Abstract
Purpose
The purpose of this study was to evaluate the prognostic value of the metabolic tumor volume (MTV), in FIGO stage IA–IIB cervical cancer patients, measured by F-18 fluorodeoxyglucose positron emission tomography (FDG-PET) imaging.
Methods
Forty-five patients with invasive cervical cancer who underwent FDG-PET imaging were recruited. Metabolically active tumor regions were delineated on the pretreatment FDG-PET scans by encompassing regions equal to or greater than an standardized uptake value (SUV) of 40% of the peak tumor intensity. The relationship of the metabolic tumor volume (MTV) to the disease-free survival was analyzed. The MTV of the cervical cancer was compared with pathological and clinical prognostic factors, including lymph node metastasis, parametrial invasion, the depth of invasion, resection margins, tumor differentiation and FIGO stages.
Results
Cox proportional hazard regression analysis showed that the MTV was a significant independent predictor of recurrence of cervical cancer (p = 0.027). Patients with an MTV of >20 cm3 had a significantly reduced disease-free survival compared with patients with an MTV ≤ 20 cm3 (p = 0.029). The correlation of the MTV with traditional prognostic factors showed significantly higher values in patients that were lymph node (LN) metastasis positive (p = 0.028) and parametrial invasion positive (p = 0.022). The MTV significantly differed among the groups according to tumor differentiation (p = 0.0319) and FIGO stage (p = 0.001).
Conclusion
The MTV measured by FDG-PET was an independent prognostic factor for tumor recurrence in patients with stage IA–IIB cervical cancer. These findings must be confirmed by large population based prospective studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is one of the most common causes of cancer-related death in women worldwide [1]. Accurate prediction of prognosis is important as it influences survival and patient management decisions. The traditional prognostic factors, such as lymph node (LN) metastasis, parametrial invasion, positive tumor margins, a large tumor size, deep stromal invasion and lymphovascular invasion (LVI) are currently considered important prognostic factors for survival and provide some useful clinical and pathological information [1]. However, the accuracy of these traditional prognostic factors continues to be debated, except for the presence of LN metastasis in patients with cervical cancer [2]. Therefore, substantial research efforts have focused on the identification of novel prognostic factors to accurately predict the prognosis of patients with cervical cancer.
Positron emission tomography (PET) with F-18 fluorodeoxyglucose (FDG) is used for the staging and follow-up of a wide variety of cancers, including lymphomas, non-small cell lung cancers (NSCLC), colorectal cancers, malignant melanoma, breast cancer, and esophageal cancer [3–5]. Previous research has shown that FDG-PET is valuable for assessment of prognosis in patients with cervical cancer [6–8]; it readily identifies the primary tumor and accurately assesses spread to lymph nodes as well as distant metastases [9, 10]. A widely accepted functional parameter derived from FDG-PET is the standardized uptake value (SUV); however, a volumetric parameter for the FDG-PET has been rarely established.
Recent clinical studies in patients with lung cancer and head and neck cancer have indicated that a high tumor volume measured by FDG-PET is associated with poor survival and a poor patient outcome [11, 12]. However, the metabolic tumor volume (MTV) of FDG PET/CT imaging, as a prognostic factor, has rarely been studied in patients with cervical cancer.
The goal of the present study was to determine whether the MTV detected on FDG PET/CT imaging could be used as a prognostic marker for the disease-free survival in patients with International Federation of Gynecology and Obstetrics (FIGO) stage IA to IIB cervical cancer that underwent surgery, with or without adjuvant therapy.
Materials and Methods
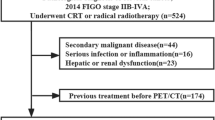
Selection of Patients
In this retrospective study, 45 patients with FIGO stage IA–IIB cervical cancer were evaluated. The patients were recruited between October 2006 and June 2009. All patients underwent a physical examination, intravenous pyelography (IVP), cystoscopy, chest X-ray, magnetic resonance imaging (MRI) of the pelvis, and FDG PET/computed tomography (CT) as well as other routine laboratory tests prior to surgery. Patients who were treated with neoadjuvant chemotherapy or conization as a diagnostic method were excluded in this study group. All patients were treated by radical hysterectomy with pelvic lymph node dissection. The pathologists divided the pathological risk factors into a high and an intermediate risk group. The high-risk group included patients that had positive pelvic lymph nodes, microscopic parametrial invasion, or positive resection margins. The intermediate group included patients with stromal invasion (≥1 cm), LVI, or a bulky tumor (≥4 cm). Patients with one or more high risk factors, and in all patients that were FIGO stage IIb, received treatment with irradiation and concurrent 5-FU (1 g/m2 body-surface area for days 1–4, by intravenous infusion) and cisplatin (50 mg/m2 on day 1, intravenously), which was repeated every 4 weeks up to four cycles. Patients that had one or more intermediate risk factors received adjuvant radiation therapy (RT) alone. The radiotherapy performed included: 10 MV X-rays using a four-field box technique, with 1.8 Gy daily, 5 days per week, up to a total dose of 50.4 Gy, and if necessary, a booster dose of 5.4–9.0 Gy was delivered to the lateral pelvic wall.
F-18 FDG PET/CT
All patients were examined using a dedicated PET/CT scanner (Gemini, Philips, Milpitas, Calif., USA), consisting of a dedicated germanium oxyorthosilicate full-ring PET scanner and a dual-slice helical CT scanner. Standard patient preparation included at least 8 h of fasting and a serum glucose level of less than 120 mg/dl before F-18 FDG administration. F-18 FDG PET-CT imaging was performed 60 min after injection of F-18 FDG (mean dose, 383.7 ± 47.4 MBq; range, 314.5-488.4 MBq). At 60 min after administration of F-18 FDG, low-dose CT (30 mA, 120 kV) covering the area from the base of the skull to the proximal thighs was performed for the purpose of attenuation correction and precise anatomical localization. Thereafter, the emission scan was performed in the three-dimensional (3D) mode. The emission scan time per bed position was 3 min; nine bed positions were acquired. PET data was obtained using a high-resolution whole-body scanner with an axial field of view of 18 cm. The average axial resolution varied between 4.2 mm full width at half maximum (FWHM) in the center and 5.6 mm at 10 cm. The average total PET/CT examination time was 30 min. After scatter and decay correction, the PET data was reconstructed iteratively with attenuation correction and reoriented in axial, sagittal, and coronal slices. The row action maximum-likelihood algorithm was used for 3D reconstruction.
Metabolic Tumor Volume Calculation
The tumor area was delineated on the FDG-PET image by circle encompassing regions equal to or greater than an SUV of 40% of the peak tumor intensity [13] (Fig. 1). The MTV of each slice was determined by multiplying the area within the threshold margin by the CT interval. The final metabolic tumor volume was calculated by adding all metabolic tumor volumes of each slice. The SUVmax within the MTV was calculated automatically:
- Si:
-
the area with abnormal metabolism of each slice
- d:
-
the interval of CT scan
- n:
-
the number of slices with abnormal metabolism
Follow-up
Clinical follow-up examinations were performed at 3-month intervals after completion of treatment. The purpose of the follow-up studies was to analyze the duration of the disease-free survival. The disease-free interval was defined as the time from the initial treatment to relapse noted on the images or the last follow-up visit.
Statistical Analysis
The pathological and clinical factors as well as outcome data were analyzed for their correlation with the FDG-PET tumor volume. The independent t-test was used to compare the mean MTV values in the different subgroups. The difference in the MTV among the FIGO stages and tumor differentiation was analyzed by the Kruskal-Wallis test. The optimal MTV cut-off value was determined by receiver-operator characteristic (ROC) curves. Linear regression was employed for the correlation of the SUVmax with the MTV. The disease-free survival was calculated using the Kaplan–Meier method. The log-rank test was used for the univariate analysis of prognostic factors. Variables shown to be significant and borderline significant (p < 0.1) were selected for the multivariate analysis. The Cox proportional-hazards model was used for the multivariate analyses. The statistical analyses were performed using MedCalc for Windows version 8.1 and statistical significance was defined as p < 0.05.
Results
Patients
The patient characteristics are summarized in Table 1. The mean age was 52.6 ± 9.4. The median follow-up was 21 months (range, 4–38 months). Five patients had disease recurrence. None died of the cervical cancer during the follow-up period. The median MTV was 5.4 cm3 (range, 0–112.9 cm3). There were 11 patients (24.5%) with FIGO stage IA disease, 29 (64.5%) with IB, one (2.2%) with IIA, and four (8.8%) with IIB. Thirty-four tumors (75.5%) were classified as squamous cell carcinomas and 11 (24.5%) as adenocarcinomas. Twenty-eight carcinomas (62.2%) were graded as well differentiated, 14 (31.1%) as moderately differentiated, and three (6.7%) as poorly differentiated. Thirteen patients (28.8%) had pelvic LN metastases, six (13.3%) had microscopic parametrial invasion, and 16 (35.5%) had LVI. Twenty-five patients (55.5%) had a 1-cm or greater depth of invasion. Five (11.1%) patients had positive resection margins.
Comparison of MTV According to Pathological and Clinical Factors
The MTV among the FIGO stages (p = 0.0012) and tumor differentiation (p = 0.0319) showed statistically significant differences by the Kruskal-Wallis test. According to the tumor stage, the mean MTV was 1.2 ± 1.9 cm3 for stage IA, 17.3 ± 21.1 cm3 for IB, 17.6 ± 0.0 cm3 for IIA and 57.9 ± 46.8 cm3 for IIB. The MTV was significantly higher in patients with pelvic lymph node metastasis (p = 0.0286) and parametrial invasion (p = 0.0229) compared with the negative patients (Table 2). However, the difference in the MTV, for patients with LVI, resection margins and stromal invasion were not statistically significant.
Survival Analysis
The univariate analysis of tumor differentiation, resection margins, depth of invasion, SUVmax and MTV were significant parameters associated with the disease-free survival (Table 3). To further elucidate the effects of the MTV, the patients were divided into two groups with a cut-off value of 20.0 cm3 determined by the ROC curves (Fig. 2). Kaplan–Meier analysis, for the disease-free survival, was divided into patients with relatively larger (>20 cm3) compared with small tumor volumes (≤20 cm3). When stratified by an MTV of 20 cm3, only one patient out of 33 cases (3.03%) showed an event such as nodal metastasis or distant metastasis in MTV ≤20 cm2,. However, four in 12 cases (33.3%) showed the events when MTV >20 cm2. Event frequency is significantly high in MTV >20 cm2 (χ2 = 4.726, p = 0.029) (Fig. 3).
The optimal MTV cut-off value was determined by ROC curves: The optimal cut-off value for the MTV was 20.0 cm3. When 20.0 cm3 was used as the cut-off value, the sensitivity and specificity were 80.0% (95% CI: 28.4-99.5) and 82.5% (95% CI: 67.2-92.7), respectively. The area under the curve was 0.825 (95% CI: 0.683-0.922) and the standard error was 0.100 (p = 0.001)
The two metabolic indices, the SUVmax and the MTV, were predictive of disease recurrence and had a significant correlation with each other by linear regression analysis. The coefficient of determination, R 2 = 0.406, and the best fit line at the 95% confidence intervals (CIs) were determined (p < 0.001).
Prediction of Disease-Free Survival
The Cox proportional hazard regression analysis showed that only the MTV was an independent prognostic factor for the disease-free survival (p = 0.027) (Table 4).
Discussion
F-18 FDG PET/CT is an increasingly popular modality that incorporates both anatomical localization and functional information that is potentially a useful tool for risk stratification in patients with cervical cancer [14]. Several studies have suggested that a higher SUV is associated with a worse prognosis in patients with cervical cancer [9, 10]. According to Kidd et al. [9], the SUVmax of a tumor, at diagnosis, was a sensitive biomarker for future treatment response and prognosis in patients with cervical cancer. Xue et al. [10] reported that a higher SUV was correlated with a poor prognosis, including a poorer disease-free survival. This study differs from these prior investigations. The univariate statistical analysis showed that the SUVmax had only borderline significance (p = 0.06). In addition, the multivariate analysis showed that the SUVmax was not statistically significant. These findings suggest that the SUVmax could not be used as a prognostic factor with the other traditional pathological and clinical prognostic factors. Further study is needed to determine the usefulness of the SUVmax as a prognostic factor in patients with cervical cancer.
The degree of tumor uptake of FDG on PET as assessed by the SUV was shown to be an independent prognostic factor in various cancers [15, 16]. However, there have been conflicting results in the use of SUV for predicting prognosis [11]. Thus, more effective prognostic factors are needed. It has been reported that the volume of tumor tissue demonstrating increased FDG uptake on PET, or metabolic tumor volume (MTV), is a novel potential prognostic factor. The MTV represents the metabolic extent of the tumor and the size of the viable tumor cells. For lung cancer, head and neck cancer, and lymphomas, the MTV has been shown to be highly prognostic for disease progression and death, independent of other established prognostic factors [11, 12, 17]. The results of this study suggest that the MTV is an important independent prognostic factor for the disease-free survival of patients with FIGO stage IA–IIB cervical cancer. It appears to be of greater importance for patient prognosis than other conventional prognostic factors and the SUVmax in patients with cervical cancer. Similar results were reported from a prior study [13]. Miller and Grigsby [13] evaluated the value of the tumor volume measurement using FDG-PET in patients with advanced cervical cancer and found that the tumor volume was predictive of the progression-free survival.
Previous investigators showed that tumor size is an important prognostic factor in patients with cervical carcinoma [18, 19]. Tumor volume has been measured with CT and MRI until recently. Plataniotis et al. [20] found that tumor volume measured by MRI was the most significant independent factor for overall survival in patients with advanced head and neck cancer. Bradley et al. [21] reported that the gross tumor volume determined by CT scanning was the most significant factor associated with the overall survival of patients with non-small cell lung cancer.
This study differs from prior studies in that the tumor volumes were derived from FDG-PET scans. The tumor volume detected by FDG-PET has advantages compared with tumor volumes determined by CT and MRI. First, tumor volumes determined by FDG-PET have higher tumor-to-background ratios. This feature facilitates tumor detection and quantitative analysis. Second, the tumor volume detected by FDG-PET represents the size of highly viable tumor cells. Whereas, the tumors detected by CT or MRI can include non-viable necrotic tissues in the anatomical information. Thus, measurement of tumor volume by FDG-PET provides more accurate information than by either CT or MRI [22].
In contrast to prior studies, this study failed to show any significance of the SUVmax for the disease-free survival by the Cox multivariate survival analysis. However, the SUVmax was one of the prognostic factors that was statistically significant on the univariate analysis and showed a significant correlation with the MTV in the current study. The underlying causes of such a discrepancy might be due to a small sample size and inconsistent ranges of FIGO stages compared with previous studies. Moreover, other conventional prognostic factors such as LVI, depth of invasion, tumor resection margins, and tumor differentiation were not significant by the Cox proportional-hazard regression model. These traditional prognostic factors were not significant for determining disease-free survival in patients with cervical cancer in this study.
The limitations of this study included the following. One of the limitations is PET-CT has a relatively low sensitivity for the assessment of early stage cervical cancer evaluation, especially for stage IA cervical cancer, due to limited spatial resolution. In this study, only four out of 11 stage 1A cervical cancer exhibited FDG uptake. Such lower sensitivity detection of early cervical cancer might have diluted the prognostic effect of SUVmax in the current study. The other limitation of the study is relatively small sample size and short follow up period. The median follow-up was 21 months, which was relatively short. A longer follow-up, incorporating a broader subject base could potentially produce a significant change in the results. Despite these limitations, highly significant results were obtained, demonstrating a correlation between a high MTV and the disease-free survival of patients with cervical cancer. These findings suggest that patients with a high MTV may be at increased risk for disease recurrence and may benefit from more aggressive treatment and follow-up.
In conclusion, the results of the present study suggest that the MTV, a volumetric parameter of FDG-PET, is an important independent prognostic marker for survival in patients with stage IA–IIB cervical cancer, and that the MTV is a better predictor of disease-free survival than traditional prognostic factors in these patients. Patients with cervical cancer and a high pretreatment MTV (>20.0 cm3) should be considered for more careful follow-up and may need more aggressive treatment. Additional prospective studies with a larger number of patients are needed to confirm the prognostic utility of this promising functional parameter derived from the FDG-PET.
References
Jermal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics. CA Cancer J Clin. 2009;59:225–49.
Lee YY, Choi CH, Kim CJ, Kang H, Kim TJ, LEE JW, et al. The prognostic significance of the SUVmax (maximum standardized uptake value for F-18 fluorodeoxyglucose) of the cervical tumor in PET imaging for early cervical cancer: preliminary results. Gynecol Oncol. 2009;115:65–8.
Conti PS, Lilien DL, Hawley K, Keppler J, Grafton ST, Bading JR. PET and 18 F-FDG in oncology: a clinical update. Nucl Med Biol. 1996;23:717–35.
Rigo P, Paulus P, Kaschten BJ, Hustinx R, Bury T, Jersalem G, et al. Oncological applications of positron emission tomography with fluorine-18 fluorodeoxyglucose. Eur J Nucl Med. 1996;23:1641–74.
Gambhir SS, Czernin J, Schwimmer J, Silverman DH, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med. 2001;42:1S–93.
Rose PG, Adler LP, Rodriguez M, Faulhaber PF, Abdul-Karim FW, Miraldi F. Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: a surgicopathologic study. J Clin Oncol. 1999;17:41–5.
Wong TZ, Jones EL, Coleman RE. Positron emission tomography with 2-deoxy-2-[(18)F]fluoro-d-glucose for evaluating local and distant disease in patients with cervical cancer. Mol Imag Biol. 2004;6:55–62.
Miller TR, Pinkus E, Dehdashti F, Grigsby PW. Improved prognostic value of 18 F-FDG PET using a simple visual analysis of tumor characteristics in patients with cervical cancer. J Nucl Med. 2003;44:192–7.
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. The SUV for 18FDG-PET is a sensitive predictive biomarker for cervical cancer treatment response and survival. Cancer. 2007;110:1738–44.
Husain A, Akhurst T, Larson S, Alektiar K, Barakat RR, Chi DS. A prospective study of the accuracy of 18Fluorodeoxyglucose positron emission tomography (18FDG PET) in identifying sites of metastasis prior to pelvic exenteration. Gynecol Oncol. 2007;106:177–80.
Lee P, Weerasuriya DK, Lavori PW, Quon A, Hara W, Maxim PG, et al. Metabolic tumor burden predicts for disease progression and death in lung cancer. Int J Radiat Oncol Biol Phys. 2007;69:328–33.
Seol YM, Kwon BR, Song MK, Choi YJ, Shin HJ, Chung JS, et al. Measurement of tumor volume by PET to evaluate prognosis in patients with head and neck cancer treated by chemo-radiation therapy. Acta Oncol. 2010;49:201–8.
Miller TR, Grigsby PW. Measurement of tumor volume by PET to evaluate prognosis in patients with advanced cervical cancer treated by radiation therapy. Int J Radiat Oncol Biol Phys. 2002;53:353–9.
Kyzas PA, Evangelou E, Denaxa-Kyza D, Ioannidis JPA. 18 F-fluorodeoxyglucose positron emission tomography to evaluate cervical node metastases in patients with head and neck squamous cell carcinoma: a meta-analysis. J Natl Cancer Inst. 2008;100:712–20.
Chan SC, Chang JT, Wang HM, Lin CY, Ng SH, Fan KH, et al. Prediction for distant failure in patients with stage M0 nasopharyngeal carcinoma: the role of standardized uptake value. Oral Oncol. 2009;45:52–8.
Eschmann SM, Friedel G, Paulsen F, Reimold M, Hehr T, Budach W, et al. Is standardized (18)F-FDG uptake value an outcome predictor in patients with stage III non-small cell lung cancer? Eur J Nucl Med Mol Imaging. 2006;33:263–9.
Shapiro M, Yun M, junkins-Hopkins JM, Vittorio CC, Schulman N, Saidman BH, et al. Assessment of tumor burden and treatment response by 18 F-fluorodeoxyglucose positron emission tomography in patients with cutaneous T- and B-cell lymphoma. J Am Acad Dermatol. 2002;47:623–8.
Alvarez RD, Potter ME, Soong SJ, Gay FL, Hatch KD, Partridge EE, et al. Rationale for using pathologic tumor dimensions and nodal status to subclassify surgically treated stage Ib cervical cancer patients. Gynecol Oncol. 1991;43:108–12.
Sethi TK, Bhalla NK, jena AN, Rawat S, Orberoi R. Magnetic resonance imaging in carcinoma cervix-does in have a prognostic relevance. J Cancer Res Ther. 2005;1:103–7.
Plataniotis GA, Theofanopoulou ME, Kalogera-Fountzila A, Haritanti A, Ciuleanou E, Ghilezan N. Prognostic impact of tumor volumetry in patients with locally advanced head-and-neck carcinoma (non-nasopharyngeal) treated by radiotherapy alone or mbined radiochemotherapy in a randomized trial. Int J Radiat Oncol Biol Phys. 2004;59:1018–26.
Bradley JD, leumwananonthachi N, Purdy JA, Wasserman TH, Lockett MA, Graham MV, et al. Gross tumor volume, critical prognostic factor in patients treated with three-dimensional conformal radiation therapy for non-small-cell lung carcinoma. Int J Radiat Oncol Biol Phys. 2002;52:49–57.
Xie P, Yue JB, Zhao HX, Sun XD, Kong L, Fu Z, et al. Prognostic value of F-18 FDG PET-CT metabolic index for nasopharyngeal carcinoma. J Cancer Res Clin Oncol. 2009. doi:10.1007/s00432-009-0729-7. Nov 20 [Epub ahead of print].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, B.S., Kim, I.J., Kim, SJ. et al. The Prognostic Value of the Metabolic Tumor Volume in FIGO stage IA to IIB Cervical Cancer for Tumor Recurrence: Measured by F-18 FDG PET/CT. Nucl Med Mol Imaging 45, 36–42 (2011). https://doi.org/10.1007/s13139-010-0062-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-010-0062-8