Abstract
Purpose of Review
Some personality traits seem to be associated with obesity, but there is little information available regarding their association with obesity treatment outcomes. The aim of this systematic review was therefore to assess the associations between personality traits—evaluated by means of the Temperament and Character Inventory (TCI)—and outcomes of obesity treatment, including attrition, weight loss, and weight loss maintenance. The PubMed database was searched, and studies were screened as per the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines, and data were collated using a narrative approach.
Recent Findings
Of the 886 articles retrieved, 9 studies assessing personality traits by means of the TCI in participants with obesity met the inclusion criteria and were reviewed. This approach revealed three main findings: (i) only one study found that attrition rate—during a 6-month behavioral weight loss program—is predicted by low reward dependence scores at baseline; (ii) two studies found that lower novelty-seeking and higher self-directedness scores at baseline positively predict short-term weight-loss magnitude; and (iii) four studies found that higher persistence and lower novelty-seeking scores at baseline predicted weight maintenance at 12 and 24 months.
Summary
Novelty-seeking and self-directedness traits appear to be predictors of short-term weight loss (≤ 6 months), and persistence and novelty-seeking traits may be related to long-term weight loss maintenance (≥ 12 months), although great uncertainty still exists regarding predictors of attrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Associations have been reported between personality traits—generally defined as habitual patterns of behavior, thought, and emotion [1]—and eating behaviors and disorders [2,3,4,5]. This suggests that personality traits may be involved in obesity development [6] and may therefore potentially influence weight management treatment outcomes [7, 8•].
Many of the earliest studies of personality in obesity relied on the Karolinska Scales of Personality (KPS) [9] or the Minnesota Multiphasic Inventory [10]; the inconsistency in their results is therefore not surprising, as both of these tools were designed and validated for assessing pathological personality traits rather than inter-individual variation in normal traits [11]. Indeed, more homogeneous findings have been obtained using instruments that assess personality traits within the five-factor model of personality (5FM) [2]—a theory used to describe the five basic traits that serve as the building blocks of personality, namely extroversion, agreeableness, conscientiousness, neuroticism, and openness. Of these, conscientiousness and neuroticism have been most consistently associated with adiposity [12].
The Temperament and Character Inventory (TCI) has been widely used to study obesity in recent years [11]. It was designed to provide a comprehensive evaluation of normal personality, and all its dimensions are closely linked to those of the 5FM [13, 14]. This makes TCI a useful tool in defining patient subgroups and pinpointing personality traits that may influence—both biologically and psychologically—the development of emotional and behavioral disturbances [13]. It is based on a psychobiological model of personality that includes seven dimensions, divided into “temperament” and “character.” Temperament is defined as the partly inherited emotional responses, considered stable throughout life and mediated by neurotransmitter functioning in the central nervous system [15]. It is identified through the following four dimensions: (i) novelty seeking, which expresses the tendency to seek out new stimuli and experiences, to be easily bored, impulsive, inclined to avoid monotony, and have a strong appetite [11]—; (ii) harm avoidance, which reflects the tendency to be motivated by a desire to avoid aversive experiences; (iii) reward dependence, which is the tendency to respond markedly to signals of reward, particularly to verbal signals of sentiment, social approval and support; and (iv) persistence, which expresses the preservation of resistance-to-frustration behavior. Character, on the other hand, is considered the sum of personality traits acquired through experience; it is identified through the following three dimensions: (i) self-directedness, a measure of self-concepts about oneself, self-acceptance, and the ability to direct one’s own life according to personal goals and values; (ii) cooperativeness, which encompasses self-concepts about others, and the ability to collaborate well with others; and (iii) self-transcendence, an expression of the relationship between the self and the external world as a whole, including nature, the universal complex and a supreme spiritual entity, but also the ability to think creatively and appreciate art, or the poetry of nature.
In view of the above, we set out to conduct a timely systematic review of the literature on the association between personality traits, attrition, weight loss, and maintenance outcomes in individual with obesity. The literature was assessed in accordance with the PICO process [16] (as far as we know for the first time) as follows: P, population—participants of both genders who met the standard criteria for obesity, in whom personality traits have been assessed by means of TCI; I, intervention—any weight management program defined as such by the authors; C, comparison—before and after weight loss intervention (when available); O, outcome—attrition rate and magnitude of weight loss and maintenance, however expressed.
Methods
The review was conducted in conformity to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [17].
Inclusion and Exclusion Criteria
All studies evaluating personality traits by means of TCI were included if they met the following criteria: (i) papers written in English reporting human data; (ii) the sample met standard criteria for definition of obesity in humans; (iii) original articles on studies with longitudinal design; (iv) prospective or retrospective observational, experimental, or quasi-experimental controlled or non-controlled studies documenting weight management in patients with obesity; (v) documentation of intentional changes in weight during short-term (≤ 6 months) or long-term (≥ 8–12 months) weight loss programs, however expressed (e.g., as absolute or percentage weight change, BMI). The following criteria were grounds for exclusion: (i) reviews or non-original articles (i.e., case reports, editorials, Letters to the Editor, or book chapters); (ii) personality assessment by means of tools other than TCI (e.g., KPS, MMPI, Big 5, etc.); and (iii) studies designed to assess personality disorders.
Information Source and Search Strategy
The literature search was designed and performed independently in duplicate by two authors. The PubMed database [18] was systematically screened using the following MeSH terms:
-
(((“Obesity”[mesh] OR “obesity”[all fields] OR “overweight”[MeSH Terms] OR “overweight”[All Fields]) OR (“weight loss”[MeSH Terms] OR “weight loss”[All Fields]) OR (“weight maintenance”[MeSH Terms] OR “weight maintenance”[All Fields]) OR (“weight reduction”[MeSH Terms] OR “weight reduction”[All Fields])) AND ((“personality trait”[MeSH Terms] OR “personality trait”[All Fields]) OR (“Harm avoidance”[MeSH Terms] OR “Harm avoidance”[All Fields]) OR (“Novelty seeking”[MeSH Terms] OR “Novelty seeking”[All Fields]) OR (“Persistence”[MeSH Terms] OR “Persistence”[All Fields]) OR (“Reward dependence”[MeSH Terms] OR “Reward dependence”[All Fields]) OR (“Self-directedness”[MeSH Terms] OR “Self-directedness”[All Fields]) OR (“Cooperativeness”[MeSH Terms] OR “Cooperativeness”[All Fields]) OR (“Self-transcendence”[MeSH Terms] OR “Self-transcendence”[All Fields]))).
In addition, a manual free text search of the above terms was also carried out in order to retrieve other articles that had not been identified via the initial search strategy, and the references lists of all articles were carefully checked to ensure that all relevant studies had been identified. Publication date was not considered an exclusion criterion for the purposes of this review.
Data Collection Process and Data Items
First, two authors carried out independent assessments of the title and abstract of each paper regarding the suitability of language and relevance of subject matter. The selected papers in this manner were then examined for their appropriateness for inclusion and method quality. The first author, year of publication, site of study, design, sample, gender, age, duration of follow-up, BMI, treatments received, and personality trait outcome measures are reported in Table 1.
Study Selection
The National Institute for Health and Care Excellence (NICE) guidelines checklist was used for quality appraisal of studies [19], in which a total score of 0–3 indicates poor quality; between 4 and 6, fair quality; and ≥ 7 good quality.
Data Synthesis
Due to the lack of RCTs among the resulting studies—since personality traits are not subject to experimental manipulation—a meta-analysis could not be performed. Therefore, all studies that met the inclusion criteria have been presented as a narrative synthesis [20].
Results
The initial search retrieved 886 papers. After the first round of screening, 671 papers were excluded for being in a language other than English, not being conducted on humans, not dealing with obesity or overweight, or dealing with obesity but not with personality traits, or vice versa. The second round of screening excluded 207 articles due to inappropriate type of paper, methodology and content; contributions other than original research articles (i.e., case reports, comments, and reviews) were excluded at this stage. Also excluded were papers describing studies that dealt with obesity and personality traits but did not assess the latter by means of TCI, and studies on obesity and personality traits assessed by TCI but with a cross-sectional design and making no reference to any weight-loss treatment (Fig. 1). Thus, at the end of the screening process, nine articles were considered suitable for systematic review and narrative analysis. According to the NICE guidelines checklist, the quality of selected studies ranged from fair to good (mean score 6.66 points) (Table 2).
Personality Traits and Obesity in Longitudinal Studies
In 2006, De Panfilis and colleagues [21] aimed to provide data regarding preoperative personality dimensions and weight loss prediction at 12 months after laparoscopic adjustable gastric banding (LAGB). Personality patterns were assessed by means of TCI in a total of 35 patients (31 females, 4 males) who underwent LAGB. At postsurgical follow-up, participants (age 41.2 ± 8.3 years; BMI 45.5 ± 4.8 kg/m2) had achieved a mean BMI reduction of 7.7 kg/m2. After controlling for the effect of other independent variables, i.e., baseline BMI, age, gender, level of education, and presence of psychiatric disorders, the TCI persistence scale was found to be positively correlated to postsurgical BMI reduction (b = 0.69, p = 0.004); the preoperative TCI persistence scores were reported to account for > 40% of the variance in BMI reduction 1 year after LAGB. However, some limitations of this study are apparent, such as the small size of the study sample, which raises questions of adequacy of statistical power. In addition, there was a relatively short follow-up period (1 year)—weight loss after bariatric surgery continues until 18 to 24 months after the intervention, with some weight regain usually being observed after the second year [22]. It is also likely that physiological mechanisms of surgery mask the effect of personality traits in the short term, while the impact of psychosocial variables tends to become more evident in the long term, with the attenuation of the biological effect of bariatric surgery.
In 2007, Leombruni and colleagues [23] also assessed personality traits by means of TCI in 38 surgical patients with severe obesity (6 males and 32 females; age 39.8 ± 9.9 years; BMI 43.5 ± 5.5 kg/m2), who in this case underwent laparoscopic vertical banded gastroplasty (VBG). A comparison between T0 and T1 scores showed a significant weight loss and BMI reduction of 10.43 kg/m2 6 months after surgery and indicated the self-directedness scale as a positive predictor of short-term weight loss outcome. However, this study was limited by the small patient sample and the very brief follow-up (6 months), as well as by the focus on VBG, which is now rarely performed.
In the same year, Sullivan and colleagues [11] evaluated the personality characteristics of 183 patients (age 45.17 ± 10.4 years; BMI = 44 ± 10 kg/m2) enrolled in the non-surgical Washington University Weight Management Program (WUWMP); this involved weekly group behavioral therapy and dietary education sessions for 5.5 months. They noted that patients with successful outcomes (> 10% weight loss; n = 52) after 22 weeks of behavioral therapy scored lower in novelty-seeking at baseline than those who had an unsuccessful outcome (< 5% weight loss; n = 69). However, it is evident that the very short duration of follow-up (< 6 months) is a major limitation of this study.
Another study conducted in 2007, by De Panfilis and colleagues [24], assessed the TCI predictors of compliance (i.e., decreased caloric intake and light-to-moderate physical activity) and weight loss after 8 months of behavioral weight loss treatment in 68 consecutive outpatients with obesity (age 38.9 ± 12.8 years; BMI 36.1 ± 6.9 kg/m2). These authors found no difference in personality traits between patients who completed the treatment and those who dropped out, or between responders and non-responders in terms of weight loss magnitude. However, the small sample size raises questions about the adequacy of statistical power to detect differences between the two samples.
In 2008, De Panfilis and colleagues [7] conducted a study on a different sample of patients, exploring whether or not personality variables assessed by the TCI can predict attrition from a behavioral weight loss program. To this end, TCI was administered to 92 patients of both genders with obesity (age 41.8 ± 12.7 years; BMI 38.5 ± 6.3 kg/m2) who underwent a 6-month weight loss treatment consisting of reduced caloric intake combined with behavioral therapy and recommendations for physical exercise. Two thirds of the subjects completed the 6-month program, while one third dropped out, and logistic stepwise regression analysis was performed to evaluate whether TCI scores predicted treatment attrition, after controlling for baseline psychiatric comorbidity, age, gender, age at onset of obesity, and initial BMI. This analysis showed that treatment attendance was predicted by high reward dependence scores (P = 0.37). That being said, the study does present some limitations that weaken the strength of its conclusions. Firstly, the small sample size raises questions about the adequacy of its statistical power, and secondly, the weight loss program in this study consisted of unstructured conventional hospital-based outpatient treatment. It is possible that personality variables would have a different impact on the outcome of more structured programs (i.e., manualized and more standardized) could lead to different outcomes.
In a later study, in 2014, De Panfilis and colleagues [25], evaluated whether personality traits assessed by TCI influenced weight-loss magnitude at 12 months after gastric bypass. Forty-nine adult patients of both genders with severe obesity (BMI = 46.4 ± 6.7 kg/m2) completed a thorough psychiatric evaluation before surgery. Predictors of weight loss were investigated with multivariate linear hierarchical regression, and results revealed that higher TCI persistence scores independently predicted 1-year outcomes of gastric bypass and accounted for 40% of the variance in total weight loss percentage (%TWL). The authors concluded that patients with low persistence scores showed significantly less weight loss than patients with high scores. Nonetheless, two major limitations of this study are evident, namely the small size of the sample, and the 1-year follow-up period—too short to assess the impact of psychological variables on bariatric surgery outcomes.
In the same year, Gordon et al. [26•] investigated the impact of personality traits on Roux-en-Y gastric bypass (RYGB) outcomes over long-term follow-up. The study included a total of 333 participants with obesity (age 35.4 ± 9.5 years; mean BMI 43.3 ± 4.8 kg/m2), and authors reported that lower persistence scores at baseline predicted lower percentage excess weight loss at 24 months. On the whole, they concluded that personality traits assessed during preoperative evaluation significantly predicted weight loss and maintenance after bariatric surgery, and a greater impact was observed at long-term follow-up (i.e., 2 years). Unfortunately, the short-term follow-up after bariatric surgery and the high proportion of dropouts make it difficult to confidently interpret these results.
Nevertheless, this finding is partially in line with those reported in 2015 by Agüera and colleagues [27], who used the TCI-R to evaluate personality traits and determine their ability to predict bariatric surgery outcomes at 24-month follow-up, after controlling for relevant confounding variables. Their sample comprised 139 patients with severe obesity (31 men and 108 women; age 40.6 ± 10.3 years; BMI 46.3 ± 6.4 kg/m2) who underwent various bariatric surgery procedures (i.e., gastric bypass, duodenal switch, and vertical sleeve), and they found an association between higher cooperativeness scores (OR = 1.05, 95% CI 1.00–1.10; p = 0.022) at baseline and better bariatric surgery outcome (%EWL > 50%) at 24-month follow-up. To our knowledge, this is the first time that greater cooperativeness has been noted as predictor of successful weight loss maintenance after medium-term follow-up in bariatric surgery patients. As this personality trait is related specifically to a persons’ ability to cooperate with others, we can speculate that greater cooperativeness may translate into greater collaboration of the patient with the clinical team, and therefore greater success in terms of weight loss maintenance. However, this finding should be interpreted in light of two major limitations. First and foremost, the psychological assessment relied on self-reported data collected by means of questionnaires, which casts doubt on its accuracy. What is more, the relatively small sample size did not allow authors to evaluate or compare specific surgical procedures (i.e., gastric bypass, duodenal switch, and vertical sleeve).
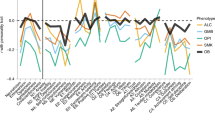
In the same year, Dalle Grave and colleagues investigated whether pretreatment personality profiles assessed with TCI were related to weight loss outcomes in 634 women with obesity (age 48.0 ± 10.6 years; BMI 37.8 ± 6.6 kg/m2) seeking treatment at eight Italian medical centers applying different non-surgical approaches, specifically lifestyle modification programs based either on cognitive behavioral therapy (individual or group sessions) or on the prescription of diet and physical activity [8•]. After adjustment for demographic and clinical confounders, authors found that no personality traits were significantly associated with attrition after 12 months. However, low scores on the novelty-seeking temperament scale at baseline remained significantly associated with 1-year weight loss ≥ 10%. In line with Sullivan et al. [11], therefore, these authors concluded that pretreatment novelty-seeking scores might be used to identify patients who could benefit most from weight loss treatments based on lifestyle modification, and to refer patients with high scores on this personality trait to treatments that include specific procedures to address impulsivity. The study, however, has several limitations. Firstly, the results only refer to women with obesity seeking treatment. Secondly, only six of the eight centers collected 1-year weight-loss data. Thirdly, assessment was based on self-report questionnaires, which are not ideal ways of assessing eating disorder features—as they tend to overestimate psychopathology—and cannot therefore be used for diagnostic purposes.
Discussion
The aim of this systematic review was to provide benchmark data on the association between personality traits, attrition, weight loss, and weight loss maintenance in individuals with obesity. As such, nine studies objectively judged to be of fair–good quality—six conducted in Italy and one each in Spain, the USA, and Brazil—including a total of 1571 participants of both genders were reviewed.
The first outcome of this analysis was an overall conclusion that it is not completely clear whether or not individual personality traits are predictors of treatment attrition during weight loss programs. Although one study found that attrition rate in a 6-month behavioral weight loss program was predicted by low reward dependence scores at baseline [7], two studies of longer duration (8 and 12 months, respectively) found no significant association between personality traits and attrition rates [8•, 24]. Although conflicting, these results may indicate that low baseline reward dependence scores could predict attrition rate during short-term non-surgical weight loss programs (≤ 6 months) [7], but not in those of longer duration (i.e., 8–12 months), at least in women [8•, 24]. The reduced dropout risk observed in individuals with higher scores on this temperamental trait may be explained by their tendency to be highly responsive to social pressure and dependent on the approval of others; it may be that such individuals prefer to seek support or protection rather than making decisions or doing things on their own [7]. It is also possible that these individuals feel more gratified by the weight loss that occurs during the first part of the program. Indeed, in such programs, the differences in the effect of reward dependence on attrition tend to disappear after 6 months—when the weight loss usually reaches a plateau, and the reward associated with weight loss gradually decreases. However, further investigation is clearly required to confirm previously published results and shed more light on this hypothesis. Potential investigators should also note that no data as regards personality traits and attrition in surgical approaches to weight loss have yet been published.
The second finding of our review concerned the relationship between weight loss outcomes and baseline personality traits assessed by means of TCI. Specifically, two studies found, respectively, that lower novelty-seeking and higher self-directedness scores at baseline appear to be predictors of better short-term weight loss outcomes [11, 23]. Although the durations of these assessments were very similar, 5.5 and 6 months, respectively, the first involved group behavioral therapy [11] while the latter examined participants who had undergone laparoscopic vertical banded gastroplasty [23]. Nevertheless, there are lessons that can be learned from both. Indeed, lower novelty-seeking scores have been associated with healthy dietary control and strong cognitive control of food (i.e., dietary restraint) [28, 29], which may explain the greater weight loss in patients who do not strongly display this trait; individuals with high novelty-seeking scores tend to be thrill-seekers who are easily bored, impulsive, inclined to avoid monotony, and have a strong appetite [11]—a combination of features that could lead these individuals to eat in order to stave off boredom. It could also make them less likely to adhere to dietary recommendations, as they may have less control over their impulses to eat a larger variety of foods (i.e., also in particular hyper-caloric food), and therefore be less successful in their attempts to lose weight [11]. High self-directedness, on the other hand, is one of the “character” dimensions of TCI that Cloninger has described as “willpower”—defined as “a metaphorical abstract concept to describe the extent to which a person identifies the imaginal self as an integrated, purposeful whole individual, rather than a disorganized set of reactive impulses” [13]. High self-directedness is also associated with an internal locus of control [13]—the degree to which people believe that they (as opposed to external forces) have control over the outcome of events in their lives—a construct that has shown some promise in predicting and explaining specific health-related behaviors such as smoking reduction, birth control utilization, and weight loss [30]. In contrast, individuals with low self-directedness tend to have lower motivation to change, and greater passivity in their treatment setting—two characteristics that may reduce the effectiveness of the treatment itself [31]. That being said, more research is needed before firm conclusions can be drawn.
Our review also yielded a more robust finding as regards the relationship between weight maintenance and personality; in particular, three studies found that higher persistence scores at baseline predicted weight loss maintenance at 12 and 24 months in bariatric surgery patients (i.e., adjustable gastric banding, gastric bypass, and RYGB) [21, 25, 26•]. As high persistence is characterized by perseverance despite frustration and fatigue [13], this may explain why individuals displaying this temperamental trait are able to better keep lost weight off by withstanding the aversive biological and environmental pressures to regain weight. Moreover, another study we assessed [8•] reinforced the correlation between weight loss magnitude and lower novelty-seeking scores [11, 32, 33], showing that the latter remain significantly associated with weight maintenance at 12 months [8•]. As derived from several large-sampled studies, this finding may be considered robust.
Less robust is the finding—from only one study—that higher baseline cooperativeness scores may be a predictor of successful weight-loss maintenance at 24-month follow-up in bariatric surgery patients [27]. This suggests that the ability to cooperate with others, and consequently with the clinical team—which might be expected to be the case with individuals with high cooperativeness scores—is associated with better weight-loss maintenance. However, as emphasized by the authors, this is the first study in which a relationship between the cooperativeness personality trait and obesity treatment has been reported [27], and it therefore requires replication.
In fact, all the reported findings need to be interpreted with extreme caution, due to the overall paucity of research into the issue. Furthermore, although only studies judged to be of fair–good quality were included in our systematic review, a small sample size was a common feature of nearly half of the studies reviewed. Moreover, it should be mentioned that only two studies included in our systematic review were multicentric, and the others may therefore be considered lacking in external validity. In addition, comparison between studies on different treatment types is also hindered because “total weight loss percentage” is generally used as an outcome in behavioral studies, while “excess weight percentage” is often used in bariatric surgery studies, and hence, the magnitude of weight loss from surgery is much greater than in behavioral weight loss treatment. Finally, it is possible that the personality factors that affect behavioral weight loss outcomes could be different from the ones that affect bariatric surgery weight loss outcomes, or the same factors affect the outcomes of the two types of weight-loss treatments differently.
Despite the above limitations, there are some potential clinical implications for the data we have uncovered. For instance, if the association between low reward-dependence, a temperamental trait that deals with the tendency to respond markedly to signals of reward, particularly to verbal signals of sentiment, social approval, and support [7], and short-term treatment attrition is confirmed by future studies, there might be a role for personality assessment via TCI in informing clinicians’ decisions. In particular, it may prompt them to place special emphasis on the patient—providing reward in order to reduce dropout risk in patients displaying this trait seeking non-surgical treatment, or even steer them towards treatment options (i.e., surgery or medication) that do not require a strong collaborative therapeutic alliance to succeed [7]. In other cases, patients with low self-directedness that manifest low motivation to change, greater passivity in the treatment, and poor weight loss could benefit from cognitive behavioral strategies specifically designed to increase self-directedness; such patients may respond more positively if they are taught strategies like setting short-term and achievable goals, developing adaptive coping behaviors through problem-solving in order to achieve these goals, and developing the confidence that they possess the resources required to achieve these goals (via progressive increases in self-efficacy through mastery experiences) [34, 35]. Similarly, individuals displaying novelty-seeking behavior may benefit from a treatment that includes procedures that address impulsivity, such as those derived from substance use therapy [36]. It would therefore be of interest to test the potential efficacy of interventions tailored to individuals with different temperament profiles in future studies.
Conclusions
This review indicates that some personality traits seem to exert an effect on treatment outcomes; specifically, low novelty-seeking and high self-directedness appear to predict successful short-term weight loss outcome (≤ 6 months), while low novelty-seeking and high persistence seem to predict better weight loss maintenance (≥ 12 months), especially after bariatric surgery. In light of these findings, and the differences noted between surgical and non-surgical treatments in this respect, the assessment of such traits may 1 day prove useful in clinical practice, enabling patients to be matched to a specific weight-management program (i.e., lifestyle modification, bariatric surgery, etc.) on the basis of their personality profile. Although such tailored approaches may conceivably be a way of improving treatment outcomes, a great deal of uncertainty still remains, especially as regards predictors of attrition, and more investigation is therefore urgently required.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Kassin S. Psychology. 4th ed. Upper Saddle River: Prentice Hall, Inc; 2003.
Elfhag K, Morey LC. Personality traits and eating behavior in the obese: poor self-control in emotional and external eating but personality assets in restrained eating. Eat Behav. 2008;9(3):285–93. https://doi.org/10.1016/j.eatbeh.2007.10.003.
Raynal P, Melioli T, Chabrol H. Personality profiles in young adults with disordered eating behavior. Eat Behav. 2016;22:119–23. https://doi.org/10.1016/j.eatbeh.2016.06.020.
Rotella F, Fioravanti G, Ricca V. Temperament and personality in eating disorders. Curr Opin Psychiatry. 2016;29(1):77–83. https://doi.org/10.1097/YCO.0000000000000212.
Turner BJ, Claes L, Wilderjans TF, Pauwels E, Dierckx E, Chapman AL, et al. Personality profiles in eating disorders: further evidence of the clinical utility of examining subtypes based on temperament. Psychiatry Res. 2014;219(1):157–65. https://doi.org/10.1016/j.psychres.2014.04.036.
Jokela M, Hintsanen M, Hakulinen C, Batty GD, Nabi H, Singh-Manoux A, et al. Association of personality with the development and persistence of obesity: a meta-analysis based on individual-participant data. Obes Rev. 2013;14(4):315–23. https://doi.org/10.1111/obr.12007.
De Panfilis C, Torre M, Cero S, Salvatore P, Dall'Aglio E, Marchesi C, et al. Personality and attrition from behavioral weight-loss treatment for obesity. Gen Hosp Psychiatry. 2008;30(6):515–20. https://doi.org/10.1016/j.genhosppsych.2008.06.003.
• Dalle Grave R, Calugi S, Compare A, El Ghoch M, Petroni ML, Colombari S, et al. Personality, attrition and weight loss in treatment seeking women with obesity. Clin Obes. 2015;5:266–72. A multicentre longitudinal study that investigated whether pre-treatment personality profiles assessed with TCI were related to weight-loss outcomes in a large sample of seeking-treatment women with obesity.
Jonsson B, Bjorvell H, Levander S, Rossner S. Personality traits predicting weight loss outcome in obese patients. Acta Psychiatr Scand. 1986;74(4):384–7. https://doi.org/10.1111/j.1600-0447.1986.tb06258.x.
Martin LF. The biopsychosocial characteristics of people seeking treatment for obesity. Obes Surg. 1999;9(3):235–43. https://doi.org/10.1381/096089299765553098.
Sullivan S, Cloninger CR, Przybeck TR, Klein S. Personality characteristics in obesity and relationship with successful weight loss. Int J Obes. 2007;31(4):669–74. https://doi.org/10.1038/sj.ijo.0803464.
Sutin AR, Ferrucci L, Zonderman AB, Terracciano A. Personality and obesity across the adult life span. J Pers Soc Psychol. 2011;101(3):579–92. https://doi.org/10.1037/a0024286.
Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50(12):975–90. https://doi.org/10.1001/archpsyc.1993.01820240059008.
Svrakic DM, Whitehead C, Przybeck TR, Cloninger CR. Differential diagnosis of personality disorders by the seven-factor model of temperament and character. Arch Gen Psychiatry. 1993;50(12):991–9. https://doi.org/10.1001/archpsyc.1993.01820240075009.
Cloninger CR. A systematic method for clinical description and classification of personality variants. A proposal. Arch Gen Psychiatry. 1987;44(6):573–88. https://doi.org/10.1001/archpsyc.1987.01800180093014.
Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12–3.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. https://doi.org/10.1136/bmj.b2700.
Pubmed Database. Available online: http://www.ncbi.nlm.nih.gov/pubmed.
El Ghoch M, Calugi S, Lamburghini S, Dalle Grave R. Anorexia nervosa and body fat distribution: a systematic review. Nutrients. 2014;6(9):3895–912. https://doi.org/10.3390/nu6093895.
Popay J, Roberts H, Sowden A, Petticrew M, Britten N, Arai L, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Available online. http://www.lancaster.ac.uk/shm/research/nssr/research/dissemination/publications/NS_Synthesis_Guidance_v1.pdf
De Panfilis C, Cero S, Torre M, Salvatore P, Dall'Aglio E, Adorni A, et al. Utility of the temperament and character inventory (TCI) in outcome prediction of laparoscopic adjustable gastric banding: preliminary report. Obes Surg. 2006;16(7):842–7. https://doi.org/10.1381/096089206777822278.
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–25. https://doi.org/10.1001/jama.2013.280928.
Leombruni P, Piero A, Dosio D, Novelli A, Abbate-Daga G, Morino M, et al. Psychological predictors of outcome in vertical banded gastroplasty: a 6 months prospective pilot study. Obes Surg. 2007;17(7):941–8. https://doi.org/10.1007/s11695-007-9173-4.
De Panfilis C, Cero S, Dall’Aglio E, Salvatore P, Torre M, Maggini C. Psychopathological predictors of compliance and outcome in weight-loss obesity treatment. Acta Biomed. 2007;78:22–8.
De Panfilis C, Generali I, Dall'Aglio E, Marchesi F, Ossola P, Marchesi C. Temperament and one-year outcome of gastric bypass for severe obesity. Surg Obes Relat Dis. 2014;10(1):144–8. https://doi.org/10.1016/j.soard.2013.09.018.
• Gordon PC, Sallet JA, Sallet PC. The impact of temperament and character inventory personality traits on long-term outcome of Roux-en-Y gastric bypass. Obes Surg. 2014;24:1647–55. A longitudinal study that evaluted the influence of personality traits assessed by TCI on Roux-en-Y gastric by pass (RYGB) over 24 months follow-up in a large sample of patients with severe obesity.
Aguera Z, Garcia-Ruiz-de-Gordejuela A, Vilarrasa N, Sanchez I, Bano M, Camacho L, et al. Psychological and personality predictors of weight loss and comorbid metabolic changes after bariatric surgery. Eur Eat Disord Rev. 2015;23(6):509–16. https://doi.org/10.1002/erv.2404.
Bjorvell H, Edman G, Rossner S, Schalling D. Personality traits in a group of severely obese patients: a study of patients in two self-chosen weight reducing programs. Int J Obes. 1985;9:257–66.
Jacobs SB, Wagner MK. Obese and nonobese individuals: behavioral and personality characteristics. Addict Behav. 1984;9(2):223–6. https://doi.org/10.1016/0306-4603(84)90062-5.
Wallston BD, Wallston KA. Locus of control and health: a review of the literature. Health Educ Monogr. 1978;6(1):107–17. https://doi.org/10.1177/109019817800600102.
Dalle Grave R, Calugi S, El Ghoch M, Marzocchi R, Marchesini G. Personality traits in obesity associated with binge eating and/or night eating. Curr Obes Rep. 2014;3(1):120–6. https://doi.org/10.1007/s13679-013-0076-5.
Fassino S, Leombruni P, Piero A, Daga GA, Amianto F, Rovera G, et al. Temperament and character in obese women with and without binge eating disorder. Compr Psychiatry. 2002;43(6):431–7. https://doi.org/10.1053/comp.2002.35906.
Davis C, Levitan RD, Carter J, Kaplan AS, Reid C, Curtis C, et al. Personality and eating behaviors: a case-control study of binge eating disorder. Int J Eat Disord. 2008;41(3):243–50. https://doi.org/10.1002/eat.20499.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression: a treatment manual. New York: Guilford Press; 1979.
McHugh RK, Hearon BA, Otto MW. Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am. 2010;33(3):511–25. https://doi.org/10.1016/j.psc.2010.04.012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Riccardo Dalle Grave, Simona Calugi, and Marwan El Ghoch declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
PubMed indexing: Dalle Grave, Calugi, El Ghoch
This article is part of the Topical Collection on Psychological Issues
Rights and permissions
About this article
Cite this article
Dalle Grave, R., Calugi, S. & El Ghoch, M. Are Personality Characteristics as Measured by the Temperament and Character Inventory (TCI) Associated with Obesity Treatment Outcomes? A Systematic Review. Curr Obes Rep 7, 27–36 (2018). https://doi.org/10.1007/s13679-018-0294-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-018-0294-y