Abstract
Purpose
The aim of the study was to examine the associations between personality, weight loss and obesity-related well-being post-bariatric surgery. It was hypothesised that persons who had undergone bariatric surgery who exhibit Extraversion, Conscientiousness, Agreeableness and Intellect/Imagination will have greater obesity-related well-being; whereas, those low on Emotional stability will have poorer obesity well-being.
Method
The cross-sectional sample comprised 127 females who had received bariatric surgery. The average age of participants was 45 years. Quality of life was measured using the Obesity-Related Well-Being scale (ORWELL 97). Personality was assessed with the International Personality Item Pool (IPIP) 50-item measure of the Five-Factor Model.
Results
The mean BMI for the sample was 34.13 (SD = 7.8). Females with a larger BMI who had undergone bariatric surgery had lower obesity-related well-being. Conscientiousness was negatively associated with BMI. Separate Hierarchical regression analyses found that Emotional stability (Beta = – .43, – .47, – .36) and Agreeableness (Beta = .27, .29, .25) predicted overall well-being, symptom occurrence and subjective relevance of distress, respectively. BMI predicted occurrence of symptoms (Beta = .23).
Conclusions
The findings have implications for the development of personality-informed interventions for bariatric patients in enhancing well-being and weight-loss maintenance following surgery.
Level of evidence
Level III: Evidence obtained from well-designed cohort or case-control analytic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Personality is fundamental to understanding an individual’s behaviour, thoughts and emotions. From a biopsychosocial perspective [1], personality has been acknowledged to impact disease risk, yet less attention has been accorded to the study of personality in adjustment to medical procedures, surgery outcomes and attendant well-being. The influence of personality on well-being post-bariatric surgery is the focus of this study.
Obesity is the abnormal or excessive accumulation of body fat and is defined as having a Body Mass Index (BMI) over 30 kg/m2. In Australia, 63% of adults are overweight or obese [2], with females being more likely than males to have a higher BMI. In 2014–15, 22,700 weight loss surgeries were performed in Australia [3] with obese women representing 79% of bariatric patients [3].
Bariatric surgery refers to the group of surgical interventions applied for weight loss. There are four types of bariatric surgery: Laparoscopic adjustable gastric banding (GB); Sleeve gastrectomy; Roux-en-Y gastric bypass (RYGB); and Duodenal switch with biliopancreatic diversion [3]. Gastric balloon is a non-surgical weight-reduction procedure whereby a balloon is inserted into the stomach to reduce the size of the stomach and, therefore, limit the amount of food the stomach can accommodate. Weight loss is achieved through these interventions by various methods of stomach reduction that in turn reduce hunger drive and the individual’s ability to consume large portions of food.
Personality traits are defined by cognitive, emotional, and behavioural patterns. The Five-Factor model or Big 5 identifies five personality traits consisting of Neuroticism (Emotional stability), Extraversion, Openness to experience (Intellect/Imagination), Agreeableness and Conscientiousness [4, 5]. The traits within the Five-Factor Model (FFM) of Personality have been linked to health outcomes and behaviours across many studies [6,7,8].
Personality traits contribute to obesity through their association with major controllable risk factors such as consumption of energy dense diets and low physical activity [9,10,11]. Australian research [12] reported Extraversion, Agreeableness and Neuroticism to be associated with obesity, while Conscientiousness was inversely associated with obesity. A meta-analysis by Jokela et al. [13] on the association between personality and obesity revealed that high Conscientiousness was associated with lower obesity risk. A more recent meta-analysis by Gerlach et al. [14] found neuroticism (and in particular the facet impulsivity) to be associated with overweight and obesity in population-based studies, and in clinical studies of obese persons undergoing bariatric surgery [14]. There was evidence for Extraversion to be associated with overweight, though only for men [14]. Conscientiousness was found to be a protective factor against obesity in population studies, and female bariatric patients had higher scores on Conscientiousness compared to matched controls [14]. Lower Openness to experience (Intellect/Imagination) has been found to be correlated with greater BMI [13, 15, 16] especially for women [17]. In regard to Agreeableness and its relation with obesity, the findings are not consistent with a meta-analysis reporting no association [13], other research reporting no difference between bariatric patients and weight-matched obese persons in the general population [18], while other research has reported a positive association [12] or a negative association [16]. The inconsistent findings are a function of the different measures of personality used and the nature of the sample, i.e. cross-sectional, general population or clinical samples.
Findings on the relationship between personality and weight loss are inconclusive and mixed [19, 20]. A 50 year longitudinal study of how personality traits are associated with fluctuations in body mass index revealed that participants higher on Neuroticism or Extraversion, or lower on Conscientiousness had higher BMIs and were more likely to go through cycles of gaining and losing weight throughout their lives [9]. Successful weight loss has been positively associated with the personality factor Neuroticism [21]. Other research did not find Neuroticism [22] or the facet impulsivity [23] to be associated with weight loss in bariatric patients. Novelty seeking, one of the personality dimensions of Cloninger’ psychobiological model of personality [24], was found to be lower in those who were successful in weight loss [25].
After Bariatric surgery, most patients report a greater improvement in psychosocial functioning and quality of life [26]. The benefits of this weight loss surgery have been recognised around the world, allowing for the dramatic increase in the demand for bariatric surgery. Improvements in well-being from baseline to 24 months post-surgery are reported regardless of type of surgery [27, 28]. Percent weight loss is positively correlated with well-being [29] though some weight regain over time is likely [30,31,32]. However, the research is lacking on personality differences in quality of life following bariatric surgery. There is research evidence for the Five-Factor Model of personality, in particular Neuroticism, Extraversion and Conscientiousness to be related to subjective well-being in general [33,34,35]. Given that personality is a determinant of BMI, weight loss, and well-being, the aim of the study was to explore whether persons with obesity have different quality-of-life outcomes following bariatric surgery, depending on their personality characteristics.
The hypotheses for the study were
-
1.
Obesity-related well-being will be lower for those with a higher BMI.
-
2.
High levels of Conscientiousness, Emotional stability and Intellect/Imagination will be associated with a lower BMI; whereas, high levels of Extraversion and Agreeableness will be associated with a higher BMI.
-
3.
Those participants scoring high on Extraversion, Emotional stability, Agreeableness, Conscientiousness and Intellect/Imagination will have higher obesity-related well-being post-bariatric surgery compared to those low on these personality markers.
-
4.
Personality will predict quality of life, symptom occurrence and symptom relevance after controlling for BMI.
Method
Participants and procedure
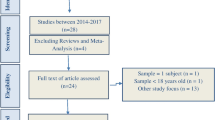
A sample of 127 females who had received bariatric surgery answered an online survey which included the International Personality Item Pool (IPIP) 50-item Questionnaire and the Orwell 97. The average age of respondents was 45 years (range 20–71 years). The Mean heaviest BMI for the sample was 47 kg/m2 (SD = 9.2), while the Mean current BMI was 34.1 kg/m2 (SD = 7.8). The Mean BMI change for the sample was 12.9 kg/m2. In regard to type of bariatric surgery undertaken, 73.9% had received the vertical sleeve, 18.5% the gastric bypass and 7.6% the gastric band. Only two respondents had received the intragastric balloon and were removed from the analyses. Bariatric surgery had occurred within the last 10 years for the majority of participants; 56.5% had received the surgery within the last 5 years with another 38.3% having received the surgery within 6 and 10 years. This study was approved by the James Cook University Human Research Ethics Committee (Approval ID H6584).
Measures
The International Personality Item Pool (IPIP) 50-item Questionnaire is a measure of the Five-Factor Model [5, 36, 37]. The scale consists of 50 items rated on a five-point Likert scale ranging from Very Inaccurate (1) to Very Accurate (5). The IPIP 50 was chosen for this study for its smaller number of items, its reliability evidence, and as its domains show a high correlation (0.85–0.92) to Costa and McCrae’s [38] revised NEO personality inventory (NEO-PI-R) [37]. Cronbach reliability estimates for the five factors of the IPIP 50 vary from 0.74 to 0.88 [37]. The current study found similar Cronbach alpha levels ranging from 0.75 to 0.88. A sample item for Extraversion is “I don’t mind being the centre of attention”. A sample item for Emotional stability is “I worry about things”, A sample item for Conscientiousness is “I pay attention to details”. The sample item “I make people feel at ease” reflects Agreeableness and the sample item “I am full of ideas” reflects Intellect/Imagination.
The Obesity-Related Well-Being Scale (Orwell 97) is a self-reported measure of obesity-related quality of life. The instrument was chosen as it considers both the intensity and subjective relevance of physical and psychosocial distress associated with obesity [39]. There are 18 questions consisting of two parts. It uses a 4-point Likert scale ranging from not at all (0) to much (3). Well-being is determined by the participants’ responses to questions that determine the occurrence of the symptoms (O:occurrence) and the relevance of said symptoms to their lives (R:relevance). Scores can be summed across items to obtain a total relevance score, and summing across items relating to occurrence gives a total occurrence score. The sum of items assessing occurrence weighted for relevance to well-being provides the total Orwell 97 score. High scores on the Orwell-97 indicate lower obesity-related well-being, while low scores indicate higher well-being [39]. Cronbach’s alpha for the overall scale was reported as 0.83 [39]. In the current study Cronbach’s alpha for the overall Orwell 97 was 0.90, for the symptom occurrence subscale α was 0.72, and for the symptom relevance subscale α was 0.89, indicating that the Orwell 97 is a very reliable assessment of obesity-related well-being. A sample item for Occurrence of symptoms is ‘Does being overweight interfere with your opinion of yourself? A sample item for the Relevance of symptoms is ‘Do you have a negative opinion of yourself?’.
Data analysis
Data were analysed using SPSS Statistics Software (Version 23). Pearson correlation was used to assess the association between BMI and obesity-related well-being (Hypothesis 1). To assess the association between personality dimensions and BMI, Pearson correlation was also used (Hypothesis 2). Hypothesis 3 assessed associations between personality and obesity-related well-being post-bariatric surgery using Pearson correlation. Hierarchical multiple regression was used to assess the predictive value of each of the personality factors for total Orwell 97 scores, symptom occurrence and the relevance of symptoms in separate regressions, after controlling for BMI of respondents (Hypothesis 4). For multiple hierarchical regression to be powered, a sample size of 98 was required (N > or equal to 50 + 8 m, where m is the number of predictor variables p. 117) [40]. There were six predictor variables, so our sample of 125 participants was powered to detect significant effects.
Results
As predicted by Hypothesis 1, BMI was significantly positively correlated with Orwell 97 total scores (r = 0.33, p = 0.001), symptom occurrence (r = 0.38, p = 0.001) and the subjective relevance of distress associated with obesity (r = 0.27, p = 0.01). Those respondents with larger BMIs had lower obesity-related quality of life.
Table 1 reports correlation coefficients and descriptive statistics for the variables. In support of Hypothesis 2, Conscientiousness was associated with a lower BMI (r = – 0.20, p < 0.05). No significant relationships were found for any of the other personality factors and BMI.
Significant correlations were found for Emotional stability and Conscientiousness on total Orwell 97 scores, and subscale scores supporting Hypothesis 3 (See Table 1). Intellect/Imagination was not associated with any of the well-being measures. Agreeableness was associated with Symptom occurrence. Extraverted respondents were more likely to have better well-being and to rate as lower the subjective relevance of physical and psychosocial distress associated with obesity, supporting Hypothesis 3. Contrary to expectation, high scores on Agreeableness were associated with lower well-being. The highest correlations were found between Emotional stability and Orwell 97 total scores (r = – 0.47), the occurrence of symptoms (r = – 0.47) and relevance of symptoms (r = – 0.41). Those respondents who had received bariatric surgery and scored high on Emotional stability were more likely to have greater obesity-related well-being, thus supporting Hypothesis 3.
The three hierarchical multiple regressions assessing the predictive value of each of the personality factors for total Orwell 97 scores, symptom occurrence and the relevance of symptoms, after controlling for BMI of respondents (Hypothesis 4) are presented in Table 2. The total variance explained by the model when the dependent variable was total Orwell 97 scores (i.e. symptoms weighted by relevance) was 33%, F(6,96) = 7.87, p = 0.001. At Step 1, BMI was associated with lower overall well-being (Beta = 0.33, p = 0.001). At Step 2 when the personality factors were entered into the regression, BMI became insignificant. Of the personality factors, the best predictor of obesity-related well-being was Emotional stability (Beta = – 0.43). Agreeableness also significantly predicted total Orwell 97 scores (Beta = 0.27). Emotionally stable persons who had undergone bariatric surgery reported better well-being. Those scoring high on Agreeableness reported lower well-being.
When the dependent variable was symptom occurrence as measured by the Orwell 97, total variance explained was 35.9%, F(6,96) = 8.96, p = 0.001. The best predictor of symptom occurrence was Emotional stability (Beta = – 0.47), followed by Agreeableness (Beta = 0.29) and BMI (Beta = 0.23). Those scoring high on Emotional stability reported less obesity-related symptoms which impact well-being; whereas, those scoring high on the personality factor of Agreeableness reported more symptoms. High BMI predicted greater symptom occurrence (see Table 2).
When the dependent variable was the subjective relevance of symptoms for well-being, 25.6% of the variance was explained by the personality factors and BMI, F(6,96) = 5.52, p = 0.001. The subjective relevance of symptoms for well-being was best predicted by Emotional stability (Beta = – 0.36). followed by Agreeableness (Beta = 0.25). Emotionally stable persons rated the subjective relevance of psychosocial distress for well-being as lower than any other personality type. High Agreeableness was associated with greater symptom rated relevance (refer to Table 2).
Discussion
The findings supported Hypothesis, 1 while partially supporting Hypotheses 2 and 3. Specific personality markers and BMI predicted overall obesity-related well-being, symptom occurrence and symptom relevance partially supporting Hypothesis 4.
Hypothesis 1: Obesity-related well-being will be lower for those with a higher BMI.
While the research indicates that quality of life is greater post-bariatric surgery, this is associated with the amount of weight lost [27, 28]. Weight regain over time is common [30,31,32] and impacts well-being. The current finding that those respondents with larger BMIs had lower well-being (Hypothesis 1) is consistent with this literature.
Hypothesis 2: High levels of Conscientiousness, Emotional stability and Intellect/Imagination will be associated with a lower BMI; whereas, high levels of Extraversion and Agreeableness will be associated with a higher BMI.
High levels of Conscientiousness were associated with a lower BMI in females who had received bariatric surgery supporting Hypothesis 2. However, there was no support for high levels of Extraversion and Agreeableness to be associated with a higher BMI. Meta-analytic findings [14] reported Extraversion to be associated with overweight only for men which is consistent with a lack of a correlation for women in the current study. Contrary to previous research [13, 15,16,17] less openness to experience (Intellect/Imagination) was not found to be associated with a greater BMI. Emotional stability was not significantly associated with a lower BMI. This finding is contrary to meta-analytic results [14] that neuroticism was associated with obesity in clinical studies of obese persons undergoing bariatric surgery. Previous Australian research [12] reported Conscientiousness to be inversely associated with obesity; whereas, neuroticism was positively associated with obesity. A meta-analysis of the association between personality and obesity furthermore reported a lower obesity risk for those individuals exhibiting the trait of Conscientiousness [13]. The current findings in relation to Conscientiousness and BMI are consistent with these previous studies.
Hypothesis 3: Those participants scoring high on Extraversion, Emotional Stability, Agreeableness, Conscientiousness and Intellect/Imagination will have higher obesity-related well-being post-bariatric surgery compared to those low on these personality markers.
In support of Hypothesis 3, participants who had bariatric surgery and exhibited Extraversion were more likely to have better well-being as measured by the Orwell 97. According to Costa and McCrae [4], extraverted individuals are more adjusted, maintain broader social networks and are happier than people who fall into the other personality traits. Extroverted traits help contribute to the individuals’ positive enjoyment and satisfaction in all aspects of life [4]. The current study adds to the research base by indicating that Extraversion is associated with a sense of well-being for obese persons post-surgery. Consistent with the literature [33,34,35] which has found Conscientiousness to be associated with subjective well-being in general, those females who were more conscientious reported higher well-being, less symptoms and less subjective relevance of symptoms to distress. Another finding was that emotionally stable participants (low on Neuroticism) had better well-being, thus supporting Hypothesis 3. This finding is consistent with research which has reported low neuroticism to be related to subjective well-being [33,34,35].
Hypothesis 4: Personality will predict quality of life, symptom occurrence and symptom relevance after controlling for BMI.
There was partial support for Hypothesis 4. BMI predicted symptom occurrence at Step 2 when personality factors were in the regression equation. When the dependent variable was overall well-being or symptom relevance, the effect of personality factors reduced BMI’s effects to insignificance. Of the personality factors, Emotional stability and Agreeableness significantly predicted all three well-being variables (total well-being, symptom occurrence and subjective relevance of symptoms). Those females who had received bariatric surgery and displayed the trait of Emotional stability (low Neuroticism) were more likely to have better well-being while those scoring high on Agreeableness had lower well-being. Conscientiousness, Extraversion and Intellect/Imagination did not have predictive value for obesity-related well-being. While Extraversion and Conscientiousness have been linked to subjective well-being in general [34, 35], they were not found to be significant predictors of well-being for females who had received bariatric surgery.
Limitations
Some limitations of the current study should be acknowledged. The cross-sectional nature of the study precludes any causal explanations. The focus of this research was females who had received bariatric surgery, as obese women represent 79% of bariatric patients in Australia [3]. Future research could study associations between personality and well-being for males who have undergone bariatric surgery. Another potential limitation is the use of the IPIP 50 as a measure of the Five-Factor Model [5, 36]. While this instrument was chosen for its brevity, reliability evidence [37], and correlations between its factors and those of the Revised NEO [37], more psychometric data need to be accumulated on the IPIP 50. Psychological disorders have been found to be preoperative predictors of weight loss following bariatric surgery [41]. This study did not collect data on any psychological disorders which the participants may have had, and future research may wish to include such information.
Implications and future directions
The current findings suggest the potential importance of emotional stability to well-being following bariatric surgery. Evidence for the malleability of traits such as neuroticism comes from intervention studies which have directly targeted emotional stability [42, 43]. The changeability of personality traits as a therapeutic outcome has implications for applied areas such as working with obese clients displaying core temperamental vulnerabilities linked to risk behaviours such as obesity.
Personality-informed interventions for emotional instability can be developed and assessed for their efficacy for bariatric patients. There is some evidence from a systematic review [44] that cognitive-behavioural, supportive psychotherapy and mixed therapeutic approaches can be effective in changing emotional instability. Components of such an intervention to target emotional instability in bariatric patients could include psychoeducation on emotions, mindfulness training of non-judgemental attitudes, identifying and changing maladaptive appraisals of situations and identification of behaviours such as emotional eating which may interfere with weight loss maintenance and well-being. Psychological interventions with a focus on mindfulness training [45] may also be useful in developing Conscientiousness in patients to facilitate weight loss maintenance following bariatric surgery.
Agreeableness characterised by altruism, compliance and sympathy [4] predicted symptom occurrence, symptom relevance and lower well-being in the current study. A possible explanation could be that obese persons may negate their own needs in favour of others’ needs, or may engage in risk behaviours such as eating inappropriate dietary foods in social settings in order to ‘fit in’. Psychological interventions for persons with obesity which target Agreeableness for change, through assertiveness and social skills training, could be implemented and tested.
Recent research [46] found that psychological counselling in general can have benefits for the mental well-being of bariatric patients. Personality assessment and interventions to change personality markers may facilitate post-surgery well-being.
Conclusion
By understanding the associations between personality, weight loss and obesity-related well-being, bariatric surgery intervention programs can be either adapted to different personality types, or can use therapeutic techniques to change personality facets to be conducive to weight loss maintenance and well-being. The challenge for clinical health psychologists working with obese clients is to negate the assumption that personality is stable and unchanging. Interventions informed by personality assessment can target for change those markers associated with poor bariatric outcomes.
What is already known on this subject?
-
Personality is linked to eating behaviours, obesity and successful weight loss.
-
Research is lacking on personality differences in quality of life following bariatric surgery.
-
What does this study add? Emotional stability and Agreeableness from the Five-Factor Model predicted obesity-related well-being, symptom occurrence and subjective relevance of distress following bariatric surgery.
-
Interventions informed by personality assessment can target for change those markers associated with poor bariatric outcomes.
Availability of data and material
The dataset generated during the study is available from the author on reasonable request.
References
Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science 196:129–136. https://www.ncbi.nlm.nih.gov/pubmed/847460
AIHW: Australian Institute of Health and Welfare (2018) Overweight and obesity. Accessed online on 28th Nov, 2018, at https://www.aihw.gov.au/reports-data/behaviours-risk-factors/overweight-obesity/overview
AIHW: Australian Institute of Health and Welfare (2017) Weight loss surgery in Australia 2014–15: Australian hospital statistics Cat. no. HSE 186. Canberra: AIHW
Costa PT, McCrae R (1980) Influence of extraversion and neuroticism on subjective well-being: Happy and unhappy people. J Pers Soc Psychol 38(4):668–678. https://doi.org/10.1037/0022-3514.38.4.668
Goldberg LR (1992) The development of markers for the Big-Five factor structure. Psychol Assessm 4:26–42. https://doi.org/10.1146/annurev.ps.41.020190.002221
Friedman H (2008) The multiple linkages of personality and disease. Brain Behav Immun 22(5):668–675. https://doi.org/10.1016/j.bbi.2007.09.004
Goodwin R, Friedman H (2006) Health status and the five-factor personality traits in a nationally representative sample. J Health Psychol 11(5):643–654. https://doi.org/10.1177/1359105306066610
Ozer D, Benet-Martínez V (2006) Personality and the prediction of consequential outcomes. Annu Rev Psychol 57:40–421. https://doi.org/10.1146/annurev.psych.57.102904.190127
Sutin A, Ferrucci L, Zonderman A, Terracciano A (2011) Personality and obesity across the adult life span. J Pers Soc Psychol 101(3):579–592. https://doi.org/10.1037/a0024286
Provencher V, Bégin C, Gagnon-Girouard M, Tremblay A, Boivin S, Lemieux S (2008) Personality traits in overweight and obese women: Associations with BMI and eating behaviours. Eat Behav 9(3):294–302. https://doi.org/10.1016/j.eatbeh.2007.10.004
Terracciano A, Sutin A, McCrae R, Deiana B, Ferrucci L, Schlessinger D, Uda M, Costa P Jr (2009) Facets of personality linked to underweight and overweight. Psychosom Med 71(6):682–689. https://doi.org/10.1097/PSY.0b013e3181a2925b
Magee CA, Heaven P (2011) Big-five personality factors, obesity and 2-year weight gain in Australian adults. J Res Pers 45:332–335. https://doi.org/10.1016/j.jrp.2011.02.009
Jokela M, Hintsanen M, Hakulinen C, Batty GD, Nabi H, Sing-Manoux A, Kivimaki M (2007) Association of personality with the development and persistence of obesity: A meta analysis based on individual participant data. Obes rev 14:315–323. https://doi.org/10.1111/obr.12007
Gerlach G, Herpertz S, Loeber S (2015) Personality traits and obesity: a systematic review. Obes Rev 16:32–63. https://doi.org/10.1111/obr.12235
McCann SJ (2011) Personality and American state differences in obesity prevalence. J Psychol 145:419–433. https://doi.org/10.1080/00223980.2011.584081
Van Reedt Dortland A, Giltay A, van Veen B, Zitman FG, Penninx BW (2102) Personality traits and childhood trauma as correlates of metabolic risk factors: the Netherlands Study of Depression and Anxiety (NESDA). Prog Neuropsychopharmacol Biol Psychiatry 36:85–91. https://doi.org/10.1016/j.pnpbp.2011.10.001
Armon G, Melamed S, Shirom A, Shapira I, Berliner S (2013) Personality traits and body weight measures: concurrent and across-time associations. Eur J Pers 27:398–408. https://doi.org/10.1002/per.1902
Pavan C, Azzi M, Lancerotto L et al (2013) Overweight/obese patients referring to plastic surgery: temperament and personality traits. Obes Surg 23:437–445. https://doi.org/10.1007/s11695-012-0769-y
Elfhag K, Rossner S (2005) Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 6(1):67–85. https://doi.org/10.1111/j.1467-789X.2005.00170.x
Van Hout G, Verschure S, Van Heck G (2005) Psychosocial predictors of success following bariatric surgery. Obes Surg 15(4):552–560. https://doi.org/10.1381/0960892053723484
Munro IA, Bore MR, Munro D, Garg ML (2011) Using personality as a predictor of diet induced weight loss and weight management. Int J Behav Nutr Phy 8:129–134. https://doi.org/10.1186/1479-5868-8-129
Van Hout GC, Hagendoren CA, Verschure SK, van Heck GL (2009) Psychosocial predictors of success after vertical banded gastroplasty. Obes Surg 19:701–707. https://doi-org.elibrary.jcu.edu.au/https://doi.org/10.1007/s11695-008-9446-6
Ryden O, Hedenbro J. Frederiksen S (1996) Weight loss after vertical banded gastroplasty can be predicted: a prospective psychological study. Obes Surg 6:237–243. https://doi-org.elibrary.jcu.edu.au/https://doi.org/10.1381/096089296765556827
Cloninger CR (1987) A systematic method for clinical description and classification of personality variants. Arch Gen Psychiatry 44:573–588
Sullivan S, Cloninger CR, Przybeck TR, Klein S (2007) Personality characteristics in obesity and relationship with successful weight loss. Int J Obesity 31:669–674. https://doi.org/10.1038/sj.ijo.0803464
Laurino Neto R, Herbella M (2013) Changes in quality of life after short and long term follow-up of roux-en-y gastric bypass for morbid obesity. Arq Gastroenterol 50(3):168–190. https://doi.org/10.1590/S0004-28032013000200033
Biter LU, van Buuren MM, Mannaerts GH, Apers JA, Dunkelgrun M, Vijgen GH (2017) Quality of life 1 year after laparoscopic sleeve gastrectomy versus laparoscopic roux-en-Y gastric bypass: a randomized controlled trial focusing on gastroesophageal reflux disease. Obes Surg 27:2557–2565. https://doi.org/10.1007/s11695-017-2688-4
Porta A, Aiolfi A, Musolino C, Antonini I, Zappa MA (2017) Prospective comparison and quality of life for single-incision and conventional laparoscopic sleeve gastrectomy in a series of morbidly obese patients. Obes Surg 27:681–687. https://doi.org/10.1007/s11695-016-2338-2
Monpellier VM, Antoniou EE, Aarts EO, Janssen IM, Jansen AT (2017) Improvement of health-related quality of life after Roux-en-Y Gastric bypass related with weight loss. Obes Surg 27:1168–1173. https://doi.org/10.1007/s11695-016-2468-6
Arapis K, Tammaro P, Parenti R et al (2017) Long-term results after Laparoscopic adjustable gastric banding for morbid obesity: 18 year follow-up in a single University unit. Obes Surg 27:630–640. https://doi.org/10.1007/s11695-016-2309-7
Kowalewski PK, Olszewski R, Kwiatkowski A, Galazka-Swiderek N, Cichon K, Pasnik K (2017) Life with a gastric band, long-term outcomes of Laparoscopic adjustable gastric banding – a Retrospective study. Obes Surg 27:1250–1253. https://doi.org/10.1007/s11695-016-2435-2
Monaco-Ferreira DV, Leandro-Merhi VA (2017) Weight regain 10 years after Roux-en-Y gastric bypass. Obes Surg 27:1137–1144. https://doi.org/10.1007/s11695-016-2426-3
Garcia D (2011) Two models of personality and well-being among adolescents. Person Individ Differ 50:1208–1212. https://doi.org/10.1016/j.paid.2011.02.009
Lyubomirsky S, Sheldon KM, Schkade D (2005) Pursuing happiness: The architecture of sustainable change. Rev Gen Psychol 9:111–131. https://doi.org/10.1037/1089-2680.9.2.111
Weiss A, Bates TC, Luciano M (2008) Happiness is a personal(ity) thing The Genetics of Personality and well-being in a representative sample. Psychol Sci 19(3):205–210
Goldberg LR, Johnson JA, Eber HW, Hogan R, Ashton MC, Cloninger CR, Gough HG (2006) The international personality item pool and the future of public-domain personality measures. J Res Pers 40:84–96. https://doi.org/10.1016/j.jrp.2005.08.007
Buchanan T, Johnson JA, Goldberg LR (2005) Implementing a five-factor personality inventory for use on the Internet. Eur J Psychol Assess 21:116–128. https://doi.org/10.1027/1015-5759.18.1.116
Costa PT, McCrae RR (1992) Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources, Odessa, FL
Mannucci E, Ricca V, Barciulli E, Di Bernardo M, Travaglini R, Cabras PL, Rotella CM (1999) Quality of life and overweight: The obesity related well-being (Orwell 97) Questionnaire. Addict Behav 24(3):345–357. https://www.ncbi.nlm.nih.gov/pubmed/10400274
Tabachnick BG, Fidell LS (2001) Using multivariate statistics, 4th edn. Allyn & Bacon, Boston
Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, Ko CY, Magggard GM (2012) Preoperative predictors of weight loss following bariatric surgery: Systematic review. Obes Surg 22:70–89. https://doi.org/10.1007/s11695-011-0472-4
Roberts BW, Luo J, Briley DA, Chow PI, Fu R, Hill PL (2017) A systematic review of personality trait change through intervention. Psychol Bull 143(2):117–141. https://doi.org/10.1037/bul0000088
Barlow DH, Ellard KK, Fairholme C, Farchione TJ, Boisseau C, Allen L, Ehrenreich-May J (2011) Unified protocol for the transdiagnostic treatment of emotional disorders. Oxford University Press, New York
Sauer-Zavala S, Wilner JG, Barlow DH (2017) Addressing neuroticism in psychological treatment. Personal Disord 8(3):191–198. https://doi.org/10.1037/per0000224
Fulton P, Germer C, Siegel R (2005) Mindfulness and Psychotherapy. Guilford Press, New York
Ristanto A, Caltabiano ML (2018) Psychological support and well-being in post-bariatric surgery patients. Obes Surg. https://doi.org/10.1007/s11695-018-3599-8
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
MC was responsible for study conceptualization, data collection and analysis, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflict of interest financial or non-financial to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the James Cook University Human Research Ethics Committee and the National Health and Medical Research (NHMRC) guidelines, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Human Research Ethics Committee of James Cook University (Approval ID H6584).
Informed consent
Informed consent was obtained from all individuals included in the study.
Consent for publication
No identifying information about participants is available in the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Caltabiano, M.L. Personality, weight loss and obesity-related well-being post-bariatric surgery. Eat Weight Disord 27, 199–206 (2022). https://doi.org/10.1007/s40519-020-01086-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-01086-0