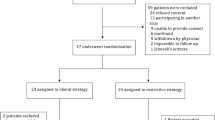
From January 1, 1998, through December 31, 2002, a total of 289 patients treated at the two level I trauma centers met our study criteria described above. Figure 1 shows that in 289 patients, 24 of 25 (96%) were transfused if their lowest recorded intensive care unit (ICU) hemoglobin level was 8.0 g/dl or less. In contrast, only 9 of 182 (5%) of these 289 patients were transfused if the hemoglobin levels were 10.0 g/dl or greater. In the remaining 82 patients with lowest ICU hemoglobin levels of 8.0–10.0 g/dl, 52% were transfused. Of these 82 patients 43 underwent at least 1 RBCT and 39 did not. We included these 82 patients in our final analysis because the transfusion practices in this group showed the most variability. The number of patients included, excluded, and stratified based on injury, hemoglobin level, and RBCT are illustrated in Fig. 2.
Red blood cell transfusion patterns in 289 patients with isolated traumatic brain injury based on lowest recorded ICU hemoglobin level. Ninety-six percent (24/25) of patients were transfused if their lowest hemoglobin level was 8.0 g/dl or less. In contrast, only 5% (9/182) of these 289 patients were transfused if the hemoglobin levels were 10.0 g/dl or greater. In the remaining 82 patients with lowest ICU hemoglobin levels of 8.0–10.0 g/dl, 52% were transfused. RBCT, red blood cell transfusion
Patient characteristics are summarized in Table 1. The RBCT and non-RBCT groups were similar in age, male-to-female ratio, admission BAL, ISS, Marshall head CT score, and prevalence of subdural hemorrhage, epidural hemorrhage, intraventricular hemorrhage, and SAH. Differences between the two groups included a lower minimum ICU blood hemoglobin level and a lower admission GCS motor score in the RBCT group.
The type and frequency of interventions for the two groups are shown in Table 2. The mean HLOS for study patients was 15.4 days. RBCT patients had a longer ICULOS, but not a longer HLOS. RBCT patients were also more frequently transfused with fresh frozen plasma (FFP) and underwent surgery, ventriculostomy placement, and tracheostomy placement more frequently than non-RBCT patients. All study patients were treated with vasopressors similarly.
The overall in-hospital mortality rate was 32%. Mortality rates were similar between the two groups (29%, non-RBCT; 35%, RBCT) (P = 0.64). Mortality rates did not differ significantly between the two hospitals. Additionally, we found little difference in the overall in-hospital morbidity—the rates of pneumonia, UTI, decubitus ulcer, bacteremia, systemic inflammatory response syndrome, myocardial infarction, and seizure activity were similar. The rate of DVT was higher in patients who were transfused with PRBC (24%, RBCT; 6%, non-RBCT) (P = 0.03), but the two groups had similar rates of pulmonary embolus. Outcome data are summarized in Table 3 and thromboembolic prophylactic measures are shown in Table 4.
In all 82 patients combined, our univariate and multivariate regression analyses revealed that the best predictors of mortality were (i) older age (P = 0.0469), (ii) motor GCS score (P = 0.0045), (iii) higher admission BAL (P = 0.0397), and (iv) lowest recorded ICU sodium level (P = 0.0190). Similarly, Cox proportional hazard regression identified these same variables and also revealed RBCT (P = 0.0463) and development of any complication (P = 0.0015) as predictors of mortality (Table 5).
Discussion
In our study, two groups of patients with severe traumatic brain injury had similar outcomes whether or not they underwent RBCT. Specifically, in patients whose lowest ICU hemoglobin level was between 8.0 and 10.0 g/dl, RBCT did not appear to alter the mortality rate. Our multivariate and Cox proportional hazard regression models demonstrated that the lowest measured ICU hemoglobin level was not predictive of mortality. Carlson et al. [2] showed that traumatic brain-injured patients tolerate persistent anemia (defined as multiple days with a hematocrit level less than 30%). In their review of 169 patients, linear regression analysis showed that patients who had more days with a hematocrit less than 30% had slightly better neurologic outcomes as measured by discharge and follow-up neurologic scores. Furthermore, transfusion was associated with significantly lower outcome scores at discharge. This review is the only one currently that specifically examined anemia and transfusion thresholds in traumatic brain-injured patients.
A number of large trials have investigated transfusion practices, risks, and benefits in critical care patients. The results have gradually effected a paradigm shift toward more conservative transfusion practices. The Transfusion Requirements in Critical Care (TRICC) trail randomized 838 patients to a restrictive (target hemoglobin, 7.0–9.0 g/dl) or liberal (target hemoglobin, 10.0–12.0 g/dl) transfusion strategy [13]. Survival tended to be higher in the restrictive group, but the difference did not reach statistical significance. However, a clear survival benefit for less transfusion was demonstrated in a subset of younger and healthier patients.
An earlier study by the same TRICC group showed that survival, as measured by an adjusted odds ratio, decreased in proportion to the volume of blood transfused for nearly 4,500 critically ill patients [14]. However, that study suggested that patients with cardiac disease or high APACHE (acute physiology and chronic health evaluation) scores do not tolerate anemia as well as other patients.
The CRIT study prospectively examined nearly 4,900 patients [15]. Aside from demonstrating that the number of RBCTs was an independent predictor for worse clinical outcome, the study showed that practitioners have been reluctant to adopt selective and restrictive transfusion protocols. These results are mirrored in a multicenter European study of 3,500 patients [16].
Subset analyses of both the TRICC and the CRIT trials for trauma patients have been published [17, 18]. The TRICC subset analysis included 203 resuscitated critically ill trauma patients (about 25% had head injuries). As with the parent TRICC study, mortality rates were no better in the liberal RBCT group than in the restrictive transfusion group.
The CRIT subset analysis included examination of 576 trauma patients (but excluded those admitted to neuroscience ICUs). Over half of the patients were transfused, but tended to remain anemic despite RBCT. Also, transfused patients tended to have longer ICULOS and HLOS, although illness severity was not controlled.
We found RBCT to be an independent predictor of mortality using our Cox proportional hazard regression model; our finding echoes previously cited studies. Immunomodulatory effects of RBCT have been implicated as a significant risk and may, in part, explain the association between transfusion and poorer outcome [19]. Moore et al. [20] found that, in 513 trauma patients, early transfusion had a dose-dependent association with the development of multiple organ dysfunction, likely due to proinflammatory mediators contained in cellular blood products. In victims of head trauma, injured brain astrocytes may be particularly sensitive to inflammatory mediators. Reactive astrocytosis (the process by which a glial scar is formed) peaks at 4 days post-injury, then tapers over the next 2–3 weeks; it is often associated with astrocyte swelling (vasogenic edema). It has been hypothesized that both reactive astrocytosis and vasogenic edema are upregulated by interleukin-6 and tumor necrosis factor-α, which are in turn upregulated with RBCT [21].
The goal in treating patients with severe traumatic brain injury is to limit secondary brain injury by decreasing intracranial pressure and increasing CPP, thus minimizing further brain ischemia [22–25]. The traumatically injured brain is thought to be particularly susceptible to injury from hypoperfusion and hypoxia and neuronal vulnerability to ischemia has been well documented. A commonly cited reason for transfusing such patients is to increase oxygen delivery to injured tissue. However, the cerebral response to RBCT is not predictable and uniform. Studies measuring brain tissue partial pressure of oxygen (PbtO2) in brain-injured patients show that most PbtO2 values increase after RBCT, but the effects are transient; some patients actually experience a drop in PbtO2. Furthermore, PbtO2 measurements have little correlation with hemoglobin levels [26, 27]. Similar studies in other critical care patient populations have documented a lack of the expected increase in local tissue oxygen delivery after RBCT [28, 29].
In addition to an incomplete understanding of cerebral physiology and healing after trauma, the microvascular response to injury and transfusion is poorly characterized. Cerebral blood flow (CBF) is dependent on CPP, blood viscosity, and vessel caliber. Transfusion increases blood viscosity and may limit CBF. Two studies have examined outcomes after nontraumatic aneurysmal SAH, but the results are conflicting. Smith et al. [30] demonstrated that transfusion was associated with worse outcomes in 441 patients undergoing surgery for ruptured aneurysms and SAH. In the patients who underwent RBCT, angiographic vasospasm was observed more frequently. In contrast, Naidech et al. [31] found no association between transfusion and poor outcome (after correction for injury severity) and no correlation between transfusion and vasospasm in 103 aneurysmal SAH patients.
In our study, Cox proportional hazard regression analysis revealed that the development of in-hospital complications was the best predictor of mortality. Age, motor GCS score, admission BAL, and minimum ICU sodium level were also strong predictors of mortality. The correlation between mortality and RBCT was weaker but still statistically significant. This correlation might argue against routine RBCT for patients with traumatic brain injury, especially for lowest recorded hemoglobin levels >10 g/dl. Similar risk factors have been described in other studies [32]. Additionally, in our study, patients who underwent RBCT were apparently more likely to develop DVT, despite similar prophylactic measures. Although this complication may be a surrogate marker for a slightly sicker patient population, it is also suggestive of another potential risk with transfusion. In a recent large observational study of perioperative allogenic transfusion, venous thromboembolism was associated with transfusion in women [33]. Alternatively, longer ICULOS and higher use of paralytic drugs in the RBCT group may contribute to a higher DVD rate.
Certainly, our study has limitations. Although the RBCT and non-RBCT groups were well-matched in terms of head and neck AIS, ISS, Marshall head CT score, and type of injury, the motor portion of the GCS score was significantly lower in the RBCT group. Patients in the RBCT group were more likely to undergo ventriculostomy and surgery; thus this group may have represented slightly sicker patients. The bias toward a slightly sicker group undergoing RBCT suggests that transfusion may have helped these patients achieve an outcome similar to that of less sick patients. However, our regression analysis argues against this possibility. We did not have data available for post-procedural blood loss or the temporal relationship between procedures and RBCT, so it is difficult to know if an increased rate of procedures and surgery in the transfused group contributed to anemia. Second, we were unable to collect neurologic outcome data in the survivors, which would have allowed examination of longer-term affects of RBCT similar to Carlson et al’s study [2]. Third, the management of traumatic brain injury has undergone changes since the completion of this study including increased use of ICP monitors, PbtO2 monitoring, and substitution of hypertonic saline for mannitol (although there are no formal guidelines for the use of PbtO2 monitors or hypertonic saline). Finally, given the retrospective methodology and relatively small sample size, this study may be underpowered to detect small differences between groups.
Our results suggest that in the acute setting it is safe to use a lower RBCT threshold in patients with anemia and severe isolated traumatic brain injury. A more powerful prospective study to determine optimal blood transfusion thresholds, benefits, and risks in patients with severe traumatic brain injury is warranted.
References
American College of Physicians. Practice strategies for elective red blood cell transfusion. Ann Intern Med 1992;116:403–6.
Carlson AP, Schermer CR, Lu SW. Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma 2006;61:567–71.
Brain Trauma Foundation. Guidelines for the prehospital management of traumatic brain injury. Guidelines for the management and prognosis of severe traumatic brain injury. Guidelines for the surgical management of traumatic brain injury. Available at: www.braintrauma.org.
Winn HR. Youmans neurological surgery: fifth edition. Philadelphia: WB Saunders Company; 2004.
Guidelines for the management of severe head injury. Brain Trauma Foundation, American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care. J Neurotrauma 1996;13:641–734.
Brain Trauma Foundation, Inc., American Association of Neurological Surgeons. Part 1: guidelines for the management of severe traumatic brain injury. New York, NY: Brain Trauma Foundation, Inc.; 2000. p. 165.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974;2:81–4.
Fischer J, Mathieson C. The history of the Glasgow Coma Scale: implications for practice. Crit Care Nurs 2001;23:52–8.
Baker SP, O’Neill B, Haddon W, Long W. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187.
Baker SP, O’Neill B. The injury severity score: an update. J Trauma 1976;6:882–5.
Eisenberg HM, Gary HE Jr, Aldrich EF, et al. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg 1990;73:688–98.
Marshall LF, Marshall SB, Klauber MR, et al. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma 1992;1:S287–92.
Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999;340:409–17.
Hebert PC, Wells G, Tweeddale M, et al. Does transfusion practice affect mortality in critically ill patients? Transfusion Requirements in Critical Care (TRICC) Investigators and the Canadian Critical Care Trials Group. Am J Respir Crit Care Med 1997;155:1618–23.
Corwin HL, Gettinger A, Pearl RG, et al. The CRIT Study: anemia and blood transfusion in the critically ill—current clinical practice in the United States. Crit Care Med 2004;32:39–52.
Vincent JL, Baron JF, Reinhart K, et al. ABC (Anemia and Blood Transfusion in Critical Care) Investigators. Anemia and blood transfusion in critically ill patients. JAMA 2002;288:1499–507.
McIntyre L, Hebert PC, Wells G, et al. Is a restrictive transfusion strategy safe for resuscitated and critically ill trauma patients? J Trauma 2004;57:563–8.
Shapiro MJ, Gettinger A, Corwin HL, et al. Anemia and blood transfusion in trauma patients admitted to the intensive care unit. J Trauma 2003;55:269–73.
Bordin JO, Heddle NM, Blajchman MA. Biological effects of leukocytes present in transfused cellular blood products. Blood 1994;84:1703–21.
Moore FA, Moore EE, Sauaia A. Blood transfusion. An independent risk factor for postinjury multiple organ failure. Arch Surg 1997;132:620–4.
Norenberg MD. Astrocyte responses to CNS injury. J Neuropathol Exp Neurol 1994;53:213–20.
Robertson CS, Valadka AB, Hannay HJ, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med 1999;27:2086–95.
Rosner MJ, Rosner SD, Johnsonn AH. Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg 1995;83:949–62.
Ling GS, Neal CJ. Maintaining cerebral perfusion pressure is a worthy clinical goal. Neurocrit Care 2005;2:75–815.
Feinstein AJ, Patel MB, Sanui M, Cohn SM, Majetschak M, Proctor KG. Resuscitation with pressors after traumatic brain injury. J Am Coll Surg 2005;201:536–45.
Smith MJ, Stiefel MF, Magge S, et al. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med 2005;33:1104–8.
Leal-Noval SR, Rincon-Ferrari MD, Marin-Niebla A, et al. Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: a preliminary study. Intensive Care Med 2006;32:1733–40.
Dietrich KA, Conrad SA, Hebert CA, Levy GL, Romero MD. Cardiovascular and metabolic response to red blood cell transfusion in critically ill volume-resuscitated nonsurgical patients. Crit Care Med 1990;18:940–4.
Lorente JA, Landin L, De Pablo R, Renes E, Rodriguez-Diaz R, Liste D. Effects of blood transfusion on oxygen transport variables in severe sepsis. Crit Care Med 1993;21:1312–8.
Smith MJ, Le Roux PD, Elliott JP, Winn HR. Blood transfusion and increased risk for vasospasm and poor outcome after subarachnoid hemorrhage. J Neurosurg 2004;101:1–7.
Naidech AM, Drescher J, Ault ML, Shaibani A, Batjer HH, Alberts MJ. Higher hemoglobin is associated with less cerebral infarction, poor outcome, and death after subarachnoid hemorrhage. Neurosurgery 2006;59:775–9.
Hukkelhoven CW, Steyerberg EW, Habbema JD, et al. Predicting outcome after traumatic brain injury: development and validation of a prognostic score based on admission characteristics. J Neurotrauma 2005;22:1025–39.
Nilsson KR, Berenholtz SM, Garrett-Mayer E, Dorman T, Klag MJ, Pronovost PJ. Association between venous thromboembolism and perioperative allogenic transfusion. Arch Surg 2007;142:126–32.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
George, M.E., Skarda, D.E., Watts, C.R. et al. Aggressive Red Blood Cell Transfusion: No Association with Improved Outcomes for Victims of Isolated Traumatic Brain Injury. Neurocrit Care 8, 337–343 (2008). https://doi.org/10.1007/s12028-008-9066-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9066-y