Abstract
Myeloid cell leukemia-1 (Mcl-1) is an anti-apoptotic Bcl-2 family member that is often overexpressed in breast tumors, and has been reported to have an important role in regulating drug resistance in various types of cancer including breast cancer. However, the mechanisms underlying the aberrant expression of Mcl-1 are still unclear. In this study, we used bioinformatics, cellular, and molecular methods to predict and prove that miR-363 directly targeted Mcl-1 3′-UTR (3′-untranslated regions) and caused downregulation of Mcl-1 in breast cancer. Resistance to chemotherapy is a major barrier for the effective treatment for advanced breast cancer, but our study indicated that miR-363 reversed the resistance of the breast cancer cell line MDA-MB-231 to the chemotherapeutic agent cisplatin (CDDP). In addition, transfection of breast cancer cells with Mcl-1 expression plasmid abolished the sensitization effect of miR-363 to cisplatin-inducing cytotoxicity. In summary, our study showed that miR-363 was a negative regulator of Mcl-1 expression, and the combination of miR-363 and cisplatin may be a novel approach in the treatment for breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is one of the leading causes of cancer deaths and the most common cancer among women worldwide [1]. It is a heterogeneous disease due to the genetic backgrounds of the patients, and environmental factors play an important role in BC pathogenesis and response to chemotherapy [2]. Despite advances in treatment strategies, the overall curative rate of BC remains low [3]. Given this, there is an urgent need to develop novel and efficient approach for BC treatment.
Cisplatin (CDDP) is a widely used chemotherapeutic agent for the treatment for various types of malignancy includes BC [4]. Despite the positive effects in BC treatment, BC cells might become resistant to CDDP due to decreased cellular uptake of CDDP, increased DNA repair, and diminished apoptosis [5, 6]. Because apoptosis is mostly controlled by mitochondrial membrane potential [7], proteins that regulate the mitochondrial apoptotic checkpoint play an important role in CDDP resistance [8]. Thus, the downregulation of pro-apoptotic proteins of the Bcl-2 family is needed in reversing the resistance of CDDP [9, 10].
Recently, microRNA (miRNA) has become increasingly relevant in cancer research. miRNAs are a class of small, endogenous, noncoding, single-stranded RNAs of 19–25 nucleotides that functionally repress target proteins via RNA binding at imperfect complementary sequences within the 3′UTR of the target mRNA, inducing mRNA degradation or translational repression regulating gene expression [11, 12]. It has become abundantly clear that miRNAs play important roles in the development of cancer by targeting the expression of a lot of genes, including oncogenes and tumor suppressor genes [13]. Thus, miRNAs regulate many cellular processes, including cell growth, differentiation, proliferation, and apoptosis [14].
Recent reports indicated that the expression of miR-363 is dysregulated in many kinds of cancers, which is profoundly involved in oncogenesis, epithelial–mesenchymal transition, and resistance to medical drugs [15, 16]. However, the function of miR-363 in BC is still little known. In the present study, bioinformatics analysis predicts that miR-363 potentially targets to Mcl-1 that is one of the key anti-apoptotic member of the Bcl-2 family [17]. The luciferase assay confirmed that the miR-363 directly targets the 3′-UTR of Mcl-1 mRNA, and transfection of miR-363 mimics significantly downregulated the Mcl-1 expression in BC cells. We also found transfection of miR-363 mimics augments CDDP-induced apoptosis dependent on the downregulation of Mcl-1.
Materials and methods
Reagents and antibodies
Cisplatin, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), Annexin V-FITC Apoptosis Detection Kit was obtained from Sigma-Aldrich (USA). 5,5′,6,6′-Tetrachloro-1,1′,3,3′-tetraethyl imidacarbo cyanine iodide (JC-1) was obtained from Molecular Probes (USA). Antibodies for rabbit antihuman Mcl-1 and rabbit antihuman β-actin were purchased from Cell Signaling (USA). MiR-363 mimics and negative control oligonucleotide (NCO) were purchased from Genepharma Company (China). The sequences of the above RNA oligonucleotides were as follows:miR-363 mimics: 5′-AAUUGCACGGUAUCCAUCUGUA-3′; NCO: 5′-UUCUCCGAACGUGUCACGUUU-3′.
Cell culture
Human BC cell lines (MDA-MB-231, MDA-MB-435, MCF-7) and the normal breast cell line (MCF-10A) were from American Type Culture Collection (ATCC, USA). Human BC cell lines were cultured in DMEM basic medium (Gibco, USA) with 10 % fetal bovine serum (FBS, Gibco, USA) at 37 °C in a humidified 5 % CO2 incubator. MCF-10A cell line was cultured in DMEM/F12 media (Gibco, USA) supplemented with 5 % horse serum (Gibco, USA), insulin (10 µg/ml, Gibco, USA), EGF (20 ng/ml, Sigma-Aldrich, USA), cholera toxin (100 ng/ml, Sigma-Aldrich, USA), and hydrocortisone (0.5 μg/ml, Sigma-Aldrich, USA) at 37 °C in humidified incubator with 5 % CO2.
Quantitative PCR (qPCR) for miR-363 expression
Total RNA was extracted with TRIzol (Invitrogen, USA). The reverse transcription of miR-363 is performed by stem-loop reverse transcription-qPCR (RT-qPCR) method [18]. Taking U6 small nuclear RNA (snRNA U6) as internal control, the relative level of miR-363 expression was determined with the 2−∆∆CT method [19]. The primer sequences are as follows: miR-363 RT primer: 5′-CTCAACTGGTGTCGTGGAGTCGGCAATTCAGTTGAGTACAGATG-3′, miR-363 qPCR forward primer: 5′-ACACTCCAGCTGGGAATTGCACGGTATCCA-3′, miR-363 qPCR reverse primer: 5′-TGGTGTCGTGGAGTCG-3′, U6 snRNA qPCR forward primer: 5′-CTCGCTTCGGCAGCACA-3′, U6 snRNA qPCR reverse primer: 5′-AACGCTTCACGAATTT GCGT-3′.
Quantitative PCR (qPCR) for Mcl-1 expression
Total RNA was extracted with TRIzol. The cDNA was reversely transcribed using M-MLV Reverse Transcriptase (Invitrogen, USA) following the manufacturer’s instructions. The Mcl-1 gene was quantitative-amplified using SYBR Green (TaKaRa, Japan) by the extracted cDNA on the Applied Biosystems 7500 Real-Time PCR System, taking GAPDH mRNA as internal control and the relative level of Mcl-1 expression was determined with the 2−∆∆CT method. The primer sequences are as follows: Mcl-1 forward: 5′-TGGCTAAACACTTGAAGACC-3′, Mcl-1 reverse: 5′-GGAAGAACTCCACAAACCC-3′, GAPDH forward: 5′-CCACTCCTCCACCTTTG-3′, GAPDH reverse: 5′-CACCACCCTGTTGCTGT-3′.
Plasmid construction
The cDNA was reversely transcribed using M-MLV Reverse Transcriptase using the primer of oligo(dT) (Takara, Japan) following the manufacturer’s instructions. Fragment containing the putative miR-363-binding sequences of Mcl-1 mRNA 3′-UTR (GenBank accession number: NM_001197320) was amplified by PCR using the cDNA as a template and cloned into the pMIR-REPORT™ miRNA Expression Reporter Vector System (pMIR, Life Technologies, USA). The recombinant plasmid was named pMIR-Mcl-1. The PCR primers are as follows: Mcl-1 3′-UTR forward: 5′-TTACTGTAAGTGCAATAG-3′, Mcl-1 3′-UTR reverse: 5′-CTACCATCTTCACTAAAT-3′. The mutant plasmid was created by mutating the seed regions of the miR-363-binding sites (GTGCAAT to GTCGAAT) by using site-directed mutagenesis kit (Takara, Japan) and named pMIR-Mcl-1-M. The open reading frame of Mcl-1 gene without 3′-UTR was amplified by PCR with the cDNA as template and cloned into the pEGFP-N1 vector (Clontech, USA). The recombinant plasmid was named pEGFP-Mcl-1.
Transient transfection
BC cells were seeded in 6-, 48-, or 96-well plates and transfected at approximately 80 % confluence. The Firefly luciferase reporters (pMIR, pMIR-Mcl-1, pMIR-Mcl-1-M), Renilla luciferase pRL-TK vector (Promega, USA), eukaryotic expression vector (pEGFP-N1, pEGFP-Mcl-1), and RNA oligonucleotides (NCO or miR-363 mimics) were transiently transfected into the BC cells with Lipofectamine 2000 reagent (Invitrogen, USA) following the manufacturer’s instructions.
Luciferase assay
MDA-MB-231 cells were cotransfected with Firefly luciferase reporters (0.4 μg/well) and Renilla luciferase pRL-TK vector (20 ng/well) combined with miR-363 (or NCO, 10 pmol/well) using Lipofectamine 2000 reagent at 80 % cell confluence in 48-well plates for 24 h. Then, the cells were lysed, and the Firefly and Renilla luciferase activities were measured by Dual-Luciferase Reporter System (Promega, USA) according to the manufacturer’s instructions. Firefly luciferase activity was normalized to the Renilla luciferase activity. Results were represented as the ratio between the various treatments and the NC control.
Western blot assay
BC cells and MCF-10A cells were seeded in 6-well plates and transfected with miR-363 mimics (or NCO, 100 pmol/well) with/without plasmid (pEGFP-Mcl-1 or pEGFP-N1, 4.0 μg/well) at approximately 80 % confluence for 24 h. Cells were then washed twice with ice-cold PBS. The total proteins were extracted with RIPA lysis buffer (Cell Signaling, USA). The protein concentrations were determined by BCA assay (Pierce, USA), and then, the samples were separated by 12.5 % SDS–PAGE, transferred to PVDF membranes by electroblotting, and probed with anti-Mcl-1 and anti-β-actin. Membranes were then incubated with horseradish peroxidase-conjugated secondary antibody of goat anti-rabbit IgG. Blots were visualized using enhanced chemiluminescence detection kit (Pierce, USA).
Measurement of cell viability by MMT
The effect of miR-363, cisplatin, and their combination on the proliferation of MDA-MB-231 cells was measured by MTT assay. MDA-MB-231 cells were seeded in triplicate in a 96-well plate at the density of 5 × 103 per well. After incubation for 12 h, cells were transfected with miR-363 (or NCO, 5 pmol/well) with/without plasmid (pEGFP-Mcl-1, pEGFP-N1, 0.2 μg/well). After incubation for 24 h, cells were treated with 10 μmol/L of cisplatin for 48 h. The inhibition of cell proliferation was detected by MTT assay [20]. Results were represented as the ratio between the various treatments and the NC control.
Measurement of apoptosis
The effect of miR-363, cisplatin, and their combination on the apoptosis induction of MDA-MB-231 cells was measured by Annexin V/Propidium Iodide staining. MDA-MB-231 cells were seeded in a 6-well plate. After incubation for 12 h, cells were transfected with miR-363 (or NCO, 100 pmol/well) with/without plasmid (pEGFP-Mcl-1, pEGFP-N1, 4.0 μg/well). After incubation for 24 h, cells were treated with 10 μmol/L of cisplatin for 24 h. Then, 1 × 105 treated cells were incubated with Annexin V/Propidium Iodide for 15 min at room temperature according to the manufacturer’s instructions and analyzed using flow cytometry.
Measurement of mitochondrial membrane potential (∆Ψm)
MDA-MB-231 cells were seeded in a 6-well plate. After incubation for 12 h, the medium was replaced with a fresh medium and cells were transfected with miR-363 (or NCO, 100 pmol/well) with/without plasmid (pEGFP-Mcl-1, pEGFP-N1, 4.0 μg/well). After incubation for 24 h, cells were treated with 10 μmol/L of cisplatin for 24 h. Next, the cells were harvested and incubated with 5 μM JC-1 in PBS for 20 min at 37 °C. Then, the cells were washed with PBS twice before FACS analysis.
Statistical analysis
Statistical analysis was conducted with SPSS 13.0 software. Student’s t test and ANOVA analysis were used to compare mean values. Data were presented as the mean ± SD and derived from at least three independent experiments. A p < 0.05 was considered to be statistically significant.
Results
Expression levels of miR-363 and Mcl-1 in BC cell line and normal breast cell line
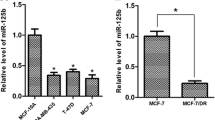
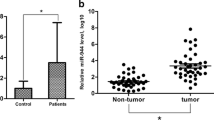
To determine the role of miR-363 and Mcl-1 in BC cells, we first measured the levels of Mcl-1 and miR-363 in normal breast cell line (MCF-10A) and three BC cell lines (MDA-MB-231, MDA-MB-435, MCF-7). The results showed that there was statistically significant difference in the expression levels of miR-363 and Mcl-1 between BC cell lines and MCF-10A. The BC cell lines expressed lower level of miR-363 (Fig. 1a) and higher Mcl-1 at both mRNA and protein levels (Fig. 1b, c) compared with MCF-10A cells, suggesting that the miR-363 may play an anticancer role in BC cells but the expression of Mcl-1 was involved in breast carcinogenesis. There may exist an inverse correlation between the expression of Mcl-1 and miR-363.
BC cell lines express higher level of Mcl-1 and lower level of miR-363 compared with normal breast cell line. a The miR-363 expression levels of MCF-10A, MDA-MB-231, MDA-MB-435, and MCF-7 cells were detected by qPCR. *p < 0.05 versus MCF-10A. b qPCR analysis for Mcl-1 mRNA expression level in above all cell lines. *p < 0.05 versus MCF-10A. c Western blot analysis for Mcl-1 protein expression level in above all cell lines
MiR-363 enhanced the cisplatin cytotoxicity in MDA-MB-231 cells
First, we treated the MDA-MB-231 cells with various doses of cisplatin for 48 h. It was noted that cisplatin inhibited cell proliferation in a dose-dependent manner (Fig. 2a). Based on these results, we selected a moderate concentration (10 µmol/l cisplatin) for combination treatment with miR-363. To further study the role of miR-363 and its mechanism in cisplatin-induced cytotoxicity, the miR-363 mimics were transfected into MDA-MB-231 cells for 24 h. Then, cells were treated with 10 µmol/l cisplatin for 48 h. The cell viability was assessed by using MTT assay. We found that the cells transfected with miR-363 mimics enhanced cisplatin-induced cytotoxicity compared with the group of cisplatin combined with NCO (Fig. 2b). The apoptosis-inducing effect of miR-363, cisplatin, and their combination was evaluated by Annexin V/PI staining. As shown in Fig. 2c, more apoptotic cells were observed in the group that treated with the combination of cisplatin and miR-363 mimics than the single-treatment group. These data suggest that overexpression of miR-363 would sensitize the BC cells to cisplatin cytotoxicity.
MiR-363 enhanced the cisplatin cytotoxicity in MDA-MB-231 cells. a The proliferative inhibitory effects of cisplatin on MDA-MB-231 cells. *p < 0.05 versus control group. b Upregulation of miR-363 by miR-363 transfection enhanced cisplatin-induced cytotoxicity in MDA-MB-231 cells as compared with cisplatin-alone treatment. *p < 0.05 c MiR-363 or NCO was transfected into MDA-MB-231 cells for 24 h and treated with 10 μM cisplatin or not for another 24 h. The percentage of apoptosis in cells transfected with miR-363 combined with cisplatin was significantly higher than in cisplatin-alone treatment groups
MiR-363 downregulated the Mcl-1 expression in BC cells
In light of the preceding data, we check the influence of miR-363 on the expression of Mcl-1. We transfected the BC cells with miR-363 mimics or NC oligonucleotide using Lipofectamine 2000 and incubated for 24 h. As shown in Fig. 3a, all of the three BC cell lines in which the miR-363 mimics were introduced, the quantity of miR-363 increased significantly compared to NCO groups. However, the upregulation of endogenous miR-363 by the miR-363 mimics led to the significant downregulation of Mcl-1 expression in the BC cells (Fig. 3b, c). These dates support our speculation that the Mcl-1 is regulated by miR-363 in BC cells.
Inverse correlation between Mcl-1 and miR-363 in BC cells. a After the BC cells were transfected with miR-363 mimics or NCO for 6 h, the miR-363 levels in BC cells were detected by qPCR analysis. *p < 0.05. b After the BC cells were transfected with miR-363 mimics or NCO for 24 h, the Mcl-1 mRNA expression in BC cells was detected by qPCR analysis. *p < 0.05. c Western blot analysis for Mcl-1 protein level in BC cells treated as above
Mcl-1 is the direct target of miR-363
Preceding results suggested that miR-363 downregulated the Mcl-1 expression. So we tried to explore the molecular mechanisms responsible for the function of miR-363 that was observed above. The public miRNA database (TargetScan) predicted that Mcl-1 might be a target gene for miR-363 for it contains putative miR-363 target sites in its 3′-UTR (GUGCAAU, position at 12–18 nucleotides of Mcl-1 mRNA 3′-UTR, Fig. 4a). In order to further identify whether Mcl-1 in BC cells responded to miR-363 through direct interactions with its 3′-UTR, we cloned the 3′-UTR fragment of Mcl-1 containing the putative miR-363 binding sequence into the pMIR reporter plasmid. Then, miR-363 mimics or NCO and pMIR-Mcl-1, pMIR-Mcl-1-M, or pMIR empty plasmid were cotransfected into MDA-MB-231 cells transiently. As shown in Fig. 4b, cotransfection of miR-363 significantly suppressed the luciferase activity of the reporter with wild-type 3′-UTR of Mcl-1 but not that of the mutant reporter as well as the empty reporter. In addition, transfection with pEGFP-Mcl-1 totally overcomes the suppression of Mcl-1 caused by miR-363 because the pEGFP-Mcl-1 contained no 3′-UTR (Fig. 4c). These data suggest that miR-363 may negatively regulate the expression of Mcl-1 by directly targeting the 3′-UTR of its mRNA.
Mcl-1 is the direct target of miR-363. a TargetScan analysis predicted that Mcl-1 3′-UTR was the possible target of miR-363. b A dual-luciferase reporter system was employed for the measurement of luciferase activity. MDA-MB-231 cells were cotransfected with RNA mimics, pRL-TK, and pMIR plasmid containing wild-type or mutant 3′-UTR of putative target gene. pRL-TK expressing Renilla luciferase was performed as an internal control to correct the differences in both transfection and harvest efficiencies. The Firefly luciferase activity of each sample was normalized to the Renilla luciferase activity. *p < 0.05 c qPCR and Western blot analysis for Mcl-1 levels in MDA-MB-231 cells after transfection with RNA mimics and plasmid for 24 h. The suppression of Mcl-1 by miR-363 was abolished by transfection of the cells with pEGFP-Mcl-1 without 3′-UTR. *p < 0.05
The sensitization of miR-363 to cisplatin-induced cytotoxicity was dependent on the Mcl-1
Our preceding results showed that miR-363 sensitized cisplatin-induced apoptosis in BC cells, and Mcl-1 is the direct target of miR-363. To further evaluate whether Mcl-1 is involved in apoptosis caused by miR-363 combined with cisplatin in BC, MDA-MB-231 cells were cotransfected with pEGFP-Mcl-1 when the cells were treated with miR-363 for 24 h. Then, the culture medium was changed fresh, and cisplatin was added into the media for 24 h. As shown in Fig. 5, exogenous expression of Mcl-1 significantly decreased the inhibition effect and apoptotic rate in combining treatment. These data supported the role of Mcl-1 that is involved in miR-363-promoted apoptosis.
Mcl-1 abolished the sensitization of miR-363 to cisplatin-induced cytotoxicity. a MDA-MB-231 cells were cotransfected with pEGFP-Mcl-1 (or empty plasmid) and miR-363 for 24 h. Then, 10μM cisplatin was added into the media for another 24 h. MTT assay was performed for evaluating the cell proliferation. *p < 0.05 b Cells were treated as above description. Then, the cell apoptosis was measured using Annexin V/PI staining on flow cytometry
MiR-363 combined with cisplatin significantly decreased the mitochondrial membrane potential of BC cells
Apoptosis through the intrinsic pathway is imminent when mitochondrial membrane potential (∆Ψm) collapses [21]. Mcl-1 is an anti-apoptotic Bcl-2 family member which plays a key role in maintaining ∆Ψm [22]. So, given that the Mcl-1 plays crucial roles in the mitochondrial apoptosis pathway, we examined whether introduction of miR-363 combined with cisplatin triggered a mitochondrial pathway, based on the assays of ∆Ψm. The ∆Ψm was detected using JC-1 as an indicator, which is a lipophilic and cationic dye that accumulates in the mitochondria in a potential-dependent manner. JC-1 emits red fluorescence in normal cells, but the fluorescence will disappear if the ∆Ψm collapses [23]. As shown in Fig. 6, the negative controls and cisplatin group displayed similar fluorescent intensity of JC-1. In contrast, an obvious increase in the proportion of cells with loss of ∆Ψm was shown in miR-363 combined with cisplatin group compared to both miR-363 and cisplatin-alone treatment group. Furthermore, the loss of ∆Ψm caused by miR-363 combined with cisplatin was reversed when the exogenous Mcl-1 was transfected into the MDA-MB-231 cells.
Combination of miR-363 and cisplatin may induce apoptosis through a mitochondrial pathway. miR-363 combined with cisplatin significantly decreased the ∆Ψm compared to both miR-363 or cisplatin-alone treatment group in MDA-MB-231 cells, but the ∆Ψm loss effect was reversed by transfecting with pEGFP-Mcl-1
Taken together, our data suggest that miR-363 was a negative regulator of Mcl-1 expression, and the combination of miR-363 and cisplatin may induce apoptosis by triggering the mitochondrial pathway.
Discussion
Previous researches have demonstrated that Mcl-1 is a key anti-apoptotic protein from the Bcl-2 family, which had been shown to mediate chemotherapy resistance in multiple cancers [24]. Moreover, many reports indicated that poor prognosis correlates with high expression of Mcl-1 protein in human cancer cells, and high expression of Mcl-1 contributes to the ability of cancer cells to survive and evade the toxic effects of chemotherapy drugs; reports showed that the Mcl-1 gene is involved in cisplatin resistance in breast cancer [25–28]. In this report, we demonstrated that the expression of Mcl-1 was upregulated and miR-363 was downregulated in MDA-MB-231 cells as compared with the normal breast cell line MCF-10A. Increasing evidence showed that the expression changes of miRNAs always lead to tumorigenesis [29]. Cancer cells always alter the transcription of oncogenes and tumor suppressor genes by rebuilding the expression of miRNAs to promote the proliferation and anti-apoptosis [30, 31]. MiR-363 has been reported to associate with tumorigenesis, and recent studies prove that miR-363 was always downregulated in multiple cancers, suggesting that miR-363 may play as tumor suppressor gene [32, 33]. Furthermore, recent studies indicated that aberrant miRNAs are associated with chemotherapy response in breast cancer [34, 35]. However, the molecular mechanisms by how miRNAs modulate the behavior of cancer cells are still largely unknown.
Breast cancer is one of the leading causes of women mortality and the most common cancer among women worldwide. Chemotherapy is irreplaceable for treating the malignant breast cancer to prolong the patients’ life span [36]. However, most chemotherapeutic drugs are referred to as cytotoxic drugs for killing rapidly dividing cells that include not only tumor cells but also normal proliferating cells such as stomach lining and marrow cells. Cisplatin is an effective chemotherapeutic agent used widely for the treatment for a variety of malignancies such as lung cancer, ovarian cancer, prostate cancer, and breast cancer [37, 38]. Despite the anti-tumor effect of cisplatin is encouraging, drug resistance has been observed in many patients who have relapsed from cisplatin treatment [39]. Because of this, combination therapy of cisplatin with other cancer drugs has been applied as novel therapeutic strategies for many human cancers. Cisplatin plus paclitaxel, osthole, or gemcitabine had been proved to delay the occurrence of drug resistance improving the effect of chemotherapy [40–42]. However, the anti-tumor effect of cisplatin combined with microRNA was known little.
The mechanism of anticancer effect of cisplatin includes the inhibition of cell proliferation and induction of cell apoptosis [43]. Cancer cells evolve to evade apoptosis because apoptosis is a major barrier that must be circumvented during tumor progression so that they can survive in the crucial tumor growth environment, such as chemotherapy treatment [44]. We showed that miR-363 could sensitize breast cancer cells to cisplatin-induced apoptosis accompany with the collapse of ∆Ψm. Therefore, downregulation of miR-363 may decrease the adaptation of breast cancer cells to the chemotherapy environment through the activation of mitochondrial pathway which as an important event in miR-363-promoted apoptosis.
Mcl-1 exerts an anti-apoptotic function through the mitochondrial signaling pathway [45]. Here, we proved that Mcl-1 is a direct target of miR-363 in MDA-MB-231 cells. Moreover, overexpression of Mcl-1 can dramatically reverse the effect of miR-363 implicates Mcl-1 as a predominant mediator of miR-363-promoted apoptosis. So, we conclude that miR-363 might take part in the cisplatin resistance through the regulation of Mcl-1 expression in breast cancer. Our study firstly described an association between miR-363/Mcl-1 expression and cisplatin-resistant breast cancer.
In summary, this study suggested that miR-363/Mcl-1 pathway might provide drug targets for the sensitivity of breast cancer cells and could be used for treating cisplatin resistance in BC patients. However, future researches are needed to further support the function of miR-363 in chemotherapy resistance. These reports may help patients who have abnormal levels of miR-363 or Mcl-1 to develop individualized treatment protocols.
References
Prabhakaran P, Hassiotou F, Blancafort P, Filgueira L. Cisplatin induces differentiation of breast cancer cells. Front Oncol. 2013;3:134.
Colombo PE, Milanezi F, Weigelt B, Reis-Filho JS. Microarrays in the 2010s: the contribution of microarray-based gene expression profiling to breast cancer classification, prognostication and prediction. Breast Cancer Res. 2011;13(3):212.
Guarneri V, Conte P. Metastatic breast cancer: therapeutic options according to molecular subtypes and prior adjuvant therapy. Oncologist. 2009;14(7):645–56.
Cobleigh MA. Other options in the treatment of advanced breast cancer. Semin Oncol. 2011;38(Suppl 2):S11–6.
Galluzzi L, Vitale I, Michels J, Brenner C, Szabadkai G, Harel-Bellan A, et al. Systems biology ofcisplatin resistance: past, present and future. Cell Death Dis. 2014;5:e1257.
Cohen SM, Lippard SJ. Cisplatin: from DNA damage to cancer chemotherapy. Prog Nucleic Acid Res Mol Biol. 2001;67:93–130.
Kroemer G, Galluzzi L, Brenner C. Mitochondrial membrane permeabilization in cell death. Physiol Rev. 2007;87(1):99–163.
Galluzzi L, Senovilla L, Vitale I, Michels J, Martins I, Kepp O, et al. Molecular mechanisms of cisplatin resistance. Oncogene. 2012;31(15):1869–83.
Castedo M, Coquelle A, Vivet S, Vitale I, Kauffmann A, Dessen P, et al. Apoptosis regulation in tetraploid cancer cells. EMBO J. 2006;25(11):2584–95.
Michaud WA, Nichols AC, Mroz EA, Faquin WC, Clark JR, Begum S, et al. Bcl-2 blocks cisplatin-induced apoptosis and predicts poor outcome following chemoradiation treatment in advanced oropharyngeal squamous cell carcinoma. Clin Cancer Res. 2009;15(5):1645–54.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97.
Winter J, Jung S, Diederichs S, et al. Many roads tomaturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol. 2009;11(3):228–34.
Song YX, Yue ZY, Luo Y, et al. MicroRNA-148b is frequently down-regulated in gastric cancer and acts as a tumor suppressor by inhibiting cell proliferation. Mol Cancer. 2011;10:1.
Cheng AM, Byrom MW, Shelton J, Ford LP. Antisense inhibition of human miRNAs and indications for an involvement of miRNA in cell growth and apoptosis. Nucleic Acids Res. 2005;33(4):1290–7.
Qiao J, Lee S, Paul P, Theiss L, Tiao J, Qiao L, Kong A, Chung DH. miR-335 and miR-363 regulation of neuroblastoma tumorigenesis and metastasis. Surgery. 2013;154(2):226–33.
Sun Q, Zhang J, Cao W, Wang X, Xu Q, Yan M, Wu X, Chen W. Dysregulated miR-363 affects head and neck cancer invasion and metastasis by targeting podoplanin. Int J Biochem Cell Biol. 2013;45(3):513–20.
Thomas L, Lam C, Edwards S. Mcl-1 the molecular regulation of protein function. FEBS Lett. 2010;584(14):2981.
Chen C, Ridzon DA, Lee DH, et al. Real-time quantification of microRNAs by stem-loop RT-PCR. Nucleic Acids Res. 2005;33(20):e179.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25(4):402–8.
Tong SJ, Liu J, Wang X, Qu LX. microRNA-181 promotes prostate cancer cell proliferation by regulating DAX-1 expression. Exp Ther Med. 2014;8(4):1296–300.
Zhang Z, Zheng L, Zhao Z, Shi J, Wang X, Huang J. Grape seed proanthocyanidins inhibit H2O2-induced osteoblastic MC3T3-E1 cell apoptosis via ameliorating H2O2-induced mitochondrial dysfunction. J Toxicol Sci. 2014;39(5):803–13.
Varadarajan S, Butterworth M, Wei J, Pellecchia M, Dinsdale D, Cohen GM. Sabutoclax (BI97C1) and BI112D1, putative inhibitors of MCL-1, induce mitochondrial fragmentation either upstream of or independent of apoptosis. Neoplasia. 2013;15(5):568–78.
Prathapan A, Vineetha VP, Raghu KG. Protective effect of Boerhaavia diffusa L. against mitochondrial dysfunction in angiotensin II induced hypertrophy in H9c2 cardiomyoblast cells. PLoS ONE. 2014;9(4):e96220.
Kelly PN, Strasser A. The role of Bcl-2 and its pro-survival relatives in tumourigenesis and cancer therapy. Cell Death Differ. 2011;18(9):1414–24.
Vinothini G, Murugan RS, Nagini S. Mitochondria-mediated apoptosis in patients with adenocarcinoma of the breast: correlation with histological grade and menopausal status. Breast. 2011;20(1):86–92.
Luo L, Zhang T, Liu H, Lv T, Yuan D, Yao Y, et al. MiR-101 and Mcl-1 in nonsmall-cell lung cancer: expression profile and clinical significance. Med Oncol. 2012;29(3):1681–6.
Zhang T, Zhao C, Luo L, Zhao H, Cheng J, Xu F. The expression ofMcl-1 in human cervical cancer and its clinical significance. Med Oncol. 2012;29(3):1985–91.
Zhang Z, Teruya K, Yoshida T, Eto H, Shirahata S. Fucoidan extract enhances the anti-cancer activity of chemotherapeutic agents in MDA-MB-231 and MCF-7 breast cancer cells. Mar Drugs. 2013;11(1):81–98.
Ren LH, Chen WX, Shi RH, et al. MicroRNA-183 promotes proliferation and invasion in oesophageal squamous cell carcinoma by targeting programmed cell death 4. Br J Cancer. 2014; [Epub ahead of print].
Qin Y, Dang X, Li W, Ma Q. miR-133a functions as a tumor suppressor and directly targets FSCN1 in pancreatic cancer. Oncol Res. 2013;21(6):353–63.
Lei SL, Zhao H, Yang Q, et al. Regulatory roles of microRNA-708 and microRNA-31 in proliferation, apoptosis and invasion of colorectal cancer cells. Oncol Lett. 2014;8(4):1768–74.
Ng SB, Yan J, Huang G, Selvarajan V, Tay JL, Lin B, et al. Dysregulated microRNAs affect pathways and targets of biologic relevance in nasal-type natural killer/T-cell lymphoma. Blood. 2011;118(18):4919–29.
Sun Q, Zhang J, Cao W, Wang X, Xu Q, Yan M, Wu X, Chen W. Dysregulated miR-363 affects head and neck cancer invasion and metastasis by targeting podoplanin. Int J Biochem Cell Biol. 2013;45(3):513–20.
Ru P, Steele R, Hsueh EC, Ray RB. Anti-miR-203 upregulates SOCS3 expression in breast cancer cells and enhances cisplatin chemosensitivity. Genes Cancer. 2011;2(7):720–7.
Sun L, Yao Y, Liu B, Lin Z, Lin L, Yang M, Zhang W, Chen W, Pan C, Liu Q, Song E, Li J. MiR-200b and miR-15b regulate chemotherapy-induced epithelial-mesenchymal transition in human tongue cancer cells by targeting BMI1. Oncogene. 2012;31(4):432–45.
Decatris MP, Sundar S, O’Byrne KJ. Platinum-based chemotherapy in metastatic breast cancer: current status. Cancer Treat Rev. 2004;30(1):53–81.
Tsimberidou AM, Braiteh F, Stewart DJ, Kurzrock R. Ultimate fate of oncology drugs approved by the us food and drug administration without a randomized trial. J Clin Oncol. 2009;27(36):6243–50.
Dhar S, Kolishetti N, Lippard SJ, Farokhzad OC. Targeted delivery of a cisplatin prodrug for safer and more effective prostate cancer therapy in vivo. Proc Natl Acad Sci USA. 2011;108(5):1850–5.
Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer. 2002;2(1):48–58.
Fang Y, Wang L, Xia GH, Shi MQ. Clinical investigation of efficacy of albumin bound paclitaxel plus platinum compounds as first-line chemotherapy for stage III/IV squamous non-small cell lung cancer. Asian Pac J Cancer Prev. 2014;15(17):7453–7.
Xu XM, Zhang Y, Qu D, Liu HB, Gu X, Jiao GY, Zhao L. Combined anticancer activity of osthole and cisplatin in NCI-H460 lung cancer cells in vitro. Exp Ther Med. 2013;5(3):707–10.
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, Roughton M, Bridgewater J. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Zhao JX, Liu H, Lv J, Yang XJ. Wortmannin enhances cisplatin-induced apoptosis in human ovarian cancer cells in vitro. Eur Rev Med Pharmacol Sci. 2014;18(17):2428–34.
Zu Y, Yang Z, Tang S, Han Y, Ma J. Effects of p-glycoprotein and its inhibitors on apoptosis in k562 cells. Molecules. 2014;19(9):13061–75.
Takahashi H, Chen MC, Pham H, Matsuo Y, Ishiguro H, Reber HA, Takeyama H, Hines OJ, Eibl G. Simultaneous knock-down of Bcl-xL and Mcl-1 induces apoptosis through Bax activation in pancreatic cancer cells. Biochim Biophys Acta. 2013;1833(12):2980–7.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grants 81200104 and 81302020).
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, R., Li, Y., Dong, X. et al. MiR-363 sensitizes cisplatin-induced apoptosis targeting in Mcl-1 in breast cancer. Med Oncol 31, 347 (2014). https://doi.org/10.1007/s12032-014-0347-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0347-3