Abstract
Background
In spite of various treatment options currently available, ovarian cancer (OC) still remains a leading cause of death in women world-wide. Diagnosis at an early stage is one of the most important factors that determines survival. Current clinical diagnostic tools have, however, a limited efficacy in early OC detection. Therefore, there is a critical need for new (early) diagnostic biomarkers and tools. Through advances in genomic, proteomic and metabolomic techniques, several novel molecular OC biomarkers have recently been identified. These biomarkers are currently subject to validation. In addition, integration of genomic, proteomic and metabolomic data, in conjunction with epidemiologic and clinical data, is considered essential for obtaining useful results. Interesting recent work has already shown that specific diagnostic biomarkers, such as BRCA mutations, may have profound therapeutic implications. Here, we review the current state of OC research through literature and database searches, with a focus on various recently identified biomarkers via different technologies for the (early) diagnosis, prognosis and treatment of OC.
Conclusions
Multi-biomarker panels accompanied by a meticulous determination of their sensitivity and specificity, as well their validation, using multivariate analyses will be critical for its clinical application, including early OC detection and tailor-made OC treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Ovarian cancers (OCs) are considered to be the most deadly gynecological cancers [1, 2]. They are the seventh leading cause of cancer and the eighth leading cause of cancer-related death among women worldwide [1]. The highest incidences are observed in Central and Eastern Europe and the lowest in West Africa [1, 2]. Although the prognosis is mostly excellent at an early stage of the disease, a lack of specific symptoms, a poor anatomical accessibility of the ovaries, ignorance of tumor growth kinetics (i.e., a possible pre-clinical latent phase), together with its relative rarity, represent barriers to its early detection [3, 4]. Although a modest improvement in OC survival in the last decades has been reported [5], women diagnosed with OC at an advanced stage still reach 5 year survival rates of less than 20%, including cases that undergo surgery and chemotherapy, whereas in women who are diagnosed at an early stage the survival rates rise up to 90% [2, 6]. Hence, early diagnosis is one of the most important determinants in the successful treatment and survival of OC. The present techniques to diagnose OC at its first stages are, however, not well developed and not very precise.
The current routine detection of OC is primarily based on the serum level of CA-125, which shows an increase of ~80–85% in women with OC. This biomarker does, however, not always show an increase at the first stages of OC development and, therefore, only ~50% of these cases can be diagnosed using this biomarker. Although CA-125 is useful and widely used for OC monitoring, it lacks both the sensitivity and the specificity for early OC detection [2]. Early detection strategies must reach both a high sensitivity (> 75%) and a very high specificity (99.6%) in order to achieve a positive predictive value (PPV) of at least 10% [2, 6–8]. Since these requirements are not met by CA-125, the discovery of new biomarkers appears to be a prerequisite. Next to several recently identified novel biomarkers, advances in translational research, including the use of liquid biopsies, are expected to accelerate the discovery of such biomarkers and, thereby, to improve personalized OC patient care. In this review we discuss novel OC biomarkers that have recently been reported, including proteomic biomarkers, metabolomic biomarkers, exosomes, circulating tumor cells, peritoneal biomarkers, epigenetic biomarkers and microRNAs, with a focus on the pathogenesis of OC and its (early) diagnostic and therapeutic perspectives.
In recent years, the number of publications on both basic and clinical OC research has shown a rapid growth (Supplementary Fig. 1) [9]. We conducted a publication search in the Scopus, Medline/PubMed and Web of Science (Thomson Reuters®) databases from 2010 to 2016, using a combination of medical subject heading terms (MeSH) and keywords. Clinical trials were searched from the registry as well as the database of the U.S. National Institute of Health (www.clinicaltrials.gov). The MeSH terms used included ‘ovarian cancer’, ‘biomarkers’, ‘diagnosis’, ‘prognosis’, ‘proteomics’, ‘metabolomics’, ‘circulating tumor cells’, ‘peritoneal biomarkers’ and ‘epigenetics’. Published full-text articles were selected from the international peer reviewed literature. We independently identified and evaluated relevant scientific literature that provided information on the use of OC biomarkers in oncological practice, experimental research and clinical trials. Each article abstract was analyzed according to pre-selected criteria. The results of this initial screening were cross-referenced and full-text records were obtained for all potentially relevant articles. The references in all included articles were also checked.
2 Histopathologic and molecular characteristics of ovarian cancer
Several recent studies have highlighted the histological and molecular heterogeneity of OCs, including subtypes with significant differences in morphology, oncogenesis, prognosis, chemo-sensitivity and molecular alterations that may serve as targets for new therapeutic approaches [10–12]. Using high throughput sequencing technologies, a vast number of genomic alterations has been identified. Specifically, it has been found that type II carcinomas (high grade) are characterized by a high genomic instability and the occurrence of frequent amplifications and deletions, whereas type I carcinomas (low grade) are stable at the overall genomic level, but frequently exhibit point mutations [13–16].
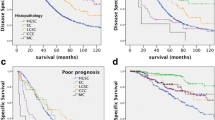
The majority of OCs is epithelial in origin (75–80%) [17, 18]. Non-epithelial OCs include germ cell tumors and other rare tumors such as small cell cancers [19, 20]. These latter OCs tend to develop in younger women, are usually diagnosed at an earlier stage and generally have a better prognosis. Among the epithelial OCs, ovarian adenocarcinomas typically occur as high-grade tumors. Epithelial OCs with a papillary serous histology, occurring in patients over 60 years of age, are usually diagnosed at an advanced stage (75% in stage III-IV) [21, 22]. They are poorly differentiated and rarely express the estrogen receptor [23]. Overall, ovarian adenocarcinomas can be divided into two sub-groups based on their grade and morphology: type I, including low-grade serous and mucinous carcinomas, endometrioid carcinomas, clear cell carcinomas and transitional cell carcinomas and type II, including high-grade serous adenocarcinomas, carcinosarcomas, undifferentiated carcinomas and high-grade endometroid carcinomas (Fig. 1a and b). Despite the occurrence of these histological subtypes, OCs are currently treated as a single disease.
2.1 Type I ovarian carcinomas
Low grade type I OCs are typically well differentiated, and are characterized by an overall genomic stability and an absence of p53 mutations. These carcinomas are often restricted to the ovary (stage I), at which stage surgical excision allows a high recovery rate [24]. In case of advanced stage or recurrence, chemotherapy with platinum salts is indicated, but this treatment does not seem to be very effective. The more advanced tumors evolve mostly from pre-invasive lesions such as serous or mucinous cystadenomas, or from endometriosis in the case of endometrioid or clear cell tumors [24, 25]. These tumors are also highly angiogenic, which has prompted the initiation of several clinical trials using tyrosine kinase receptor-associated VEGF inhibitors [26–28]. Additionally, these tumors frequently carry mutations in the KRAS and BRAF genes [17, 24].
2.2 Type II ovarian carcinomas
High grade type II OCs are usually diagnosed at an advanced stage and most of them require surgical resection in combination with adjuvant chemotherapy. Despite the fact that the response rate to cisplatin-paclitaxel combination treatment is in the order of 75%, relapse is almost inevitable and underlies a relatively low five-year survival rate of ~30% [29]. The tumors develop from epithelial cells originating from both the ovary and the fallopian tube. Recent data suggest that these tumors do not progress from pre-invasive lesions but rather develop de novo as a result of mutations in the tumor suppressor gene p53 [30–33]. Inactivating p53 mutations are indeed ubiquitous in type II adenocarcinomas [34] and high throughput sequencing has confirmed the presence of p53 mutations in 96% of the type II adenocarcinomas. These tumors are not only characterized by a high proliferation rate, but also by a high genetic instability due to their decreased DNA repair capacity. Other inactivating mutations in tumor suppressor genes such as NF1 and RB1 have also been encountered in these tumors, whereas activating mutations in oncogenes such as KRAS, BRAF, PTEN, HER2, EGFR and KIT turned out to be rare (Fig. 2 summarizes some of these alterations as well as others encountered in OC) [35].
It has also been found that up to 19–22% [36] of the high-grade serous adenocarcinomas may carry (germline or somatic) mutations in either the BRCA1 or the BRCA2 gene [37]. Also these mutations result in a decreased capacity to repair damaged DNA, especially homologous recombination repair of double-strand breaks (DSBs) generated by platinum salts [38]. Normally, single strand DNA breaks are repaired by poly-ADP-ribose polymerase (PARP). Interestingly, it has recently been found that PARP inhibitors such as olaparib elicit encouraging therapeutic effects in BRCA1 and BRCA2-deficient OCs (i.e., synthetic lethality concept) and several clinical trials have been carried out to evaluate the efficacy of PARP inhibitors in these tumors [39, 40]. In 2014, the European Medicines Agency (EMA) has approved PARP inhibitor monotherapy for maintenance treatment of adult patients with platinum-sensitive relapsed BRCA-mutated (germline or somatic) high grade serous epithelial ovarian, fallopian tube or primary peritoneal cancers. Several next-generation sequencing techniques have been developed to detect BRCA1 and BRCA2 mutations in patient-derived blood DNA [41, 42]. Until recently, the detection of such mutations in DNA derived from formalin-fixed and paraffin embedded (FFPE) tumor tissue has not attracted much attention due to its low quality and high degree of fragmentation. For an effective and reliable detection of these mutations in FFPE tissue samples, a novel and promising test has very recently been developed [36]. This test is based on single molecule molecular inversion probe (smMIP)-targeted sequencing [43] and appears to reliably detect somatic mutations in FFPE tissue samples with a sensitivity of 97,8%. As such, OC patients can now efficiently be selected for PARP inhibitor treatment and, in addition, the detection of a possible hereditary risk.
3 Serological biomarkers
Large-scale gene expression analyses have led to the identification of a myriad of genes that are over-expressed in OCs and that, as such, may serve as candidate biomarkers. However, since gene expression patterns are dynamic and may depend on both genetic and epigenetic factors, attention has shifted to protein-based biomarkers. To this end, protein microarrays (chips), as well as methods to profile metabolites and, more recently, exosomes have been developed and applied to unravel the molecular mechanisms underlying OC initiation and progression and to generate useful serological biomarkers.
3.1 Proteomic biomarkers
3.1.1 Cancer antigen-125
Cancer antigen-125 (CA-125) is a large transmembrane glycoprotein that is encoded by the MUC16 gene. CA-125 over-expression was first detected in ovarian carcinoma-derived cell lines using monoclonal antibody OC125. Despite its early identification, a specific function of CA-125 still remains to be defined both in normal physiologic conditions and in cancer development [44]. In addition, it has been found that certain factors such as race/ethnicity, age, smoking history, obesity and hysterectomy may alter CA-125 levels. Despite this well-recognized limitation, CA-125 is still regarded as the gold standard and is widely used as serum biomarker for OC detection. CA-125 is approved by the US FDA for disease monitoring in patients diagnosed with epithelial OC. It is also used for OC screening in women who have an increased risk due to congenital BRCA mutations, combined with transvaginal ultrasound examination [45]. The recommendations of the National Academy of Clinical Biochemistry (NACB) panel for CA-125 as a biomarker in OC are (i) for combined use with trans-vaginal ultrasound examination for early detection in hereditary syndromes, (ii) for differential diagnosis in cases with a suspicious pelvic mass, (iii) for recurrence detection, (iv) for therapy monitoring and (v) for prognostication. The NACB panel does not recommend CA-125 for OC screening, especially in asymptomatic women, due to its lack of sensitivity and specificity as a single marker.
In a cancer screening trial in the USA, which included prostate, lung, colorectal and ovarian cancer (PLCO), 78,216 healthy women (aged 55 to 74 years) were randomly selected for either annual CA-125 and trans-vaginal ultrasound examination or for standard care. The team reported that CA-125/transvaginal sonography (TVS) screening did not lead to a reduction in OC mortality rates compared to standard care and that, additionally, false-positive screening results were found to be associated with complications due to unnecessary surgery [46]. On the other hand, in the United Kingdom Collaborative Trial of OC Screening (UKCTOCS), 202,638 postmenopausal women assumed to be at an average risk for OC were allocated randomly for an annual multimodal screening, encompassing CA-125 screening, ultrasound screening and/or no screening [47]. The team reported that multimodal screening yielded a significantly higher specificity compared to ultrasound screening alone (99.8% versus 9.2%), as well as a higher positive predictive value (PPV; 35.1% versus 2.8%), whereas the sensitivities did not significantly differ between these two groups. Serum CA-125 levels are still widely used in large OC screening programs, but it is clear that combining CA-125 with other markers such as HE4, CA19–9, CA72–4 and/or CA-153 may considerably improve the sensitivity of the screening and the monitoring of recurrences [48]. Additionally, advances in genomic and proteomic technologies have provided opportunities for the discovery of novel OC biomarkers.
3.1.2 Risk of ovarian malignancy algorithm
A scoring system called risk of ovarian malignancy algorithm (ROMA) has been developed for the assessment of menopausal status as a reference for a high or low risk of a malignancy in women presenting with a pelvic mass. ROMA is a serum-based scoring system that combines CA-125 and HE4 serum levels. In a prospective, multicenter, blinded clinical trial, ROMA was used to evaluate 472 women diagnosed with a pelvic mass. Nine of these women were found to exhibit OC [49]. Overall, ROMA provided a 93.8% sensitivity and a 74.9% specificity, whereas a100% sensitivity and a 74.2% specificity were achieved in pre-menopausal women. Based on this clinical trial, and the fact that it was found to be beneficial for patients with OC in terms of mortality and morbidity [48], ROMA has been approved by the US FDA for OC risk estimation in pre- and post-menopausal women with pelvic masses [49]. It has been found that HE4 shows a similar specificity and sensitivity as CA-125, but a decreased false-positive yield [50]. Very recently, Xu et al. [51] reported that HE4 may serve as a better predictor of malignancy than CA-125 in patients with a pelvic mass and as a better biomarker for the diagnosis of early-stage epithelial OC.
3.1.3 Multi-marker assays
In the past, multi-marker assays have been developed to distinguish OC cases from healthy controls using different panels of old and novel biomarkers such as CA-125, ApoA1 and TTR, or CA-125, CA72.4 and M-CSF, or CA-125, IL-6, IL-8, VEGF and EGF, or CA-125, TTR and ApoA1, or CA-125, leptin, PRL, OPN, IGF-II and MIF, or CA-125, HE4, glycodelin, Plau-R, MUC1 and PAI1, or CA-125, HE4, CEA and VCAM-1, or CA-125, CRP, SAA, IL-6 and IL-8 [52, 53]. All these proteins were found to be secreted at various (elevated) levels in the majority of OCs, necessitating their combination for obtaining sensitive detection levels. Additional promising avenues have more recently been explored with new biomarkers, next to CA-125, for OC detection [54, 55]. Yurkovetsky et al. [54] for example investigated 96 serum biomarkers in healthy women and OC patients (139 patients with early stage OC, 149 patients with late stage OC and 1102 healthy women) using multiplex xMAP bead-based immunoassays. A four-biomarker panel (CA-125, HE4, CEA and VCAM-1) turned out to provide the highest diagnostic power with a 86% sensitivity for early stage OC detection and a 93% sensitivity for late stage OC detection with a specificity of 98%. This test was also applied to an independent blinded validation cohort and, by doing so, found to provide a 86% sensitivity for stage I and II OC detection and a 95% sensitivity for stage III OC detection. Recently, the European EPIC cohort was employed to prospectively evaluate the performance of some of the most promising OC screening biomarkers [56]. In this study the serological levels of CA-125, HE4, CA72.4 and CA15.3 were measured in 810 OC cases and 1939 controls. It was found that the best biomarker was CA-125, followed by HE4, CA72.4 and CA15.3, respectively. So, although CA-125 is still the best and single most widely used biomarker for the early detection of OC, its performance can be improved through its combination with other biomarkers, as has been shown using multi-marker assays.
Yet another panel (OVA1) has been approved by the US FDA as a test panel for patients with a pelvic mass [57]. This panel contains five biomarkers (CA-125, Transthyretin, APOA-1, β2-Microglobulin and TF) that have been identified using SELDI-TOF-MS [58]. The OVA1 test, which has replaced the CA-125 test in the ovarian tumor referral guidelines of the American College of Obstetricians and Gynecologists (ACOG), provides a sensitivity of 94% and a specificity of 35%, with a positive predictive value (PPV) of 40% and a negative predictive value (NPV) of 93%. It provides an increase in NPV, but a decrease in PPV, compared to the CA-125 test [59]. The US FDA-approved ROMA and OVA1 tests represent prime examples of tests for the detection of a wide range of OCs, including early-stage OCs and disease among pre- and post-menopausal women, and of obtaining specificity for benign masses.
Using nanotechnology, point-of-care platforms for OC detection hold promise for low-cost and large-scale screening purposes. Multiplexed biomarker panels may provide a high sensitivity and specificity for the early detection of OC. In this respect, Shadfan et al. [60] configured a programmable bio-nano-chip (p-BNC) with an immunoanalyzer system to quantify a multi-marker panel comprising CA-125, HE4, MMP-7 and CA72.4. By using this system, they obtained a high specificity, a low cross-reactivity, low detection limits and a short analysis time (43 min). The p-BNC system appears promising for large-scale OC screening, with rapid results at low costs. Additional interesting OC biomarker panels currently under investigation are listed in Supplementary Table 1 [53, 61, 62], for which trials encompassing large patient-control cohorts are required. Some of these trials are currently ongoing (Supplementary Table 2).
3.1.4 Other proteomic biomarkers
Additional biomarkers have shown to be promising for OC screening, including certain members of the kallikrein family, especially hK6, hK10 and hK11, of which the levels have been found to be elevated in OC patient sera [63, 64]. As a result, a combined CA-125/ hKs assay could be developed with a specificity of > 90% for early stage (stages I and II) OC detection [65]. When all these proteins were combined with CA-125, the sensitivity increased to 74% and the specificity to 97%.
The p21 protein binds with and inhibits the activity of cyclin-CDK2 and cyclin-CDK4 complexes [66] and can mediate p53-dependent G1 phase cell cycle arrest. The p21 protein also appears to be an excellent predictor of treatment response and survival among OC patients, especially the p53-negative ones [67]. In addition to p21, also p57 and p27 represent promising prognostic OC biomarkers, and a decreased p27 level has been associated with a poor survival rate [68]. Also RB1, another cell cycle regulator [69] and BCL-2, which is involved in apoptosis [70], have been found to serve as important prognostic biomarkers. The latter has also been associated with response to chemotherapy, similar to BAX [71]. VEGF, an important growth factor implicated in angiogenesis, is considered to be a biomarker for early OC detection and prognosis. Lawicki et al. [72] investigated serum VEGF levels in comparison to plasma HE4 and CA-125 levels in 100 OC patients. They found that the VEGF levels were significantly higher in the OCs compared to those in control groups, suggesting its usefulness for early OC detection, especially in combination with CA-125 and HE4 [72].
A new biomarker, protein Z (a serine protease acting in the coagulation cascade), was recently introduced as a promising biomarker for early OC detection when combined with CA-125. In a blinded study on serum collected from participants in the UKCTOCS trial, protein Z was found to be significantly up-regulated in the OC cases and to, indeed, serve as a new early OC detection biomarker [73].
3.2 Metabolomic biomarkers
OCs possess several properties that are considered essential for the development of cancer, including altered cellular signaling and metabolic pathways, as well as secondary modifications of proteins, carbohydrates and lipids. It has been found that omental adipocytes may provide energy-rich lipids for OC growth and metastasis [74]. Therefore, lipid metabolism and transport processes may serve as promising targets for therapeutic intervention [75]. It is well-known that for their energy supply cancer cells may shift from oxidative phosphorylation to glycolysis, resulting in the generation of lactate for ATP production, while their oxygen requirements remain similar to non-transformed cells (i.e., the Warburg effect) [76, 77]. Hence, by increasing their glucose catabolism, cancer cells must increase their glucose uptake through the up-regulation of glucose transporters (GLUT 1–9) [78]. This increase in glycolysis involves the AKT pathway through nuclear factor-κB (NF-κB) and hypoxia-inducible factor 1 (HIF1), as well as transporters and glycolytic enzymes (GLUT, hexokinase 2 and LDH) [78] and certain isoenzymes, such as pyruvate kinase 2 (PKM2) [79]. OC has also been found to be associated with a set of canonical pathways affecting the synthesis of aminoacyl-tRNA, phenylalanine, tyrosine and tryptophan, the urea cycle and the metabolism of glycine, serine, threonine, glutamate and amino groups [80]. These latter compounds may be used as surrogate end-points in clinical OC trials using new metabolic targets.
3.3 Exosomes
Exosomes (Exo) are small extracellular membrane vesicles with a diameter of 30–100 nm, that are derived from the endosomal cellular compartments and are released by the fusion of multi-vesicular bodies with the cell membrane [81, 82]. They are recognized as mediators of intercellular communication and as regulators of both systemic and local processes. They can transfer their functional content (i.e., proteins, metabolites, DNAs, mRNAs, non-coding RNAs and retro-transposon elements) from donor cells to recipient cells [83–85] and may serve as gene delivery systems [86]. OC-derived Exo can bind to stroma cells and, by doing so, support OC growth and progression, inducing angiogenesis and vasculogenesis, immunosuppression and the recruitment of bone marrow-derived progenitors to the primary tumor or to the sites of metastasis [87]. Exo secretion is controlled by the RAB family of small GTPases, i.e., the Rab11, Rab27, Rab35 and SNARE proteins [88]. Several proteins have been identified in OC-derived Exo such as the tetraspanins CD63 and CD81, the major histocompatibility complex I (MHCI), the lysosomal-associated membrane proteins 1 and 2 (LAMP1, LAMP2) and the tumor susceptibility gene 101 protein (TSG101) [88]. Additionally, it has been found that OC-derived Exo may contain proteins and nucleic acids that define a specific signature of a donor cell [89], in particular tetraspanins and glycosylphosphatidyl-inositol-anchored membrane proteins such as CD24 [89]. Interestingly, it has been found that patient blood serum enriched in Exo represents an easy and accessible source for potential biomarkers such as micro-RNAs, proteins and metabolites that may act in an autocrine manner, which may be instrumental for improving the diagnostic accuracy of OC and other tumor types [89–92].
4 Role of circulating tumor cells
According to Hanahan and Weinberg [93], the genesis of metastases from epithelial tumors, as is the case with OC, involves several steps. Cancer cells may actively detach from the primary tumor and subsequently circulate in the blood or lymphatic system to reach distant organs [94]. These circulating tumor cells (CTCs) are viable cells that can be isolated and detected using various approaches (highly sensitive and specific methods combined with enrichment and detection technologies) that are based on their physical and biological properties (liquid biopsy in real time conditions) [95, 96]. Since the primary way of OC spreading is direct into the peritoneal cavity and distant metastases only occur in 25% of the patients, research on CTCs in the case of epithelial OC has gained little interest. Recent studies have, nevertheless, revealed an important role of OC spread through blood and lymph vessel systems and have shown that the presence of CTCs may be associated with an advanced tumor stage. Currently, there are several ongoing clinical trials (www.clinicaltrials.gov-National Institutes of Health) that use this concept in OC and other cancers (Supplementary Table 3).
Various techniques have been developed to detect, enumerate and characterize CTCs. Currently, positive immunomagnetic enrichment methods, based on markers expressed on the surface of CTCs, in association with immunostaining and qRT-PCR for visualization and quantification, respectively, are widely used for the detection of CTCs in experimental and clinical settings, but they are still subject to changes related to the continuous emergence of new techniques [93, 97]. Recently, Obermayr et al. [98] conducted a study to identify novel CTC biomarkers in OC patients through microarray-based gene expression analyses, comparing matched OC tissues and blood leucocytes. They found that CTCs could be detected in 24.5% of the baseline (diagnosis) samples and in 20.4% of the follow-up samples, of which two thirds were identified by over-expression of the cyclophilin C gene (PPIC). The presence of CTCs at diagnosis was correlated with the presence of ascites and elevated CA-125 and HE4 levels. In another study conducted by the same group to identify new gene markers for PCR-based detection of CTCs [99], it was found that a panel of six genes (CCNE2, DKFZp762E1312, EMP2, MAL2, PPIC and SLC6A8) was superior to EpCAM (Epithelial cell adhesion molecule) and Hmam (Human mammaglobin) for the detection of CTCs in peripheral blood of breast cancer patients. These genes may also serve as biomarkers for CTCs derived from endometrial, cervical and ovarian cancers. Very recently, Kolostova et al. [100] succeeded in culturing CTCs derived from OC patients (mainly stage IIIB-C) using a recently developed separation technology (MetaCell®). By using this approach, CTCs could successfully be detected in 77 out of 118 OC patients (65.2%). In another similar study, Kolostova et al. [101] used the MetaCell® technique to detect CTCs via vital fluorescence microscopy-based cytomorphologic evaluation combined with relative gene expression analysis. This study confirmed a statistically significant difference in expression of the KRT7, WT1, EpCAM, MUC16, MUC1, KRT18 and KRT19 genes. The authors concluded that a combination of these genes may confirm the presence of CTCs in OC patients with a high degree of specificity. Since validation studies are still ongoing, no definite conclusions can currently be drawn on the use of CTCs for early OC detection. To this end, results from further CTC detection studies as well as from larger cohort trials are awaited.
5 Peritoneal biomarkers
Ascites formation frequently results from pro-inflammatory cytokines and growth factors that induce the collection of fluids and cells through lymphangiogenesis, angiogenesis and vessel obstruction. OC is considered to be the most frequent cause of malignant ascites formation [55]. The detection of cancer cells, cell-free tumor DNA and proteins in peritoneal ascitic fluids by culdocentesis and/or aspiration indicates that the epithelial basement membrane is degraded, facilitating the passage of cancer cells. As such, it constitutes a poor prognostic indicator for OC. The search for biomarkers in peritoneal fluids in patients with OC has attracted the attention of researchers whose main focus is early detection. According to the “seed and soil paradigm”, cancer cells have a tendency to disseminate via different routes such as blood vessels, lymphatic vessels and tumor stroma, to reach certain sites [102]. This is also observed in OC [103, 104]. During OC progression, tumor cells can freely metastasize to the peritoneal cavity and adhere to the peritoneal lining to reach systemic circulation. At advanced stages, the omentum is affected in 80% of the cases [17, 104, 105].
Prior to the availability of modern biochemical methods, the assessment of peritoneal fluid by culdocentesis has been used as standard method [106]. Since in the case of OC fluids cancer cells may accumulate in the posterior pelvic cul-de-sac (pouch of Douglas) [107], this notion may provide important information on OC diagnosis at an early stage [106]. Actually, two clinical trials for which patients are still being recruited use this procedure to detect tumor cell-free DNA, HE4 and CA-125 (Supplementary Table 4). Interestingly, Kucukgoz et al. [108], using a cross-sectional study, assessed CA-125, ferritin, beta-2 microglobulin (b2M) and LDH levels in peritoneal fluids of 59 patients with OC, and compared these to those in 40 patients with benign tumors. They found that the CA-125, ferritin, b2M and LDH levels in the peritoneal fluids were significantly higher in the OC patients compared to those in patients with benign tumors. The analysis of ascites by microfluidic chips was developed by Peterson et al. [109]. They evaluated 85 commonly recognized OC biomarkers and found that two-thirds of them were either non-specific for OC or exhibited a low abundance. In addition, they found that the expression of EpCAM, CD24 and TAG24 was high in OC patients compared to controls. Since microfluidic chips can be developed at a low cost and are simple to use, they are considered as promising tools for OC screening [109]. Also, up-regulated proteins in peritoneal fluids of serous OC patients have been detected using label-free mass spectrometry [110]. In this latter study, 21 proteomic biomarkers were investigated that had previously been reported as being up-regulated in OC, of which 19 were previously validated and detected in peritoneal fluids of serous OC patients.
6 Epigenetic biomarkers
Epigenetic changes are defined as chromatin alterations that do not affect the DNA sequence itself [111–113], and include DNA methylation and histone methylation, acetylation or phosphorylation [114]. Aberrant DNA methylation is frequently observed in various cancers and has been found to be one of the earliest molecular modifications during cancer development [112, 115, 116]. As such, epigenetic changes hold great promise as biomarkers for (early) cancer detection. In addition, miRNAs are considered as epigenetic modifiers that, in analogy to the above mentioned epigenetic modifications, also hold promise for (early) cancer detection.
6.1 DNA methylation and histone modification
Several technologies such as next generation bisulfite sequencing have been developed to assess DNA methylation, either genome-wide or at specific loci. This work has revealed several DNA methylation changes that may serve as biomarkers for OC (Fig. 3) [117]. Other studies have reported specific methylation patterns in cell-free circulating DNA of OC patients, indicating that DNA methylation may also serve as a non-invasive biomarker [118, 119]. Specifically, it has been shown that CpG island gene promoter hypermethylation is a recurrent event in OC [120]. However, the frequency and degree of methylation varies widely among the studies reported. Next to classical anti-oncogenes (i.e., tumor suppressor and DNA repair genes) such as BRCA1, p16, RASSF1A and MLH1 [120, 121], also other putative anti-oncogenes such as OPCML may show promoter hypermethylation [122]. Other recurrently affected genes include the putative tumor suppressor genes ARHI, PEG3 and DLEC1, the pro-apoptotic genes LOT1, DAPK and PAR-4, the cell adhesion genes ICAM-1 and CDH1, and the genome stability gene PALB2 [120]. Interestingly, specific gene promoter methylation statuses have been found to be associated with different clinical OC features. A comparison of the methylation statuses of the SFRP, SOX1 and PAX1 gene promoters between patients with benign, borderline or malignant OCs revealed that the methylation was highest in malignant OCs [120, 123, 124]. On the other hand, it has been found that also gene promoter hypomethylation may be associated with OC [125]. Although limited examples are available, they include the MCJ, TRAG-3, Claudin-4 and IGF-2 genes [120, 126, 127].
Next to DNA methylation, also different histone modifications and alterations in its related enzymes have occasionally been observed in OC [121, 128]. Normally, histone modifications may contribute to ovarian functions, including estrogen and luteal phase activity. Like DNA methylation, anomalous histone modifications may play a crucial role in the silencing of anti-oncogenes [121].
For early OC detection noninvasive techniques may be used for the identification of specific biomarkers in body fluids. As such, several methylated DNA biomarkers have been explored in blood, plasma and peritoneal fluid of OC patients [129–132]. Despite the fact that methylation status evaluation of single genes usually lacks adequate specificity for OC detection, a panel of methylation biomarkers may reach the degree of precision that is required [132, 133]. Whereas DAPK methylation in peripheral blood DNA of OC patients has e.g. been observed in 67% of the cases compared to that in healthy individuals [134, 135], it has also been found that methylation assessment of a panel of anti-oncogenes (BRCA1, APC, p16ink4a and DAPK) can be applied with a high degree of specificity and sensitivity [129, 136–139].
Epigenetic biomarkers may also provide prognostic information. According to data reviewed by Seeber and Van Diest [120], single methylated genes with a possible prognostic value for OC (including HOXA11, FBXO32 and IGFBP-3) have been associated with a poor prognosis, disease progression and a high mortality rate. Despite the fact that some of these methylated genes may be of prognostic relevance individually, it is likely that also in this case panels of these genes will be more informative.
6.2 Micro-RNAs
Micro-RNAs (miRNAs) are small, non-coding RNAs of 18–25 nucleotides that can post-transcriptionally regulate gene expression [140, 141]. They are often located in fragile regions of the genome involved in chromosomal alterations in tumors [129, 130, 142, 143]. Recently, it has been found that (circulating) miRNA profiles may exhibit strong clinically relevant signatures in OCs [144]. Indeed, Zhang et al. [145] found 4 miRNAs to be up-regulated in epithelial OCs versus normal ovarian tissues, whereas 10 out of 25 miRNAs tested were found to be down-regulated. Furthermore, it was found that 25% of the down-regulated miRNAs clustered on three chromosomes (14, 19 and X) and that 8 miRNAs, which were found to be down-regulated in early-stage ovarian epithelial cancer, were located on chromosome 14. Interestingly, a chromosome Xq27.3 miRNA cluster was found to be associated with both early relapse in advanced stage OC patients and response to front-line therapy [146]. Several studies revealed OC miRNA over-expression signatures, including miR-21, miR-29a, miR-92, miR-93, miR-126, miR-205 and miR-30c1, whereas others revealed miRNA down-regulation signatures, including miR-99b, miR-127, miR-155, miR-181a, miR-342-3p and miR-450b-5p [147–152]. Notably, several miRNAs that have been found to be differentially expressed [144, 153, 154] still require validation using different controls and detection methods. Also, several miRNAs have been found at different levels in different body fluids of OC patients, such as miR-21, miR-23b, miR-29a, miR-141, miR-200a, miR-200b, miR-200c, miR-203, miR-205, miR-214 and miR-30-5p (Supplementary Fig. 5) [91, 155, 156]. Since several of these miRNAs have been associated with clinical outcome and response to therapy, and since they are remarkably stable in blood and other body fluids, they offer a great potential as OC biomarkers (for more details see [145, 155, 157]).
7 Conclusions and future perspectives
Due to its inter- and intra-heterogeneity, OC is a disease that is difficult to manage clinically. Recent years have shown an enormous burst in both fundamental and clinical research aimed at identifying clinically relevant OC biomarkers. Most conventional screening methods use a single biomarker (CA-125), alone or in combination with ultrasound examination. However, it has become increasingly clear that this strategy is not very effective, and recent studies have shown that multi-marker panels may hold promise in this respect. An increasing body of translational research is devoted to standardizing trial designs in order to avoid low specificities and sensitivities, which frequently hampers the use of newly discovered biomarkers. The recent approvals of the ROMA and OVA1 tests are examples of some of the most important advances that have recently been made using this strategy. Another pivotal example of progress that has been made is the recent approval of targeted therapy based on the synthetic lethality paradigm, i.e., PARP inhibition in BRCA mutation-positive (germline or somatic) OC cases. Also, rapid progress that has been made in next generation detection techniques and various large-scale discovery studies have led to the identification of promising candidates, including miRNAs and CTCs, for early OC detection and prognosis. Clearly, additional and large-scale trials are needed, especially considering the emergence of comprehensive next generation detection methods and the efficacious use of liquid biopsies. The following points may be considered for future trials: (i) the diagnostic and prognostic potential of CA-125 is US FDA approved but limited, compared to combined biomarkers, (ii) CA-125 is not suitable for OC screening in the general population and a search for more sensitive and informative biomarkers is needed, (iii) combinations of different biomarkers such as ROMA and OVA1 may allow the best possible early OC detection and increase its specificity and sensitivity, (iv) DNA methylation signatures, altered miRNA expression levels and CTCs are increasingly recognized as valuable diagnostic and prognostic OC biomarkers and are subject of intense research, (v) validation tests of all recently discovered biomarkers are urgently needed. Indeed, multi-marker panels accompanied by a meticulous determination of their sensitivity, specificity and validation will be critical for translational research and precision medicine, which are urgently needed.
8 Abbreviations
Akt, Serine-threonine protein kinase; APOA2, Apolipoprotein A-II; ARH1 (also named DIRAS3), aplysia RAS homology member 1; ATP, Adenosine triphosphate; b2M, beta-2 microglobulin; BCL-2, B-cell lymphoma 2; BRCA, Breast cancer (antigen); CA-125, Cancer antigen 125; CCNE, Cyclin E1; CD9, Cluster of differentiation 9; CDH, major cadherin family; CDK, Cyclin-dependent kinase; CEA, Carcinoembryonic antigen; CLDN3, Claudin 3; CRP, C-reactive protein; DAPK, Death-associated protein kinase; DcR3, Decoy receptor 3; DNA, Deoxyribonucleic acid; DLEC, (also named CLEC4C) C-type lectin domain family 4 member C; EGF, Epidermal growth factor; EMP, Embden-Meyerhof pathway; Ep-CAM, Epithelial cell adhesion molecule; FDA, Food and drug administration; FFPE, formalin-fixed and paraffin embedded; GLUT, Glucose transporter; GTP, Guanosine triphosphate; HDAC, Histone deacetylases; HE4, Human Epididymis Protein 4; HER, Human epidermal growth factor receptor; HIF, Hypoxia-inducible factor; hK6, Kallikrein-6; IGF-2, Insulin-like growth factor 2; Hmam, Human mammaglobin; ICAM, Intercellular adhesion molecule; IL-6, Interleukin 6; KIT, proto-oncogene receptor tyrosine kinase; KRT, Keratin; LAMP, Lysosome-associated membrane glycoprotein; LOT-1, Lipo-oxytocin-1; MAL, MyD88-adapter-like; M-CSF, Macrophage colony-stimulating factor; microRNA, micro Ribonucleic acid; MIF, Müllerian inhibiting factor; MMP, Matrix metalloproteinase; MUC, Mucin 1; NF-κB, Nuclear factor kappa-light-chain-enhancer of activated B cells; NF1, Neurofibromin 1; NPV, Negative predictive value; OPCML, Opioid-binding protein/cell adhesion molecule; OPN, Osteopontin; P21, known as cyclin-dependent kinase inhibitor 1; p53, Phosphoprotein 53; PALB, (also named TTR) transthyretin; PARP, Poly ADP ribose polymerase; PAX, Paired box; pRB, Retinoblastoma protein; PAI, Plasminogen activator inhibitor; PAR-4, Prostate apoptosis response-4; PKM2, Pyruvate kinase muscle isozyme; Plau-R or uPAR, Urokinase receptor; PPIC, Peptidyl-prolyl cis-trans isomerase C; PPV, Positive predictive value; PRL, Prolactin; PTEN, Phosphatase and tensin homolog; RAF, v-Raf murine sarcoma viral oncogene homolog B; RAS, Kirsten rat sarcoma; RASSF1A, Ras association domain-containing protein 1A; RB, Retinoblastoma protein; RAB, Ras binding; RT-PCR, Reverse transcription polymerase chain reaction; SAA, Serum amyloid A; SLC, Solute carrier; SLPI, Secretory leukocyte protease inhibitor; SPINT-1, Kunitz-type protease inhibitor 1; SELDI-TOF-MS, Surface-enhanced laser desorption/ionization time-of-flight mass spectroscopy; SNARE, Soluble N-ethylmaleimide-sensitive-factor Attachment protein Receptor; SOX, Sex determining region Y boxes; TF, Transferrin; TRAG, WD repeat domain 7; TTR, Transthyretin; TVS, Transvaginal sonography; UKCTOCS, UK Collaborative Trial of Ovarian Cancer Screening; V-CAM, Vascular cell adhesion protein; VEGF, Vascular endothelial growth factor; WFDC2, WAP four-disulfide core domain protein 2.
References
J. Ferlay, I. Soerjomataram, R. Dikshit, S. Eser, C. Mathers, M. Rebelo, D.M. Parkin, D. Forman, F. Bray, Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 136, 359–386 (2015)
R.L. Siegel, K.D. Miller, A. Jemal, Cancer statistics, 2016. CA Cancer J. Clin. 66, 7–30 (2016)
R. Sankaranarayanan, R. Swaminathan, K. Jayant, H. Brenner, An overview of cancer survival in Africa, Asia, the Caribbean and Central America: the case for investment in cancer health services. IARC Sci. Publ. 162, 257–291 (2011)
I. Cass, B.Y. Karlan, Ovarian cancer symptoms speak out – but what are they really saying? J. Natl. Cancer Inst. 102, 211–212 (2010)
K.A. Lowe, V.M. Chia, A. Taylor, C. O’Malleye, M. Kelsh, M. Mohamed, F.S. Mowat, B. Goff, An international assessment of ovarian cancer incidence and mortality. Gynecol. Oncol. 130, 107–114 (2013)
R. De Angelis, M. Sant, P.M. Coleman, S. Francisci, P. Baili, D. Pierannunzio, A. Trama, O. Visser, H. Brenner, E. Ardanaz, M. Bielska-Lasota, G. Engholm, A. Nennecke, S. Siesling, F. Berrino, R. Capocaccia, EUROCARE-5 working group, cancer survival in Europe 1999-2007 by country and age: results of Eurocare-5 – a population-based study. Lancet Oncol. 15, 23–34 (2014)
F. Dayyani, S. Uhlig, B. Colson, K. Simon, V. Rolny, D. Morgenstern, M. Schlumbrecht, Diagnostic performance of risk of ovarian malignancy algorithm against CA125 and HE4 in connection with ovarian cancer: a meta-analysis. Int. J. Gynecol. Cancer 26, 1586–1593 (2016)
J.L. Walker, C.B. Powell, L.M. Chen, J. Carter, V.L. Bae, L.P. Parker, M.E. Borowsky, R.K. Gibb, Society of Gynecologic Oncology recommendations for the prevention of ovarian cancer. Cancer 121, 2108–2120 (2015)
http://www.gopubmed.com/web/gopubmed/. Accessed 30 August 2016
S. Lambrechts, D. Smeets, M. Moisse, E.I. Braicu, A. Vanderstichele, H. Zhao, E. Van, E. Berns, J. Sehouli, R. Zeillinger, S. Darb-Esfahani, D. Cacsire, D. Lambrechts, I. Vergote, Genetic heterogeneity after first-line chemotherapy in high-grade serous ovarian cancer. Eur. J. Cancer 53, 51–64 (2016)
M. Petrillo, C. Nero, G. Amadio, D. Gallo, A. Fagotti, G. Scambia, Targeting the hallmarks of ovarian cancer: the big picture. Gynecol. Oncol. 142, 176–183 (2016)
C. Santos, R. Sanz-Pamplona, E. Nadal, J. Grasselli, S. Pernas, R. Dienstmann, V. Moreno, J. Tabernero, R. Salazar, Intrinsic cancer subtypes-next steps into personalized medicine. Cell. Oncol. 38, 3–16 (2015)
A. Zaal, W.J. Peyrot, P.M. Berns, M.E. van der Burg, J.H. Veerbeek, J.B. Trimbos, I. Cadron, P.J. van Diest, W.N. van Wieringen, O. Krijgsman, G.A. Meijer, J.M. Piek, P.J. Timmers, I. Vergote, R.H. Verheijen, B. Ylstra, R.P. Zweemer, EORTC GCG translational research group, genomic aberrations relate early and advanced stage ovarian cancer. Cell. Oncol. 35, 181–188 (2012)
M.E. Maradeo, P. Cairns, Translational application of epigenetic alterations: ovarian cancer as a model. FEBS Lett. 585, 2112–2120 (2011)
J.J. Wallbillich, B. Forde, L.J. Havrilesky, D.E. Cohn, A personalized paradigm in the treatment of platinum-resistant ovarian cancer–a cost utility analysis of genomic-based versus cytotoxic therapy. Gynecol. Oncol. 142, 144–149 (2016)
B.V. Chakravarthi, S. Nepal, S. Varambally, Genomic and epigenomic alterations in cancer. Am. J. Pathol. 186, 1724–1735 (2016)
R.J. Kurman, I.-M. Shih, The origin and pathogenesis of epithelial ovarian cancer-a proposed unifying theory. Am. J. Surg. Pathol. 34, 433–443 (2010)
N.N. Nik, R. Vang, I.M. Shih, R.J. Kurman, Origin and pathogenesis of pelvic (ovarian, tubal, and primary peritoneal) serous carcinoma. Annu. Rev. Pathol. 9, 27–45 (2014)
N. Colombo, M. Peiretti, A. Garbi, S. Carinelli, C. Marini, C. Sessa, Non-epithelial ovarian cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 23, 20–26 (2012)
W.D. Foulkes, M. Gore, W.G.M. Cluggage, Rare non-epithelial ovarian neoplasms: pathology, genetics and treatment. Gynecol. Oncol. 142, 190–198 (2016)
M. Köbel, S.E. Kalloger, D.G. Huntsman, J.L. Santos, K.D. Swenerton, J.D. Seidman, C.B. Gilks, Cheryl Brown ovarian cancer outcomes unit of the British Columbia Cancer Agency, Vancouver BC. Differences in tumor type in low-stage versus high-stage ovarian carcinomas. Int. J. Gynecol. Pathol. 29, 203–211 (2010)
J. Prat, New insights into ovarian cancer pathology. Ann. Oncol. 23 (Suppl 10), 111–117 (2012)
A. Halon, V. Materna, M. Drag-Zalesinska, E. Nowak-Markwitz, T. Gansukh, P. Donizy, M. Spaczynski, M. Zabel, M. Dietel, H. Lage, P. Surowiak, Estrogen receptor alpha expression in ovarian cancer predicts longer overall survival. Pathol. Oncol. Res. 17, 511–518 (2011)
R.J. Kurman, I.M. Shih, The dualistic model of ovarian carcinogenesis: revisited, revised, and expanded. Am. J. Pathol. 186, 733–747 (2016)
Cancer Genome Atlas Research Network, Integrated genomic analyses of ovarian carcinoma. Nature 474, 609–615 (2011)
A. Bamias, S. Pignata, E. Pujade-Lauraine, Angiogenesis: a promising therapeutic target for ovarian cancer. Crit. Rev. Oncol. Hematol. 84, 314–326 (2012)
N.G. Gavalas, M. Liontos, S.P. Trachana, T. Bagratuni, C. Arapinis, C. Liacos, M.A. Dimopoulos, A. Bamias, Angiogenesis-related pathways in the pathogenesis of ovarian cancer. Int. J. Mol. Sci. 14, 15885–15909 (2013)
J. Farley, W.E. Brady, V. Vathipadiekal, H.A. Lankes, R. Coleman, M.A. Morgan, R. Mannel, S.D. Yamada, D. Mutch, W.H. Rodgers, M. Birrer, D.M. Gershenson, Selumetinib in women with recurrent low-grade serous carcinoma of the ovary or peritoneum: an open-label, single-arm, phase 2 study. Lancet Oncol. 14, 134–140 (2013)
L.M. Landrum, J. Java, C.A. Mathews, G.S. Lanneau, L.J. Copeland, D.K. Armstrong, J.L. Walker, Prognostic factors for stage III epithelial ovarian cancer treated with intraperitoneal chemotherapy: a gynecologic oncology group study. Gynecol. Oncol. 130, 12–18 (2013)
I. Romero, R.C. Bast Jr., Minireview: human ovarian cancer: biology, current management, and paths to personalizing therapy. Endocrinology 153, 1593–1602 (2012)
Y. Yang-Hartwich, M.G. Soteras, Z.P. Lin, J. Holmberg, N. Sumi, V. Craveiro, M. Liang, E. Romanoff, J. Bingham, F. Garofalo, A. Alvero, G. Mor, p53 protein aggregation promotes platinum resistance in ovarian cancer. Oncogene 34, 3605–3616 (2015)
O. Caron, Oncogenetics in the management of ovarian cancer: state-of-the art. Gynecol. Obstet. Fertil. 43, 335–337 (2015)
A.A. Ahmed, D. Etemadmoghadam, J. Temple, A.G. Lynch, M. Riad, R. Sharma, C. Stewart, S. Fereday, C. Caldas, A. Defazio, D. Bowtell, J.D. Brenton, Driver mutations in TP53 are ubiquitous in high grade serous carcinoma of the ovary. J. Med. Surg. Pathol. 221, 49–56 (2010)
R. Wu, S.J. Baker, T.C. Hu, K.M. Norman, E.R. Fearon, K.R. Cho, Type I to type II ovarian carcinoma progression: mutant Trp53 or Pik3ca confers a more aggressive tumor phenotype in a mouse model of ovarian cancer. Am. J. Pathol. 182, 1391–1399 (2013)
J. Prat, Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Arch. 460, 237–249 (2012)
R.D.A. Weren, A.R. Mensenkamp, M. Simons, A. Eijkelenboom, A.S. Sie, H. Ouchene, M. van Asseldonk, E.B. Gomez-Garcia, M.J. Blok, J.A. de Hullu, M.R. Nelen, A. Hoischen, J. Bulten, B.B.J. Tops, N. Hoogerbrugge, M.J.L. Ligtenberg, Novel BRCA1 and BRCA2 tumor test as basis for treatment decisions and referral for genetic counselling of patients with ovarian carcinomas. Hum. Mutat. (2016). doi:10.1002/humu.23137
K.P. Pennington, T. Walsh, M.I. Harrell, M.K. Lee, C.C. Pennil, M.H. Rendi, A. Thornton, B.M. Norquist, S. Casadei, A.S. Nord, K.J. Agnew, C.C. Pritchard, S. Scroggins, R.L. Garcia, M. King, E.M. Swisher, Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas. Clin. Cancer Res. 20, 764–775 (2014)
J.R. McLaughlin, B. Rosen, J. Moody, T. Pal, I. Fan, P.A. Shaw, H.A. Risch, T.A. Sellers, P. Sun, S.A. Narod, Long-term ovarian cancer survival associated with mutation in BRCA1 or BRCA2. J. Natl. Cancer Inst. 105, 141–148 (2013)
S.B. Kaye, J. Lubinski, U. Matulonis, J.E. Ang, C. Gourley, B.Y. Karlan, A. Amnon, K.M. BellMcGuinn, L.M. Chen, M. Friedlander, T. Safra, I. Vergote, M. Wickens, E.S. Lowe, J. Carmichael, B. Kaufman, I.I. Phase, Open-label, randomized, multicenter study comparing the efficacy and safety of olaparib, a poly (ADP-ribose) polymerase inhibitor, and pegylated liposomal doxorubicin in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer. J. Clin. Oncol. 30, 372–379 (2012)
J.F. Liu, P.A. Konstantinopoulos, U.A. Matulonis, PARP inhibitors in ovarian cancer: current status and future promise. Gynecol. Oncol. 133, 362–369 (2014)
Y. Hirotsu, H. Nakagomi, I. Sakamoto, K. Amemiya, H. Mochizuki, M. Omata, Detection of BRCA1 and BRCA2 germline mutations in Japanese population using next-generation sequencing. Mol. Genet. Genomic. Med. 3, 121–129 (2015)
C.M. Strom, S. Rivera, C. Elzinga, T. Angeloni, S.H. Rosenthal, D. Goos-Root, M. Siaw, J. Platt, C. Braastadt, L. Cheng, D. Ross, W. Sun, Development and validation of a next-generation sequencing assay for BRCA1 and BRCA2 variants for the clinical laboratory. PLoS One 10, e0136419 (2015)
J.B. Hiatt, C.C. Pritchard, S.J. Salipante, B.J. O'Roak, J. Shendure, Single molecule molecular inversion probes for targeted, high-accuracy detection of low-frequency variation. Genome Res. 23, 843–854 (2013)
P. Bottoni, R. Scatena, The role of CA 125 as tumor marker: biochemical and clinical aspects. Adv. Exp. Med. Biol. 867, 229–244 (2015)
V.A. Moyer, Screening for ovarian cancer: US preventive services task force reaffirmation recommendation statement. Ann. Intern. Med. 157, 900–904 (2012)
S.S. Buys, E. Partridge, A. Black, C.C. Johnson, L. Lamerato, C. Isaacs, D.J. Reding, R.T. Greenlee, L.A. Yokochi, B. Kessel, E.D. Crawford, T.R. Church, G.L. Andriole, J.L. Weissfeld, M.N. Fouad, D. Chia, B. O'Brien, L.R. Ragard, J.D. Clapp, J.M. Rathmell, T.L. Riley, P. Hartge, P.F. Pinsky, C.S. Zhu, G. Izmirlian, B.S. Kramer, A.B. Miller, J.L. Xu, P.C. Prorok, J.K. Gohagan, C.D. Berg, PLCO Project Team, Effect of screening on ovarian cancer mortality: the prostate, lung, colorectal and ovarian (PLCO) cancer screening randomized controlled trial. JAMA 305, 2295–2303 (2011)
I.J. Jacobs, U. Menon, A. Ryan, A. Gentry-Maharaj, M. Burnell, J.K. Kalsi, N.N. Amso, S. Apostolidou, E. Benjamin, D. Cruickshank, D.N. Crump, S.K. Davies, A. Dawnay, S. Dobbs, G. Fletcher, J. Ford, K. Godfrey, R. Gunu, M. Habib, R. Hallett, J. Herod, H. Jenkins, C. Karpinskyj, S. Leeson, S.J. Lewis, W.R. Liston, A. Lopes, T. Mould, J. Murdoch, D. Oram, D.J. Rabideau, K. Reynolds, I. Scott, M.W. Seif, A. Sharma, N. Singh, J. Taylor, F. Warburton, M. Widschwendter, K. Williamson, R. Woolas, L. Fallowfield, A.J. McGuire, S. Campbell, M. Parmar, S.J. Skates, Ovarian cancer screening and mortality in the UK collaborative trial of ovarian cancer screening (UKCTOCS): a randomised controlled trial. Lancet 387, 945–956 (2016)
B.M. Nolen, A.E. Lokshin, Biomarker testing for ovarian cancer: clinical utility of multiplex assays. Mol. Diagn. Ther. 17, 139–146 (2013)
R.G. Moore, M.C. Miller, P. Disilvestro, L.M. Landrum, W. Gajewski, J.J. Ball, S.J. Skates, Evaluation of the diagnostic accuracy of the risk of ovarian malignancy algorithm in women with a pelvic mass. Obstet. Gynecol. 118, 280 (2011)
T. Van Gorp, I. Cadron, E. Despierre, A. Daemen, K. Leunen, F. Amant, D. Timmerman, B. De Moor, I. Vergote, HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the risk of ovarian malignancy algorithm. Brit. J. Cancer 104, 863–870 (2011)
Y. Xu, R. Zhong, J. He, R. Ding, H. Lin, Y. Deng, L. Zhou, X. Li, J. Jiang, Y. Bao, X. Luo, C. Duan, Modification of cut-off values for HE4, CA125 and the ROMA algorithm for early-stage epithelial ovarian cancer detection: results from 1021 cases in South China. Clin. Biochem. 49, 32–40 (2016)
M.R. Andersen, B.A. Goff, K.A. Lowe, N. Scholler, L. Bergan, C.W. Drescher, P. Paley, N. Urban, Use of a symptom index, CA125, and HE4 to predict ovarian cancer. J. Gynecol. Oncol. 116, 378–383 (2010)
T. Edgell, G. Martin-Roussety, G. Barker, D.J. Autelitano, D. Allen, P. Grant, G.E. Rice, Phase II biomarker trial of a multimarker diagnostic for ovarian cancer. J. Cancer Res. Clin. Oncol. 136, 1079–1088 (2010)
Z. Yurkovetsky, S. Skates, A. Lomakin, B. Nolen, T. Pulsipher, F. Modugno, J. Marks, A. Godwin, E. Gorelik, I. Jacobs, U. Menon, K. Lu, D. Badgwell, R.C. Bast Jr., A.E. Lokshin, Development of a multimarker assay for early detection of ovarian cancer. J. Clin. Oncol. 28, 2159–2166 (2010)
E. Kipps, D.S. Tan, S.B. Kaye, Meeting the challenge of ascites in ovarian cancer: new avenues for therapy and research. Nat. Rev. Cancer 13, 273–282 (2013)
K.L. Terry, H. Schock, R.T. Fortner, A. Hüsing, R.N. Fichorova, H.S. Yamamoto, A.F. Vitonis, T. Johnson, K. Overvad, A. Tjønneland, M.C. Boutron-Ruault, S. Mesrine, G. Severi, L. Dossus, S. Rinaldi, H. Boeing, V. Benetou, P. Lagiou, A. Trichopoulou, V. Krogh, E. Kuhn, S. Panico, H.B. Bueno-de-Mesquita, N.C. Onland-Moret, P.H. Peeters, I.T. Gram, E. Weiderpass, E.J. Duell, M.J. Sanchez, E. Ardanaz, N. Etxezarreta, C. Navarro, A. Idahl, E. Lundin, K. Jirström, J. Manjer, N.J. Wareham, K.T. Khaw, K. Smith Byrne, R.C. Travis, M.J. Gunter, M.A. Merritt, E. Riboli, D. Cramer, R. Kaaks, A prospective evaluation of early detection biomarkers for ovarian cancer in the European EPIC cohort. Clin. Cancer Res. 22, 1078–10432 (2016)
P. Vinken, S. Starckx, E. Barale-Thomas, A. Looszova, M. Sonee, N. Goeminne, L. Versmissen, K. Buyens, A. Lampo, Tissue Kim-1 and urinary clusterin as early indicators of cisplatin-induced acute kidney injury in rats. Toxicol. Pathol. 40, 1049–1062 (2012)
Z. Zhang, D.W. Chan, The road from discovery to clinical diagnostics: lessons learned from the first FDA-cleared in vitro diagnostic multivariate index assay of proteomic biomarkers. Cancer Epidem. Biomar. 19, 2995–2999 (2010)
R.W. Miller, A. Smith, C.P. DeSimone, L. Seamon, S. Goodrich, I. Podzielinski, L. Sokoll, J.R. van Nagell Jr., Z. Zhang, F.R. Ueland, Performance of the American College of Obstetricians and Gynecologists' ovarian tumor referral guidelines with a multivariate index assay. Obstet. Gynecol. 117, 1298–1306 (2011)
B.H. Shadfan, A.R. Simmons, G.W. Simmons, A. Ho, J. Wong, K.H. Lu, R.C. Bast, J.T. McDevitt, A multiplexable, microfluidic platform for the rapid quantitation of a biomarker panel for early ovarian cancer detection at the point-of-care. Cancer Prev. Res. 8, 37–48 (2015)
Y.W. Kim, S.M. Bae, H. Lim, Y.J. Kim, W.S. Ahn, Development of multiplexed bead-based immunoassays for the detection of early stage ovarian cancer using a combination of serum biomarkers. PLoS One 7, e44960 (2012)
S. Kato, L. Abarzua-Catalan, C. Trigo, A. Delpiano, C. Sanhueza, K. García, C. Ibañez, K. Hormazábal, D. Diaz, J. Brañes, E. Castellón, E. Bravo, G. Owen, M. Cuello, Leptin stimulates migration and invasion and maintains cancer stem-like properties in ovarian cancer cells: an explanation for poor outcomes in obese women. Oncotarget 6, 21100–21119 (2015)
N.M.A. White, T.F. Chow, S. Mejia-Guerrero, M. Diamandis, Y. Rofael, H. Faragalla, G.M. Yousef, Three dysregulated miRNAs control kallikrein 10 expression and cell proliferation in ovarian cancer. Brit. J. Cancer 102, 1244–1253 (2010)
M.A.H. El Sherbini, M.M. Sallam, E.A.K. Shaban, A.H. El-Shalakany, Diagnostic value of serum kallikrein-related peptidases 6 and 10 versus CA125 in ovarian cancer. Int. J. Gynecol. Cancer 21, 625–632 (2011)
S.C.L. Koh, C.Y. Huak, D. Lutan, J. Marpuang, S. Ketut, N.G. Budiana, N.K.H. Hoan, Combined panel of serum human tissue kallikreins and CA-125 for the detection of epithelial ovarian cancer. J. Gynecol. Oncol. 23, 175–181 (2012)
M.K. Siu, H.Y. Chan, D.S. Kong, E.S. Wong, O.G. Wong, H.Y. Ngan, K.F. Tam, H. Zhang, Z. Li, Q.K. Chan, S.W. Tsao, p21-activated kinase 4 regulates ovarian cancer cell proliferation, migration, and invasion and contributes to poor prognosis in patients. Proc. Natl. Acad. Sci. U. S. A. 107, 18622–18627 (2010)
X. Xia, Q. Ma, X. Li, T. Ji, P. Chen, H. Xu, S. Liao, Z. Han, R. Liu, T. Zhu, S. Wang, G. Xu, L. Meng, J. Zhou, D. Ma, Cytoplasmic p21 is a potential predictor for cisplatin sensitivity in ovarian cancer. BMC Cancer 11, 399 (2011)
K. Wurz, R.L. Garcia, B.A. Goff, P.S. Mitchell, J.H. Lee, M. Tewari, E.M. Swisher, MiR-221 and MiR-222 alterations in sporadic ovarian carcinoma: relationship to CDKN1B, CDKNIC and overall survival. Genes Chromosom. Cancer 49, 577–584 (2010)
L. Szabova, C. Yin, S. Bupp, T.M. Guerin, J.J. Schlomer, D.B. Householder, M.L. Baran, M. Yi, Y. Song, W. Sun, J.E. McDunn, Perturbation of Rb, p53, and Brca1 or Brca2 cooperate in inducing metastatic serous epithelial ovarian cancer. Cancer Res. 72, 4141–4153 (2012)
K. Avraam, K. Pavlakis, C. Papadimitriou, T. Vrekoussis, T. Panoskaltsis, I. Messini, E. Patsouris, The prognostic and predictive value of ERCC-1, p53, bcl-2 and bax in epithelial ovarian cancer. Eur. J. Gynaecol. Oncol. 32, 516–520 (2010)
F. Kong, C. Sun, Z. Wang, L. Han, D. Weng, Y. Lu, G. Chen, miR-125b confers resistance of ovarian cancer cells to cisplatin by targeting pro-apoptotic Bcl-2 antagonist killer 1. J. Huazhong Univ. Sci. Technolog. Med. Sci. 31, 543–549 (2011)
S. Lawicki, G.E. Będkowska, E. Gacuta-Szumarska, M. Szmitkowski, The plasma concentration of VEGF, HE4 and CA125 as a new biomarkers panel in different stages and sub-types of epithelial ovarian tumors. J. Ovarian Res. 6, 1 (2013)
M.R. Russell, M.J. Walker, A.J. Williamson, A. Gentry-Maharaj, A. Ryan, J. Kalsi, S. Skates, A. D'Amato, C. Dive, M. Pernemalm, P.C. Humphryes, Protein Z: a putative novel biomarker for early detection of ovarian cancer. Int. J. Cancer 138, 2984–2992 (2016)
K.M. Nieman, H.A. Kenny, C.V. Penicka, A. Ladanyi, R. Buell-Gutbrod, M.R. Zillhardt, I.L. Romero, M.S. Carey, G.B. Mills, G.S. Hotamisligil, S.D. Yamada, Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat. Med. 17, 1498–1503 (2011)
M. Zou, X. Zhang, C. Xu, IL6-induced metastasis modulators p-STAT3, MMP-2 and MMP-9 are targets of 3,3′-diindolylmethane in ovarian cancer cells. Cell. Oncol. 39, 47–57 (2016)
S.J. Bensinger, H.R. Christofk, New aspects of the Warburg effect in cancer cell biology, Semin. Cell. Dev. Biol. 23, 352–361 (2012)
M.V. Liberti, J.W. Locasale, The Warburg effect: how does it benefit cancer cells? Trends Biochem. Sci. 41, 211–218 (2016)
A.J. Levine, A.M. Puzio-Kuter, The control of the metabolic switch in cancers by oncogenes and tumor suppressor genes. Science 330, 1340–1344 (2010)
M.G. Vander Heiden, J.W. Locasale, K.D. Swanson, H. Sharfi, G.J. Heffron, D. Amador-Noguez, H.R. Christofk, G. Wagner, J.D. Rabinowitz, J.M. Asara, L.C. Cantley, Evidence for an alternative glycolytic pathway in rapidly proliferating cells. Science 329, 1492–1499 (2010)
M.Y. Fong, J. McDunn, S.S. Kakar, Identification of metabolites in the normal ovary and their transformation in primary and metastatic ovarian cancer. PLoS One 6, e19963 (2011)
A. Beach, H.G. Zhang, M.Z. Ratajczak, S.S. Kakar, Exosomes: an overview of biogenesis, composition and role in ovarian cancer. J. Ovarian Res. 7, 14 (2014)
A. Caivano, F. La Rocca, V. Simeon, M. Girasole, S. Dinarelli, I. Laurenzana, A. De Stradis, L. De Luca, S. Trino, A. Traficante, G. D’Arena, G. Mansueto, O. Villani, G. Pietrantuono, L. Laurenti, L. Del Vecchio, P. Musto, MicroRNA-155 in serum-derived extracellular vesicles as a potential biomarker for hematologic malignancies - a short report. Cell. Oncol. (2016) doi:10.1007/s13402-016-0300-x
L. Balaj, R. Lessard, L. Dai, Y.J. Cho, S.L. Pomeroy, X.O. Breakefield, J. Skog, Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nat. Commun. 2, 180 (2011)
A. Waldenstrom, N. Genneback, U. Hellman, G. Ronquist, Cardiomyocyte microvesicles contain DNA/RNA and convey biological messages to target cells. PLoS One 7, e34653 (2012)
C.A. Maguire, L. Balaj, S. Sivaraman, M.H. Crommentuijn, M. Ericsson, L. Mincheva-Nilsson, V. Baranov, D. Gianni, B.A. Tannous, M. Sena-Esteves, X.O. Breakefield, Microvesicle-associated AAV vector as a novel gene delivery system. Mol. Ther. 20, 960–971 (2012)
C. Escrevente, S. Keller, P. Altevogt, J. Costa, Interaction and uptake of exosomes by ovarian cancer cells. BMC Cancer 11, 108 (2011)
K.D.P. Dorayappan, J.J. Wallbillich, D.E. Cohn, K. Selvendiran, The biological significance and clinical applications of exosomes in ovarian cancer. Gynecol. Oncol. 142, 199–205 (2016)
A. Bobrie, M. Colombo, G. Raposo, C. Thery, Exosome secretion: molecular mechanisms and roles in immune responses. Traffic 12, 1659–1668 (2011)
I. Nazarenko, S. Rana, A. Baumann, J. McAlear, A. Hellwig, M. Trendelenburg, G. Lochnit, K.T. Preissner, M. Zöller, Cell surface tetraspanin Tspan8 contributes to molecular pathways of exosome-induced endothelial cell activation. Cancer Res. 70, 1668–1678 (2010)
R. Cappellesso, A. Tinazzi, T. Giurici, F. Simonato, V. Guzzardo, L. Ventura, M. Crescenzi, S. Chiarelli, A. Fassina, Programmed cell death 4 and microRNA 21 inverse expression is maintained in cells and exosomes from ovarian serous carcinoma effusions. Cancer Cytopathol. 122, 685–693 (2014)
O. Vaksman, C. Tropé, B. Davidson, R. Reich, Exosome-derived miRNAs and ovarian carcinoma progression. Carcinogenesis 35, 2113–2120 (2014)
A. Liga, A.D.B. Vliegenthart, W. Oosthuyzen, J.W. Dear, M. Kersaudy-Kerhoas, Exosome isolation: a microfluidic road-map. Lab Chip 15, 2388–2394 (2015)
D. Hanahan, R.A. Weinberg, Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011)
R. Paduch, The role of lymphangiogenesis and angiogenesis in tumor metastasis. Cell. Oncol. 39, 397–410 (2016)
L.H.A. Broersen, G.W. van Pelt, R.A.E.M. Tollenaar, W.E. Mesker, Clinical application of circulating tumor cells in breast cancer. Cell. Oncol. 37, 9–15 (2014)
C. Van Berckelaer, A.J. Brouwers, D.J.E. Peeters, W. Tjalma, X.B. Trinh, P.A. van Dam, Current and future role of circulating tumor cells in patients with epithelial ovarian cancer. Eur. J. Surg. Oncol. (2016). doi:10.1016/j.ejso.2016.05.010
C. Van Berckelaer, A.J. Brouwers, D.J. Peeters, W. Tjalma, X.B. Trinh, P.A. van Dam, Current and future role of circulating tumor cells in patients with epithelial ovarian cancer. Eur. J. Surg. Oncol. (2016). doi:10.1016/j.ejso.2016.05.010
E. Obermayr, D.C. Castillo-Tong, D. Pils, P. Speiser, I. Braicu, T. Van Gorp, S. Mahner, J. Sehouli, I. Vergote, R. Zeillinger, Molecular characterization of circulating tumor cells in patients with ovarian cancer improves their prognostic significance—a study of the OVCAD consortium. Gynecol. Oncol. 128, 15–21 (2013)
E. Obermayr, F. Sanchez-Cabo, M.K.M. Tea, C.F. Singer, M. Krainer, M.B. Fischer, J. Sehouli, A. Reinthaller, R. Horvat, G. Heinze, D. Tong, Assessment of a six gene panel for the molecular detection of circulating tumor cells in the blood of female cancer patients. BMC Cancer 10, 666 (2010)
K. Kolostova, M. Pinkas, A. Jakabova, E. Pospisilova, P. Svobodova, J. Spicka, M. Cegan, R. Matkowski, V. Bobek, Molecular characterization of circulating tumor cells in ovarian cancer. Am. J. Cancer Res. 6, 973–980 (2016)
K. Kolostova, R. Matkowski, M. Jędryka, K. Soter, M. Cegan, M. Pinkas, A. Jakabova, J. Pavlasek, J. Spicka, V. Bobek, The added value of circulating tumor cells examination in ovarian cancer staging. Am. J. Cancer Res. 5, 3363–3375 (2015)
R.R. Langley, I.J. Fidler, The seed and soil hypothesis revisited—the role of tumor-stroma interactions in metastasis to different organs. Int. J. Cancer 128, 2527–2535 (2011)
E. Kolwijck, J. Kos, N. Obermajer, P.N. Span, C.M. Thomas, L.F. Massuger, F.C. Sweep, The balance between extracellular cathepsins and cystatin C is of importance for ovarian cancer. Eur. J. Clin. Investig. 40, 591–599 (2010)
E. Lengyel, Ovarian cancer development and metastasis. Am. J. Pathol. 177, 1053–1064 (2010)
S.M. Khan, H.M. Funk, S. Thiolloy, T.L. Lotan, J. Hickson, G.S. Prins, C.W. Rinker-Schaeffer, In vitro metastatic colonization of human ovarian cancer cells to the omentum. Clin. Exp. Metastasis 27, 185–196 (2010)
M. Galea, G. Gauci, J. Calleja-Agius, P. Schembri-Wismayer, Peritoneal biomarkers in the early detection of ovarian cancer. Minerva. Ginecol. (2016, in press)
R. Drake, A.W. Vogl, A.W.M. Mitchel, Gray's anatomy for students (Churchill Livingstone/Elsevier, Philadelphia, 2010)
U. Kucukgoz Gulec, S. Paydas, A.B. Guzel, S. Buyukkurt, G. Seydaoglu, M.A. Vardar, Comparative analysis of CA 125, ferritin, beta-2 microglobulin, lactic dehydrogenase levels in serum and peritoneal fluid in patients with ovarian neoplasia. Med. Oncol. 29, 2937–2943 (2012)
V.M. Peterson, C.M. Castro, J. Chung, N.C. Miller, A.V. Ullal, M.D. Castano, R.T. Penson, H. Lee, M.J. Birrer, R. Weissleder, Ascites analysis by a microfluidic chip allows tumor-cell profiling. Proc. Natl. Acad. Sci. U. S. A. 110, E4978–E4986 (2013)
L.M. Amon, W. Law, M.P. Fitzgibbon, J.A. Gross, K. O'Briant, A. Peterson, C. Drescher, D.B. Martin, M. McIntosh, Integrative proteomic analysis of serum and peritoneal fluids helps identify proteins that are up-regulated in serum of women with ovarian cancer. PLoS One 5, e11137 (2010)
M.A. Dawson, T. Kouzarides, Cancer epigenetics: from mechanism to therapy. Cell 150, 12–27 (2012)
H. Easwaran, H.C. Tsai, S.B. Baylin, Cancer epigenetics: tumor heterogeneity, plasticity of stem-like states, and drug resistance. Mol. Cell 54, 716–727 (2014)
A. Ferraro, Altered primary chromatin structures and their implications in cancer development. Cell. Oncol. 39, 195–210 (2016)
E. Heard, R.A. Martienssen, Transgenerational epigenetic inheritance: myths and mechanisms. Cell 157, 95–109 (2014)
W.L. Tam, R.A. Weinberg, The epigenetics of epithelial-mesenchymal plasticity in cancer. Nat. Med. 19, 1438–1449 (2013)
J.S. You, P.A. Jones, Cancer genetics and epigenetics: two sides of the same coin? Cancer Cell 22, 9–20 (2012)
J. Tost, I.G. Gut, in Molecular Diagnostics (Third Edition), ed. by George P. Patrinos, Philip B. Danielson and Wilhelm J. Ansorge (Elsevier/Academic Press, Amsterdam, 2017), pp.103–139. doi:10.1016/B978-0-12-802971-8.00007-9
T.E. Liggett, A. Melnikov, Q. Yi, C. Replogle, W. Hu, J. Rotmensch, A. Kamat, A.K. Sood, V. Levenson, Distinctive DNA methylation patterns of cell-free plasma DNA in women with malignant ovarian tumors. Gynecol. Oncol. 120, 113–120 (2011)
C. Marsit, B. Christensen, Epigenetic Alterations in Oncogenesis, ed. by Adam R. Karpf (Springer, Berlin Heidelberg New York) (2013), pp. 233–252
L.M.S. Seeber, P.J. Van Diest. Epigenetics in Cancer Epigenetics: Methods and Protocols, ed. by G. D. Ramona and V. Mukesh (Springer, Berlin Heidelberg New York, 2012), pp 253–269.
J.A.T. Pepin, H. Cardenas, C. Moore, S. Condello, J. Guanglong, L. Yunlong, D. Matei, Epigenetic vulnerabilities in ovarian cancer. Cancer Res. 76, 4486–4486 (2016)
M. Longacre, N.A. Snyder, G. Housman, M. Leary, K. Lapinska, S. Heerboth, A. Willbanks, S. Sarkar, A comparative analysis of genetic and epigenetic events of breast and ovarian cancer related to tumorigenesis. Int. J. Mol. Sci. 17, 759 (2016)
H. Mirzaei, F. Yazdi, R. Salehi, H.R. Mirzaei, SiRNA and epigenetic aberrations in ovarian cancer. J. Cancer Res. Ther. 12, 498–508 (2016)
M. Kaur, A. Singh, K. Singh, S. Gupta, M. Sachan, Development of a multiplex MethyLight assay for the detection of DAPK1 and SOX1 methylation in epithelial ovarian cancer in a north Indian population. Genes Genet. Syst. (2016). doi:10.1266/ggs.15-00051
Y.P. Liao, L.Y. Chen, R.L. Huang, P.H. Su, M.W. Chan, C.C. Chang, M.H. Yu, P.H. Wang, M.S. Yen, K.P. Nephew, H.C. Lai, Hypomethylation signature of tumor-initiating cells predicts poor prognosis of ovarian cancer patients. Hum. Mol. Genet. 23, 1894–1906 (2014)
X. Lin, X. Shang, G. Manorek, S. Howell, Control of integrin expression and signaling by claudin-3 and claudin-4 in ovarian cancer. Cancer Res. 73, 211–211 (2013)
Y.F. Huang, W.F. Cheng, Y.P. Wu, Y.M. Cheng, K.F. Hsu, C.Y. Chou, Circulating IGF system and treatment outcome in epithelial ovarian cancer. Endocr. Relat. Cancer 21, 217–229 (2014)
D.J. Marsh, J.S. Shah, A.J. Cole, Histones and their modifications in ovarian cancer–drivers of disease and therapeutic targets. Front Oncol. 4, 144 (2014)
K.R. Davis, K.J. Flower, J.V. Borley, C.S.M. Wilhelm-Benartzi, Cell-free circulating tumor DNA methylation in high-grade serous ovarian cancer. Cancer Res. 76, 3154–3154 (2016)
S.N. Akers, K. Moysich, W. Zhang, G. Collamat Lai, A. Miller, S. Lele, K. Odunsi, A.R. Karpf, LINE1 and Alu repetitive element DNA methylation in tumors and white blood cells from epithelial ovarian cancer patients. Gynecol. Oncol. 132, 462–467 (2014)
A. DiazLuis, A. Bardelli, Liquid biopsies: genotyping circulating tumor DNA. J. Clin. Oncol. 32, 579–586 (2014)
H. Holger, M. Esteller, DNA methylation profiling in the clinic: applications and challenges. Nat. Rev. Genet. 13, 679–692 (2012)
C. Montavon, B.S. Gloss, K. Warton, C.A. Barton, A.L. Statham, J.P. Scurry, B. Tabor, T.V. Nguyen, W. Qu, G. Samimi, N.F. Hacker, Prognostic and diagnostic significance of DNA methylation patterns in high grade serous ovarian cancer. Gynecol. Oncol. 124, 582–588 (2012)
F. Yin, X. Liu, D. Li, Q. Wang, W. Zhang, L. Li, Tumor suppressor genes associated with drug resistance in ovarian cancer (review). Oncol. Rep. 30, 3–10 (2013)
B. Zhang, F.F. Cai, X.Y. Zhong, An overview of biomarkers for the ovarian cancer diagnosis. Eur. J. Obstet. Gynecol. 158, 119–123 (2011)
B.L. Valle, E. Kuhn, D. Sidransky, R. Guerrero-Preston, DNA promoter hypermethylation of genes as potential diagnostic and prognostic biomarkers for ovarian cancer. Cancer Res. 75, 2960–2960 (2015)
A. Dobrovic, T. Mikeska, K. Alsop, I. Candiloro, J. George, G. Mitchell, D. Bowtell, Constitutional BRCA1 methylation is a major predisposition factor for high-grade serous ovarian cancer. Cancer Res. 74, 290–290 (2014)
O.A. Al-Shabanah, M.M. Hafez, Z.K. Hassan, M.M. Sayed-Ahmed, W.N. Abozeed, A. Alsheikh, S.S. Al-Rejaie, Methylation of SFRPs and APC genes in ovarian cancer infected with high risk human papillomavirus. Asian Pac. J. Cancer Prev. 15, 2719–2725 (2013)
R. Bhagat, S. Chadaga, C.S. Premalata, G. Ramesh, C. Ramesh, V.R. Pallavi, L. Krishnamoorthy, Aberrant promoter methylation of the RASSF1A and APC genes in epithelial ovarian carcinoma development. Cell. Oncol. 35, 473–479 (2012)
V. Taucher, H. Mangge, J. Haybaeck, Non-coding RNAs in pancreatic cancer: challenges and opportunities for clinical application. Cell. Oncol. 39, 295–318 (2016)
M. Vitiello, A. Tuccoli, L. Poliseno, Long non-coding RNAs in cancer: implications for personalized therapy. Cell. Oncol. 38, 17–28 (2015)
M.D. Jansson, A.H. Lund, MicroRNA and cancer. Mol. Oncol. 6, 590–610 (2012)
M. Acunzo, G. Romano, D. Wernicke, C.M. Croce, MicroRNA and cancer–a brief overview. Adv. Biol. Regul. 57, 1–9 (2015)
L. Ayaz, F. Cayan, Ş. Balci, A. Görür, S. Akbayir, H. YıldırımYaroğlu, N. DoğruerUnal, L. Tamer, Circulating microRNA expression profiles in ovarian cancer. J. Obstet. Gynaecol. 4, 620–624 (2014)
S. Zhang, Z. Lu, A.K. Unruh, C. Ivan, K.A. Baggerly, G.A. Calin, Z. Li, R.C. Bast Jr., X.F. Le, Clinically relevant microRNAs in ovarian cancer. Mol. Cancer Res. 13, 393–401 (2015)
M. Bagnoli, L. De Cecco, A. Granata, R. Nicoletti, E. Marchesi, P. Alberti, B. Valeri, M. Libra, M. Barbareschi, F. Raspagliesi, D. Mezzanzanica, S. Canevari, Identification of a chrXq27.3 microRNA cluster associated with early relapse in advanced stage ovarian cancer patients. Oncotarget 2, 1265–1278 (2011)
S.F. Hausler, A. Keller, P.A. Chandran, K. Ziegler, K. Zipp, S. Heuer, M. Krockenberger, J.B. Engel, A. Hönig, M. Scheffler, J. Dietl, J. Wischhusen, Whole blood-derived miRNA profiles as potential new tools for ovarian cancer screening. Br. J. Cancer 103, 693–700 (2010)
Y.W. Chung, H.S. Bae, J.Y. Song, J.K. Lee, N.W. Lee, T. Kim, K.W. Lee, Detection of microRNA as novel biomarkers of epithelial ovarian cancer from the serum of ovarian cancer patients. Int. J. Gynecol. Cancer 23, 673–679 (2013)
H. Zheng, L. Zhang, Y. Zhao, D. Yang, F. Song, Y. Wen, Q. Hao, Z. Hu, W. Zhang, K. Chen, Plasma miRNAs as diagnostic and prognostic biomarkers for ovarian cancer. PLoS One 8, e77853 (2013)
I. Shapira, M. Oswald, J. Lovecchio, H. Khalili, A. Menzin, J. Whyte, L. Dos Santos, S. Liang, T. Bhuiya, M. Keogh, C. Mason, Circulating biomarkers for detection of ovarian cancer and predicting cancer outcomes. Br. J. Cancer 110, 976–983 (2014)
C.W. Kan, V.M. Howell, M.A. Hahn, D.J. Marsh, Genomic alterations as mediators of miRNA dysregulation in ovarian cancer. Genes Chromosom. Cancer 54, 1–19 (2015)
R. Langhe, L. Norris, F.A. Saadeh, G. Blackshields, R. Varley, A. Harrison, N. Gleeson, C. Spillane, C. Martin, D.M. O'Donnell, T. D'Arcy, J. O'Leary, S. O'Toole, A novel serum microRNA panel to discriminate benign from malignant ovarian disease. Cancer Lett. 356, 628–636 (2015)
S. Leskelä, L.J. Leandro-García, M. Mendiola, J. Barriuso, L. Inglada-Pérez, I. Muñoz, B. Martínez-Delgado, A. Redondo, J. de Santiago, M. Robledo, D. Hardisson, The miR-200 family controls β-tubulin III expression and is associated with paclitaxel-based treatment response and progression-free survival in ovarian cancer patients. Endocr. Relat. Cancer 18, 85–95 (2011)
S. Marchini, D. Cavalieri, R. Fruscio, E. Calura, D. Garavaglia, I.F. Nerini, C. Mangioni, G. Cattoretti, L. Clivio, L. Beltrame, D. Katsaros, Association between miR-200c and the survival of patients with stage I epithelial ovarian cancer: a retrospective study of two independent tumour tissue collections. Lancet Oncol. 12, 273–285 (2011)
K. Nakamura, K. Sawada, A. Yoshimura, Y. Kinose, E. Nakatsuka, T. Kimura, Clinical relevance of circulating cell-free microRNAs in ovarian cancer. Mol. Cancer 15, 48 (2016)
J. Zhou, G. Gong, H. Tan, F. Dai, X. Zhu, Y. Chen, J. Wang, Y. Liu, P. Chen, X. Wu, J. Wen, Urinary microRNA-30a-5p is a potential biomarker for ovarian serous adenocarcinoma. Oncol. Rep. 33, 2915–2923 (2015)
Y. Chen, L. Zhang, Q. Hao, Candidate microRNA biomarkers in human epithelial ovarian cancer: systematic review profiling studies and experimental validation. Cancer Cell Int. 13, 86 (2013)
Acknowledgements
We are grateful to Pr. Fourtassi Maryam, associate professor of physical medicine and rehabilitation at the Medical School of Oujda-Morocco, for her constant encouragement and to Pr. SELLAM Amar for revising the English of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Supplementary Figure 1
(DOCX 69 kb)
Supplementary Figure 5
(DOCX 65 kb)
Supplementary Table 1
(DOCX 12 kb)
Supplementary Table 2
(DOCX 16 kb)
Supplementary Table 3
(DOCX 13 kb)
Supplementary Table 4
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
El Bairi, K., Kandhro, A.H., Gouri, A. et al. Emerging diagnostic, prognostic and therapeutic biomarkers for ovarian cancer. Cell Oncol. 40, 105–118 (2017). https://doi.org/10.1007/s13402-016-0309-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-016-0309-1