Abstract
With increasing rates of survival throughout the past several years, stroke remains one of the leading causes of adult disability. Following the onset of stroke, spontaneous mechanisms of recovery at the cellular, molecular, and systems levels ensue. The degree of spontaneous recovery is generally incomplete and variable among individuals. Typically, the best recovery outcomes entail the restitution of function in injured but surviving neural matter. An assortment of restorative therapies exists or is under development with the goal of potentiating restitution of function in damaged areas or in nearby ipsilesional regions by fostering neuroplastic changes, which often rely on mechanisms similar to those observed during spontaneous recovery. Advancements in stroke rehabilitation depend on the elucidation of both spontaneous and therapeutic-driven mechanisms of recovery. Further, the implementation of neural biomarkers in research and clinical settings will enable a multimodal approach to probing brain state and predicting the extent of post-stroke functional recovery. This review will discuss spontaneous and therapeutic-induced mechanisms driving post-stroke functional recovery while underscoring several potential restorative therapies and biomarkers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
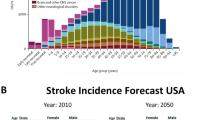
Stroke alters the landscape of the brain, compromising the function of various systems and structures. In conjunction with increasing survival rates over the past several years, stroke remains one of the leading causes of long-term disability in the USA and other developed countries [1]. The financial repercussion associated with stroke and subsequent disability is substantial, totaling over 30 billion dollars annually [2]. Behavioral deficits following stroke span domains of cognition, sensation, vision, and language with motor-related impairments most abundant [3]. Most patients experience some degree of spontaneous recovery, defined by Kwakkel et al. [4] as the amount of improvement in body function and activity determined solely by time.
Spontaneous recovery, however, is often incomplete and the recovery rates of neurological function vary. Impairments of the motor system are most frequently diagnosed and, consequently, most studied in the literature [3]. The majority of motor function gains occur within the first 3 months post-stroke [4–7]. Whereas, recovery of visuospatial neglect and orientation follow 5–6 months after stroke [8–10], and gains in cognition [11], memory [12], and language function [13, 14] may extend over a period of months to years post-stroke. Individual factors such as genetics [15–17], previous medical comorbidities, initial severity of deficits, age [18], stroke mechanism, neuroanatomical details such as lesion size and location, and areas spared injury [19–22] impact recovery.
To address the underlying complexity of recovery and stroke heterogeneity, a wide spectrum of restorative treatments encompassing drugs, stem cells, behavioral therapies, robotics, and non-invasive brain stimulation exists [23]. Accompanying this vast array of restorative therapies is a growing list of potential therapeutic targets. One viable therapeutic target rich in recovery potential is the penumbra, or the peri-infarct region. In astronomy, the penumbra is a region of half light and shadow [24]. In acute stroke, it has been defined as a region of electrical failure but preserved energy metabolism that holds recovery potential [25]. The conceptualization of the penumbra, in the context of stroke rehabilitation, is a region that survived the initial insult and is galvanized for reorganization in support of recovery. Other therapeutic targets include both local and remote non-injured areas. The aim of the above treatment approaches is to boost restitution of function in the penumbra and in functionally related targets by fostering neuroplastic change [26]. Often, the underlying mechanisms of these therapies rely on similar mechanisms observed during spontaneous recovery. Both spontaneous and therapeutic-induced mechanisms of plasticity that promote the resumption of activity and function in stroke-damaged areas can positively impact post-stroke recovery. However, as discussed below, not all plasticity mechanisms support restitution of function in stroke-damaged areas and structures.
The proceeding discussion will review both spontaneous and therapeutically induced mechanisms of post-stroke recovery while highlighting the growing assortment of restorative therapies and promising biomarkers of functional recovery in stroke.
Spontaneous Mechanisms of Functional Recovery
Stroke triggers a cascade of cellular and molecular events that facilitates neural protection and spontaneous recovery [27]. Animal studies have enhanced our understanding of these mechanisms and in-depth reviews are provided elsewhere [28, 29]. In short, experimental stroke models depict subsequent growth of synapses and dendrites [30–32], axonal remodeling and angiogenesis [33–35], increased expression of growth-related genes and proteins [36], and enhanced brain excitability mediated by alterations in N-methyl-D-aspartate (NMDA) and gamma-aminobutyric acid (GABA) receptor subtypes [37] and upregulation of NMDA receptors [38]. These events are not confined exclusively to the peri-lesioned region. Stroke-induced modulations in synaptic efficacy arise in homologous regions in the contralesional hemisphere [30], in ipsilesional areas functionally and/or structurally connected to the lesioned area [39], and even downstream in the spinal cord [40].
These brain changes, driven by discrete physiological and pathological events, can be organized into three recovery epochs. The first epoch occurs during the initial hours after stroke onset and represents an opportunity to salvage threatened tissue, e.g., via reperfusion or neuroprotection. The second epoch commences days to weeks following stroke and corresponds to an initiation of brain repair. Mechanisms of spontaneous recovery are most robust during this time. The third epoch denotes a chronic phase of brain repair when the brain is relatively stable with regards to endogenous repair-related events but modifications in brain structure and function are still possible. Because these epochs delineate periods of neuroprotection and repair, they pose important clinical implication related to the delivery of restorative therapies.
The application of restorative therapies (discussed below) in humans further elucidates the above-described cellular and molecular underpinnings of post-stroke functional recovery, but obtaining precise molecular measurements similar to those in animals proves difficult. Neuroimaging and brain mapping approaches comprising functional magnetic resonance imaging (fMRI), positron emission tomography (PET), single photon emission computed tomography (SPECT), electroencephalography (EEG), magnetoencephalography (MEG), transcranial magnetic stimulation (TMS), and near-infrared spectroscopy (NIRS), for example, provide a systems-level perspective of brain repair. The primary focus of this review entails fMRI, TMS, and EEG application to examine spontaneous and treatment-induced mechanisms of post-stroke functional recovery.
Studies employing fMRI, TMS, and EEG show modulations in local and distant cortical and subcortical activity, changes in interactions between hemispheres, shifts in cortical representational maps, and alterations in functional and effective brain connectivity. Many of these events contributing to spontaneous recovery are compensatory. In other words, areas and/or structures distinct from the injured area assume function of the injured area. These compensatory events may provide some benefit to individuals with considerable stroke-related injury and severe functional deficits [41–43]. However, compensatory events may also have the opposite effect on individuals with less severe post-stroke injury and deficits similar to how a crutch may simultaneously improve gait function for more impaired individuals and hinder gait function in less impaired individuals. Typically, mechanisms of stroke recovery that promote restitution of function to injured areas yield better rehabilitation outcomes [44].
One particular event that has received limited attention to date but may be important in stroke recovery is diaschisis. As one of several theories of functional recovery originally postulated by Von Monakow in the early twentieth century, diaschisis entails a decline in function in brain areas spatially discrete but functionally connected to the site of injury [45]. Both animals [37, 46, 47] and humans [48] demonstrate diaschisis with changes in cerebral blood flow, metabolism, and neurotransmitter activity in areas distant from the lesion. A reversal of diaschisis is suggestive of recovery, but additional work is needed to better understand the timing of diaschisis and the process of diaschisis reversal relative to time post-stroke.
Modulation of Local Cortical Structure and Function
Stroke injury to the cortex and underlying white matter results in reduced cortical activity and cortical thickness [49, 50]. Over time, a resurgence of activity occurs in conjunction with functional motor recovery [42, 44, 49, 51, 52]. Similar time-dependent shifts in cortical activity for language [53, 54] and spatial attention [55] also arise and correlate with positive functional recovery in these domains. Schaechter et al. [49] compared functional activation and cortical thickness between individuals with chronic stroke and healthy controls following a unilateral tactile stimulation activity during fMRI. Compared to control subjects, individuals with stroke demonstrated significantly greater activation in areas along the ventral postcentral gyrus and significantly greater cortical thickness within these same areas. These results depict area-specific functional and structural plasticity following stroke.
TMS is another modality used to examine local cortical function. TMS involves non-invasive brain stimulation, operating through electromagnetic induction [56], and enables individuals the ability to probe motor pathway physiology and cortical network excitability [57]. When a TMS pulse of sufficient intensity is delivered to the motor cortex region, a downstream muscle response, referred to as a motor-evoked potential (MEP), occurs. Examination of various properties of the MEP such as size, area, and latency provide valuable information about cortical and corticospinal tract excitation. Studies utilizing TMS in stroke demonstrate an initial downregulation in ipsilesional hemisphere excitability often with an absent MEP, elevated motor thresholds [58–61], diminished MEP size [62, 63], and/or prolonged MEP conduction time [64]. In instances of profound corticospinal tract damage, stimulation of the contralesional hemisphere elicits MEPs in the ipsilateral (i.e., stroke-affected) hand [65], suggestive of uncrossed contralesional corticospinal tract fibers contributing to stroke-affected (i.e., ipsilateral) extremity movement.
Shifts in motor threshold and MEP properties over time, consistent with increased cortical excitability in the ipsilesional hemisphere, are associated with positive recovery [66, 67]. Mangonotti et al. [66] observed a significant decrease in ipsilesional motor threshold during a timeframe spanning 5–7 days to 30 days post-stroke in individuals that exhibited improvements across several activities of daily living (i.e., feeding, grooming, dressing, etc.).
Modulation of Brain Regions Distant From Injury
In addition to diminished activity in the ipsilesional hemisphere, increased activation in sites distant from the infarct occurs resulting in the formation of distributed motor, language, and attention networks, sometimes bilaterally [68–74]. The utility of these distributed networks in post-stroke recovery is dependent on the amount of clinical impairment, the extent of injury, and the complexity of the functional task. The contralesional hemisphere is a particularly controversial area under study [75] especially in the context of upper-extremity motor recovery (detailed review by Buetefisch, 2015) [76]. Numerous studies support the role of the contralesional hemisphere in recovery of the stroke-affected upper-extremity [41, 43, 77–80]. However, other studies view the contralesional hemisphere as a hindrance [81–83]. For example, in an exploratory study that examined cortical activity during an fMRI hand squeezing task in individuals with chronic, subcortical stroke, investigators found increased activation in the contralesional primary motor and premotor cortices that negatively correlated to stroke-affected arm use [84]. As another example that recruitment of contralesional sensorimotor areas is not always a favorable event in the context of motor performance after stroke, significant correlations have been reported between increased contralesional primary sensorimotor cortex activation and poorer performance on a fine motor task [85]. The role of the contralesional hemisphere in functional recovery is complex and requires further investigation.
Changes in Ipsilesional and Contralesional Hemisphere Interaction
Stroke affects the interactions between hemispheres as evidenced by changes in the distribution of the blood-oxygen-level-dependent (BOLD) signal activation (i.e., laterality index) and by changes in the amount cortical inhibition imparted by one hemisphere onto the other (i.e., interhemispheric inhibition, IHI). The BOLD signal is an indirect measure of neural activity based on changes in blood flow and deoxyhemoglobin concentration [86]. IHI is a type of GABAergic-driven cortical inhibition [87–89] measured by applying a single TMS pulse to one hemisphere and a second TMS pulse to the homologous region on the other hemisphere several milliseconds later [90]. A decrease in MEP amplitude and/or area following the delivery of two TMS pulses (paired-pulse TMS) compared to the delivery of a single TMS pulse is indicative of IHI.
Individuals with stroke often exhibit a negative laterality index [68], a measure that reflects increased recruitment of the contralesional hemisphere, relative to the ipsilesional hemisphere, when performing various motor tasks using their stroke-affected extremity. Indeed, brain mapping studies show increased recruitment of contralesional motor, supplementary, and premotor cortical areas with voluntary movement from the stroke-affected extremity [70, 74, 85, 91–96]. The extent of contralesional hemisphere activation is typically predicated on the integrity of the corticospinal tract, with greater contralesional hemisphere activation associated with greater ipsilesional corticospinal tract injury [97–99]. Better motor outcomes are generally associated with progressive reductions in contralesional hemisphere recruitment and/or increased recruitment in the ipsilesional hemisphere, comparable to a pre-stroke contralateral motor organization scheme [44, 51, 52, 68, 85, 93, 100–103], although the extent to which this finding generalizes likely varies according to severity of impairment.
Imbalances in transcallosal-mediated [90, 104, 105] IHI also emerge after stroke. Compared to healthy controls, individuals with stroke often demonstrate greater inhibition in the contralesional to ipsilesional primary motor cortex direction [105–108] and/or less inhibition in the ipsilesional to contralesional primary motor cortex direction [105, 109]. Murase et al. [106] measured the amount of IHI during a simple reaction time paradigm using paired-pulse TMS. Subjects with stroke did not demonstrate significant differences in IHI at rest compared to controls. However, just prior to movement initiation of the stroke-affected hand, individuals demonstrated an increase in IHI in the contralesional to ipsilesional primary motor cortex direction that correlated to reduced finger-tapping speed and overall motor performance. In contrast, control subjects demonstrated a decrease in IHI, indicative of facilitation, prior to movement onset. Future research is required to better understand the relationship between cortical vs. subcortical lesion involvement and IHI as current work is inconclusive [104, 105, 109, 110].
Shifting of Cortical Representational Maps
Another compensatory response to stroke is reorganization or remapping of somatotopic representation. Somatotopic ordering, or maps, exist in the cortex, white matter, and subcortical structures such as the basal ganglia [111–113]. These maps are found in numerous neural systems including auditory and vision, with much of the map reorganization literature focused on the sensorimotor cortex. The most striking illustrations of cortical re-mapping following ischemic injury are in non-human primates that depict changes in map size and location occurring in conjunction with underlying axonal sprouting and the formation of new neuronal connections [39, 114, 115]. Lesion size influences the extent of cortical re-mapping [116], and subsequent rehabilitation/behavioral training alters map size and location [114, 115, 117].
In humans, studies employing fMRI [100, 101, 118, 119] and TMS [64, 119–121] depict stroke-driven alterations in map representation. Several studies reported shifts in the motor cortex hand representation in dorsal [122], ventral [100, 101, 120, 123–125], and posterior [101, 102, 119, 126, 127] directions that may represent the extent of corticospinal tract injury [128–131]. Previous work has also shown that the side and extent of injury and degree of behavioral impairment likely influence the reorganizational pattern [100, 101]. Available data suggests that while the relative position of certain map fine features shift when stroke injures these maps, key features of map organization, such as the arm motor map being dorsal to the face motor map, do not [101]. More positive motor outcomes are significantly associated with the preservation of ipsilesional motor map area [118].
Alterations in Functional and Effective Connectivity
An emerging area of study in post-stroke recovery centers on brain network connectivity (reviewed by Friston, 2011) [132]. Resting-state fMRI and EEG are attractive tools to measure functional connectivity, defined as low-frequency temporal correlations in the BOLD signal or synchronization of electrical oscillations, respectively, between distinct brain regions [132–135]. In contrast to task-oriented fMRI that requires subjects to complete a physical task during scanning, during resting-state fMRI, the subject maintains a relaxed but awake state. One important advantage of resting-state fMRI is that subjects’ physical impairments do not confound BOLD signal interpretation as they may in task-oriented fMRI. However, as with task-oriented fMRI, interpretation of functional connectivity is complicated whenever the stroke injures the very areas under study, as one must then disentangle injury effects from plasticity effects within the same zone. One strategy to address this issue is to exclude damaged regions of interest [136] or exclude subjects with a pre-specified percentage of damage to those region(s) of interest under study from analyses [137].
Research demonstrated disruptions in resting-state functional connectivity involving regions of motor [136, 138, 139], sensory, attention, and language [140] early after stroke. These disruptions often relate to the extent of white matter damage [141, 142]. Akin to previous animal work [143], functional recovery positively correlates to resting-state connectivity between interhemispheric networks. Indeed, our laboratory found that resting-state connectivity between contra- and ipsilesional primary motor cortex correlated with treatment-induced gains in motor function (r = 0.45, p = 0.01) [137].
EEG measures of coherence or phase and amplitude consistency of neural oscillations between two brain regions may function as additional probes of those processes evaluated with resting-state fMRI functional connectivity analyses as above [144, 145]. Dubovik et al. [146] found greater disruption of functional connectivity in the alpha frequency band in individuals with stroke relative to healthy controls. Further, diminished coherence in the alpha frequency band related to the severity of motor and cognitive deficits. Similar to post-stroke IHI imbalances favoring the contralesional hemisphere [105–108], Gerloff and colleagues [147] discovered greater cortico-cortical coherence in the contralesional hemisphere and reduced coherence in the ipsilesional hemisphere in individuals with chronic stroke. These results further demonstrate a compensatory functional shift in the contralesional hemisphere direction.
Effective connectivity studies extend functional connectivity studies by utilizing sophisticated modeling techniques on task-based and resting-state fMRI and EEG to explain the direction and causal relationship between two remote brain regions [134, 148, 149]. Rehme et al. [150] applied dynamic causal modeling to task-based fMRI data to examine effective connectivity between ipsilesional primary and secondary motor regions. The group found reduced positive couplings between supplementary motor area and ventral premotor cortices with ipsilesional primary motor cortex immediately after stroke that eventually increased (i.e., strengthened) over time and related to positive functional recovery. Collectively, functional and effective connectivity provide insight to the intricate brain circuitry comprising brain networks. This information may prove especially valuable when considering post-stroke therapies and corresponding therapeutic targets.
Treatment-Driven Functional Recovery Mechanisms
There are many types of restorative therapies and combinations of restorative therapies currently under study (Table 1): activity and cognitive-based training [93, 98, 151–155], robotics and brain-computer interface systems [156–158], non-invasive brain stimulation [159–161], pharmacological compounds [162–165], stem cells [166, 167], and growth factors [168]. Several meta-analyses provide treatment effect sizes for arm motor impairment following therapy: 0.34 (constraint-induced movement therapy, CIMT) [169], 0.55 (repetitive TMS) [161], 0.65 (robotic arm training) [170], and 0.92 (selective serotonin reuptake inhibitors) [171]. The implementation of these therapies to clinical practice may be hindered in part by the overall quality of evidence available. Many studies are underpowered and issues of heterogeneity between studies and inconsistent data reporting exist.
Comprehensive reviews of restorative therapies and their purported mechanisms are available [172, 173]. Briefly, several of the above therapies manipulate the peripheral nervous system while others directly stimulate brain matter. The mechanisms of action of various pharmacological-based restorative therapies may also elucidate those mechanisms asserting neuroplastic change post-stroke. For instance, the Fluoxetine for Motor Recovery After Acute Ischemic Stroke (FLAME) study investigated motor recovery in non-depressed patients randomly assigned to oral fluoxetine (20 mg/day) or placebo pill for 3 months [164]. Patients receiving fluoxetine displayed significantly greater gains in arm/leg Fugl-Meyer motor score at day 90 than the placebo group (a 9.7 point difference between groups on a 100-point scale, p = 0.003). In this study, the underlying interaction of fluoxetine and neurotransmitters resulted in enhanced motor recovery outcomes. In general, treatment-driven and spontaneous mechanisms of recovery overlap.
Carey et al. [93] observed activation of contralesional brain regions when subjects with chronic stroke performed a finger tracking exercise using their stroke-affected hand. Following a series of training sessions, subjects demonstrated significant changes in brain laterality consistent with increased utilization of the ipsilesional hemisphere. Importantly, improvement in finger tracking accuracy and shifts in brain activation translated to gains in functional activity with significant increases in Box and Block scores. Results from this seminal study demonstrated a resumption of ipsilesional hemisphere activity and an improvement in stroke-affected hand function resulting from task-specific training. Other work has shown similar shifts in cortical activation and an enlargement of ipsilesional motor map representation following various motor rehabilitation programs including CIMT that involves forced-use of the hemiparetic arm [103, 154, 155, 174, 175]. Recent work employing robotic upper-extremity training exhibited changes in EEG coherence between ipsilesional primary motor, premotor [176], and bilateral primary sensory areas [156]. Specifically, heightened coherence in the high frequency beta band (defined as 20–30 Hz by Wu et al. [176] and 24–33 Hz by Pellegrino et al. [156]) correlated with upper-extremity motor function improvement. Together, these results reinforce previous work showing associations between motor system function and the beta frequency band [135, 177]. Additionally, enhanced resting-state fMRI network connectivity involving supplementary and bilateral motor cortices and visuospatial areas with the cerebellum and association areas also correlated with gains in upper-extremity function following robotic and brain-computer interface-led upper-extremity training [158].
Due to the high frequency of motor-related impairments after stroke and their impact on overall post-stroke disability, a large portion of rehabilitation literature focuses on treatment of motor deficit. Nonetheless, repetitive TMS [178] and behavioral training [179] in individuals with post-stroke hemineglect resulted in improvements in spatial attention and neglect tasks. Accompanying these behavioral improvements were increases in bilateral white matter integrity and cortical activation in structures and areas associated with visual attention. Pilot work in patients with aphasia also demonstrated comparable increases in cortical activity in language-specific areas following a 2-week language rehabilitation program [153]. Collectively, these findings illustrate domain-specific structural and functional changes following targeted interventions. The ability of restorative therapies to exert both behavioral and neuroplastic change strengthens the potential to translate these therapies to clinical practice.
Brain Repair and Treatment Considerations
Timing of Treatment Delivery
Many studies examining therapeutic-induced mechanisms of recovery occur during the chronic phase. In a rodent stroke model, Clarkson and colleagues [180] found that administration of AMPA receptor agonists several days after stroke enhanced stroke-affected forelimb use, whereas earlier administration adversely affected recovery. These findings provide evidence that neural targets relevant to repair at one timepoint may not be relevant at a later timepoint.
Biernaskie et al. [181] provided a similar message. They found that introducing enriched rehabilitation 5 days after experimental stroke in rodents improved behavioral outcomes, possibly on the basis of enhanced dendritic growth within undamaged motor cortex. However, the same intervention introduced 30 days after stroke had no effect; introduction 14 days after stroke had an intermediate effect.
Because treatment effects vary based on their timeframe of delivery, one cannot simply extrapolate intervention findings from a chronic stroke population to an acute stroke population. Relatedly, great debate surrounds the timing of therapy initiation. Early commencement of CIMT in a rodent stroke model led to an exacerbation of neural injury [182]. However, others have found enhanced expression of growth-related proteins and dendritic growth in the ipsilesional hemisphere and improved behavioral outcomes following early vs. late CIMT [183] and reaching training [181] in rodents.
Similar CIMT investigation in humans also demonstrates variable findings. The Extremity Constraint-Induced Therapy Evaluation (EXCITE) trial was a prospective, single-blind, randomized, multisite clinical trial that compared a 2-week CIMT program to customary care in 222 enrolled individuals with moderate motor arm impairment resulting from stroke 3–9 months earlier [184]. Subjects receiving CIMT demonstrated a significant improvement in both primary outcome measures: a 52 % reduction in time to complete tasks (Wolf Motor Function Test) and a 76–77 % increase in quantity and quality of stroke-affected arm movement (Motor Activity Log). These improvements were significantly greater than those observed for the control group receiving customary care and persisted for 1 year. A related study from the EXCITE trial compared two delivery timeframes of the same 2-week CIMT program [185]. Subjects receiving early (3–9 months post-stroke) and delayed (15–21 months post-stroke) CIMT demonstrated improvements in the Wolf Motor Function Test and Motor Activity Log from pretest to 12 months following CIMT administration. However, the early CIMT group exhibited a significantly greater amount of improvement than the delayed CIMT group. These group differences were not significant at long-term follow-up (24 months after study enrollment). In a smaller-scale comparison of early vs. late CIMT, individuals receiving early (<9 months post-stroke) CIMT demonstrated greater behavioral improvement of the stroke-affected upper-extremity compared to those receiving late (>12 months post-stroke) CIMT. Yet, those receiving late CIMT showed greater changes in cortical reorganization as assessed by positional shifts in TMS motor maps [186]. The consensus from these studies is that early rehabilitation is safe and preferable to late onset therapy.
Treatment Dosage
Treatment dosage (i.e., frequency, duration, and intensity) also influences functional recovery. The relationship between treatment dosage and functional improvement is not straightforward. Restated, more does not always equate to better, and research in post-stroke motor [187] and language [188] function confirm this assertion. The VECTORS study randomized subjects with acute stroke to traditional upper-extremity therapy, dose-matched CIMT, or high-intensity CIMT [187]. All groups demonstrated positive recovery and, importantly, no anatomical MRI evidence of lesion enlargement. However, participants randomized to the high-intensity CIMT demonstrated less motor improvement at 3 months post-stroke compared to the other groups. In a related study examining treatment dosage, participants receiving aphasia rehabilitation in a distributed (6 h per week for 8 weeks) vs. intensive (16 h per week for 3 weeks) schedule demonstrated significantly greater improvements immediately after therapy and at 1 month follow-up. Additional work is necessary to examine associated structural and functional brain changes with varying therapeutic dosages.
Severity of Baseline Impairment
Differences in baseline functional status among subjects can impact the informative value of brain mapping in discerning underlying, therapeutic-induced recovery mechanisms. Könönen et al. [155] observed greater increases in sensorimotor cortex activation following CIMT among subjects possessing poorer hand motor behavior at baseline. These findings parallel previous work [98] illustrating greater supplementary motor cortex activation following CIMT in participants with diminished corticospinal tract integrity. Differences in baseline functional status may therefore influence subsequent patterns of therapeutic-driven neurological reorganization and may account for discrepancies in the literature regarding the efficacy of certain therapies and/or drugs. An overwhelming amount of post-stroke intervention studies include fairly well-recovered individuals. However, as the above studies indicate, expanding interventional studies to include participants with severe impairment or poor functional recovery is necessary toward our understanding of therapy-induced mechanisms of recovery.
The Role of Biomarkers
Biomarkers are measurements that demonstrate strong associations to disease state and progression [189]. For example, HIV RNA levels serve as a marker for AIDS and thyroid stimulating hormone concentration acts a marker for hyper/hypothyroidism. A biomarker might also be conceptualized as providing correlative behavior in a cross-sectional manner, as predicting future behavioral course, or as being measured serially in parallel with behavioral observations. A stroke biomarker, therefore, signifies an underlying brain state event linked to behavioral status or to recovery and behavioral change [190]. Examples of stroke biomarkers include measures of structure and function and genetic measures (Table 2). Past work has shown corticospinal tract injury to be predictive of spontaneous motor recovery [191] and treatment-induced motor recovery [22]. The implementation of biomarkers in stroke rehabilitation would address several existing challenges in the field of stroke. One challenge is to understand and control the amount of heterogeneity between patients with regards to functional recovery and its response to therapeutic intervention. A second challenge is that behavioral-based stroke measures commonly used in the hospital and clinic settings likely do not fully capture post-stroke neurological change and functional improvement [137]. Biomarkers combined with well-established behavioral measurements provide a more complete account of post-stroke brain change.
Though there are no established biomarkers in stroke recovery, there are several potential examples in domains of language and motor function. For instance, Marchina and colleagues [192] found that the volume of stroke-related damage (i.e., lesion load) to the left arcuate fasciculus predicted speech impairment. Additional work has also shown right arcuate fasciculus volume predictive of language recovery following left hemisphere stroke [193]. Blicher et al. [151] found significant correlations between behavioral improvement of the stroke-affected hand and changes in the GABA:creatine ratio in primary motor cortex of individuals 3–12 months post-stroke participating in a CIMT program. Decreases in the GABA:creatine ratio were associated with greater gains in motor function. Additional work is warranted to substantiate these findings. Other examples of potential stroke biomarkers include total infarct volume [194], white matter tract injury [20–22, 137, 195], cortical activation [42, 52, 91, 137, 174, 196, 197] and connectivity [136–138, 144, 146, 176, 198], and genetic polymorphisms derived from simple blood tests [15, 16, 199]. These measures may serve an important role in guiding treatment, stratifying subjects in intervention studies, and ultimately predicting functional outcome and response to therapy. Future research is necessary to confirm the reliability and validity of potential stroke biomarkers.
Difficulty associated with distinguishing cellular and molecular mechanisms of spontaneous stroke recovery in humans is an additional challenge that may limit the identification and accessibility of stroke biomarkers in humans. Brain mapping and blood analysis will continue to guide the development of human stroke biomarkers; however, future advancements in the capability of probing the human brain will likely uncover additional potential biomarkers.
Summary and Conclusions
Destruction of the neural environment following stroke propels a series of spontaneous recovery mechanisms at the cellular, molecular, and systems levels. These mechanisms are often compensatory and incomplete since many individuals continue to endure persistent disability years following their stroke. The heterogeneity of stroke has spurred the development of numerous restorative therapies that harness neuroplasticity [26] to reinstate activity in injured but surviving areas to ultimately improve motor, sensory, language, and cognitive impairments. Often, the mechanisms underlying these therapies rely on similar mechanisms as observed in spontaneous recovery. Several factors such as time of delivery, dosage, and severity of baseline impairment likely influence the effects of restorative therapies. Finally, identifying human stroke biomarkers will enhance clinical and research practices and result in greater insight into functional recovery mechanisms.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi:10.1161/01.cir.0000441139.02102.80.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220.
Rathore SS, Hinn AR, Cooper LS, Tyroler HA, Rosamond WD. Characterization of incident stroke signs and symptoms: findings from the atherosclerosis risk in communities study. Stroke. 2002;33(11):2718–21.
Kwakkel G, Kollen BJ, van der Grond J, Prevo AJ. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke. 2003;34(9):2181–6. doi:10.1161/01.str.0000087172.16305.cd.
Kwakkel G, Kollen BJ. Predicting activities after stroke: what is clinically relevant? Int J Stroke. 2013;8(1):25–32. doi:10.1111/j.1747-4949.2012.00967.x.
Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Recovery of walking function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995;76(1):27–32.
Nakayama H, Jorgensen HS, Raaschou HO, Olsen TS. Recovery of upper extremity function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil. 1994;75(4):394–8.
Hier DB, Mondlock J, Caplan LR. Recovery of behavioral abnormalities after right hemisphere stroke. Neurology. 1983;33(3):345–50.
Cassidy TP, Lewis S, Gray CS. Recovery from visuospatial neglect in stroke patients. J Neurol Neurosurg Psychiatry. 1998;64(4):555–7.
Pedersen PM, Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Impaired orientation in acute stroke: frequency, determinants, and time-course of recovery. The Copenhagen Stroke Study. Cerebrovasc Dis. 1998;8(2):90–6.
Desmond DW, Moroney JT, Sano M, Stern Y. Recovery of cognitive function after stroke. Stroke. 1996;27(10):1798–803.
Wade DT, Parker V, Langton HR. Memory disturbance after stroke: frequency and associated losses. Int Rehabil Med. 1986;8(2):60–4.
Kertesz A, McCabe P. Recovery patterns and prognosis in aphasia. Brain. 1977;100(Pt 1):1–18.
Pedersen PM, Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Aphasia in acute stroke: incidence, determinants, and recovery. Ann Neurol. 1995;38(4):659–66. doi:10.1002/ana.410380416.
Kleim JA, Chan S, Pringle E, Schallert K, Procaccio V, Jimenez R, et al. BDNF val66met polymorphism is associated with modified experience-dependent plasticity in human motor cortex. Nat Neurosci. 2006;9(6):735–7.
Cramer SC, Procaccio V. Correlation between genetic polymorphisms and stroke recovery: analysis of the GAIN Americas and GAIN International Studies. Eur J Neurol. 2012;19(5):718–24. doi:10.1111/j.1468-1331.2011.03615.x.
Helm EE, Tyrell CM, Pohlig RT, Brady LD, Reisman DS. The presence of a single-nucleotide polymorphism in the BDNF gene affects the rate of locomotor adaptation after stroke. Exp Brain Res. 2015. doi:10.1007/s00221-015-4465-8.
Chang EY, Chang EH, Cragg S, Cramer SC. Predictors of gains during inpatient rehabilitation in patients with stroke—a review. Crit Rev Phys Rehabil Med. 2013;25(3-4):203–21. doi:10.1615/CritRevPhysRehabilMed.2013008120.
Hillis AE, Barker PB, Wityk RJ, Aldrich EM, Restrepo L, Breese EL, et al. Variability in subcortical aphasia is due to variable sites of cortical hypoperfusion. Brain Lang. 2004;89(3):524–30. doi:10.1016/j.bandl.2004.01.007.
Lindenberg R, Renga V, Zhu LL, Betzler F, Alsop D, Schlaug G. Structural integrity of corticospinal motor fibers predicts motor impairment in chronic stroke. Neurology. 2010;74(4):280–7. doi:10.1212/WNL.0b013e3181ccc6d9.
Zhu LL, Lindenberg R, Alexander MP, Schlaug G. Lesion load of the corticospinal tract predicts motor impairment in chronic stroke. Stroke; J Cerebral Circ. 2010;41(5):910–5. doi:10.1161/STROKEAHA.109.577023.
Riley JD, Le V, Der-Yeghiaian L, See J, Newton JM, Ward NS, et al. Anatomy of stroke injury predicts gains from therapy. Stroke. 2011;42(2):421–6. doi:10.1161/strokeaha.110.599340.
Cramer SC. Repairing the human brain after stroke. II. Restorative therapies. Ann Neurol. 2008;63(5):549–60. doi:10.1002/ana.21412.
Lo EH. A new penumbra: transitioning from injury into repair after stroke. Nat Med. 2008;14(5):497–500.
Astrup J, Siesjo BK, Symon L. Thresholds in cerebral ischemia—the ischemic penumbra. Stroke. 1981;12(6):723–5.
Cramer SC, Sur M, Dobkin BH, O’Brien C, Sanger TD, Trojanowski JQ, et al. Harnessing neuroplasticity for clinical applications. Brain. 2011;134(Pt 6):1591–609. doi:10.1093/brain/awr039.
Overman JJ, Carmichael ST. Plasticity in the injured brain: more than molecules matter. Neuroscientist. 2014;20(1):15–28. doi:10.1177/1073858413491146.
Carmichael ST. Cellular and molecular mechanisms of neural repair after stroke: making waves. Ann Neurol. 2006;59(5):735–42. doi:10.1002/ana.20845.
Murphy TH, Corbett D. Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci. 2009;10(12):861–72.
Jones TA, Kleim JA, Greenough WT. Synaptogenesis and dendritic growth in the cortex opposite unilateral sensorimotor cortex damage in adult rats: a quantitative electron microscopic examination. Brain Res. 1996;733(1):142–8.
Jones TA, Schallert T. Overgrowth and pruning of dendrites in adult rats recovering from neocortical damage. Brain Res. 1992;581(1):156–60.
Zhang RL, Zhang ZG, Chopp M. Ischemic stroke and neurogenesis in the subventricular zone. Neuropharmacology. 2008;55(3):345–52. doi:10.1016/j.neuropharm.2008.05.027.
Ding G, Jiang Q, Li L, Zhang L, Zhang ZG, Ledbetter KA, et al. Magnetic resonance imaging investigation of axonal remodeling and angiogenesis after embolic stroke in sildenafil-treated rats. J Cereb Blood Flow Metab. 2008;28(8):1440–8. doi:10.1038/jcbfm.2008.33.
Seevinck PR, Deddens LH, Dijkhuizen RM. Magnetic resonance imaging of brain angiogenesis after stroke. Angiogenesis. 2010;13(2):101–11. doi:10.1007/s10456-010-9174-0.
Teng H, Zhang ZG, Wang L, Zhang RL, Zhang L, Morris D, et al. Coupling of angiogenesis and neurogenesis in cultured endothelial cells and neural progenitor cells after stroke. J Cereb Blood Flow Metab. 2008;28(4):764–71. doi:10.1038/sj.jcbfm.9600573.
Li S, Carmichael ST. Growth-associated gene and protein expression in the region of axonal sprouting in the aged brain after stroke. Neurobiol Dis. 2006;23(2):362–73. doi:10.1016/j.nbd.2006.03.011.
Redecker C, Wang W, Fritschy JM, Witte OW. Widespread and long-lasting alterations in GABA(A)-receptor subtypes after focal cortical infarcts in rats: mediation by NMDA-dependent processes. J Cereb Blood Flow Metab. 2002;22(12):1463–75.
Que M, Schiene K, Witte OW, Zilles K. Widespread up-regulation of N-methyl-D-aspartate receptors after focal photothrombotic lesion in rat brain. Neurosci Lett. 1999;273(2):77–80.
Dancause N, Barbay S, Frost SB, Plautz EJ, Chen D, Zoubina EV, et al. Extensive cortical rewiring after brain injury. J Neurosci. 2005;25(44):10167–79. doi:10.1523/jneurosci.3256-05.2005.
Sist B, Fouad K, Winship IR. Plasticity beyond peri-infarct cortex: spinal up regulation of structural plasticity, neurotrophins, and inflammatory cytokines during recovery from cortical stroke. Exp Neurol. 2014;252:47–56. doi:10.1016/j.expneurol.2013.11.019.
Lotze M, Markert J, Sauseng P, Hoppe J, Plewnia C, Gerloff C. The role of multiple contralesional motor areas for complex hand movements after internal capsular lesion. J Neurosci. 2006;26(22):6096–102. doi:10.1523/jneurosci.4564-05.2006.
Johansen-Berg H, Rushworth MF, Bogdanovic MD, Kischka U, Wimalaratna S, Matthews PM. The role of ipsilateral premotor cortex in hand movement after stroke. Proc Natl Acad Sci U S A. 2002;99(22):14518–23. doi:10.1073/pnas.222536799.
Bradnam LV, Stinear CM, Barber PA, Byblow WD. Contralesional hemisphere control of the proximal paretic upper limb following stroke. Cereb Cortex. 2012;22(11):2662–71. doi:10.1093/cercor/bhr344.
Ward NS, Brown MM, Thompson AJ, Frackowiak RS. Neural correlates of motor recovery after stroke: a longitudinal fMRI study. Brain. 2003;126(Pt 11):2476–96. doi:10.1093/brain/awg245.
Feeney DM, Baron JC. Diaschisis. Stroke. 1986;17(5):817–30.
Buchkremer-Ratzmann I, August M, Hagemann G, Witte OW. Electrophysiological transcortical diaschisis after cortical photothrombosis in rat brain. Stroke. 1996;27(6):1105–9.
Carmichael ST, Tatsukawa K, Katsman D, Tsuyuguchi N, Kornblum HI. Evolution of diaschisis in a focal stroke model. Stroke. 2004;35(3):758–63.
Pappata S, Levasseur M, Gunn RN, Myers R, Crouzel C, Syrota A, et al. Thalamic microglial activation in ischemic stroke detected in vivo by PET and [11C] PK11195. Neurology. 2000;55(7):1052–4.
Schaechter JD, Moore CI, Connell BD, Rosen BR, Dijkhuizen RM. Structural and functional plasticity in the somatosensory cortex of chronic stroke patients. Brain. 2006;129(Pt 10):2722–33. doi:10.1093/brain/awl214.
Zhang J, Meng L, Qin W, Liu N, Shi FD, Yu C. Structural damage and functional reorganization in ipsilesional m1 in well-recovered patients with subcortical stroke. Stroke. 2014;45(3):788–93. doi:10.1161/strokeaha.113.003425.
Fridman EA, Hanakawa T, Chung M, Hummel F, Leiguarda RC, Cohen LG. Reorganization of the human ipsilesional premotor cortex after stroke. Brain. 2004;127(Pt 4):747–58. doi:10.1093/brain/awh082.
Favre I, Zeffiro TA, Detante O, Krainik A, Hommel M, Jaillard A. Upper limb recovery after stroke is associated with ipsilesional primary motor cortical activity: a meta-analysis. Stroke. 2014;45(4):1077–83. doi:10.1161/strokeaha.113.003168.
Heiss WD, Thiel A. A proposed regional hierarchy in recovery of post-stroke aphasia. Brain Lang. 2006;98(1):118–23. doi:10.1016/j.bandl.2006.02.002.
Warburton E, Price CJ, Swinburn K, Wise RJ. Mechanisms of recovery from aphasia: evidence from positron emission tomography studies. J Neurol Neurosurg Psychiatry. 1999;66(2):155–61.
Corbetta M, Kincade MJ, Lewis C, Snyder AZ, Sapir A. Neural basis and recovery of spatial attention deficits in spatial neglect. Nat Neurosci. 2005;8(11):1603–10. doi:10.1038/nn1574.
Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1(8437):1106–7.
Talelli P, Greenwood RJ, Rothwell JC. Arm function after stroke: neurophysiological correlates and recovery mechanisms assessed by transcranial magnetic stimulation. Clin Neurophysiol. 2006;117(8):1641–59. doi:10.1016/j.clinph.2006.01.016.
Stinear CM, Barber PA, Smale PR, Coxon JP, Fleming MK, Byblow WD. Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain. 2007;130(Pt 1):170–80.
van Kuijk AA, Anker LC, Pasman JW, Hendriks J, van Elswijk G, Geurts ACH. Stimulus–response characteristics of motor evoked potentials and silent periods in proximal and distal upper-extremity muscles. J Electromyogr Kinesiol. 2009;19(4):574–83.
Pennisi G, Alagona G, Rapisarda G, Nicoletti F, Costanzo E, Ferri R, et al. Transcranial magnetic stimulation after pure motor stroke. Clin Neurophysiol. 2002;113(10):1536–43.
Escudero JV, Sancho J, Bautista D, Escudero M, Lopez-Trigo J. Prognostic value of motor evoked potential obtained by transcranial magnetic brain stimulation in motor function recovery in patients with acute ischemic stroke. Stroke; J Cerebral Circ. 1998;29(9):1854–9.
Traversa R, Cicinelli P, Oliveri M, Giuseppina Palmieri M, Filippi MM, Pasqualetti P, et al. Neurophysiological follow-up of motor cortical output in stroke patients. Clin Neurophysiol. 2000;111(9):1695–703. doi:10.1016/S1388-2457(00)00373-4.
Cicinelli P, Traversa R, Rossini PM. Post-stroke reorganization of brain motor output to the hand: a 2–4 month follow-up with focal magnetic transcranial stimulation. Electroencephalogr Clin Neurophysiol. 1997;105(6):438–50.
Traversa R, Cicinelli P, Bassi A, Rossini PM, Bernardi G. Mapping of motor cortical reorganization after stroke a brain stimulation study with focal magnetic pulses. Stroke. 1997;28(1):110–7.
Netz J, Lammers T, Homberg V. Reorganization of motor output in the non-affected hemisphere after stroke. Brain: J Neurol. 1997;120(Pt 9):1579–86.
Manganotti P, Patuzzo S, Cortese F, Palermo A, Smania N, Fiaschi A. Motor disinhibition in affected and unaffected hemisphere in the early period of recovery after stroke. Clin Neurophysiol. 2002;113(6):936–43.
Thickbroom GW, Byrnes ML, Archer SA, Mastaglia FL. Motor outcome after subcortical stroke: MEPs correlate with hand strength but not dexterity. Clin Neurophysiol. 2002;113(12):2025–9.
Cramer SC, Nelles G, Benson RR, Kaplan JD, Parker RA, Kwong KK, et al. A functional MRI study of subjects recovered from hemiparetic stroke. Stroke. 1997;28(12):2518–27.
Weiller C, Isensee C, Rijntjes M, Huber W, Muller S, Bier D, et al. Recovery from Wernicke’s aphasia: a positron emission tomographic study. Ann Neurol. 1995;37(6):723–32. doi:10.1002/ana.410370605.
Nelles G, Jentzen W, Bockisch A, Diener HC. Neural substrates of good and poor recovery after hemiplegic stroke: a serial PET study. J Neurol. 2011;258(12):2168–75. doi:10.1007/s00415-011-6085-y.
Frost SB, Barbay S, Friel KM, Plautz EJ, Nudo RJ. Reorganization of remote cortical regions after ischemic brain injury: a potential substrate for stroke recovery. J Neurophysiol. 2003;89(6):3205–14. doi:10.1152/jn.01143.2002.
Nair DG, Hutchinson S, Fregni F, Alexander M, Pascual-Leone A, Schlaug G. Imaging correlates of motor recovery from cerebral infarction and their physiological significance in well-recovered patients. Neuroimage. 2007;34(1):253–63. doi:10.1016/j.neuroimage.2006.09.010.
Nelles G, Spiekermann G, Jueptner M, Leonhardt G, Muller S, Gerhard H, et al. Reorganization of sensory and motor systems in hemiplegic stroke patients. A positron emission tomography study. Stroke. 1999;30(8):1510–6.
van Oers CA, Vink M, van Zandvoort MJ, van der Worp HB, de Haan EH, Kappelle LJ, et al. Contribution of the left and right inferior frontal gyrus in recovery from aphasia. a functional MRI study in stroke patients with preserved hemodynamic responsiveness. Neuroimage. 2010;49(1):885–93. doi:10.1016/j.neuroimage.2009.08.057.
Grefkes C, Ward NS. Cortical reorganization after stroke: how much and how functional? Neuroscientist. 2014;20(1):56–70. doi:10.1177/1073858413491147.
Buetefisch CM. Role of the contralesional hemisphere in post-stroke recovery of upper extremity motor function. Front Neurol. 2015;6:214. doi:10.3389/fneur.2015.00214.
Bestmann S, Swayne O, Blankenburg F, Ruff CC, Teo J, Weiskopf N, et al. The role of contralesional dorsal premotor cortex after stroke as studied with concurrent TMS-fMRI. J Neurosci. 2010;30(36):11926–37. doi:10.1523/jneurosci.5642-09.2010.
Ackerley SJ, Stinear CM, Barber PA, Byblow WD. Combining theta burst stimulation with training after subcortical stroke. Stroke. 2010;41(7):1568–72. doi:10.1161/strokeaha.110.583278.
Schaechter JD, Perdue KL. Enhanced cortical activation in the contralesional hemisphere of chronic stroke patients in response to motor skill challenge. Cereb Cortex. 2008;18(3):638–47. doi:10.1093/cercor/bhm096.
Mohapatra S, Harrington R, Chan E, Dromerick AW, Breceda EY, Harris-Love M. Role of contralesional hemisphere in paretic arm reaching in patients with severe arm paresis due to stroke: a preliminary report. Neurosci Lett. 2016;617:52–8. doi:10.1016/j.neulet.2016.02.004.
Kim DY, Lim JY, Kang EK, You DS, Oh MK, Oh BM, et al. Effect of transcranial direct current stimulation on motor recovery in patients with subacute stroke. Am J Phys Med Rehabil. 2010;89(11):879–86. doi:10.1097/PHM.0b013e3181f70aa7.
Grefkes C, Nowak DA, Wang LE, Dafotakis M, Eickhoff SB, Fink GR. Modulating cortical connectivity in stroke patients by rTMS assessed with fMRI and dynamic causal modeling. Neuroimage. 2010;50(1):233–42. doi:10.1016/j.neuroimage.2009.12.029.
Fregni F, Boggio PS, Mansur CG, Wagner T, Ferreira MJ, Lima MC, et al. Transcranial direct current stimulation of the unaffected hemisphere in stroke patients. Neuroreport. 2005;16(14):1551–5.
Kokotilo KJ, Eng JJ, McKeown MJ, Boyd LA. Greater activation of secondary motor areas is related to less arm use after stroke. Neurorehabil Neural Repair. 2010;24(1):78–87. doi:10.1177/1545968309345269.
Calautti C, Naccarato M, Jones PS, Sharma N, Day DD, Carpenter AT, et al. The relationship between motor deficit and hemisphere activation balance after stroke: a 3T fMRI study. NeuroImage. 2007;34(1):322–31.
Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature. 2001;412(6843):150–7.
Irlbacher K, Brocke J, Mechow JV, Brandt SA. Effects of GABA(A) and GABA(B) agonists on interhemispheric inhibition in man. Clin Neurophysiol. 2007;118(2):308–16.
Palmer LM, Schulz JM, Murphy SC, Ledergerber D, Murayama M, Larkum ME. The cellular basis of GABA(B)-mediated interhemispheric inhibition. Science. 2012;335(6071):989–93.
Daskalakis ZJ, Christensen BK, Fitzgerald PB, Roshan L, Chen R. The mechanisms of interhemispheric inhibition in the human motor cortex. J Physiol. 2002;543(1):317–26.
Ferbert A, Priori A, Rothwell JC, Day BL, Colebatch JG, Marsden CD. Interhemispheric inhibition of the human motor cortex. J Physiol. 1992;453:525–46.
Ward NS, Brown MM, Thompson AJ, Frackowiak RS. The influence of time after stroke on brain activations during a motor task. Ann Neurol. 2004;55(6):829–34. doi:10.1002/ana.20099.
Chollet F, DiPiero V, Wise RJ, Brooks DJ, Dolan RJ, Frackowiak RS. The functional anatomy of motor recovery after stroke in humans: a study with positron emission tomography. Ann Neurol. 1991;29(1):63–71. doi:10.1002/ana.410290112.
Carey JR, Kimberley TJ, Lewis SM, Auerbach EJ, Dorsey L, Rundquist P, et al. Analysis of fMRI and finger tracking training in subjects with chronic stroke. Brain. 2002;125(Pt 4):773–88.
Rehme AK, Eickhoff SB, Rottschy C, Fink GR, Grefkes C. Activation likelihood estimation meta-analysis of motor-related neural activity after stroke. Neuroimage. 2012;59(3):2771–82. doi:10.1016/j.neuroimage.2011.10.023.
Ward NS, Brown MM, Thompson AJ, Frackowiak RS. Longitudinal changes in cerebral response to proprioceptive input in individual patients after stroke: an FMRI study. Neurorehabil Neural Repair. 2006;20(3):398–405. doi:10.1177/1545968306286322.
Pundik S, McCabe JP, Hrovat K, Fredrickson AE, Tatsuoka C, Feng IJ, et al. Recovery of post stroke proximal arm function, driven by complex neuroplastic bilateral brain activation patterns and predicted by baseline motor dysfunction severity. Front Hum Neurosci. 2015;9:394. doi:10.3389/fnhum.2015.00394.
Ward NS, Newton JM, Swayne OBC, Lee L, Thompson AJ, Greenwood RJ, et al. Motor system activation after subcortical stroke depends on corticospinal system integrity. Brain. 2006;129(3):809–19.
Hamzei F, Liepert J, Dettmers C, Weiller C, Rijntjes M. Two different reorganization patterns after rehabilitative therapy: an exploratory study with fMRI and TMS. NeuroImage. 2006;31(2):710–20.
Wei W, Bai L, Wang J, Dai R, Tong RK, Zhang Y, et al. A longitudinal study of hand motor recovery after sub-acute stroke: a study combined FMRI with diffusion tensor imaging. PLoS One. 2013;8(5):e64154. doi:10.1371/journal.pone.0064154.
Zemke AC, Heagerty PJ, Lee C, Cramer SC. Motor cortex organization after stroke is related to side of stroke and level of recovery. Stroke. 2003;34(5):e23–8. doi:10.1161/01.str.0000065827.35634.5e.
Cramer SC, Crafton KR. Somatotopy and movement representation sites following cortical stroke. Exp Brain Res. 2006;168(1-2):25–32. doi:10.1007/s00221-005-0082-2.
Cramer SC, Moore CI, Finklestein SP, Rosen BR. A pilot study of somatotopic mapping after cortical infarct. Stroke. 2000;31(3):668–71.
Johansen-Berg H, Dawes H, Guy C, Smith SM, Wade DT, Matthews PM. Correlation between motor improvements and altered fMRI activity after rehabilitative therapy. Brain. 2002;125(Pt 12):2731–42.
Boroojerdi B, Diefenbach K, Ferbert A. Transcallosal inhibition in cortical and subcortical cerebral vascular lesions. J Neurol Sci. 1996;144(1):160–70.
Li J-Y, Lai P-H, Chen R. Transcallosal inhibition in patients with callosal infarction. J Neurophysiol. 2013;109(3):659–65.
Murase N, Duque J, Mazzocchio R, Cohen L. Influence of interhemispheric interactions on motor function in chronic stroke. Ann Neurol. 2004;55(3):400–9.
Duque J, Hummel F, Celnik P, Murase N, Mazzocchio R, Cohen L. Transcallosal inhibition in chronic subcortical stroke. NeuroImage. 2005;28(4):940–6.
Cicinelli P, Pasqualetti P, Zaccagnini M, Traversa R, Oliveri M, Rossini PM. Interhemispheric asymmetries of motor cortex excitability in the postacute stroke stage: a paired-pulse transcranial magnetic stimulation study. Stroke. 2003;34(11):2653–8.
Butefisch CM, Wessling M, Netz J, Seitz RJ, Homberg V. Relationship between interhemispheric inhibition and motor cortex excitability in subacute stroke patients. Neurorehab Neural Repair. 2008;22(1):4–21.
Shimizu T, Hosaki A, Hino T, Sato M, Komori T, Hirai S, et al. Motor cortical disinhibition in the unaffected hemisphere after unilateral cortical stroke. Brain. 2002;125(8):1896–907.
Scholz VH, Flaherty AW, Kraft E, Keltner JR, Kwong KK, Chen YI, et al. Laterality, somatotopy and reproducibility of the basal ganglia and motor cortex during motor tasks. Brain Res. 2000;879(1-2):204–15.
Morecraft RJ, Herrick JL, Stilwell-Morecraft KS, Louie JL, Schroeder CM, Ottenbacher JG, et al. Localization of arm representation in the corona radiata and internal capsule in the non-human primate. Brain. 2002;125(Pt 1):176–98.
Maillard L, Ishii K, Bushara K, Waldvogel D, Schulman AE, Hallett M. Mapping the basal ganglia: fMRI evidence for somatotopic representation of face, hand, and foot. Neurology. 2000;55(3):377–83.
Xerri C, Merzenich MM, Peterson BE, Jenkins W. Plasticity of primary somatosensory cortex paralleling sensorimotor skill recovery from stroke in adult monkeys. J Neurophysiol. 1998;79(4):2119–48.
Nudo RJ, Milliken GW. Reorganization of movement representations in primary motor cortex following focal ischemic infarcts in adult squirrel monkeys. J Neurophysiol. 1996;75(5):2144–9.
Dancause N, Barbay S, Frost SB, Zoubina EV, Plautz EJ, Mahnken JD, et al. Effects of small ischemic lesions in the primary motor cortex on neurophysiological organization in ventral premotor cortex. J Neurophysiol. 2006;96(6):3506–11. doi:10.1152/jn.00792.2006.
Plautz EJ, Barbay S, Frost SB, Friel KM, Dancause N, Zoubina EV, et al. Post-infarct cortical plasticity and behavioral recovery using concurrent cortical stimulation and rehabilitative training: a feasibility study in primates. Neurol Res. 2003;25(8):801–10. doi:10.1179/016164103771953880.
Bastings EP, Greenberg JP, Good DC. Hand motor recovery after stroke: a transcranial magnetic stimulation mapping study of motor output areas and their relation to functional status. Neurorehabil Neural Repair. 2002;16(3):275–82.
Rossini PM, Caltagirone C, Castriota-Scanderbeg A, Cicinelli P, Del Gratta C, Demartin M, et al. Hand motor cortical area reorganization in stroke: a study with fMRI, MEG and TCS maps. Neuroreport. 1998;9(9):2141–6.
Delvaux V, Alagona G, Gerard P, De Pasqua V, Pennisi G, de Noordhout AM. Post-stroke reorganization of hand motor area: a 1-year prospective follow-up with focal transcranial magnetic stimulation. Clin Neurophysiol. 2003;114(7):1217–25.
Liepert J, Bauder H, Miltner WHR, Taub E, Weiller C. Treatment-induced cortical reorganization after stroke in humans. Stroke. 2000;31(6):1210–6.
Jaillard A, Martin CD, Garambois K, Lebas JF, Hommel M. Vicarious function within the human primary motor cortex? a longitudinal fMRI stroke study. Brain. 2005;128(Pt 5):1122–38. doi:10.1093/brain/awh456.
Schaechter JD, Perdue KL, Wang R. Structural damage to the corticospinal tract correlates with bilateral sensorimotor cortex reorganization in stroke patients. Neuroimage. 2008;39(3):1370–82. doi:10.1016/j.neuroimage.2007.09.071.
Weiller C, Ramsay SC, Wise RJ, Friston KJ, Frackowiak RS. Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Ann Neurol. 1993;33(2):181–9. doi:10.1002/ana.410330208.
Tombari D, Loubinoux I, Pariente J, Gerdelat A, Albucher JF, Tardy J, et al. A longitudinal fMRI study: in recovering and then in clinically stable sub-cortical stroke patients. Neuroimage. 2004;23(3):827–39. doi:10.1016/j.neuroimage.2004.07.058.
Calautti C, Leroy F, Guincestre JY, Baron JC. Displacement of primary sensorimotor cortex activation after subcortical stroke: a longitudinal PET study with clinical correlation. Neuroimage. 2003;19(4):1650–4.
Pineiro R, Pendlebury S, Johansen-Berg H, Matthews PM. Functional MRI detects posterior shifts in primary sensorimotor cortex activation after stroke: evidence of local adaptive reorganization? Stroke. 2001;32(5):1134–9.
Newton JM, Ward NS, Parker GJ, Deichmann R, Alexander DC, Friston KJ, et al. Non-invasive mapping of corticofugal fibres from multiple motor areas—relevance to stroke recovery. Brain. 2006;129(Pt 7):1844–58. doi:10.1093/brain/awl106.
Schaechter JD, Fricker ZP, Perdue KL, Helmer KG, Vangel MG, Greve DN, et al. Microstructural status of ipsilesional and contralesional corticospinal tract correlates with motor skill in chronic stroke patients. Hum Brain Mapp. 2009;30(11):3461–74. doi:10.1002/hbm.20770.
Schulz R, Park CH, Boudrias MH, Gerloff C, Hummel FC, Ward NS. Assessing the integrity of corticospinal pathways from primary and secondary cortical motor areas after stroke. Stroke. 2012;43(8):2248–51. doi:10.1161/strokeaha.112.662619.
Schulz R, Braass H, Liuzzi G, Hoerniss V, Lechner P, Gerloff C, et al. White matter integrity of premotor-motor connections is associated with motor output in chronic stroke patients. Neuroimage Clin. 2015;7:82–6. doi:10.1016/j.nicl.2014.11.006.
Friston KJ. Functional and effective connectivity: a review. Brain Connect. 2011;1(1):13–36. doi:10.1089/brain.2011.0008.
Corbetta M. Functional connectivity and neurological recovery. Dev Psychobiol. 2012;54(3):239–53. doi:10.1002/dev.20507.
Grefkes C, Fink GR. Connectivity-based approaches in stroke and recovery of function. Lancet Neurol. 2014;13(2):206–16. doi:10.1016/s1474-4422(13)70264-3.
Pfurtscheller G, Stancak Jr A, Neuper C. Post-movement beta synchronization. A correlate of an idling motor area? Electroencephalogr Clin Neurophysiol. 1996;98(4):281–93.
Carter AR, Astafiev SV, Lang CE, Connor LT, Rengachary J, Strube MJ, et al. Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Ann Neurol. 2010;67(3):365–75. doi:10.1002/ana.21905.
Burke Quinlan E, Dodakian L, See J, McKenzie A, Le V, Wojnowicz M, et al. Neural function, injury, and stroke subtype predict treatment gains after stroke. Ann Neurol. 2015;77(1):132–45. doi:10.1002/ana.24309.
Wadden KP, Woodward TS, Metzak PD, Lavigne KM, Lakhani B, Auriat AM, et al. Compensatory motor network connectivity is associated with motor sequence learning after subcortical stroke. Behav Brain Res. 2015;286:136–45. doi:10.1016/j.bbr.2015.02.054.
Golestani AM, Tymchuk S, Demchuk A, Goodyear BG. Longitudinal evaluation of resting-state FMRI after acute stroke with hemiparesis. Neurorehabil Neural Repair. 2013;27(2):153–63. doi:10.1177/1545968312457827.
Bannister LC, Crewther SG, Gavrilescu M, Carey LM. Improvement in touch sensation after stroke is associated with resting functional connectivity changes. Front Neurol. 2015;6:165. doi:10.3389/fneur.2015.00165.
Carter AR, Patel KR, Astafiev SV, Snyder AZ, Rengachary J, Strube MJ, et al. Upstream dysfunction of somatomotor functional connectivity after corticospinal damage in stroke. Neurorehabil Neural Repair. 2012;26(1):7–19. doi:10.1177/1545968311411054.
Liu J, Qin W, Zhang J, Zhang X, Yu C. Enhanced interhemispheric functional connectivity compensates for anatomical connection damages in subcortical stroke. Stroke. 2015;46(4):1045–51. doi:10.1161/strokeaha.114.007044.
van Meer MP, van der Marel K, Wang K, Otte WM, El Bouazati S, Roeling TA, et al. Recovery of sensorimotor function after experimental stroke correlates with restoration of resting-state interhemispheric functional connectivity. J Neurosci. 2010;30(11):3964–72. doi:10.1523/jneurosci.5709-09.2010.
Nicolo P, Rizk S, Magnin C, Pietro MD, Schnider A, Guggisberg AG. Coherent neural oscillations predict future motor and language improvement after stroke. Brain. 2015;138(Pt 10):3048–60. doi:10.1093/brain/awv200.
Mikell CB, Banks GP, Frey HP, Youngerman BE, Nelp TB, Karas PJ, et al. Frontal networks associated with command following after hemorrhagic stroke. Stroke. 2015;46(1):49–57. doi:10.1161/strokeaha.114.007645.
Dubovik S, Pignat JM, Ptak R, Aboulafia T, Allet L, Gillabert N, et al. The behavioral significance of coherent resting-state oscillations after stroke. Neuroimage. 2012;61(1):249–57. doi:10.1016/j.neuroimage.2012.03.024.
Gerloff C, Bushara K, Sailer A, Wassermann EM, Chen R, Matsuoka T, et al. Multimodal imaging of brain reorganization in motor areas of the contralesional hemisphere of well recovered patients after capsular stroke. Brain. 2006;129(Pt 3):791–808. doi:10.1093/brain/awh713.
Rehme AK, Grefkes C. Cerebral network disorders after stroke: evidence from imaging-based connectivity analyses of active and resting brain states in humans. J Physiol. 2013;591(Pt 1):17–31. doi:10.1113/jphysiol.2012.243469.
Friston KJ, Harrison L, Penny W. Dynamic causal modelling. Neuroimage. 2003;19(4):1273–302.
Rehme AK, Eickhoff SB, Wang LE, Fink GR, Grefkes C. Dynamic causal modeling of cortical activity from the acute to the chronic stage after stroke. Neuroimage. 2011;55(3):1147–58. doi:10.1016/j.neuroimage.2011.01.014.
Blicher JU, Near J, Naess-Schmidt E, Stagg CJ, Johansen-Berg H, Nielsen JF, et al. GABA levels are decreased after stroke and GABA changes during rehabilitation correlate with motor improvement. Neurorehabil Neural Repair. 2015;29(3):278–86. doi:10.1177/1545968314543652.
Dodakian L, Campbell Stewart J, Cramer SC. Motor imagery during movement activates the brain more than movement alone after stroke: a pilot study. J Rehabil Med. 2014;46(9):843–8. doi:10.2340/16501977-1844.
Mattioli F, Ambrosi C, Mascaro L, Scarpazza C, Pasquali P, Frugoni M, et al. Early aphasia rehabilitation is associated with functional reactivation of the left inferior frontal gyrus: a pilot study. Stroke. 2014;45(2):545–52. doi:10.1161/strokeaha.113.003192.
Hubbard IJ, Carey LM, Budd TW, Levi C, McElduff P, Hudson S, et al. A randomized controlled trial of the effect of early upper-limb training on stroke recovery and brain activation. Neurorehabil Neural Repair. 2015;29(8):703–13. doi:10.1177/1545968314562647.
Kononen M, Tarkka IM, Niskanen E, Pihlajamaki M, Mervaala E, Pitkanen K, et al. Functional MRI and motor behavioral changes obtained with constraint-induced movement therapy in chronic stroke. Eur J Neurol. 2012;19(4):578–86. doi:10.1111/j.1468-1331.2011.03572.x.
Pellegrino G, Tomasevic L, Tombini M, Assenza G, Bravi M, Sterzi S, et al. Inter-hemispheric coupling changes associate with motor improvements after robotic stroke rehabilitation. Restor Neurol Neurosci. 2012;30(6):497–510. doi:10.3233/rnn-2012-120227.
Sale P, Infarinato F, Del Percio C, Lizio R, Babiloni C, Foti C, et al. Electroencephalographic markers of robot-aided therapy in stroke patients for the evaluation of upper limb rehabilitation. Int J Rehabil Res. 2015;38(4):294–305. doi:10.1097/mrr.0000000000000125.
Varkuti B, Guan C, Pan Y, Phua KS, Ang KK, Kuah CW, et al. Resting state changes in functional connectivity correlate with movement recovery for BCI and robot-assisted upper-extremity training after stroke. Neurorehabil Neural Repair. 2013;27(1):53–62. doi:10.1177/1545968312445910.
Di Lazzaro V, Rothwell JC, Talelli P, Capone F, Ranieri F, Wallace AC, et al. Inhibitory theta burst stimulation of affected hemisphere in chronic stroke: a proof of principle, sham-controlled study. Neurosci Lett. 2013;553:148–52. doi:10.1016/j.neulet.2013.08.013.
Khedr EM, Ahmed MA, Fathy N, Rothwell JC. Therapeutic trial of repetitive transcranial magnetic stimulation after acute ischemic stroke. Neurology. 2005;65(3):466–8. doi:10.1212/01.wnl.0000173067.84247.36.
Hsu WY, Cheng CH, Liao KK, Lee IH, Lin YY. Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke. 2012;43(7):1849–57. doi:10.1161/strokeaha.111.649756.
Scheidtmann K, Fries W, Muller F, Koenig E. Effect of levodopa in combination with physiotherapy on functional motor recovery after stroke: a prospective, randomised, double-blind study. Lancet. 2001;358(9284):787–90. doi:10.1016/s0140-6736(01)05966-9.
Crisostomo EA, Duncan PW, Propst M, Dawson DV, Davis JN. Evidence that amphetamine with physical therapy promotes recovery of motor function in stroke patients. Ann Neurol. 1988;23(1):94–7. doi:10.1002/ana.410230117.
Chollet F, Tardy J, Albucher JF, Thalamas C, Berard E, Lamy C, et al. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): a randomised placebo-controlled trial. Lancet Neurol. 2011;10(2):123–30. doi:10.1016/s1474-4422(10)70314-8.
Brenneman MM, Hylin MJ, Corwin JV. The time-dependent and persistent effects of amphetamine treatment upon recovery from hemispatial neglect in rats. Behav Brain Res. 2015;293:153–61. doi:10.1016/j.bbr.2015.07.032.
Chen J, Li Y, Katakowski M, Chen X, Wang L, Lu D, et al. Intravenous bone marrow stromal cell therapy reduces apoptosis and promotes endogenous cell proliferation after stroke in female rat. J Neurosci Res. 2003;73(6):778–86. doi:10.1002/jnr.10691.
Bang OY, Lee JS, Lee PH, Lee G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol. 2005;57(6):874–82. doi:10.1002/ana.20501.
Kawamata T, Dietrich WD, Schallert T, Gotts JE, Cocke RR, Benowitz LI, et al. Intracisternal basic fibroblast growth factor enhances functional recovery and up-regulates the expression of a molecular marker of neuronal sprouting following focal cerebral infarction. Proc Natl Acad Sci U S A. 1997;94(15):8179–84.
Corbetta D, Sirtori V, Castellini G, Moja L, Gatti R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Database Syst Rev. 2015;10:CD004433. doi:10.1002/14651858.CD004433.pub3.
Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil Neural Repair. 2008;22(2):111–21. doi:10.1177/1545968307305457.
Mead GE, Hsieh CF, Lee R, Kutlubaev MA, Claxton A, Hankey GJ, et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database Syst Rev. 2012;11:CD009286. doi:10.1002/14651858.CD009286.pub2.
Cramer SC. An overview of therapies to promote repair of the brain after stroke. Head Neck. 2011;33 Suppl 1:S5–7. doi:10.1002/hed.21840.
Vu Q, Xie K, Eckert M, Zhao W, Cramer SC. Meta-analysis of preclinical studies of mesenchymal stromal cells for ischemic stroke. Neurology. 2014;82(14):1277–86. doi:10.1212/wnl.0000000000000278.
Laible M, Grieshammer S, Seidel G, Rijntjes M, Weiller C, Hamzei F. Association of activity changes in the primary sensory cortex with successful motor rehabilitation of the hand following stroke. Neurorehabil Neural Repair. 2012;26(7):881–8. doi:10.1177/1545968312437939.
Sawaki L, Butler AJ, Leng X, Wassenaar PA, Mohammad YM, Blanton S, et al. Constraint-induced movement therapy results in increased motor map area in subjects 3 to 9 months after stroke. Neurorehabil Neural Repair. 2008;22(5):505–13. doi:10.1177/1545968308317531.
Wu J, Quinlan EB, Dodakian L, McKenzie A, Kathuria N, Zhou RJ, et al. Connectivity measures are robust biomarkers of cortical function and plasticity after stroke. Brain. 2015;138(Pt 8):2359–69. doi:10.1093/brain/awv156.
Roopun AK, Middleton SJ, Cunningham MO, LeBeau FE, Bibbig A, Whittington MA, et al. A beta2-frequency (20–30 Hz) oscillation in nonsynaptic networks of somatosensory cortex. Proc Natl Acad Sci U S A. 2006;103(42):15646–50. doi:10.1073/pnas.0607443103.
Yang W, Liu TT, Song XB, Zhang Y, Li ZH, Cui ZH, et al. Comparison of different stimulation parameters of repetitive transcranial magnetic stimulation for unilateral spatial neglect in stroke patients. J Neurol Sci. 2015;359(1-2):219–25. doi:10.1016/j.jns.2015.08.1541.
Thimm M, Fink GR, Kust J, Karbe H, Sturm W. Impact of alertness training on spatial neglect: a behavioural and fMRI study. Neuropsychologia. 2006;44(7):1230–46. doi:10.1016/j.neuropsychologia.2005.09.008.
Clarkson AN, Overman JJ, Zhong S, Mueller R, Lynch G, Carmichael ST. AMPA receptor-induced local brain-derived neurotrophic factor signaling mediates motor recovery after stroke. J Neurosci. 2011;31(10):3766–75. doi:10.1523/jneurosci.5780-10.2011.
Biernaskie J, Chernenko G, Corbett D. Efficacy of rehabilitative experience declines with time after focal ischemic brain injury. J Neurosci. 2004;24(5):1245–54. doi:10.1523/jneurosci.3834-03.2004.
Kozlowski DA, James DC, Schallert T. Use-dependent exaggeration of neuronal injury after unilateral sensorimotor cortex lesions. J Neurosci. 1996;16(15):4776–86.
Ishida A, Misumi S, Ueda Y, Shimizu Y, Cha-Gyun J, Tamakoshi K, et al. Early constraint-induced movement therapy promotes functional recovery and neuronal plasticity in a subcortical hemorrhage model rat. Behav Brain Res. 2015;284:158–66. doi:10.1016/j.bbr.2015.02.022.
Wolf SL, Winstein CJ, Miller JP, Taub E, Uswatte G, Morris D, et al. Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA. 2006;296(17):2095–104. doi:10.1001/jama.296.17.2095.
Wolf SL, Thompson PA, Winstein CJ, Miller JP, Blanton SR, Nichols-Larsen DS, et al. The EXCITE stroke trial: comparing early and delayed constraint-induced movement therapy. Stroke. 2010;41(10):2309–15. doi:10.1161/strokeaha.110.588723.
Sawaki L, Butler AJ, Leng X, Wassenaar PA, Mohammad YM, Blanton S, et al. Differential patterns of cortical reorganization following constraint-induced movement therapy during early and late period after stroke: a preliminary study. NeuroRehabilitation. 2014;35(3):415–26. doi:10.3233/nre-141132.
Dromerick AW, Lang CE, Birkenmeier RL, Wagner JM, Miller JP, Videen TO, et al. Very Early Constraint-Induced Movement during Stroke Rehabilitation (VECTORS): a single-center RCT. Neurology. 2009;73(3):195–201. doi:10.1212/WNL.0b013e3181ab2b27.
Dignam J, Copland D, McKinnon E, Burfein P, O’Brien K, Farrell A, et al. Intensive versus distributed aphasia therapy: a nonrandomized, parallel-group. dosage-controlled study. Stroke. 2015;46(8):2206–11. doi:10.1161/strokeaha.115.009522.
Milot MH, Cramer SC. Biomarkers of recovery after stroke. Curr Opin Neurol. 2008;21(6):654–9. doi:10.1097/WCO.0b013e3283186f96.
Burke E, Cramer SC. Biomarkers and predictors of restorative therapy effects after stroke. Curr Neurol Neurosci Rep. 2013;13(2):329. doi:10.1007/s11910-012-0329-9.
Feng W, Wang J, Chhatbar PY, Doughty C, Landsittel D, Lioutas VA, et al. Corticospinal tract lesion load: an imaging biomarker for stroke motor outcomes. Ann Neurol. 2015;78(6):860–70. doi:10.1002/ana.24510.
Marchina S, Zhu LL, Norton A, Zipse L, Wan CY, Schlaug G. Impairment of speech production predicted by lesion load of the left arcuate fasciculus. Stroke. 2011;42(8):2251–6. doi:10.1161/strokeaha.110.606103.
Forkel SJ, Thiebaut de Schotten M, Dell’Acqua F, Kalra L, Murphy DG, Williams SC. Anatomical predictors of aphasia recovery: a tractography study of bilateral perisylvian language networks. Brain. 2014;137(Pt 7):2027–39. doi:10.1093/brain/awu113.
Saver JL, Johnston KC, Homer D, Wityk R, Koroshetz W, Truskowski LL, et al. Infarct volume as a surrogate or auxiliary outcome measure in ischemic stroke clinical trials. The RANTTAS investigators. Stroke. 1999;30(2):293–8.
Groisser BN, Copen WA, Singhal AB, Hirai KK, Schaechter JD. Corticospinal tract diffusion abnormalities early after stroke predict motor outcome. Neurorehabil Neural Repair. 2014;28(8):751–60. doi:10.1177/1545968314521896.
Thickbroom GW, Byrnes ML, Archer SA, Mastaglia FL. Motor outcome after subcortical stroke correlates with the degree of cortical reorganization. Clin Neurophysiol. 2004;115(9):2144–50. doi:10.1016/j.clinph.2004.04.001.
Schaechter JD, van Oers CA, Groisser BN, Salles SS, Vangel MG, Moore CI, et al. Increase in sensorimotor cortex response to somatosensory stimulation over subacute poststroke period correlates with motor recovery in hemiparetic patients. Neurorehabil Neural Repair. 2012;26(4):325–34. doi:10.1177/1545968311421613.
Urbin MA, Hong X, Lang CE, Carter AR. Resting-state functional connectivity and its association with multiple domains of upper-extremity function in chronic stroke. Neurorehabil Neural Repair. 2014;28(8):761–9. doi:10.1177/1545968314522349.
Kim DY, Quinlan EB, Gramer R, Cramer SC. BDNF Val66Met polymorphism is related to motor system function after stroke. Phys Ther. 2015. doi:10.2522/ptj.20150135.
Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med. 1995;34(4):537–41.
Acknowledgments
This work received support from the NIH (K24HD074722 and T32AR047752).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cassidy has no conflicts of interest. Dr. Cramer served as a consultant for Dart Neuroscience, RAND Corporation, Dart Neuroscience, and MicroTransponder.
Rights and permissions
About this article
Cite this article
Cassidy, J.M., Cramer, S.C. Spontaneous and Therapeutic-Induced Mechanisms of Functional Recovery After Stroke. Transl. Stroke Res. 8, 33–46 (2017). https://doi.org/10.1007/s12975-016-0467-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-016-0467-5