Abstract
Systemic docosahexaenoic acid (DHA) has been explored as a clinically feasible protectant in stroke models. However, the mechanism for DHA-afforded neuroprotection remains elusive. Transient middle cerebral artery occlusion (tMCAO) was induced for 1 h. DHA (i.p., 10 mg/kg) was administered immediately after reperfusion and repeated daily for 3 days. Stroke outcomes, systemic inflammatory status, and microglia/macrophage phenotypic alterations were assessed 3 days after stroke. Macrophage depletion was induced by clodronate liposomes injection. Primary macrophage cultures were used to evaluate the direct effect of DHA on macrophages. We demonstrated that post-stroke DHA injection efficiently reduced brain infarct and ameliorated neurological deficits 3 days after tMCAO. Systemic DHA treatment significantly inhibited immune cell infiltration (macrophages, neutrophils, T lymphocytes, and B lymphocytes) and promoted macrophage polarization toward an anti-inflammatory M2 phenotype in the ischemic brain. Meanwhile, systemic DHA administration inhibited the otherwise elevated pro-inflammatory factors in blood and shifted circulating macrophage polarity toward M2 phenotype after ischemic stroke. The numbers of circulating immune cells in blood and spleen, however, were equivalent between DHA- and vehicle-treated groups. The protective effects of DHA were macrophage-dependent, as macrophage depletion abolished DHA-afforded neuroprotection. In vitro studies confirmed that DHA suppressed production of chemokines and pro-inflammatory cytokines from macrophages under inflammatory stimulation. These data indicate that post-stroke DHA treatment ameliorated acute ischemic brain injury in a macrophage-dependent manner and DHA enhanced macrophage phenotypic shift toward an anti-inflammatory phenotype to reduced central and peripheral inflammation after stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune responses are initiated promptly after stroke onset and play critical roles in ischemic brain injury and recovery. The local microglia and peripheral macrophages are among the first responders to cells damaged in the central nervous system (CNS) and are mobilized to the site of injuries within hours. These immune cells, although necessary for clearance of debris and activation of reparative processes, can release detrimental products that either directly injure the surrounding cells or recruit harmful immune cells to exacerbate the brain lesion. Modulation of microglia/macrophage response represents an important therapeutic strategy for ischemic stroke [1].
Omega-3 polyunsaturated fatty acids (n-3 PUFAs) have been shown to offer potent protection against acute ischemic stroke. Docosahexaenoic acid (DHA) is a major form of n-3 PUFAs in the CNS. Prophylactic or therapeutic diet supplementation of n-3 PUFAs is well documented to elevate brain levels of DHA and reduce brain injury under pathological conditions including stroke [2,3,4]. Specifically, increased n-3 PUFA intake favors an anti-inflammatory environment in the injured brain and drives microglia/macrophage polarization toward an inflammation-resolving M2 phenotype [2, 5]. However, dysphagia and poor general condition make per oral systemic (os) therapy of n-3 PUFAs difficult for stroke patients. Systemic DHA treatment (intraperitoneal or intravenous injection) after stroke has therefore widely been investigated as a clinically relevant approach to ameliorate acute ischemic brain injury and enhance functional recovery [6,7,8]. DHA and its metabolites are important immune modulators and play critical roles in inflammation resolution [9]. Impairment in systemic synthesis of DHA dysregulates macrophage polarization and exacerbates inflammation in peripheral tissues [10]. Previous in vitro study has identified the capacity of DHA to directly adjust microglia phenotypic changes under normal or inflammatory environments [5]. However, the impact of systemically administered DHA on the central and peripheral immune milieu after stroke and the underlying mechanisms are not fully characterized.
The present study evaluated the therapeutic efficacy of repeated DHA injection after transient cerebral ischemia and investigated the impact of DHA on peripheral and central immune responses. Our results showed that post-stroke injection of DHA improved stroke outcomes during the acute phase of cerebral ischemia in a macrophage-dependent manner. DHA dampened the expression of chemokines and pro-inflammatory cytokines by activated macrophages, while arousing their expression of anti-inflammatory factors, and driving macrophages toward an anti-inflammation phenotype.
Materials and Methods
Animals
In total, 123 C57BL/6 mice (including 99 male and 24 female, 8- to 12-week-old, weight 18–25 g) were purchased from Guangdong Medical Laboratory Animal Center (Guangzhou, China) and housed in a humidity- and temperature-controlled animal facility in Sun Yat-sen University with a 12-h light-dark cycle for at least 1 week before induction of ischemic stroke. Food and water were freely accessible. All the experimental procedures for the current study were in compliance with the National Institutes of Health’s Guide for the Care and Use of Laboratory Animals. All the experimental protocols were approved by the Animal Care and Use Committee of Sun Yat-sen University following the Guide for the Care and Use of Laboratory Animals (8th edition, 2011) [11].
Ischemic Stroke Model
A focal ischemic stroke model was induced in mice with transient middle cerebral artery occlusion (tMCAO) as described previously [12]. Briefly, mice were anesthetized with 1.5% isoflurane in air under spontaneous breathing. A midline neck incision was made and soft tissues over the trachea are retracted gently. The left common carotid artery (CCA) was isolated and ligated temporarily. A permanent knot was placed on the distal part of the external carotid artery (ECA) and a loose temporal knot was placed on both the proximal parts of the ECA. A tight temporal knot was placed on the internal carotid artery (ICA). The ECA was cut between the permanent knot and the temporal knot; a filament was inserted into the ECA and directed to the middle cerebral artery (MCA) through the ICA after loosening the temporal knot on the ICA. Once the filament insertion into the MCA was confirmed, the loose temporal knot on the ECA was tightened and the temporal knot on the CCA was loosen. Filament insertion into the ICA was maintained for 60 min followed by reperfusion. Sham-operated animals underwent the same anesthesia and surgical procedures but were not subjected to arterial occlusion. Core body temperatures were maintained with a heating pad. The cerebral blood flow (CBF) during the surgery was measured by laser Doppler flowmetry. Mice with less than 70% reduction of blood flow in the ischemic core or that died during surgery were excluded from further analyses.
Drug Administration
DHA sodium salt (Sigma-Aldrich D8768) was dissolved in sterile saline and administered (10 mg/kg) intraperitoneally (i.p.) immediately to animals in the DHA-treated group after reperfusion and repeated daily for consecutive 3 days. Animals in the vehicle (Veh)-treated group and sham group received an equivalent volume of sterile saline i.p. injection. Animals were sacrificed 3 days after tMCAO. All outcome endpoints were measured by investigators blinded to experimental group assignments.
Immunofluorescence Staining and Quantification
At 3 days after tMCAO, animals were euthanized and perfused with saline followed by PBS containing 4% paraformaldehyde (PFA, Sigma-Aldrich). Brains were removed and cut into 25-μm frozen cryosections using a microtome. Brain sections were incubated with primary antibodies at 4 °C overnight. After washing in PBS, sections were incubated with secondary antibodies for 1 h at room temperature. Sections were then washed and mounted with DAPI Fluoromount-G (Southern Biotech). The following primary antibodies were used: rabbit anti-NeuN (1:500, Millipore), rabbit anti-Iba1 (1:1000, Wako), goat anti-CD206 (1:500, R&D system), and rat anti-CD16/CD32 (1:500, BD bioscience). The following secondary antibodies were applied: anti-rabbit secondary antibody conjugated with Cy3 (1:1000, Jackson ImmunoResearch Laboratories), anti-rabbit secondary antibody conjugated with Alexa Fluor 488 (1:1000, Jackson ImmunoResearch Laboratories), anti-rat secondary antibody conjugated with Alexa Fluor 488 (1:1000, Jackson ImmunoResearch Laboratories), and anti-goat secondary antibody conjugated with Alexa Fluor 488 (1:1000, Jackson ImmunoResearch Laboratories). For neuronal apoptosis analysis, terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) was processed after NeuN labeling according to instructions from the manufacturer (In Situ Cell Death Detection Fluorescein, Roche). Immuno-positive cell quantification and area analysis were performed with the software of Image J by an investigator who was blinded to the experimental design (National Institutes of Health). In quantification of cell count, the stroke core was identified as the region in which the majority of DAPI-stained nuclei were shrunken, and the stroke penumbra was defined as the region of generally morphologically normal cells, approximately 450–500 μm wide, surrounding the stroke core [13].
Infarct Volume Analysis
The volume of brain infarct was assessed by immunostaining using rabbit anti-NeuN antibodies (Millipore) or 2,3,5-triphenyltetrazolium chloride (TTC) staining. A series of six sections in the middle cerebral artery territory were selected from each mouse brain and stained with anti-NeuN antibodies or TTC. For TTC staining, 4% TTC (Sigma) dissolved in sterile saline was used to stain the fresh cut brain coronal brain slices (1 mm thick) followed by fixation of the slices with 4% PFA. The area of infarct lesion for each section was determined as the difference between the NeuN/TTC-positive area of contralateral hemisphere and ipsilateral hemisphere. Brain infarct was determined by multiplying the mean area of tissue loss by the distance between the two adjacent stained brain slices (1 mm).
Neurological Deficit Scoring
Neurological deficit score was assessed right after ischemia-reperfusion (0d) and every 24 h in the following 3 consecutive days (1d, 2d, 3d). Neurological deficit score was determined on a 0–4 scale, 0, no apparent deficit; 1, weakness in the ipsilateral forelimb (right); 2, circulating to the ipsilateral side (right); 3, body unbalance and trunk incline to ipsilateral; 4, no spontaneous motor activity or death. Eight mice in the Veh-treated group and 10 mice in the DHA-treated group were submitted to assessment of neurological deficit score [14].
Flow Cytometric Analysis
Single cells from the brain, blood, and spleen were prepared for flow cytometric analysis (FACS) 3d after tMCAO. Briefly, blood and spleen were extracted before animals were perfused with ice-cold saline. Brains were dissected and ipsilateral hemispheres were collected. Each hemisphere was subjected to 0.25% trypsin-EDTA (Thermo Fisher) digestion at 37 °C for 21 min. Brain tissue was then pressed through a cell strainer (70 μm, Fisherbrand). Brain cells were separated from myelin debris by centrifuge in 30%/70% Percoll solution (GE healthcare). Brain cells at the interface were collected, washed with PBS, and subjected to further staining. The spleen was homogenized and pressed through a cell strainer (40 μm, Fisherbrand). Red blood cell lysis buffer (Sigma-Aldrich) was applied to get rid of red blood cells in spleen and blood. Spleen cells and blood leukocytes were then subjected to further staining.
Single cells from the brain, spleen, and blood were stained with CD45-PerCp/Cy4.5 (1:400, Biolegend), CD11b-PE (1:400, Biolegend), Ly6G-APC/Cy7 (1:400, Biolegend), CD3-PerCP (1:400, Biolegend), and CD19-APC (1:400, Biolegend) or CD45-PerCp/Cy4.5 (1:400, Biolegend), CD11b-PE (1:400, Biolegend), CD206-Alexa Fluor 647 (1:200, BD bioscience), and CD16-PE/Cy7 (1:400, Thermo Fisher eBioscience). To evaluate CD206 expression of in vitro macrophage, cells were collected and stained with CD206-Alexa Fluor 647 (1:200, BD bioscience). FACS was performed using a fluorescence-activated cell sorter flow cytometer (BD Biosciences), and data was analyzed using FlowJo X 10.0.7r2 software. Appropriated isotype controls were stained following the manufacturer’s instruction (Thermo-eBioscience). Fluor-chrome compensation was performed with single-stained OneComp eBeads (Thermo-eBioscience).
Real-Time Polymerase Chain Reaction
Total RNA was isolated from brains and primary cultured macrophages using the RNeasy Mini Kit (QIAGEN) according to the manufacturer’s instructions; 1 μg RNA (OD260 nm/OD280 nm = 1.8–2.2) was used to synthesize the first strand of cDNA using the PrimeScript RT reagent Kit (Takara). PCR was performed on a 7500 fast (ABI) real-time polymerase chain reaction (RT-PCR) machine using SYBR Premix Ex Taq (Takara). Primers for the following mRNA were used: IL-10 (GenBank: NM_010548.2), IL-4 (GenBank: NM_021283.2), Arg1 (GenBank: AB047402.1), TGFβ (GenBank: NM_011577.2), CD206 (GenBank: NM_008625.2), IL-1α (GenBank: NM_010554.4), IL-6 (GenBank: NM_031168.2), IL-17 (GenBank: NM_010552.3), TNFα (GenBank: NM_013693.3), IFNγ (GenBank: NM_008337.4), CD86 (GenBank: NM_019388.3), CCL2 (GenBank: NM_011333.3), CCL17 (GenBank: NM_011332.3), CXCL1 (GenBank: NM_008176.3), CXCL2 (GenBank: NM_009140.2), CXCL10 (GenBank: NM_021274.2), CXCL12 (GenBank: NM_021704.3), and CXCL13 (GenBank: NM_018866.2). The cycle values were normalized to GAPDH (GenBank: NM_001289726.1). Primer sequences are shown in Table S3. For real-time PCR, the following program was performed: 95 °C 30 s (pre-denaturation); 95 °C 5 s and 60 °C 34 s for 40 cycles (amplification); 95 °C 15 s, 60 °C 1 min; and 95 °C 15 s (melt curve). The expression levels of the mRNAs were then reported as fold change vs sham brain or vehicle-treated macrophages.
Protein Array
Inflammatory mediators in serum were assessed with Proteome Profiler Mouse Cytokine Array Kit (R&D system, ARY006) at 3 days after tMCAO according to the manufacturer’s instruction. For each sample, 300 μl of serum was applied to the test strip. Image density was calculated with Image J (National Institutes of Health) and was normalized to reference of each sample and concerted to the fold change of the sham.
Macrophage Depletion
Hematogenous macrophages were depleted with clodronate liposomes. Empty liposomes were injected as the control (Clodrosome Macrophage Depletion Kits, Clodrosome). Clodronate liposomes or empty liposomes were injected into mice 36 h before tMCAO (i.p., 75 mg/kg). Efficiency of macrophage depletion was assessed with FACS and the effect to microglia was determined with Iba1-immunofluorescence staining.
Primary Macrophage-Enriched Culture
Primary macrophage-enriched cultures were prepared from the bone marrow of 8- to 10-week-old healthy C57BL/6J mouse using EasySep Mouse Monocyte Enrichment Kit (Stem Cell, Cat. No. 19761) according to manufacturer’s instructions. Macrophages were induced with macrophage colony-stimulating factor (MCSF) for 6 days (50 ng/ml) in culture medium (RPMI1640 + 10% FBS). Enriched macrophages were treated with LPS (2.5 ng/ml) with or without DHA (20 μM) for 24 h.
Statistical Analysis
All results were presented as mean ± standard error of the mean. The differences in the means among multiple groups were analyzed using one- or two-way analysis of variance (ANOVA). When ANOVA showed significant differences, pair-wise comparisons between means were tested by Dunnett’s tests. The Student t test was used for two-group comparisons. In all analysis, P < 0.05 was considered statistically significant.
Results
Post-stroke Injection of DHA Ameliorates Brain Infarct and Neuronal Death After tMCAO
Male C57/BL6 wild-type (WT) mice were treated with DHA (i.p., 10 mg/kg) or saline (Veh) immediately after reperfusion and repeated daily for 3 days. DHA post-stroke-treated male mice exhibited significantly smaller infarct volume (Fig. 1a) and reduced neurological deficits (Fig. 1b) 3 days after tMCAO as compared to vehicle-treated mice. The number of dead neurons, as revealed by NeuN (green) and TUNEL (red) double staining, in the penumbra area was significantly reduced by DHA post-treatment (Fig. 1c). To affirm the therapeutic effects of post-stroke DHA injection in male mice, female mice in proestrus or estrus phases were subjected to tMCAO and systemic treatment was applied after cerebral ischemia. Female mice that received post-stroke DHA therapy showed significantly smaller infarct volume as assessed with TTC staining. These results indicate that systemic DHA treatment after stroke provides potent protection against acute ischemic brain injury, to both male and female mice. Since spleen size could vary along with stroke severity, splenocytes of male and female mice were counted at 3d after stroke or sham operation. No significant alteration in the number of splenocyte was detected (Fig. 1e).
Post-stroke DHA treatment protects against acute cerebral ischemia. C57/BL6 mice were subjected to 60-min tMCAO followed by daily DHA (10 mg/kg, i.p.) or saline (Veh, vehicle) treatment for 3 days. Animals were sacrificed at 3d after tMCAO. a Infarct volume of male mice was quantified on NeuN (green)-stained coronal sections (n = 10 for Veh- and n = 8 for DHA-treated group). Dashed lines outline the infarct area. b Neurological deficit score was assessed at days 1–3 after tMCAO (n = 10 for Veh- and n = 8 for DHA-treated group). c (left) Representative images demonstrating TUNEL (red) co-labeling with NeuN (green) in infarct penumbra 3 days after tMCAO. c (right) Quantification of the number of NeuN+TUNEL+ neurons (yellow, emphasized with white arrows). n = 4 mice per group. d Infarct volume of female mice was quantified on TTC (red)-stained coronal sections (n = 8 for Veh- and n = 8 for DHA-treated group). Dashed lines outline the infarct area. e Spleen size of male and female mice was evaluated with splenocyte count at 3d after tMCAO or sham operation. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001 versus Veh. STR, striatum; CTX, cortex
Systemic DHA Therapy Reduces Immune Cell Infiltration into the Ischemic Brain
Cerebral inflammation, as hallmarked by the activation of CNS glial cells and abrupt influx of peripheral immune cells into the ischemic brain, is known to exacerbate brain injury [15]. Flow cytometry was used to determine the influence of DHA treatment on immune cell responses in the ischemic brain 3 days after stroke. The presence of peripheral macrophages (CD11b+CD45highLy6G−), neutrophils (CD11b+CD45highLy6G+), B lymphocytes (CD19+CD3−), and T lymphocytes (CD3+CD19−) in the ischemic brains was identified with specific markers (Fig. 2a). Post-stroke DHA treatment slightly decreased the total cell counts (including immune and non-immune cells such as neurons and astrocytes) in the ischemic hemisphere though not up to significance (Fig. 2b). Meanwhile, the percentage among brain cells of CNS microglia (CD11b+CD45intermediate) remained the same between DHA- and vehicle-treated stroke mice (Fig. 2c). Consistent with the reduced brain injury, systemic DHA therapy dramatically reduced the percentage among brain cells of infiltrated peripheral immune cells as compared to vehicle-treated mice 3 days after stroke (Fig. 2d, e).
Systemic DHA therapy reduces immune cell infiltration into the ischemic brain. Immune cell infiltration in ipsilateral cerebral hemisphere was analyzed by flow cytometry 3 days after tMCAO. a Gating strategy for macrophages (CD11b+CD45hiLy6G−), neutrophils (CD11b+CD45hiLy6G+), microglia (CD45intCD11b+), B lymphocytes (CD19+CD3−), and T lymphocytes (CD3+CD19−). b Total brain cells of vehicle- and DHA-treated mice in the ischemic hemisphere analyzed with flow cytometry. c–e Representative FACS panels and quantification of the percentage among brain cells of immune cells, namely microglia c, neutrophils and macrophages d, as well as B and T lymphocytes e, in the ipsilateral brain. Total cells included both immune and non-immune cells such as neurons and astrocytes. n = 5 for Veh- and n = 6 for DHA-treated group. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001 versus Veh. Veh, vehicle; SSC, side scatter; FSC, forward scatter; A, area; W, width; H, height; hi, high; int, intermediate
Post-stroke DHA Therapy Induces an Inflammation-Resolving Phenotype of Macrophages in the Ischemic Brain
It is more and more accepted that the functional status of microglia/macrophages is important in stroke outcomes [15,16,17,18]. We therefore further assessed the effect of post-stroke DHA treatment on microglia/macrophage functional phenotypes after stroke. Flow cytometric analysis was performed on single-cell suspensions prepared from ischemic brains 3 days after tMCAO. The percentages of anti-inflammatory M2 phenotypic cells (CD206+CD16−) and inflammatory M1 phenotypic cells (CD206−CD16+) were quantified among the CD45highCD11b+ macrophage population. Repeated DHA injection significantly increased the percentage of M2 phagocytes, without altering the percentage of M1 cells (Fig. 3a). The expression of CD206 or CD16 remained low in microglia (CD45intermediateCD11b+) in both DHA- and vehicle-treated stroke mice (Fig. 3b). Double immunofluorescent staining of CD206 or CD16 with a microglia/macrophage marker Iba1 confirmed an enhanced M2 polarization 3 days after stroke in DHA-treated mice as compared to vehicle-treated mice. DHA treatment resulted in an increase in the number of CD206+Iba1+ microglia/macrophages (Fig. 3c, d), while the number of CD16+Iba1+ microglia/macrophages remained the same (Fig. 3e). Consistent with the anti-inflammatory phenotypic shift in macrophages, the mRNA expression of anti-inflammatory markers, including IL-10, Arginase-1, and TGFβ, after stroke significantly increased in the brains of DHA-treated mice. The levels of pro-inflammatory markers, however, did not show any significant difference between DHA and vehicle groups (Fig. 3f).
Post-stroke DHA therapy induces anti-inflammatory phenotype of macrophages in the ischemic brain. Microglia/macrophage phenotypes in the ischemic brain were analyzed with flow cytometry, immunofluorescent staining, and RT-PCR 3 days after tMCAO. a Representative FACS panels and quantification showing that DHA treatment induced an anti-inflammatory phenotype (CD206+CD16−) of macrophages (CD45hiCD11b+), while had no impact on the pro-inflammatory subset (CD206−CD16+). n = 5 for Veh- and n = 6 for DHA-treated group. b Representative FACS panels showing that microglia (CD45intCD11b+) expressed low levels of CD206 and CD16 3 days after tMCAO in DHA- (n = 6) or vehicle-treated (n = 5) mice. c Immunofluorescent staining and statistical analysis of CD206 (green) and Iba1 (red) showed that DHA treatment increased the number of anti-inflammatory M2 phenotype microglia/macrophages (CD206+Iba1+). n = 4 mice per group. d 3D reconstructed plot showing CD206-Alexa Fluor 488 fluorescence intensity in DHA- (n = 4) or vehicle-treated (n = 4) stroke mice. e 3D reconstructed plot showing CD16-Alexa Fluor 488 fluorescence intensity in DHA- (n = 4) or vehicle-treated (n = 4) stroke mice. f mRNA expression of pro-inflammatory and anti-inflammatory mediators was measured with RT-PCR in the ipsilateral brain 3 days after tMCAO. Data were converted to fold change over sham. n = 3 mice per group. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, versus Veh. Veh, vehicle; hi, high; int, intermediate; STR, striatum; CTX, cortex; IL, interleukin; Arg1, Arginase1; TGFβ, transforming growth factor beta; TNFα, tumor necrosis factor alpha; IFNγ, interferon gamma
Post-stroke Systemic DHA Injection Shifts the Circulating Macrophage Polarity Toward an Anti-inflammatory M2 Phenotype Without Changing the Immune Cell Numbers in Blood and Spleen
DHA has been reported to ameliorate the inflammatory responses in peripheral immune cells [19]. It is possible that systemic administration of DHA may exert a general anti-inflammatory effect not only in the ischemic brain, but also in the periphery. Therefore, the immune cell composition in the blood and spleen was evaluated by flow cytometry 3 days after stroke. Interestingly, systemic DHA treatment did not significantly alter the number of neutrophils (CD11b+CD45hiLy6G+), macrophages (CD11b+CD45+Ly6G−), B cells (CD19+CD3−), or T cells (CD3+CD19−) in spleen (Fig. 4a) or blood (Fig. 4b).
Systemic DHA injection shifts circulating macrophage polarity toward anti-inflammatory M2 phenotype after ischemic stroke without changing the immune cell numbers in blood and spleen. a, b Immune cells in spleen (a) and blood (b) were assessed with flow cytometry 3 days after tMCAO. n = 5–6 mice per group. n = 5 for Veh- and n = 6 for DHA-treated group. c, d Representative FACS panels and quantification showing that DHA treatment increased anti-inflammatory macrophages in blood (e) while it had no impact on macrophage phenotype in spleen (d). Gating strategy of macrophages in blood and spleen for CD206 and CD16 expression was shown (c). n = 3 for Veh- and DHA-treated group. **P ≤ 0.01, versus Veh (vehicle)
Macrophage polarization in spleen and blood was also assessed by flow cytometry. We found that post-stroke DHA treatment did not change macrophage polarization in the spleen (Fig. 4c). However, the anti-inflammatory phenotype of macrophages (CD206+CD16−) in blood was elevated in DHA-injected mice 3 days after stroke (Fig. 4d). The percentage of CD16+CD206− pro-inflammatory macrophages in blood was not affected by post-stroke DHA therapy (Fig. 4d).
Systemic DHA Injection Reduces Circulating Inflammatory Factors After Ischemic Stroke
We then measured the expression of inflammatory factors in blood 3 days after tMCAO using a commercial protein array focusing on inflammatory cytokines and chemokines (Fig. 5a). Despite the lack of influence on the number of peripheral immune cells (Fig. 4a, b), post-stroke DHA injection resulted in dramatic decreases in the levels of 18 kinds of chemokines (CCL1, CCL2, CCL3, CCL17, CXCL1, CXCL2, CXCL10, CXCL12, and CXCL13), complement (C5/5a), cytokines (IL-1α, IL-1rα, IL-27, IFNγ, and TNFα), or myeloid cell activators (GCSF, TIMP1, and TREM1) (Fig. 5b, c) in the premise of comparable reference protein, while the other 22 inflammatory factors analyzed with the array remained unchanged. Taken together, these data suggest that post-stroke DHA treatment adjusts the peripheral inflammatory milieu, probably through regulating the activation of immune cells (e.g., macrophages) instead of changing their numbers in the circulation or peripheral lymph organs.
Systemic DHA injection reduces circulating inflammatory factors after ischemic stroke. Cytokine and chemokine production was measured in blood using protein array 3 days after tMCAO. Heat map (a), representative dot plots (b), and quantification (c) showed that post-stroke DHA treatment downregulated 17 inflammatory factors including chemokines, complement, cytokines, and myeloid cell activators in blood 3d after MCAO among 40 tested factors. n = 3 mice in Sham group and n = 4 mice from Veh- or DHA-treated group. *P ≤ 0.05, **P ≤ 0.01, versus Veh. Veh, vehicle; CCL, CC chemokine ligand; CXCL, CXC chemokine ligand; IL, interleukin; IFNγ, interferon gamma; TNFα, tumor necrosis factor alpha; GCSF, granulocyte colony-stimulating factor; MCSF, macrophage colony-stimulating factor; GMCSF, granulocyte-macrophage colony-stimulating factor; TIMP1, tissue inhibitor of metalloproteinases 1; TREM1, triggering receptor expressed on myeloid cells 1
Systemic DHA Administration Failed to Improve Stroke Outcome in Macrophage-Depleted Animals
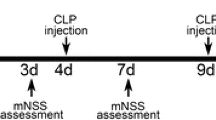
To further evaluate the role of macrophages in DHA-afforded neuroprotection after ischemic stroke, we depleted macrophages with clodronate liposomes (i.p., 75 mg/kg) 36 h before tMCAO (Fig. 6a). Compared with empty liposomes, clodronate liposomes efficiently cleared macrophages in the blood (Fig. 6b), while microglia in the brain remained intact (Fig. 6c). tMCAO was then induced in macrophage-depleted mice. Depletion of macrophages (CL-Veh) significantly reduced acute brain infarct (Fig. 6d) and neurological deficits (Fig. 6e) as compared to macrophage-competent stroke mice (EL-Veh). Interestingly, post-stroke DHA treatment to macrophage-depleted mice (CL-DHA) failed to further reduce the lesion size or neurological deficits (Fig. 6d, e). We then investigated the direct effect of DHA on macrophages in vitro. Cultured primary macrophages were activated with LPS (2.5 ng/ml). DHA (20 μM) or vehicle was applied immediately after LPS. After 24 h of treatment, LPS-activated macrophages displayed an amoeba-like morphology, while DHA-treated macrophages largely maintained a polygon shape as seen in unstimulated cultures (Fig. 6f). The mRNA expression of various inflammatory mediators was assessed. During LPS-activating treatment of macrophages, DHA treatment dramatically elevated the expression of anti-inflammatory mediators (Arginase-1 and TGFβ) and suppressed production of chemokines (CCL2 and CXCL10) and pro-inflammatory cytokines (IL-1α and TNFα) (Fig. 6g). To evaluate the direct effect of DHA treatment to CD206 expression of macrophage, flow cytometry was performed. After 48-h treatment, LPS-activated macrophages showed downregulated CD206 expression, while DHA treatment reverses the alteration (Fig. 6g).
Macrophages are indispensable for the neuroprotective effects of systemic DHA administration. a Timeline of clodronate liposomes application and stroke outcome analysis. Macrophages were depleted with clodronate liposomes (i.p., 75 mg/kg). Administration of empty liposomes without clodronate was set as control. tMCAO was induced 36 h after clodronate liposomes application. b, c Impact of clodronate liposomes on blood macrophages (b) and brain microglia (c) in sham mice 36 h after liposome application. n = 3 mice per group. d Infarct volume was assessed with TTC staining 3 days after stroke. n = 6 mice per group. ***P ≤ 0.001, versus EL-Veh (empty liposomes injected mice and treated with vehicle after tMCAO). e Neurological deficit score was assessed at 0–3 days after stroke. n = 6 mice per group. *P ≤ 0.05, versus EL-Veh. f–h Primary cultured macrophages were activated with LPS (2.5 ng/ml). DHA (20 μM) or vehicle was applied immediately after LPS. f Representative images showing morphological alteration of macrophages after LPS activation with or without DHA treatment for 24 h from 3 independent experiments. g mRNA expression of inflammatory mediators in activated macrophages were measured by RT-PCR after 24 h treatment. h Expression of CD206 protein was analyzed with flow cytometry after 48-h treatment. Data were collected from 3 independent experiments. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001. EL, empty liposomes; CL, clodronate liposomes; Veh, vehicle
Discussion
Neuroinflammation promotes the progression of tissue damage after cerebral ischemia, leading to secondary brain injury and neuronal death [20,21,22,23]. The functional and phenotypic plasticity of macrophages has been characterized in the ischemic brain [24] and documented to be important for stroke outcomes. The present study demonstrates that intraperitoneal DHA administration after stroke provides protective effects against acute cerebral ischemia. The systemic DHA-afforded neuroprotection relied on its modification of macrophage plasticity.
The protective effect of systemic-applied DHA on acute ischemic brain injury has been reported previously in models of ischemic stroke- and hyperglycemia-enhanced hemorrhage transformation after stroke [25,26,27,28]. The mechanisms of protection are attributed to reduced cell apoptosis and ameliorated glial cell activation. Unesterified DHA can be converted into a stereospecific derivative NPD1, which is a neuroprotectant that reduces apoptotic DNA damage and inhibits cell death [7, 29, 30]. Intravenous application of DHA has been reported to elevate NPD1 synthesis in the penumbra, extensively attenuate the death of CNS cells including astrocytes and neurons, and reduce microglial activation [7]. Despite these solid studies elucidating the roles of DHA in the brain, its peripheral effect has not been well-characterized. Actually, systemically administered DHA is immediately accessible to peripheral immune cells, which are well-known key players in ischemic brain injury. This study is therefore focused on the effect of systemic DHA application on peripheral immune cells. We found that post-stroke DHA treatment dampened the production of circulating inflammatory mediators without disturbing relative cell components in the blood and spleen.
Remarkably, our study revealed the importance of macrophages in DHA-afforded neuroprotection. The depletion of circulating macrophages with a single dose of clodronate liposomes before stroke significantly removed the protective effect of DHA. It is noted that depletion of macrophages prior to stroke induction reduced brain infarct in our model, which is consistent with a previous report using the pre-stroke dosing regimen [31]. However, a recent study with repeated dosing of clodronate liposomes to induce macrophage depletion showed no impact on infarct volume but increased mortality in macrophage-depleted stroke mice [32]. There are several possibilities for this discrepancy. First, in our study, the number of CNS microglia remained intact after a single dose of clodronate liposomes. In contrast, the repeated dosing of clodronate liposomes, even after stroke, may cause extensive depletion of not only hematogenous macrophages but also CNS microglia [33, 34], depriving the brain tissue of potential neuroprotective effects from local microglia. In the current study, since microglia played marginal role in polarization (Fig. 3b), and only single dose of clodronate liposomes was applied, the impact on microglia could be elided. Second, clodronate liposome dosing after stroke may result in a rapid drug penetration through the leaky blood-brain barrier (BBB) and provoke a macroscopically visible hemorrhage [35]. Third, unknown neurotoxicity from a large dose of clodronate liposomes, which was attested by the increased mortality, may blanket any effect of macrophage depletion. Despite the discrepancy, it is found that the pro-inflammatory CCR2+ macrophages (M1) that infiltrated into the ischemic brain were critical for functional recovery after stroke [36]. The evidence indicated that although administration of clodronate liposomes might ameliorated stroke severity at acute phase, whether the treatment would compromise the repair and recovery processes in later stage of disease remained elusive. Nevertheless, our study clearly demonstrated the importance of macrophages in DHA-mediated neuroprotection in the acute phase of ischemic stroke. The in vivo and in vitro studies revealed an effect of DHA treatment in shifting macrophage polarization toward an anti-inflammatory phenotype with potent production of anti-inflammatory cytokines and reduced production of inflammatory cytokines after stimulation. This observation is consistent with studies about the effect of DHA and its derivatives on macrophages in other diseases [37, 38]. Despite the effect of DHA on both anti-inflammatory and pro-inflammatory mediators in macrophage cultures and in blood, intraperitoneal DHA treatment showed marginal effect on pro-inflammatory cytokines in the ischemic brain, which may be due to the diverse sources of these cytokines from other immune or non-immune cells.
The protection on BBB integrity after stroke represents another potential mechanism for DHA-afforded neuroprotection [7, 27]. Here, systemic DHA treatment globally restrained the infiltration of immune cells, including neutrophils, macrophages, T cells, and B cells, into the ischemic brain, which could, at least partially, contribute to preserve BBB after DHA treatment. On the other hand, we found that the levels of a cluster of chemokines in blood were reduced after repeated DHA injections after cerebral ischemia. The dampened production of CCL2, CCL3, CCL17, CXCL1, CXCL2, CXCL10, CXCL12, and CXCL13 may also contribute to the decreased quantity of neutrophils (CXCL1 and CXCL2), macrophages (CCL2), T cells (CCL3, CCL17, CXCL10, and CXCL12), and B cells (CXCL13) in the ischemic lesion after post-stroke DHA administration [35, 39, 40]. Macrophages are one of the major sources for chemokine production after stroke [41, 42]. Our results showed that DHA suppresses the expression of chemokines by macrophages, suggesting another potential mechanism for reduced immune cell infiltration in DHA-treated stroke mice.
Our results showed that the CD45hiCD11b+ cells, which are mainly recognized as infiltrated macrophages, expressed high level of phenotypic signature genes (CD206+ or CD16+) after stroke, and their phenotypes were regulated by DHA treatment. In contrast, the microglia population (CD45intCD11b+) exhibited low levels of phenotypic markers and appeared to be less involved in DHA-afforded immune modulation. However, it has previously been documented that microglial expression of CD45 increased in response to inflammation [43,44,45,46]. It is possible that the CD45intCD11b+ population included both macrophages and activated microglia. Given our previous study addressing the effect of DHA on microglia polarization [5], we cannot exclude the possible involvement of microglia in DHA-afforded neuroprotection [47]. Nevertheless, the experiment with macrophage depletion unequivocally confirmed the importance of macrophages to the protective effect of DHA in our stroke model.
Conclusion
In summary, the current study demonstrated the therapeutic efficacy of post-stroke systemic DHA treatment. Intraperitoneal DHA treatment induced an anti-inflammatory subtype of macrophages, which is important for its neuroprotection during the acute stage of stroke. Additionally, DHA is well documented to target multiple mechanisms including cell death, oxidative stress, and vascular disruption after stroke, all of which may contribute to DHA-afforded neuroprotection against ischemic stroke [48]. With its protective potency, multiple-targeting capacity, accessibility, and safety, further clinical investigation into DHA as a therapeutic agent for stroke is warranted.
References
Zhao H, Garton T, Keep RF, Hua Y, Xi G. Microglia/macrophage polarization after experimental intracerebral hemorrhage. Transl Stroke Res. 2015;6:407–9.
Jiang X, Pu H, Hu X, Wei Z, Hong D, Zhang W, et al. A post-stroke therapeutic regimen with omega-3 polyunsaturated fatty acids that promotes white matter integrity and beneficial microglial responses after cerebral ischemia. Transl Stroke Res. 2016;7:548–61.
Pu H, Jiang X, Hu X, Xia J, Hong D, Zhang W, et al. Delayed docosahexaenoic acid treatment combined with dietary supplementation of omega-3 fatty acids promotes long-term neurovascular restoration after ischemic stroke. Transl Stroke Res. 2016;7:521–34.
Zhang M, Wang S, Mao L, Leak RK, Shi Y, Zhang W, et al. Omega-3 fatty acids protect the brain against ischemic injury by activating Nrf2 and upregulating heme oxygenase 1. J Neurosci. 2014;34:1903–15.
Chen S, Zhang H, Pu H, et al. n-3 PUFA supplementation benefits microglial responses to myelin pathology. Sci Rep. 2014;4:7458.
Hong SH, Belayev L, Khoutorova L, Obenaus A, Bazan NG. Docosahexaenoic acid confers enduring neuroprotection in experimental stroke. J Neurol Sci. 2014;338:135–41.
Hong SH, Khoutorova L, Bazan NG, Belayev L. Docosahexaenoic acid improves behavior and attenuates blood-brain barrier injury induced by focal cerebral ischemia in rats. Exp Transl Stroke Med. 2015;7:3.
Berressem D, Koch K, Franke N, Klein J, Eckert GP. Intravenous treatment with a long-chain omega-3 lipid emulsion provides neuroprotection in a murine model of ischemic stroke - a pilot study. PLoS One. 2016;11:e167329.
Kuda O. Bioactive metabolites of docosahexaenoic acid. Biochimie. 2017;136:12–20.
Talamonti E, Pauter AM, Asadi A, Fischer AW, Chiurchiù V, Jacobsson A. Impairment of systemic DHA synthesis affects macrophage plasticity and polarization: implications for DHA supplementation during inflammation. Cell Mol Life Sci. 2017;74:2815–26.
National Research Council (US). Guide for the care and use of laboratory animals. 8th ed. Washington (DC): National Academies Press (US); 2011.
Stetler RA, Cao G, Gao Y, Zhang F, Wang S, Weng Z, et al. Hsp27 protects against ischemic brain injury via attenuation of a novel stress-response cascade upstream of mitochondrial cell death signaling. J Neurosci. 2008;28:13038–55.
Adelson JD, Barreto GE, Xu L, Kim T, Brott BK, Ouyang YB, et al. Neuroprotection from stroke in the absence of MHCI or PirB. Neuron. 2012;73:1100–7.
Yang Y, Liu H, Zhang H, Ye Q, Wang J, Yang B, et al. ST2/IL-33-dependent microglial response limits acute ischemic brain injury. J Neurosci. 2017;37:4692–704.
Hu X, Leak RK, Shi Y, Suenaga J, Gao Y, Zheng P, et al. Microglial and macrophage polarization-new prospects for brain repair. NAT REV NEUROL. 2015;11:56–64.
Solomon AC, Stout JC, Weaver M, Queller S, Tomusk A, Whitlock KB, et al. Ten-year rate of longitudinal change in neurocognitive and motor function in prediagnosis Huntington disease. Mov Disord. 2008;23:1830–6.
Yang Y, Liu H, Zhang H, Ye Q, Wang J, Yang B, et al. ST2/IL-33-dependent microglial response limits acute ischemic brain injury. J Neurosci. 2017;37:4692–704.
Liu X, Liu J, Zhao S, Zhang H, Cai W, Cai M, et al. Interleukin-4 is essential for microglia/macrophage M2 polarization and long-term recovery after cerebral ischemia. Stroke. 2016;47:498–504.
Ghasemi FS, Wang F, Sinclair AJ, Elliott G, Turchini GM. How does high DHA fish oil affect health? A systematic review of evidence. Crit Rev Food Sci Nutr. 2018:1–44.
Wang J, Ye Q, Xu J, et al. DRalpha1-MOG-35-55 reduces permanent ischemic brain injury. Transl Stroke Res. 2017;8:284–93.
Fan X, Jiang Y, Yu Z, Liu Q, Guo S, Sun X, et al. Annexin A2 plus low-dose tissue plasminogen activator combination attenuates cerebrovascular dysfunction after focal embolic stroke of rats. Transl Stroke Res. 2017;8:549–59.
Shimamura N, Katagai T, Kakuta K, Matsuda N, Katayama K, Fujiwara N, et al. Rehabilitation and the neural network after stroke. Transl Stroke Res. 2017;8:507–14.
Yigitkanli K, Zheng Y, Pekcec A, Lo EH, van Leyen K. Increased 12/15-Lipoxygenase leads to widespread brain injury following global cerebral ischemia. Transl Stroke Res. 2017;8:194–202.
Hu X, Li P, Guo Y, Wang H, Leak RK, Chen S, et al. Microglia/macrophage polarization dynamics reveal novel mechanism of injury expansion after focal cerebral ischemia. Stroke. 2012;43:3063–70.
Lin Y, Xu M, Wan J, Wen S, Sun J, Zhao H, et al. Docosahexaenoic acid attenuates hyperglycemia-enhanced hemorrhagic transformation after transient focal cerebral ischemia in rats. Neuroscience. 2015;301:471–9.
Belayev L, Khoutorova L, Atkins KD, Bazan NG. Robust docosahexaenoic acid-mediated neuroprotection in a rat model of transient, focal cerebral ischemia. Stroke. 2009;40:3121–6.
Belayev L, Khoutorova L, Atkins KD, Eady TN, Hong S, Lu Y, et al. Docosahexaenoic acid therapy of experimental ischemic stroke. Transl Stroke Res. 2011;2:33–41.
Chen J, Cui C, Yang X, Xu J, Venkat P, Zacharek A, et al. MiR-126 affects brain-heart interaction after cerebral ischemic stroke. Transl Stroke Res. 2017;8:374–85.
Marcheselli VL, Hong S, Lukiw WJ, Tian XH, Gronert K, Musto A, et al. Novel docosanoids inhibit brain ischemia-reperfusion-mediated leukocyte infiltration and pro-inflammatory gene expression. J Biol Chem. 2003;278:43807–17.
Li L, Tao Y, Tang J, Chen Q, Yang Y, Feng Z, et al. A cannabinoid receptor 2 agonist prevents thrombin-induced blood-brain barrier damage via the inhibition of microglial activation and matrix metalloproteinase expression in rats. Transl Stroke Res. 2015;6:467–77.
Ma Y, Li Y, Jiang L, Wang L, Jiang Z, Wang Y, et al. Macrophage depletion reduced brain injury following middle cerebral artery occlusion in mice. J Neuroinflammation. 2016;13:38.
Schmidt A, Strecker JK, Hucke S, Bruckmann NM, Herold M, Mack M, et al. Targeting different monocyte/macrophage subsets has no impact on outcome in experimental stroke. Stroke. 2017;48:1061–9.
Kumamaru H, Saiwai H, Kobayakawa K, et al. Liposomal clodronate selectively eliminates microglia from primary astrocyte cultures. J Neuroinflammation. 2012;9:116.
Lee JC, Seong J, Kim SH, Lee SJ, Cho YJ, An J, et al. Replacement of microglial cells using clodronate liposome and bone marrow transplantation in the central nervous system of SOD1(G93A) transgenic mice as an in vivo model of amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2012;418:359–65.
Gliem M, Schwaninger M, Jander S. Protective features of peripheral monocytes/macrophages in stroke. Biochim Biophys Acta. 2016;1862:329–38.
Fang W, Zhai X, Han D, Xiong X, Wang T, Zeng X, et al. CCR2-dependent monocytes/macrophages exacerbate acute brain injury but promote functional recovery after ischemic stroke in mice. THERANOSTICS. 2018;8:3530–43.
Shibui N, Kondo K. Long-term observation of patients with trauma of the lower anterior primary teeth. Shigaku. 1989;76:1556–68.
Haitz KA, Anandasabapathy N. Docosahexaenoic acid alleviates atopic dermatitis in mice by generating T regulatory cells and m2 macrophages. J INVEST DERMATOL. 2015;135:1472–4.
Roy-O’Reilly M, Ritzel RM, Conway SE, et al. CCL11 (Eotaxin-1) levels predict long-term functional outcomes in patients following ischemic stroke. Transl Stroke Res. 2017;8:578–84.
Bang OY, Moon GJ, Kim DH, et al. Stroke induces mesenchymal stem cell migration to infarcted brain areas via CXCR4 and C-Met signaling. Transl Stroke Res. 2017;8:449–60.
Xie L, Sun F, Wang J, Mao X, Xie L, Yang SH, et al. mTOR signaling inhibition modulates macrophage/microglia-mediated neuroinflammation and secondary injury via regulatory T cells after focal ischemia. J Immunol. 2014;192:6009–19.
Prinz M, Priller J. Microglia and brain macrophages in the molecular age: from origin to neuropsychiatric disease. NAT REV NEUROSCI. 2014;15:300–12.
Sedgwick JD, Ford AL, Foulcher E, Airriess R. Central nervous system microglial cell activation and proliferation follows direct interaction with tissue-infiltrating T cell blasts. J Immunol. 1998;160:5320–30.
Masliah E, Mallory M, Hansen L, Alford M, Albright T, Terry R, et al. Immunoreactivity of CD45, a protein phosphotyrosine phosphatase, in Alzheimer’s disease. Acta Neuropathol. 1991;83:12–20.
Garton T, Keep RF, Hua Y, Xi G. CD163, a hemoglobin/haptoglobin scavenger receptor, after intracerebral hemorrhage: functions in microglia/macrophages versus neurons. Transl Stroke Res. 2017;8:612–6.
Wu L, Walas S, Leung W, Sykes DB, Wu J, Lo EH, et al. Neuregulin1-beta decreases IL-1beta-induced neutrophil adhesion to human brain microvascular endothelial cells. Transl Stroke Res. 2015;6:116–24.
Zhang Z, Zhang Z, Lu H, Yang Q, Wu H, Wang J. Microglial polarization and inflammatory mediators after intracerebral hemorrhage. Mol Neurobiol. 2017;54:1874–86.
Shi Z, Ren H, Luo C, Yao X, Li P, He C, et al. Enriched endogenous omega-3 polyunsaturated fatty acids protect cortical neurons from experimental ischemic injury. Mol Neurobiol. 2016;53:6482–8.
Acknowledgments
The authors thank Dr. Lisheng Peng for technical support with the tMCAO stroke model. We thank Michael Hezel for editorial assistance.
Funding
This work was supported by grant 81671178 from the National Natural Science Foundation of China and funding from the Natural Science Foundation of Guangdong Province (2017A030311013).
Author information
Authors and Affiliations
Contributions
WC designed and performed the experiments, collected and analyzed data, and drafted the manuscript. SL carried out immunostaining, imaging, and quantification and drafted the manuscript. MH and XS performed animal experiments and collected data. WQ contributed to the experimental design and the manuscript. SZ contributed to the experimental design and revised the manuscript. XH designed the experiment and critically revised the manuscript. ZL designed and supervised the study and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethics Approval
All animal experiments were approved by the Third Affiliated Hospital of Sun Yat-sen University and performed following the Guide for the Care and Use of Laboratory Animals (8th edition, 2011) [11].
Electronic Supplementary Material
ESM 1
(DOC 267 kb)
Rights and permissions
About this article
Cite this article
Cai, W., Liu, S., Hu, M. et al. Post-stroke DHA Treatment Protects Against Acute Ischemic Brain Injury by Skewing Macrophage Polarity Toward the M2 Phenotype. Transl. Stroke Res. 9, 669–680 (2018). https://doi.org/10.1007/s12975-018-0662-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-018-0662-7