Abstract
Postpartum angiopathy as clinical presentation of reversible cerebral vasoconstriction syndrome remains an intriguing phenomenon. The diagnosis needs to be considered in women presenting with thunderclap headache with or without associated neurological deficits. Here, we present a patient with thunderclap headache with initial normal laboratory and cerebral imaging findings, including intracranial angiography. Her condition worsened over several days and magnetic resonance imaging revealed changes initially compatible with posterior reversible encephalopathy syndrome, sequentially ischemic stroke and narrowing of the intracranial arteries. Although the patient was in coma for several days, she completely recovered and the focal vasoconstriction fully resolved. This case underscores the complex and variable presentation of postpartum angiopathy and illustrates the diagnosis to be (re)considered even if cerebral vasoconstriction is not documented at the onset of symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Headache in the postpartum period can be due to many causes including primary headache disorders such as migraine, tension-type headache or primary thunderclap headache; and secondary headaches like postdural puncture headache, dissection, ischemic or hemorrhagic stroke, subarachnoid hemorrhage, venous sinus thrombosis, preeclampsia and eclampsia and postpartum angiopathy. The latter was originally considered an isolated clinical entity, but it is now thought to occur as part of a larger syndrome: reversible cerebral vasoconstriction syndrome (RCVS) [1]. Here, we present the case of RCVS in a patient presenting with postpartum headache complicated with posterior reversible leukoencephalopathy syndrome (PRES) and ischemic stroke as revealed by sequential neuroimaging.
Case report
A 30-year-old woman experienced severe thunderclap headache, 6 days following the birth of her second child. The pregnancy and delivery had been uncomplicated, in particular without evidence of (pre)eclampsia. Her medical history consisted of systemic lupus erythematosus, for which she received intermittent hydroxychloroquine, and migraine without aura.
The severe headache started rather suddenly and was localized in the frontal areas radiating to the neck and was associated with mild nausea, photo- and phonophobia. Considering the severe intensity and sudden onset, the headache was described as thunderclap headache. Her clinical examination was unremarkable including the absence of nuchal rigidity and a normal blood pressure (129/87 mmHg). Computed tomography (CT) of the brain revealed no abnormalities and cerebrospinal fluid (CSF) had a normal opening pressure, without elevated cell count and absence of xanthochromia, arguing against a cerebral venous thrombosis or subarachnoid hemorrhage. The patient requested to be discharged to take care of her recent newborn child and was advised to return to the hospital if symptoms would increase. Magnetic resonance (MR) of the brain, without MR angiography (MRA), but including cerebral venography 2 days following discharge, was normal (Fig. 1a).
Serial imaging of RCVS documenting PRES, ischemic lesions and intracerebral vasoconstriction. At initial presentation MR of the brain was unremarkable (a). On day 8 after symptom onset, FLAIR images showed diffuse increased signal intensity both cortical and subcortical (b–e) with only moderate diffusion restriction in the right parieto-occipital region (f, arrowhead), without changes on ADC (not shown). Follow-up MR on day 16 revealed a clear reduction in FLAIR lesions (g and h almost at the same level as b and c) while regions of marked diffusion restriction (i) with concomitant hypointense signal on ADC (j) had become apparent
Over the following days, paracetamol, non-steroidal anti-inflammatory drugs and sporadic sumatriptan relieved the headache only partially. She continued to experience persistent daily attacks of thunderclap headache with abrupt onset which could be partially alleviated over hours by the intake of analgetics. The pain was most intense in the supine position and caused sleep deprivation. Five days later, she was readmitted for intravenous analgesic therapy. Clinical examination and CT of the brain were normal, but her blood pressure was now elevated (177/98 mmHg). The next day, she had a secondary generalized seizure after which she did not regain consciousness for 2 days. An electroencephalogram did not show a status epilepticus. A lumbar puncture was repeated and elevated CSF protein was documented. A CT cerebral angiography (CTA) showed no evidence of focal narrowing or aneurysms. In addition, no arguments for acute neurolupus could be identified in the analysis of urine (protein) and blood (complement) samples nor was other organ (kidney) involvement determined. MR of the brain now showed several abnormalities with identification of regions of vasogenic edema on diffusion-weighted and fluid-attenuated inversion recovery (FLAIR) imaging without abnormalities on apparent diffusion coefficient (ADC) (Fig. 1b–e). A posterior reversible encephalopathy syndrome (PRES) possibly in connection with eclampsia was suspected and intravenous therapy with magnesium sulfate was initiated. However, neither the clinical findings nor the blood and urine analysis confirmed the presence of eclampsia.
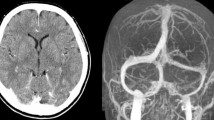
Antihypertensive treatment resulted in normalization of blood pressure and clinical improvement with some remaining cognitive deficits over the following days. MR of the brain was repeated which now showed bilateral ischemic lesions and narrowing of the intracranial arteries (Figs. 1g–j, 2a). Clinical examination 2 months after the initial presentation was normal. MRA of the brain showed normalization of the focal stenoses on the intracranial vessels (Fig. 2a). Based on these findings, a diagnosis of reversible cerebral vasoconstriction syndrome was made.
Reversible intracerebral vascoconstriction. MR angiography of the intracranial vessels 2 weeks after symptom onset showed focal narrowing most pronounced in the posterior circulation (a, arrows). Two months after symptom onset focal stenoses on the intracranial arteries could no longer be demonstrated (b)
Discussion
Transient, fully reversible cerebral vasoconstriction was first documented by Call and Fleming [2]. Over the years, several syndromes with a similar clinical presentation but different etiologies have been described as Call–Fleming syndrome, including migraine angiitis, postpartum angiopathy, drug-induced vasospasm and benign angiopathy of the central nervous system. However, since there was a clear clinical and radiological overlap, the term reversible cerebral vasoconstriction syndrome (RCVS) was suggested in 2007 and criteria presented [1]. These include: documentation of segmental cerebral artery vasoconstriction; absence of aneurysmal subarachnoid hemorrhage; normal or near-normal cerebrospinal fluid analysis; severe and acute headache (with or without additional neurological symptoms which can be caused by PRES, stroke or subarachnoid hemorrhage); and finally the diagnosis is confirmed by the reversibility of the angiographic abnormalities within 12 weeks after symptom onset. Since the term RCVS was presented, numerous series have been published documenting the clinical presentation, risk factors and outcome of this syndrome [3–7]. However, the pathophysiology remains speculative [8]. Postpartum angiopathy has been the describing term for RCVS occurring in women shortly after pregnancy and has been an important differential diagnosis in these patients presenting with various acute neurological events e.g. subarachnoid hemorrhage and PRES [9–13]. Our patient had no abnormalities on routine brain imaging and elevated blood pressure was not present at initial presentation. In series of RCVS, normal brain imaging has been documented [7]. Unfortunately, no MRA was obtained on this occasion, while a CTA a few days later was normal although the sensitivity of CTA might be reduced compared to MRA [14]. The infarct in the splenium of the corpus callosum (supplied by the posterior pericallosal artery) is of interest since this is not a common region for an ischemic lesion to occur possibly due to interarterial anastomoses between the posterior pericallosal and the pericallosal artery [15].
The further simultaneous development of PRES and RCVS has been described quite commonly [3, 7] underscoring the hypothesis that these conditions have a common pathophysiology [13]. It has been hypothesized that either the episodes of systemic hypertension leading to hyperperfusion, or cerebral vasoconstriction and therefore hypoperfusion could cause vasogenic edema observed in PRES [16]. Since in patients with RCVS both hypertension and intracranial vasoconstriction have been documented both mechanisms could be at play in this syndrome.
The focal narrowing of intracranial vessels resolved 2 months after symptom onset, a finding required for the diagnosis of RCVS (Fig. 2b). As an additional precipitating factor for development of the syndrome, exposure to sumatriptan was documented [1]. In accordance with most case series, she had a good outcome with a modified Rankin Scale of 0 despite the presence of coma. This case report underscores the difficult diagnosis of RCVS in the initial presentation and shows the various clinical and imaging findings associated with this complex and poorly understood syndrome.
References
Calabrese LH et al (2007) Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med 146(1):34–44
Call GK et al (1988) Reversible cerebral segmental vasoconstriction. Stroke 19(9):1159–1170
Ducros A et al (2007) The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome. A prospective series of 67 patients. Brain 130(Pt 12):3091–3101
Williams TL et al (2007) A fatal case of postpartum cerebral angiopathy with literature review. Arch Gynecol Obstet 275(1):67–77
Chen SP et al (2008) Transcranial color doppler study for reversible cerebral vasoconstriction syndromes. Ann Neurol 63(6):751–757
Chen SP, Fuh JL, Wang SJ (2010) Reversible cerebral vasoconstriction syndrome: an under-recognized clinical emergency. Ther Adv Neurol Disord 3(3):161–171
Singhal AB et al (2011) Reversible cerebral vasoconstriction syndromes: analysis of 139 cases. Arch Neurol 68(8):1005–1012
Ducros A, Bousser MG (2009) Reversible cerebral vasoconstriction syndrome. Pract Neurol 9(5):256–267
Ursell MR et al (1998) Recurrent intracranial hemorrhage due to postpartum cerebral angiopathy: implications for management. Stroke 29(9):1995–1998
Konstantinopoulos PA et al (2004) Postpartum cerebral angiopathy: an important diagnostic consideration in the postpartum period. Am J Obstet Gynecol 191(1):375–377
Neudecker S, Stock K, Krasnianski M (2006) Call–Fleming postpartum angiopathy in the puerperium: a reversible cerebral vasoconstriction syndrome. Obstet Gynecol 107(2 Pt 2):446–449
Chik Y et al (2009) A case of postpartum cerebral angiopathy with subarachnoid hemorrhage. Nat Rev Neurol 5(9):512–516
Singhal AB (2004) Postpartum angiopathy with reversible posterior leukoencephalopathy. Arch Neurol 61(3):411–416
Muhlenbruch G et al (2010) Comparison of dual-source CT angiography and MR angiography in preoperative evaluation of intra- and extracranial vessels: a pilot study. Eur Radiol 20(2):469–476
Phan TG et al (2007) Digital map of posterior cerebral artery infarcts associated with posterior cerebral artery trunk and branch occlusion. Stroke 38(6):1805–1811
Bartynski WS (2008) Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. Am J Neuroradiol 29(6):1043–1049
Acknowledgments
Robin Lemmens is supported by Research Fund KU Leuven. Vincent Thijs is a Senior Clinical Investigator of FWO Flanders.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lemmens, R., Smet, S., Wilms, G. et al. Postpartum RCVS and PRES with normal initial imaging findings. Acta Neurol Belg 112, 189–192 (2012). https://doi.org/10.1007/s13760-012-0051-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-012-0051-z