Abstract
MicroRNAs (miRNAs) are a class of naturally occurring, small, non-coding RNAs which play important roles in diverse biological processes and are acting as key regulators of tumorigenesis and chemotherapy resistance. In this study, a downregulation of miR-125b was observed in breast cancer cell lines, suggesting miR-125b is a tumor suppressor in breast cancer. Moreover, the miR-125b levels were significantly decreased in doxorubicin-resistant MCF-7 (MCF-7/DR) cells compared with MCF-7 cells. Transfection of miR-125b significantly enhanced the cytotoxicity of doxorubicin to MCF-7/DR cells. However, the overexpression of miR-125b did not influence the doxorubicin accumulation but downregulated the myeloid cell leukemia-1 (Mcl-1) levels, which may be the mechanism of apoptosis induction caused by doxorubicin combining with miR-125b in MCF-7/DR cells. Furthermore, luciferase reporter assay proved that Mcl-1 is the target of miR-125b. Importantly, we found that the sensitization of miR-125b to doxorubicin cytotoxicity is caspase-dependent in MCF-7/DR cells, which can be inhibited by zVAD-fmk. Finally, we indicated that the treatment of miR-125b plus doxorubicin leads to loss of mitochondrial membrane potential (MMP) and mitochondria outer membrane permeability (MOMP), which were interacted with the activation of caspases. Thus, this study revealed the role of miR-125b in doxorubicin resistance and therapy, which may provide novel approaches for the treatment of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the second leading cause of cancer-related deaths in the USA and Europe [1], and its incidence is increasing in China [2]. Mortality from this disease remains high largely because of the resistance of cancer cells to chemotherapeutic agents, resulting in the subsequent metastasis of tumor cells [3]. Doxorubicin (DOX), an anthracycline drug, is widely used as a chemotherapeutic agent for the treatment breast cancer [4]. Despite the remarkable anti-cancer activity of DOX, the high dose of DOX causes serious side effects such as cardiotoxicity, and drug resistance is the main limitation of DOX clinical application [5]. Given this, combined treatment with other drugs is desirable to decrease the dose of DOX and overcome the DOX resistance.
MicroRNAs (miRNAs) belong to a large family of non-coding single-stranded RNAs, which are composed of 19–25 nucleotides in length. miRNAs are functional, which can regulate the stability and translation of target messenger RNAs (mRNAs) generally through binding to their 3′-untranslated regions (3′-UTRs) [6]. Studies have demonstrated that over 1000 miRNAs are known to be responsible for regulating more than 30 % of genes in the human genome [7]. Since then, miRNAs play important roles in various biological processes, such as development, cell proliferation, differentiation, and apoptosis [8, 9]. Dysregulation of miRNAs is essential for the development of diseases, including cancer [10].
Recent studies showed a correlation between miRNAs and chemoresistance in multiple cancers, such as lymphoma and ovarian cancer, and miR-136 as well as miR-363 showed a synergism in cisplatin treatment [11–13]. However, the molecular mechanisms underlying this process remains largely unknown. Herein, we have provided evidences showing the absence of miR-125b in breast cancer cell lines. Furthermore, we found that miR-125b levels are decreased further in DOX-resistant MCF-7 (MCF-7/DR) cells. Our data suggest that downregulated miR-125b promotes myeloid cell leukemia-1 (Mcl-1) expression, which is an anti-apoptotic B cell lymphoma 2 (Bcl-2) family member [14], and plays an important role in doxorubicin resistance and therapy in human breast cancer.
Materials and methods
Reagents and antibodies
Doxorubicin, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), zVAD-fmk, digitonin, Annexin V-FITC Apoptosis Detection Kit were obtained from Sigma-Aldrich (USA). 5,5′,6,6′-Tetrachloro-1,1′,3,3′-tetraethyl-imidacarbo-cyanine iodide (JC-1) was purchased from Molecular Probes (USA). Antibodies for anti-human Mcl-1, anti-human caspase-3, anti-human poly-ADP-ribose polymerase (PARP), anti-human cytochrome c, anti-human second mitochondria-derived activator of caspases/direct IAP binding protein with low pI (smac/DIABLO), and anti-human β-actin were purchased from Cell Signaling (USA). miR-125b mimics, miR-298 mimics, and negative control oligonucleotide (NCO) were purchased from GenePharma Company (China), and the sequences were as follows: miR-125b mimics: 5′-AGUGUUCAAUCCCAGAGUCCCU-3′; 2′-O-methyl modified miR-125b inhibitor: 5′-AGGGACUCUGGGAUUGAACACU-3′; NCO: 5′-GUUUCAGCCACUCCUACAGGUA-3′; miR-298 mimics: 5′-ACCCUCUUGGAGGGACGA AGACGA-3′.
Cell culture
Normal breast epithelial cell line MCF-10A and breast cancer cell lines including MDA-MB-435, T-47D, and MCF-7 were from the Institute of Biochemistry and Cell Biology, Chinese Academy of Sciences (Shanghai, China). MCF-10A cell line was cultured in Dulbecco’s Modified Eagle’s medium (DMEM)/F12 media (Gibco, USA) supplemented with 5 % horse serum (Gibco, USA), 10 μg/ml insulin (Gibco, USA), 100 ng/ml cholera toxin (Sigma-Aldrich, USA), 20 ng/ml EGF (Sigma-Aldrich, USA), and 0.5 ug/ml hydrocortisone (Sigma-Aldrich, USA) at 37 °C in humidified incubator with 5 % CO2. Breast cancer cell lines were cultured in DMEM basic medium (Gibco, USA) with 10 % fetal bovine serum (FBS, Gibco, USA) at 37 °C in a humidified 5 % CO2 incubator. MCF-7/DR cells were established by stepwise exposure of MCF-7 cells to increasing concentrations of doxorubicin. The cells were initially treated with DOX at 0.1 μg/ml for 2 months, and the DOX concentration was increased every 3 weeks by 0.02 μg/ml up to a final concentration of 0.3 μg/ml. The MCF-7/DR cells were exposed to DOX over a time period of 12 months. DOX was removed from the culture medium of MCF-7/DR cells for 2 weeks before the following experiments were performed.
Transfection
After cells were plated at approximately 80 % confluence, the firefly luciferase reporters (pMIR plasmid containing Mcl-1 3′-UTR, 2 μg/ml, Life Technologies, USA), Renilla luciferase pRL-TK vector (100 ng/ml, Promega, USA), eukaryotic expression vector (pEGFP-N1 plasmid containing Mcl-1 open reading frame, 2 μg/ml, Clontech, USA), and RNA oligonucleotides (NCO, miR-125b mimics, miR-125b inhibitors, or miR-298 mimics, 50 nM) were transiently transfected into the MCF-7 cells with Lipofectamine 2000 reagent (Invitrogen, USA) following the manufacturer’s instructions.
Quantitative real-time polymerase chain reaction
Total cellular RNA was isolated from cell lines using TRIzol (Invitrogen, USA) and the complementary DNA (cDNA) was synthesized using M-MLV Reverse Transcriptase (Invitrogen, USA) following the manufacturer’s instructions. Reverse transcription for miR-125b or endogenous control small nuclear U6 was performed by using total RNA with stem-loop RT [15] specific primers, and the sequences are as follows: miR-125b: 5′-CTCAACTGGTGTCGTGGAGTCGGCAATTCAGTT GAGAGGGACTC-3′; U6: 5′-AACGCTTCACGAATTTGCGT-3′. The expression of Mcl-1 mRNA was determined by quantitative real-time polymerase chain reaction (qPCR) using SYBR Green (TaKaRa, Japan) according to the manufacturer’s protocol, and the GAPDH mRNA was taken as internal control. The primer sequences are as follows: Mcl-1 F: 5′-GGCTAAACACTTGAAGACCA-3′, R: 5′-TGGAAGAACTCCACAAACC-3′; GAPDH F: 5′-CACTCCTCCACCTTTGA-3′, GAPDH R: 5′-CCACCACCCTGTTGCTG-3′. To calculate expression of miR-125b and Mcl-1, 2−△△CT method was used [16].
Plasmid construction and luciferase assay
The open reading frame of Mcl-1 gene without 3′-UTR was amplified by PCR with the cDNA as template and cloned into the pEGFP-N1 vector, and the recombinant plasmid was named pEGFP-Mcl-1. For the luciferase assay, a pMIR-REPORT™ miRNA Expression Reporter Vector consisting of the firefly luciferase coding sequence followed by the Mcl-1 3′-UTR (GenBank accession no. NM_001197320) was constructed. The mutations of pMIR-Mcl-1 plasmid was generated by mutating the complementary site for the seed region of miR-125b (UCUCAGGGA to UCUGUCGGA) by using site-directed mutagenesis kit (TaKaRa, Japan) based on the wild-type plasmid. MCF-7/DR cells were incubated in 48-well plates and cotransfected with miR-125b mimics plus pMIR-Mcl-1 plasmid together with Renilla luciferase pRL-TK vector. Cells were collected 24 h after transfection and analyzed using the dual-luciferase reporter system (Promega, USA) according to the manufacturer’s instructions. Firefly luciferase activity was normalized to the Renilla luciferase activity.
Doxorubicin accumulation detection
MCF-7/DR cells were transfected with miR-125b mimics, miR-298 mimics, or NCO for 24 h, and then the cells were treated with 2.5 μg/ml doxorubicin. After 2 h incubation, cells were washed three times with phosphate buffered solution (PBS), and the mean fluorescence intensity of intracellular DOX was determined using flow cytometry at an excitation wavelength of 488 nm and an emission wavelength of 575 nm.
Western blot analysis
Total cell lysates were quantified by BCA protein assay kit (Pierce, USA), and 50 μg of the protein from each sample was separated by 12.5 % SDS-PAGE and transferred onto PVDF membranes. The following primary antibodies were used for Western blot analysis: Mcl-1, caspase-3, PARP, cytochrome c, smac/DIABLO, and β-actin. In all cases, the membranes were incubated overnight at 4 °C with the primary antibodies in PBS with 5 % non-fat dry milk. After being washed with PBS, the membranes were then incubated with horseradish peroxidase-conjugated secondary antibody for 2 h. The proteins were then visualized with an enhanced chemiluminescence detection kit (Pierce, USA).
Measurement of cell viability by MTT
The viability of the MCF-7 or MCF-7/DR cells was measured with a MTT assay. Briefly, cells were seeded in triplicate in a 96-well plate at the density of 5 × 103 per well. After the cells were transfected with RNA oligonucleotides and treated with DOX for 48 h, MTT (20 ml, 5 mg/ml) was added to each well and incubated for another 4 h. Medium was then aspirated and 100 μl DMSO was added to each well. The absorbance values were determined at 570/655 nm using an automated ELISA plate reader. Results were represented as the ratio between the various treatments and the negative control.
Apoptosis assay
MCF-7/DR cells were transfected with RNA oligonucleotides for 24 h, and then the cells were treated with DOX for another 24 h. After treatment, cells were incubated with annexin V and propidium iodide (PI) for 15 min at room temperature according to the manufacturer’s instructions and analyzed using flow cytometry (Becton Dickinson, USA).
Mitochondrial membrane potential analysis
Mitochondrial membrane potential (MMP, ∆Ψm) was detected using JC-1 as an indicator. JC-1 accumulates in the mitochondria emitting red fluorescence when the ∆Ψm is high, but the fluorescence will disappear if the ∆Ψm collapses in cells [17]. MCF-7/DR cells were transfected with RNA oligonucleotides for 24 h, and then the cells were treated with DOX for another 24 h. After treatment, cells were harvested then washed with cold PBS and resuspended with PBS containing JC-1 at a final concentration of 5 μM. Following a 20-min incubation period at 37 °C in the dark, MMP was determined by FACS analysis.
Mitochondria isolation
After being treated with miR-125b plus DOX, the MCF-7/DR cells were resuspended in 60 μl PBS. Resuspended cells were then lysed with the same volume of digitonin lysis buffer (150 μg digitonin dissolved in 1 ml 500 mM sucrose solutions) for 10 min at room temperature followed by centrifugation (3000 rpm) for 5 min at 4 °C. The supernatant was centrifuged again (14,000 rpm) for 30 min at 4 °C. Then the resulting supernatant was transferred into another tube and used for Western blot as cytoplasmic fraction. The remaining cell pellet that contains the mitochondrial fraction was resuspended and lysed on ice followed by centrifugation for 20 min by 14,000 rpm. The supernatant was collected and performed for Western blot as mitochondrial fraction.
Statistical analysis
Data analysis was performed with SPSS 11.0 statistical software and expressed as mean ± SE. Differences were assessed by Student’s t test and ANOVA analysis. P < 0.05 was considered to be statistically significant.
Results
miR-125b is downregulated in human breast cancer cell lines and associated with doxorubicin resistance
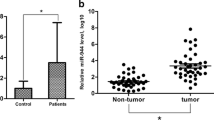
Since recent researches suggested that miR-125b plays an antitumor role in multiple types of cancers [18, 19], we studied the difference of miR-125b expression level between breast cancer cell lines and normal mammary epithelial cell line. As shown in Fig. 1a, the expression of miR-125b was significantly lower in all of the three breast cancer cell lines (MDA-MB-435, T-47D, and MCF-7) compared with MCF-10A which is the normal breast epithelial cell line, suggesting miR-125b functions as a tumor suppressor miRNA in breast cancer. More importantly, our date showed the miR-125b level was further downregulated after the cancer cells (MCF-7) were exposed to chemotherapeutics (doxorubicin) for a long time (more than 12 months) (Fig. 1b). These results suggest that miR-125b is a tumor suppressor and associated with doxorubicin resistance in breast cancer.
miR-125b is downregulated in human breast cancer cell lines and associated with doxorubicin resistance. a Analysis of miR-125b expression in human breast cancer cell lines and normal mammary epithelial cell line by RT-qPCR. *p < 0.05 vs. MCF-10A cells. b miR-125b expression was further downregulated in doxorubicin-resistant MCF-7/DR cells compared with its parental MCF-7 cells. *p < 0.05
miR-125b is essential for doxorubicin sensitivity to MCF-7 cells
To investigate the anti-cancer effect of DOX, different concentrations of DOX were added into culture medium, and cell viability as well as 50 % cell death (IC50) was detected by MTT assay after incubating for 48 h in MCF-7 cells and MCF-7/DR cells, respectively. As shown in Fig. 2a, doxorubicin markedly inhibited the viability of MCF-7 in a dose-dependent manner, whereas the MCF-7/DR cells were resistant to DOX for the IC50 between the parent and resistant cells, which was 23.83-fold. To investigate whether miR-125b modulated chemosensitivity in breast cancer, miR-125b mimics or miR-125b inhibitors were transfected into MCF-7/DR cells and MCF-7 cells, respectively. We showed that miR-125b mimics could significantly increase the miR-125b level in MCF-7/DR cells. In contrast, the miR-125b expression was downregulated after the transfection of miR-125b inhibitors in MCF-7 cells (Fig. 2b). We subsequently used the MTT assays to examine the effect of miR-125b on DOX treatment in MCF-7 and MCF-7/DR cells. As shown in Fig. 2c, knockdown of miR-125b by its inhibitors significantly decreased the sensitivity of MCF-7 cells to DOX. In contrast, enforced expression of miR-125b plus DOX led to a more significant decrease in the viability of MCF-7/DR cells, and the IC50 was lower compared to the group of DOX combined with NCO (Fig. 2d). All these data strongly suggest that the expression level of miR-125b is negatively correlated with DOX resistance in breast cancer cells.
miR-125b plays an important role in DOX resistance for MCF-7 cells. a MCF-7 and MCF-7/DR cells were treated with different concentrations of doxorubicin, and cell viability was determined by MTT assay. The IC50 was determined according to the survival curves. b miR-125b mimics increased the miR-125b level in MCF-7/DR cells, and miR-125b inhibitors decreased the miR-125b level in MCF-7 cells. The expression level of miR-125b was detected by RT-qPCR analysis after the cells were transfected with RNA oligonucleotides. c MTT assay was performed to evaluate the viability of MCF-7 cells after treatment of low doses of DOX plus miR-125b inhibitor or NCO (50 nM). IC50 was determined according to the survival curves. *p < 0.05. d MTT assay was performed to evaluate the viability of MCF-7/DR cells after treatment of high doses of DOX plus miR-125b mimics or NCO. IC50 was determined according to the survival curves. *p < 0.05
miR-125b increases the apoptosis of MCF-7/DR cells without influencing the doxorubicin accumulation
To explore the mechanisms why miR-125b reversed the DOX resistance in MCF-7/DR cells, we measured the DOX accumulation in MCF-7/DR cells transfected with miR-125b mimics. Since a previous study reported overexpression of miR-298 could increase the DOX accumulation via downregulating the P-glycoprotein, cells transfected with miR-298 was considered as the positive control to increase the accumulation of DOX [20]. Our results showed the transfection of miR-298 mimics significantly increased the uptake of DOX in MCF-7/DR cells as described. However, the DOX accumulation in MCF-7/DR cells was not influenced after miR-125b transfection, suggesting some other pathway is essential for the synergism of miR-125b and DOX (Fig. 3a). Therefore, in order to further investigate the mechanisms, we examined the effect of miR-125b as well as DOX on apoptosis. After analyzing cell apoptosis of MCF-7/DR treated with miR-125b, DOX, and their combination with annexin V assays using flow cytometry, we found that apoptotic rate for cells with combining treatment of DOX and miR-125b is much higher than that for the single-treatment cells (Fig. 3b). These data suggest that the overexpression of miR-125b could reverse the DOX resistance in MCF-7/DR cells through apoptosis pathways.
miR-125b increases the apoptosis of MCF-7/DR cells without influencing the doxorubicin accumulation. a MCF-7/DR cells were transfected with NCO, miR-125b, or miR-298. After 24 h incubation, cells were treated with 2.5 μg/ml doxorubicin for another 2 h, and the accumulation of DOX was evaluated by flow cytometry analysis. b MiR-125b or NCO was transfected into MCF-7/DR cells for 24 h, and then the cells were treated with/without 2.5 μg/ml DOX for another 24 h. The percentage of apoptosis was evaluated by flow cytometry analysis
miR-125b modulates the expression of Mcl-1
To determine how miR-125b promotes cancer cell apoptosis, we used public database TargetScan and found Mcl-1 maybe the putative target of miR-125b (Fig. 4a). The preceding results showed us that the miR-125b level in MCF-7/DR cells was lower than its parental MCF-7 cells (Fig. 1b). Therefore, the Mcl-1 expression level should be higher in MCF-7/DR cells rather than MCF-7 cells if miR-125b modulates the expression of Mcl-1. Consistent with the inference, the expression of Mcl-1 was downregulated in MCF-7/DR cells at both mRNA level and protein level (Fig. 4b). Moreover, decreased Mcl-1 expression level was observed by qPCR and Western blot analysis in MCF-7/DR cells transfected with miR-125b compared with control cells (Fig. 4c). To validate whether Mcl-1 is an actual target of miR-125b, the Mcl-1 3′-UTR containing either a wild-type or mutant miR-125b binding sites was cloned into pMIR reporter plasmid. The relative luciferase activity of the wild-type reporter in MCF-7/DR cells was significantly suppressed by miR-125b. In contrast, the luciferase activity of the mutant reporter in the presence of miR-125b was almost unaffected (Fig. 4d), indicating that miR-125b may suppress the expression of Mcl-1 through the binding sequence at its 3′-UTR. Furthermore, to study the function of Mcl-1 which was downregulated by exogenous miR-125b in MCF-7/DR cells with DOX treatment, we transfected the MCF-7/DR cells with pEGFP-Mcl-1 plasmid to examine whether enforced expression of Mcl-1 could “rescue” the fate of MCF-7/DR cells treated with DOX plus miR-125b. We found that the enforced expression of Mcl-1 significantly decreased the apoptotic rate of MCF-7/DR cells with combining treatment of DOX plus miR-125b (Fig. 4e). Taken together, these results suggest that the expression of Mcl-1 was negatively regulated by miR-125b, and Mcl-1 gene is the target of miR-125b to reverse the DOX resistance in breast cancer cells.
miR-125b modulates the expression of Mcl-1. a Putative miR-125b binding sequence in the 3′-UTR of Mcl-1 mRNA. b The expression of Mcl-1 was detected by qPCR and Western blot analysis in MCF-7/DR cells and MCF-7 cells. c Mcl-1 expression level was determined after miR-125b transfection by qPCR analysis and Western blot analysis in MCF-7/DR cells. d MCF-7/DR cells were cotransfected with pMIR reporter, pRL-TK vector, and miR-125b, incubating for 24 h. Firefly luciferase activity was measured and normalized to Renilla luciferase. e MCF-7/DR cells were cotransfected with pEGFP-Mcl-1 vector (or pEGFP-N1 control) and miR-125b for 24 h; 2.5 μg/ml DOX was then added into the culture medium incubating for another 24 h; apoptotic rate of MCF-7/DR cells was evaluated by flow cytometry analysis
The sensitization of miR-125b to doxorubicin-inducing cell death is caspase-dependent in MCF-7/DR cells
Since our data showed the overexpression of miR-125b reversed the DOX resistance in MCF-7/DR cells through inducing apoptosis, we investigated whether the synergistic effect of miR-125b on DOX-inducing cell death is relevant with caspase pathway. As shown in Fig. 5a, treatment with DOX plus miR-125b led to an obvious cleavage of caspase-3 and its substrate poly-ADP-ribose polymerase (PARP) compared with the single-treatment group, which could be impaired by cell-permeable pan caspase inhibitor zVAD-fmk [21]. More importantly, cell death induced by DOX combining with miR-125b treatment was inhibited in the presence of zVAD-fmk, suggesting the sensitization of miR-125b to DOX-mediated cell death is caspase-dependent in DOX-resistant breast cancer cells (Fig. 5b). Our preceding results showed Mcl-1 gene is the target of miR-125b to reverse the DOX resistance in MCF-7/DR, so we studied the effect of exogenous Mcl-1 on the activation of caspase-3 induced by the treatment of DOX combing with miR-125b. Consistent with our conclusion, transfection of pEGFP-Mcl-1 significantly decreased the activation of caspase-3 induced by DOX plus miR-125b (Fig. 5c).
The sensitization of miR-125b to doxorubicin inducing cell death is caspase-dependent in MCF-7/DR cells. a MCF-7/DR cells were treated with DOX (2.5 μg/ml) plus miR-125b or NCO (50 nM) for 24 h in the absence or presence of zVAD-fmk (10 μM), and Western blot analysis was performed to measure the cleavage of caspase-3 and its substrate PARP. b MCF-7/DR cells were treated with different concentrations of DOX plus miR-125b (50 nm) for 48 h in the absence or presence of zVAD-fmk (10 μM), and the cell viability was determined by MTT assay. c MCF-7/DR cells were cotransfected with pEGFP-Mcl-1 vector (or pEGFP-N1 control) and miR-125b for 24 h; 2.5 μg/ml DOX was then added into the culture medium incubating for another 24 h; caspase-3 activation of MCF-7/DR cells was evaluated by Western blot analysis
Downregulation of Mcl-1 by miR-125b enhanced the effect of doxorubicin to result in loss of MMP and release of mitochondrial proteins
Destroying the mitochondria is one of the important mechanisms for DOX to kill the cancer cells [22]. Mcl-1 suppression allows disintegration of mitochondria by loss of MMP and mitochondria outer membrane permeability (MOMP), resulting in the release of proteins such as cytochrome c and smac/DIABLO mitochondria that induces caspase-dependent cell death [23–25]. To further dissect the impact of miR-125b and DOX in MCF-7/DR cells, MMP was analyzed. As shown in Fig. 6a, miR-125b alone treatment did not influence the MMP of DOX-resistant MCF-7 cells, but significantly promoted the DOX to destroy their mitochondria. Consistent with our conclusion, exogenous Mcl-1 significantly inhibited the sensitization of miR-125b to doxorubicin-inducing ∆Ψm loss. As miR-125b plus DOX induced caspase-dependent cell death, and activation of caspases may escalate mitochondrial dysfunction [26], we found miR-125b plus DOX-mediated loss of MMP was partially blocked by zVAD-fmk, indicating that the loss of MMP is caspase-dependent. As the opening of mitochondrial permeability transition pore results in loss of MMP [27], we found the mitochondria-derived apoptogenic proteins, in particular cytochrome c and smac/DIABLO, were released into the cytoplasm when the MCF-7/DR cells were treated with miR-125b plus DOX. Importantly, the release of mitochondrial proteins were inhibited by exogenous Mcl-1 transfection or zVAD-fmk addition, suggesting Mcl-1 suppression promoted DOX-induced caspase-dependent release of mitochondria-derived proteins in DOX-resistant breast cancer cells.
miR-125b combined with doxorubicin caused loss of MMP and MOMP in MCF-7/DR cells. a MCF-7/DR cells were treated with DOX (2.5 μg/ml) plus miR-125b or NCO (50 nM) for 24 h in the absence or presence of zVAD-fmk (10 μM), and then the mitochondrial membrane potential was analyzed by JC-1 assay. b After MCF-7/DR cells were treated as describe above, cytochrome c and smac/DIABLO levels in the mitochondria and cytoplasm were measured by Western blot analysis
Discussion
Emerging evidence indicates that miR-125b acts as a tumor suppressor in multiple cancer types. Guan et al. demonstrated that down-expression of miR-125b was significantly correlated with proliferation and metastasis by targeting the proto-oncogene B cell CLL/lymphoma 3 (BCL3) in ovarian cancer [28]. Huang et al. showed that overexpression of miR-125b inhibited the cell cycle in bladder cancer cells [29]. Consistent with potential tumor suppressor gene function, miR-125b dysregulation is involved in breast cancer patients’ tumors [30]. In this paper, we conformed miR-125b is a tumor suppressor in breast cancer.
Previous researches showed that some miRNAs could modulate the acquired resistance of cancer cells to chemotherapeutic drugs, including breast cancer [31, 32]. However, the molecular mechanisms of sensitization to chemotherapy caused by miRNAs were still unclear. Our data suggested that miR-125b is associated with drug resistance in breast cancer, and then we reconfirmed that overexpression of miR-125b by its mimics can effectively increase the sensitivity of MCF-7/DR cells to DOX-induced cell death. Interestingly, DOX cytotoxicity to primary MCF-7 cells was significantly reduced when the function of miR-125b was inhibited in MCF-7 cells. These results directly support our conclusion that miR-125b plays a key role for reversing DOX resistance in breast cancer cells.
Since aberrant regulation of apoptosis plays a key role in cancer formation and development, tumor cells must evolve a variety of strategies to escape from apoptosis so that they can survive in the harsh tumor microenvironment, where nutrient deprivation and hypoxia are common [33]. More importantly, the strategy of circumventing apoptosis is well used by tumor cells to develop the acquired chemotherapy resistance [34]. The Bcl-2 family, which consists of both pro- and anti-apoptotic proteins, decides whether a cell continues to live or undergoes death through the apoptotic pathway. Commonly, tumor cells increase the expression of anti-apoptotic regulators (Bcl-2, Bcl-xL, Mcl-1, and Bcl-w) for surviving [35]. In this study, we found Mcl-1 was significantly upregulated in the doxorubicin-resistant cells, which is consistent with other published studies [36, 37]. More importantly, our data confirmed the sensitization of miR-125b is dependent on the downregulation of Mcl-1.
We further investigated whether the synergistic effect of miR-125b on doxorubicin-inducing cell death is caspase-3-dependent, whose cleavage is the common step in both extrinsic and apoptosis pathways [38]. Our results demonstrated the overexpression of miR-125b enhanced the activation of caspase-3 and its substrate induced by doxorubicin, which could be inhibited by zVAD-fmk. More importantly, overexpressed Mcl-1 significantly decreased the caspase-3 activation, further illustrating the mechanism of miR-125b on drug resistance reversal.
Study deeply, we found downregulation of Mcl-1 caused by miR-125 promoted doxorubicin-resistant MCF-7 cell response to doxorubicin therapy by MOMP-mediated cell death induction, activation of caspase-3, and caspase-dependent release of mitochondria-derived proteins. Based on these observations, we explained mitochondrial apoptosis is essential in doxorubicin therapy [39]. However, overexpression of Mcl-1 protects the mitochondria in doxorubicin-resistant breast cancer cells from the damage by doxorubicin, making MCF-7/DR cells survive. MiR-125b transfection modulated the Mcl-1 level in MCF-7/DR cells, making their mitochondria lost the protection of Mcl-1 from the doxorubicin treatment. Responding to doxorubicin, the MMP decreased and the mitochondrial permeability transition pore became open. And then, the mitochondria-derived apoptogenic proteins, such as cytochrome c and smac/DIABLO, released into the cytoplasm, activating caspase-dependent apoptosis. Interestingly, we found zVAD-fmk partially inhibited the loss of MMP, indicating the activation of caspases may escalate mitochondrial dysfunction [26]. These findings show the indispensable function of Mcl-1 as resistance factor that protects from intrinsic pathway-induced cell death in MCF-7/DR cells.
In summary, we investigated the altered expression pattern of miR-125b in breast cancer and its synergistic effect on DOX-inducing cell death by promoting cell apoptosis through the downregulation of Mcl-1 expression, resulting in mitochondria damage and caspase-3 activation. Our data demonstrated an important role for miR-125b in DOX-based therapy, and the miR-125b-mitochondria-caspase-3 pathway may provide a novel therapeutic strategy for treatment of breast cancer.
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
He M, Guo Q, Hu G. Reversed urban-rural differences in breast cancer mortality (China, 2002–2008). Breast Cancer Res Treat. 2011;126:231–4.
Stockler M, Wilcken NR, Ghersi D, Simes RJ. Systematic reviews of chemotherapy and endocrine therapy in metastatic breast cancer. Cancer Treat Rev. 2000;26:151–68.
Xu F, Wang F, Yang T, Sheng Y, Zhong T, Chen Y. Differential drug resistance acquisition to doxorubicin and paclitaxel in breast cancer cells. Cancer Cell Int. 2014;14:538.
Shuhendler AJ, Prasad P, Zhang RX, Amini MA, Sun M, Liu PP, et al. Synergistic nanoparticulate drug combination overcomes multidrug resistance, increases efficacy, and reduces cardiotoxicity in a nonimmunocompromised breast tumor model. Mol Pharm. 2014;11:2659–74.
Inui M, Martello G, Piccolo S. MicroRNA control of signal transduction. Nat Rev Mol Cell Biol. 2010;11:252–63.
He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5:522–31.
Zhang L, Ge Y, Fuchs E. MiR-125b can enhance skin tumor initiation and promote malignant progression by repressing differentiation and prolonging cell survival. Genes Dev. 2014;28:2532–46.
Wang S, Li K. MicroRNA-96 regulates RGC-5 cell growth through caspase-dependent apoptosis. Int J Clin Exp Med. 2014;7:3694–702.
Lee YS, Dutta A. MicroRNAs in cancer. Annu Rev Pathol. 2009;4:199–227.
Zheng RL, Jiang YJ, Wang X. Role of microRNAs on therapy resistance in non-Hodgkin’s lymphoma. Int J Clin Exp Med. 2014;7:3818–32.
Zhao H, Liu S, Wang G, Wu X, Ding Y, Guo G, et al. Expression of miR-136 is associated with the primary cisplatin resistance of human epithelial ovarian cancer. Oncol Rep. 2015;33:591–8.
Zhang R, Li Y, Dong X, Peng L, Nie X. MiR-363 sensitizes cisplatin-induced apoptosis targeting in Mcl-1 in breast cancer. Med Oncol. 2014;31:347.
Woo SM, Min KJ, Seo BR, Nam JO, Choi KS, Yoo YH, et al. Cafestol overcomes ABT-737 resistance in Mcl-1-overexpressed renal carcinoma Caki cells through downregulation of Mcl-1 expression and upregulation of Bim expression. Cell Death Dis. 2014;5, e1514.
Chen C, Ridzon DA, Lee DH, et al. Real-time quantification of microRNAs by stem-loop RT-PCR. Nucleic Acids Res. 2005;33, e179.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-delta delta C(T)) method. Methods. 2001;25:402–8.
Prathapan A, Vineetha VP, Raghu KG. Protective effect of Boerhaavia diffusa L. against mitochondrial dysfunction in angiotensin II induced hypertrophy in H9c2 cardiomyoblast cells. PLoS One. 2014;9, e96220.
Tsang FH, Au V, Lu WJ, Shek FH, Liu AM, Luk JM, et al. Prognostic marker microRNA-125b inhibits tumorigenic properties of hepatocellular carcinoma cells via suppressing tumorigenic molecule eIF5A2. Dig Dis Sci. 2014;59:2477–87.
Li J, You T, Jing J. MiR-125b inhibits cell biological progression of Ewing’s sarcoma by suppressing the PI3K/Akt signalling pathway. Cell Prolif. 2014;47:152–60.
Bao L, Hazari S, Mehra S, Kaushal D, Moroz K, Dash S. Increased expression of P-glycoprotein and doxorubicin chemoresistance of metastatic breast cancer is regulated by miR-298. Am J Pathol. 2012;180:2490–503.
Amaral C, Borges M, Teixeira N, et al. Apoptosis and autophagy in breast cancer cells following exemestane treatment. PLoS One. 2012;7, e42398.
Friedhuber AM, Chandolu V, Manchun S, Donkor O, Sriamornsak P, Dass CR. Nucleotropic doxorubicin nanoparticles decrease cancer cell viability, destroy mitochondria, induce autophagy and enhance tumour necrosis. J Pharm Pharmacol. 2015;67:68–77.
Pareja F, Macleod D, Shu C, Crary JF, Canoll PD, Ross AH, et al. PI3K and Bcl-2 inhibition primes glioblastoma cells to apoptosis through downregulation of Mcl-1 and Phospho-BAD. Mol Cancer Res. 2014;12:987–1001.
Fulda S, Galluzzi L, Kroemer G. Targeting mitochondria for cancer therapy. Nat Rev Drug Discov. 2010;9:447–64.
Galluzzi L, Vitale I, Abrams JM, Alnemri ES, Baehrecke EH, Blagosklonny MV, et al. Molecular definitions of cell death subroutines: recommendations of the Nomenclature Committee on Cell Death 2012. Cell Death Differ. 2012;19:107–20.
Tait SW, Green DR. Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol. 2010;11:621–32.
Bonora M, Pinton P. The mitochondrial permeability transition pore and cancer: molecular mechanisms involved in cell death. Front Oncol. 2014;4:302.
Guan Y, Yao H, Zheng Z, Qiu G, Sun K. MiR-125b targets BCL3 and suppresses ovarian cancer proliferation. Int J Cancer. 2011;128:2274–83.
Huang L, Luo J, Cai Q, Pan Q, Zeng H, Guo Z, et al. MicroRNA-125b suppresses the development of bladder cancer by targeting E2F3. Int J Cancer. 2011;128:1758–69.
Feliciano A, Castellvi J, Artero-Castro A, Leal JA, Romagosa C, Hernández-Losa J, et al. miR-125b acts as a tumor suppressor in breast tumorigenesis via its novel direct targets ENPEP, CK2-α, CCNJ, and MEGF9. PLoS One. 2013;8:e76247.
Liu R, Liu X, Zheng Y, Gu J, Xiong S, Jiang P, et al. MicroRNA-7 sensitizes non-small cell lung cancer cells to paclitaxel. Oncol Lett. 2014;8:2193–200.
Boyerinas B, Park SM, Murmann AE, Gwin K, Montag AG, Zillhardt M, et al. Let-7 modulates acquired resistance of ovarian cancer to Taxanes via IMP-1-mediated stabilization of multidrug resistance 1. Int J Cancer. 2012;130:1787–97.
Gong J, Zhang JP, Li B, Zeng C, You K, Chen MX, et al. MicroRNA-125b promotes apoptosis by regulating the expression of Mcl-1, Bcl-w and IL-6R. Oncogene. 2013;32:3071–9.
Yang P, Tuo L, Wu Q, Cao X. Licochalcone-A sensitizes human esophageal carcinoma cells to TRAIL-mediated apoptosis by proteasomal degradation of XIAP. Hepatogastroenterology. 2014;61:1229–34.
Zhao J, Li X, Zou M, He J, Han Y, Wu D, et al. miR-135a inhibition protects A549 cells from LPS-induced apoptosis by targeting Bcl-2. Biochem Biophys Res Commun. 2014;452:951–7.
Rao YM, Shi HR, Ji M, Chen CH. MiR-106a targets Mcl-1 to suppress cisplatin resistance of ovarian cancer A2780 cells. J Huazhong Univ Sci Technol Med Sci. 2013;33:567–72.
Sugio A, Iwasaki M, Habata S, Mariya T, Suzuki M, Osogami H, et al. BAG3 upregulates Mcl-1 through downregulation of miR-29b to induce anticancer drug resistance in ovarian cancer. Gynecol Oncol. 2014;134:615–23.
Geserick P, Wang J, Feoktistova M, Leverkus M. The ratio of Mcl-1 and Noxa determines ABT737 resistance in squamous cell carcinoma of the skin. Cell Death Dis. 2014;5, e1412.
Ortiz-Lazareno PC, Bravo-Cuellar A, Lerma-Díaz JM, Jave-Suárez LF, Aguilar-Lemarroy A, Domínguez-Rodríguez JR, et al. Sensitization of U937 leukemia cells to doxorubicin by the MG132 proteasome inhibitor induces an increase in apoptosis by suppressing NF-kappa B and mitochondrial membrane potential loss. Cancer Cell Int. 2014;14:13.
Acknowledgments
This work was supported by the Natural Science Foundation of Zhejiang Province (No. LY12H16008).
Conflicts of interest
None
Authors’ contributions
XG designed the study. XX, YH, and YF wrote the manuscript. XX, YH, and LX performed the immunohistochemistry and the related statistical analysis. XX, JT, HZ, RH, and SZ carried out the cell culture and transfection, Western blot, RT-PCR, and flow cytometry. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xie, X., Hu, Y., Xu, L. et al. The role of miR-125b-mitochondria-caspase-3 pathway in doxorubicin resistance and therapy in human breast cancer. Tumor Biol. 36, 7185–7194 (2015). https://doi.org/10.1007/s13277-015-3438-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3438-7