Abstract
Looming drug resistance cases of leishmaniasis infection are an undeniably serious danger to worldwide public health, also jeopardize the efficacy of available drugs. Besides this, no successful vaccine is available till date. Since the ancient era, many plants and their parts have been used as medicines against various ailments. Hence, the importance of drug development for new molecules against Leishmania infection is significant that is a cost-effective and safer drug preferably from the natural herbal resources. We evaluated the GC–MS screening and efficacy of Putranjiva roxburghii (PR) against the sensitive and resistant promastigotes of L. donovani. GC–MS profiling revealed that the extract was rich in myo-inositol-4-C-methyl, azulene and desulphosinigrin. Quantitative investigation of phytoconstituents confirmed that PR was rich in phenols, flavonoids and terpenoids. We found an IC50 25.61 ± 0.57 µg/mL and 29.02 ± 1.21 µg/mL of PR against sodium stibogluconate sensitive and resistant strain respectively. It was found to be safer in cytotoxicity assay and generated ROS mediated oxidative stress in the parasitic cells which was evidenced by the increased and decreased levels of superoxide radicals, lipid peroxidation products, lipid bodies and levels of thiol, plasma membrane integrity respectively. Therefore, our results support the importance of P. roxburghii as a medicinal plant against L. donovani and showed potential for exploration as an antileishmanial agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Our planet is immensely rich in the biodiversity and we could not scrutinize more than a pinch of it. Hence, still there is vast inventory of plants having important phytoconstituents; those are biologically active molecules against various infections. Moreover, drug resistance is a serious issue which is being developed with time and it prompted the need of new molecules against different infections with safety profile.
Looming drug resistance cases of leishmaniasis infection are an undeniably serious danger to worldwide public health, also jeopardize the efficacy of available drugs (Ponte-Sucre et al. 2017). The drug resistance crisis has been credited to the excessive use and abuse of these medicaments and lack of new medication advancement (Ayukekbong et al. 2017). Besides this, no successful vaccine is available till date (Goyal et al. 2021a). Hence, coordinated endeavours to develop new, safe, cost effective, and easily accessible treatment option to manage the crisis are significantly required. Secondary metabolites of plant extracts are immensely capable of partial reversal of resistance and control of parasitic diseases (Molnár et al. 2010).
Leishmaniasis is a vector-borne and neglected tropical disease, which represents 3 major forms: mucocutaneous, cutaneous, and visceral. It is spread by the sand fly through the transmission of a flagellate protozoan parasite of the genus Leishmania. Its prevalence is high among populations of resource deprived nations. An estimated 0.7–1.5 million fresh cases come to notice each year in around 100 countries, which are endemic to leishmaniasis throughout the globe (Rezvan and Moafi 2015; Gannavaram et al. 2016; Kaye et al. 2020).
Visceral leishmaniasis (VL) is more crucial due to its severity than other forms. In the absence of timely treatment, the infection can be fatal (Goyal et al. 2021b). It is caused by Leishmania donovani or Leishmania infantum and characterized by clinical manifestations such as fever, anemia, weight loss, hepatomegaly, and splenomegaly. Ten countries account for more than 95% burden of the disease i.e. India, Brazil, Sudan, Ethiopia, Nepal, South Sudan, Somalia, China, Iraq, and Kenya (WHO 2018).
For the last 70 years, pentavalent antimonials are the established treatment agents for leishmaniasis, although, their irregular use has posed the risk of resistance development to the standard drugs. Sodium stibogluconate (SG) is a first-line drug treatment against the Leishmania infection. However, fast-growing drug resistance fails to treat the patients in more than 50% cases especially in the key endemic state; Bihar in India and the drug is abundantly toxic as well. Second-line drug amphotericin B has now emerged as a first-line drug due to its efficacy and fewer side effects than the former. SG and Amphotericin B are administered through the injection and the only option for oral drug available is miltefosine but, resistance is being developed against it too. Apart from the resistance and toxicity, lengthy regimen and high cost are the key restricting factors for their use (Guerin et al. 2002; Roy et al. 2017).
The long half-life of Amphotericin B and miltefosine poses the risk of creating resistance against Leishmania. The risk of resistance increases with the discontinued use of these drugs especially in the areas of low literacy rate and underprivileged societies of the Indian Sub-continent and Sudan (East Africa) (Bryceson 2001; Croft et al. 2006; Sundar et al. 2014). The major considerations such as safety profile and risk of resistance should be taken into account at the time of drug development against this infection. It could be achieved by the evaluation of new drug candidates against the resistant strain along with the sensitive strain of parasite (Hefnawy et al. 2017).
Since the ancient era, many plants and their parts have been used as medicines against various ailments. Plants and derived products hold potential to develop novel and promising chemotherapeutics. Therefore, we selected Putranjiva roxburghii to explore its potential against parasitic infection by Leishmania. P. roxburghii belongs to the family Putranjivaceae and its parts are used as a good source of traditional medicines. It signifies its name as it is considered to be helpful in conception in females by inducing fertility (Gupta 2016). The leaves and fruits of this plant are useful for curing cold, cough, fever, and arthralgia. P. roxburghii has been reported to be active as anthelmintic, hypoglycemic, antibacterial, antifungal, anticancer, antipyretic, anti-inflammatory, and aphrodisiac, etc. (Reanmongkol et al. 2009; Varma et al. 2011; Gupta 2016; Dar et al. 2018; Balkrishna et al. 2020; Kumar 2020). In the present study, we assessed the antileishmanial potential of P. roxburghii against the sensitive and resistant strains of L. donovani.
Material and methods
Plant material collection and extraction procedure
The leaves of P. roxhburghii (PR) were collected from the botanical garden of Panjab University, Chandigarh. The plant material was authenticated by the Department of Botany, Panjab University, Chandigarh. The leaves were shade dried, crushed, and grounded to get the fine powder and extracted with hydroethanol (30:70) in a soxhlet extractor. The extracted solution was subjected to a rota evaporator and lyophilized. The final extract was kept at -20 °C until further use.
Phytochemical screening
The extract was analyzed for the presence of various phytochemical components following the standard methods (Harborne 1973).
Quantitative analysis
Total terpenoid content (TTC)
The method illustrated by Ghorai et al. (2012) was employed for the determination of total terpenoid content in PR extract. Linalool was used as the standard for TTC estimation. In 1.5 mL chloroform the crude plant extract (200 µL) was mixed thoroughly and kept for 3 min followed by the addition of concentrated sulphuric acid (100 µL). The mixture was incubated for 2 h at room temperature and checked for the presence of reddish brown precipitate. Around 1.5 mL methanol (95%) was used for dissolving the precipitate and the absorbance was read at 538 nm on spectrophotometer. The results were quantified as mg/g of linalool equivalent.
Total flavonoid content estimation (TFC)
Determination of total flavonoid content in the hydroethanolic extract of P. roxburghii was carried out by employing AlCl3 colorimetric method. 200 µL of 1 mg/mL sample was dissolved in 800 µL distilled water. 60 µL, 5% NaNO2 was added and incubated for 5 min. Then 60 µL of 10% AlCl3 solution was added to the reaction mixture and rested for 5 min. Following this 1 M NaOH (400 µL) and distilled H2O was added. The volume was adjusted to 5 mL and absorbance was measured by UV–visible spectrophotometer at 510 nm. Quercetin was used as a standard to estimate total flavonoid content and the result was expressed as mg quercetin equivalent per g dry weight (Park et al. 2008).
Total phenol content estimation (TPC)
The total phenolic content in the crude extract was estimated using Folin-Ciocalteu reagent as described by Zhou et al. (2009). To 200 µL, 1 mg/mL sample 500 µL Folin-Ciocalteu reagent was added and mixed well. To neutralize the mixture 2 mL of Na2CO3 solution was added and incubated for 1 h in dark at room temperature with intermittent shaking for the development of colour. The sample absorption was determined at 765 nm on spectrophotometer. For plotting calibration curve gallic acid was used as a standard. The total phenol content was expressed as gallic acid equivalents (GAE) mg/1 g of the extract.
The GC–MS profiling
The PR extract was subjected to GC–MS analysis for chromatographic separation. It was carried out with Thermo Scientific TRACE 1300 GC equipped with Thermo TSQ 8000 Triple Quadrupole MS. A TraceGOLD™ TG 5MS GC column (phase: 5% diphenyl/95% dimethyl polysiloxane; dimensions: 30 mm × 0.25 mm, 0.25 µM film thickness) was used. The oven temperature was programmed as initial temperature was 60 °C with hold time 2 min and it was rose to 200 °C with hold time 4 min. Helium was the carrier gas with a constant flow rate of 1.5 mL/min. The injection volume was 1 µL. The sample was run at a range of 50–600 m/z. The total running time of GC–MS was 20.77 min. The retention time was used as basic criterion for the peak identification. The components were identified by NIST mass spectral library.
Parasite culture
Leishmania donovani sensitive strain (MHOM/IN/80/Dd8) was obtained from the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, UT, India. The sodium stibogluconate (SG)-resistant strain (P.B.-0014) of L. donovani was acquired from RMRIMS, Patna, Bihar. Both the strains were grown and cultured in modified NNN and RPMI-1640 media at 22 ± 2 °C in a B.O.D. chamber.
Antipromastigote analysis
Sensitive and resistant strain promastigotes of L. donovani were harvested from the culture vials. After washing with PBS, 1 × 106 cells/mL were seeded in a culture plate and incubated in a B.O.D. at 22 ± 2 °C with different concentrations of SG (sodium stibogluconate, Sigma-Aldrich) and PR for 72 h. DMSO (0.01%) served as negative control and SG as the positive control. Sample and trypan blue (1:1) were mixed and loaded on a Neubauer’s chamber for counting (Strober 2001). The % growth was calculated as follows:
The IC50 was computed by the Probit analysis using SPSS software.
Cytotoxicity assay
Human monocytic leukemia cell line THP-1 was utilized to assess the cytotoxicity of standard and tested drug. It is done by the colorimetric assessment of mitochondrial activity based on the depletion of MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) or tetrazolium salt (yellow) to formazan crystals (purple) showing the metabolic activity of cells. The THP-1 cell line was differentiated by PMA and cultured in RPMI-1640 medium at 37 °C and 5% CO2 in an incubator. SG and PR (20–1000 µg/ml) concentrations were added to different wells. After 72 h, MTT was added (10 µL of 1 mg/mL) and again incubated for the next 4-5 h. The plate was read at 550 nm in an ELISA reader after formazan crystals were dissolved by the addition of DMSO (Essid et al. 2015). The following formula was considered for the calculation of % cytotoxicity:
where At- O.D. of treated, Ab- O.D. of Blank, Ac-O.D. of untreated cells.
The computation of the CC50 value was calculated by SPSS software.
Selectivity index (SI)
It is an indicator of safety and efficacy. The drug with less toxicity and higher activity at mammalian macrophages is sorted by its selectivity index. It is a relationship between IC50 and CC50:
ROS generation
Promastigotes of L. donovani (1 × 106 cells/mL) were kept with the IC50 values of the drug (SG or PR) and without a drug in a B.O.D. for 72 h at 22 ± 2 °C. H2DCFDA, a cell-permeable probe was employed for the detection of intracellular reactive oxygen species (ROS) generation. It was added (10 µM) after washing with PBS and incubated for 20 min in dark at room temperature. The plate was read at excitation and emission wavelength of 504 nm and 529 nm respectively in a microplate reader. The results were represented as fluorescence intensity units after triplicate measurements (Cataneo et al. 2019).
Total lipid peroxidation products
The method described by Mukherjee et al. (2016) was followed for the estimation of lipid peroxidation products. The promastigotes were harvested and pelleted down after treatment with SG or PR for 72 h. The cells were washed with PBS and the final pellet was dissolved in 15% SDS solution in PBS (2 mL). The total lipid peroxidation products were measured by reading fluorescence intensities at 360 nm and 430 nm excitation and emission wavelengths.
Thiol content
The total intracellular thiol content was assessed from the deproteinized cell extract of sensitive and resistant promastigotes. SG and PR treated promastigotes for 72 h were pelleted down and washed with PBS. The final pellet was suspended in TCA (0.6 mL of 25%) and kept on ice for 10 min. Cell debris and denatured proteins were removed by centrifugation at 4 °C for 10 min. The thiol content was assessed spectrophotometrically in the resulting supernatant using 0.6 mM 5, 5′- dithio-bis (2-nitrobenzoic acid) in 0.2 M Na3PO4 buffer (pH 8.0) and OD as read at 412 nm (Purkait et al. 2012).
Superoxide radicals
SG or PR treated Leishmania promastigotes were harvested and washed with PBS and the final pellet was dissolved in PBS (100 µL). 10 µL of this suspension was mixed with reaction mixture (1 mL) having 0.1 mM EDTA, 50 mM sodium carbonate, 50 µM nitrobluetetrazolium, and 0.5% Triton X-100. The absorbance was read in a spectrophotometer at 560 nm (Das et al. 2017).
Lipid bodies
Nile red dye was used for the determination of lipid bodies. SG or PR treated promastigotes of L. donovani for 72 h were garnered and given two washings with PBS. 10 µg/mL Nile Red was added to the promastigotes containing wells and incubated at room temperature for 30 min. Washing with PBS followed by plate reading for fluorescence at 485 nm and 535 nm of excitation and emission wavelengths in a microplate reader (De MacEdo Silva et al. 2018).
Cell membrane integrity
The propidium iodide (PI) was employed to assess cell membrane integrity. Untreated or treated promastigotes with SG or PR were harvested and centrifuged. These were washed and incubated at room temperature with PI (0.2 µg/mL) for 5 min in dark in a 96-well microplate. The plate was read in a microplate reader at 535 nm and 617 nm (da Silva Rodrigues et al. 2019).
Data analysis
One way ANOVA with Bonferroni multiple comparison was applied to analyze the data. The results are expressed as mean ± SD and p < 0.05 taken as statistically significant.
Results
Phytochemical analysis
These are 2° plant metabolites and their presence indicates the strength of any drug of herbal origin. All the major phytoconstituents were present in PR such as alkaloids, phenols, flavonoids, terpenoids, glycosides, and saponins. The quantitative phytochemical analysis revealed that the maximum quantity of total phenol was present in PR extract. It was observed that the total phenolic content was 46.58 ± 2.52 mg/g GAE. The extract was also enriched with 29.0 ± 2 mg/g QE of total flavonoid and 23.6 ± 1.6 mg/g LE of total terpenoid content.
GC–MS screening
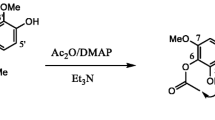
The extract of P. roxburghii leaves was screened by GC–MS for the chemical composition and the results depicted the presence of various bioactive compounds. A total of 10 chemical compounds were observed in screening (Table 1). The corresponding peaks of reported compounds are represented in the chromatogram (Fig. 1). The components associated with diverse classes of phytochemicals are present in it. Myo-inositol-4-C-methyl showed maximum abundance (90.05%), followed by azulene (3.99%) and desulphosinigrin (2%).
Anti-promastigotes activity
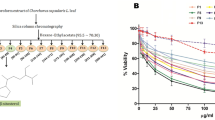
The effects of different concentrations of SG and PR were assessed for their activity against the sensitive and resistant strains of L. donovani. A dose-dependent curve was observed for the percentage growth inhibition of parasites. The IC50 value of PR and SG was 25.61 ± 0.57 µg/mL and 14.40 ± 0.53 µg/mL after 72 h of exposure to sensitive strain whereas, the IC50 value of PR and SG against the resistant strain of L. donovani was 29.02 ± 1.21 µg/mL and 49.84 ± 1.09 µg/mL respectively (Fig. 2).
Inhibitory concentration (50%). IC50 of sodium stibogluconate (SG) and Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain after 72 h. *p value: S + SG vs S + PR, *p < 0.05 (significant). #p value: R + SG vs R + PR, #p < 0.05 (significant). @p value: S + SG vs R + SG, @p < 0.05 (significant)
Cytotoxicity against THP-1 cell line
The cytotoxicity of drugs was tested on the THP-1 cell line by MTT assay. The test signifies the cellular energy profile and mitochondrial respiration. The CC50 value of SG was 52.34 ± 2.43 µg/mL and 1182.36 ± 73.14 µg/mL for PR. The SG resulted as a toxic compound as compared to PR which was non-toxic and safe.
Selectivity index (SI)
An active and safe drug with a selectivity index > 10 shows its safety and efficacy in terms of less toxicity with high antiparasitic activity. In our observations, SI of SG and PR were < 10 and > 10 respectively. This indicates the toxic nature of SG and the safety of PR.
Treatment derived ROS augmentation
The key property of ROS is to combat the pathogens. The H2DCFDA was employed for the assessment of ROS generation. It is a fluorogenic dye that diffuses into the cell. The cellular esterases deacetylate the H2DCFDA from fluorescent to non-fluorescent. Reactive oxygen species regulate their oxidation from non-fluorescent to highly fluorescent DCF (2′,7′-dichlorofluorescin). PR was able to generate the ROS in promastigotes of the sensitive and resistant strain. The ROS generation was observed significantly (p < 0.05) more in PR exposed resistant promastigotes in comparison to resistant promastigotes exposed to SG. Augmentation of endoparasitic ROS in both the strains upon PR treatment than untreated promastigotes was observed and concluded in Fig. 3, which could lead to the apoptosis in parasites.
Reactive oxygen species (ROS) generation. Levels of ROS after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain in contrast to untreated control of sensitive (UCS) and untreated control of resistant (UCR) respectively. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). %p value: UCR vs R + SG, %p > 0.05 (non significant). #p value: UCR vs R + PR, #p < 0.05 (significant). @p value: R + SG vs R + PR, @p < 0.05 (significant)
Lipid peroxidation
Total fluorescent lipid peroxide products were measured in drug-treated promastigotes. The SG or PR treatment to sensitive Leishmania promastigotes leads to the higher (p < 0.05) lipid peroxides in comparison to the untreated cells. The resistant strain parasites exposed to PR increased (p < 0.05) the lipid peroxides whereas SG did increase non significantly (p > 0.05) in contrast to untreated cells (Fig. 4).
Total lipid peroxidation. Levels of fluorescent lipid peroxidation products after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). #p value: UCR vs R + SG; R + PR, #p < 0.05 (significant). @p value: R + SG vs R + PR, @p < 0.05 (significant)
Total thiol content
Reduced thiol level is the characteristic of the action potential of antimonials that depends upon redox potential. Antimonials diminish the thiol levels in parasitic cells. The higher thiol level in resistant parasites is the escaping mechanism from the ROS mediated oxidative stress. The level of thiols after treatment with PR was significantly (p < 0.05) less in contrast to SG in resistant promastigotes (Fig. 5). Sensitive promastigotes also showed less thiol with high ROS after PR exposure that indicates the connecting activation for the apoptosis.
Thiol content. Levels of thiol after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). %p value: UCR vs R + SG, %p > 0.05 (non significant). #p value: UCR vs R + PR, #p < 0.05 (significant). ^p value: R + SG vs R + PR, ^p > 0.05 (non significant)
Superoxide radicals
Oxidative stress-induced by drug exposure interrupts the normal cellular physiology and leads to cell death. Therefore, drug-treated promastigotes were assessed for the generation of superoxide radicals. The superoxide radicals generation was higher (p < 0.05) in the cell lysate of promastigotes exposed to SG or PR than untreated promastigotes (Fig. 6).
Superoxide radicals. The levels of superoxide radicals after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). %p value: UCR vs R + SG, %p > 0.05 (non significant). #p value: UCR vs R + PR, #p < 0.05 (significant). ^p value: R + SG vs R + PR, ^p > 0.05 (non significant)
Lipid Bodies
Neutral lipid bodies were measured by utilizing a metachromatic dye in treated and untreated parasites. The increased level of lipid bodies was evidenced by the treatment of drugs (SG or PR) (Fig. 7). PR treated promastigotes were found to have higher (p < 0.05) lipid bodies in both the strains than untreated promastigotes. The sensitive promastigotes showed an increased (p < 0.05) level of lipid bodies in sensitive but not in resistant promastigotes.
Lipid bodies. Levels of lipid bodies after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). %p value: UCR vs R + SG, %p > 0.05 (non significant). #p value: UCR vs R + PR, #p < 0.05 (significant). @p value: R + SG vs R + PR, @p < 0.05 (significant)
Cell membrane integrity
The cell membrane integrity was also checked using propidium iodide as it enters the disrupted cell membrane and represents the loss in membrane integrity. A high (p < 0.05) level of integrity loss was observed in promastigotes of sensitive strain after treatment with SG or PR. Whereas it was higher (P < 0.05) in resistant promastigotes when exposed to PR only (Fig. 8).
Plasma membrane Integrity. The loss in plasma membrane integrity after exposure to sodium stibogluconate (SG) or Putranjiva roxburghii (PR) against sensitive (S) and resistant (R) strain. *p value: UCS vs S + SG; S + PR, *p < 0.05 (significant). $p value: S + SG vs S + PR, $p < 0.05 (significant). #p value: UCR vs R + SG; R + PR, #p < 0.05 (significant). @p value: R + SG vs R + PR, @p < 0.05 (significant)
Discussion
The widespread availability of pentavalent antimonials and their rampant misuse contributed to developing resistance, especially in the Indian Sub-continent. The major possible reasons for misuse include inappropriate use by unqualified practitioners and break in regimen causing sub-therapeutic blood concentration that results in more parasitic tolerance to the drug (Chakravarty and Sundar 2010). Therefore, more pressure is being exerted on the safekeeping of the available drug from the high risk of getting resistance against them. Other than the issue of resistance, the toxic nature of the drugs also is of great concern at the time of drug development. It strongly favours the notion of herbal research, which is proven to have options against various ailments including the infectious diseases from the pre-antibiotic era. Thus it’s the need of the hour to develop a drug that is effective, safe with no or fewer side effects, and can be available at a reasonable price to the main target of the disease as the target population is the impoverished community of developing nations.
Natural products derived from various plants are utilized against different diseases as a drug. Several crude plant extracts and plant-derived compounds have been evaluated for their activity against infections by helminths, fungi, and protozoa recently (Cragg and Newman 2013; Sales et al. 2016; Pramanik et al. 2019). Moreover, these are safe, non-toxic, cost-effective, and efficiently active (Hammi et al. 2020). Therefore, it is a better way to get a drug of choice based on today’s need and many more herbal sources are to be explored for their active potential against this infection by Leishmania spp.
In the wake of exploration of bioactive and novel herbal leads phytochemical screening is the initial step. Phytochemicals are plant secondary metabolites that serve as significant defence against diseases and pathogens as well as crucial for pertinent physiological processes (Forni et al. 2019). Phenols are most promising phytoconstituents associated with the cure of myriad of human diseases. The presence of excess of phenols and flavonoids in P. roxburghii extract drove us to study further and explore its antileishmanial potential. Umpteen polyphenolic compounds have shown antileishmanial activity (Montrieux et al. 2014; Ogungbe et al. 2014; Monzote et al. 2016). Furthermore, the extract is also rich in terpenoids and alkaloids, substantiating the usage of this plant in folk medicine.
Additionally the GC–MS profiling of P. roxburghii revealed the identification of 10 compounds. Among the identified components desulphosinigrin, 1-( +)-Ascorbic acid-2, 6-dihexadecanoate, phthalic acid-butyl hex-3-ester, 1-Hexadecanol, and pentadecane reported to have antimicrobial activity. Myo-inositol-4-C-methyl is a potent hypoglycemic agent (Pintaudi et al. 2016; Owczarczyk-Saczonek et al. 2018). Therewithal, azulene from Achillea millefolium and pentadecane were also reported to have antileishmanial activity against L. amazonensis and L. infantum respectively (Rohloff et al. 2013; Bruno et al. 2015).
Based on the aforementioned phytochemical lavishness of Putranjiva roxburghii we investigated it as an antileishmanial drug candidate against the sensitive and resistant strain as well. The antipromastigote activity of PR in contrast to SG was assessed. Inhibitory concentration (50%) of PR was evaluated by exposing the promastigotes of sensitive and resistant strains to different concentrations of PR. The PR showed its potential against both the strains of L. donovani in vitro. It was noticed that the IC50 of PR for both strains were non-significantly dissimilar. No cytotoxicity in association with its efficacy showed its potential. Our results are in agreement with the study of Chouhan et al. (2015) where they assessed the efficacy of Azadirachta indica against L. donovani and found an IC50 of 34 and 77.66 µg/mL for leaves and seeds respectively. The IC50 values 12.5 mg/mL of Vigna radiata, 50 mg/mL of Tamarix ramosissima, and 25/12.5 mg/mL of Carthamus lanatus against L. major and L. trpoica respectively were assessed by Akya et al. (2020). The IC50 of Physalis angulata was reported to be 39.5 µg/mL ± 5.1 against L. amazonensis (da Silva et al. 2015).
ROS is a key regulatory molecule for the parasite killing and elimination. The generation of apoptosis-inducing reactive oxygen species (ROS) takes place within the mitochondria in uni- and multicellular organisms (Kathuria et al. 2014). The cell death of parasite is a consequence of increase in the level of reactive oxygen species due to damage in various biomolecules such as lipids, proteins, DNA, RNA, and membranes (Redza-Dutordoir and Averill-Bates 2016). Therefore, we evaluated the level of ROS before and after treatment with standard and tested drug i.e. SG and PR respectively. ROS generation was higher in sensitive strain after exposure to SG or PR in contrast to untreated promastigotes. PR treatment generated more ROS in resistant strain in contrast to SG treatment. Different natural compounds such as curcumin, withaferin A, eugenol-rich oil of S. aromaticum, and Piper betle (ethanolic extract) have been tested and shown to generate ROS and induction of apoptosis in promastigotes (Sen et al. 2007; Das et al. 2008; Misra et al. 2009; Islamuddin et al. 2013). Tan et al. (2016) observed the role of oxidative stress generated by ROS and NO in DNA degradation and cell death. Chandrasekaran et al. (2013) reported the apoptotic like death of L. donovani by withanolides powered by ROS generation. The killing of L. donovani promastigotes through the production of ROS by the neem leaf extract has been reported (Dayakar et al. 2015). Different cell systems are affected by higher ROS production in response to drug exposure, mefloquine killed the protozoan parasite Plasmodium falciparum due to high ROS generation in treated cells (Gunjan et al. 2016).
Cellular metabolism and normal physiology rely on the well-regulated redox state and fluctuations in the cellular redox state can sensitize the thiols in eukaryotes (Baba and Bhatnagar 2018). In leishmanial cells, the redox of ROS and thiol are inversely proportional to each other. The more production of ROS in resistant strain after treatment with SbIII successfully reduced the thiol content and made them sensitive to it (Magalhães et al. 2018). In this study, thiol content was evaluated and the higher level of thiol was noted in resistant than sensitive promastigotes. Exposure of resistant strain to SG could not produce sufficient ROS and thereby the thiol level got increased whereas, it was lesser after exposure to PR in both the strains with higher ROS level. PR mediated oxidative stress due to the generation of ROS and down-regulation of thiol in both the strains contributed to their killing. Integrity disruption of the plasma membrane and imbalanced homeostasis of thiol causes the leishmanicidal potential of Allium sativum (Sharma et al. 2009). SbIII-resistant promastigotes of L. amazonensis were found to have higher thiol content (do Monte-Neto et al. 2011). The increase and decrease in ROS and thiol levels respectively was observed after the treatment with leaf extract of Corchorus capsularis against the L. donovani promastigotes (Pramanik et al. 2019).
Lipid deposition is ubiquitous in all life forms i.e. prokaryotes and eukaryotes that stockpiled as lipid droplets or lipid bodies in the cell (Lee et al. 2013; Onal et al. 2017). Lipid body accumulation is the repercussion of different imbalances in the normal cellular functioning of parasite and is a characteristic of stress in cellular physiology. Hence, we analysed the levels of lipid bodies in the parasitic cells to see the effects of drug exposure. Our results depict that PR treatment to promastigotes of sensitive and resistant strains enhance the lipid bodies formation. The accumulation of lipid bodies was also reported by the study of Dantas et al. (2003) where they exposed Trypanosoma cruzi with Taxol. One more study suggested similar findings in promastigotes of L. amazonensis treated with Ravuconazole (De MacEdo Silva et al. 2018). Increased levels of intracellular lipid bodies caused alteration in the sterol composition of the cell membrane of the parasite, which is responsible for the membrane integrity disruption and ultimately cell death. It was reported by the treatment of L. amazonensis and L. donovani promastigotes with 4-nitobenzaldehyde thiosemicarbazone (BZTS) and zerumbone respectively (Britta et al. 2014; Mukherjee et al. 2016).
Free radicals are the possible agents those are responsible for the lipid peroxidation that diminish fluidity, plasma membrane integrity, physicochemical properties, and eventually keeps the cell at the verge of apoptosis (Abdel Moneim 2016; El-Khadragy et al. 2018). For that reason, the total lipid perxidation products were assessed in response to drug action on parasitic cells. The drug-exposed generation of superoxide radicals and lipid peroxidation products were also assessed in this study. The treatment of Leishmania promastigotes with SG elevated the levels of lipid peroxidation and superoxide radicals in sensitive strain but could not in resistant strain. However, PR exposure to promastigotes of both the strains successfully increased their levels. Our results are supported by the study of Das et al. (2017) where they found an increased level of lipid peroxidation and superoxide generation in promastigotes of L. donovani treated with Sterculia villosa extract.
The plasma membrane integrity is an essential factor that predicts the health of cells and loss in the integrity depicts that cell machinery is being disturbed and ultimately leading to cell death. In this study, results showed the loss in plasma membrane integrity due to drug treatment as compared to untreated promastigotes. PR efficiently disrupted the cell membrane of promastigotes of both the strains whereas SG performed it only on sensitive promastigotes. The study by da Silva Rodrigues et al. (2019) supported our results where they observed loss in plasma membrane integrity in L. amazonensis promastigotes after treated with clomipramine. The Caryocar coriaceum extract treatment degraded the plasma membrane of L. amazonensis parasites (Tomiotto-Pellissier et al. 2018).
The depletion in mitochondrial membrane potential generates ROS that down-regulate the GSH level and in turn elevates the oxidative stress in the parasitic cell (Sen et al. 2007). We found such a series of events; oxidative stress required for the killing of parasitic cells induced by decreased GSH level, higher ROS production, and depleted membrane integrity following drug exposure. Therefore, successful drug activated killing of the parasite was evident in the present study.
Conclusion
Medicinal and restorative plants have been a focal point of consideration since time immemorial. The synthetic drugs have numerous clinical complexities; hence looking forward to the herbal origin drugs and medicaments are an excellent option. The results of the present study revealed antileishmanial activity of Putranjiva roxburghii against SG sensitive and resistant strain of L. donovani, which is majorly potentiated by its capability to incite the parasite killing through the ROS generation and thereby induce oxidative stress in parasitic cells. These functions might be due to the contributory action of rich phytochemical treasure of P. roxburghii.
Availability of data and material
All data generated during this study are included in this article.
References
Abdel Moneim AE (2016) Indigofera oblongifolia prevents lead acetate-induced hepatotoxicity, oxidative stress, fibrosis and apoptosis in rats. PLoS ONE 11:1–18. https://doi.org/10.1371/journal.pone.0158965
Akya A, Chegene Lorestani R, Zhaleh H et al (2020) Effect of Vigna radiata, Tamarix ramosissima and Carthamus lanatus extracts on Leishmania major and Leishmania tropica: an in vitro study. Chin Herb Med 12:171–177. https://doi.org/10.1016/j.chmed.2019.12.006
Ayukekbong JA, Ntemgwa M, Atabe AN (2017) The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control 6:1–8. https://doi.org/10.1186/s13756-017-0208-x
Baba SP, Bhatnagar A (2018) Role of thiols in oxidative stress. Curr Opin Toxicol 7:133–139. https://doi.org/10.1016/j.cotox.2018.03.005
Balkrishna A, Sharma VK, Das SK et al (2020) Characterization and anti-cancerous effect of putranjiva roxburghii seed extract mediated silver nanoparticles on human colon (HCT-116), pancreatic (PANC-1) and breast (MDA-MB 231) cancer cell lines: a comparative study. Int J Nanomed 15:573–585. https://doi.org/10.2147/IJN.S230244
Britta EA, Scariot DB, Falzirolli H et al (2014) Cell death and ultrastructural alterations in Leishmania amazonensis caused by new compound 4-Nitrobenzaldehyde thiosemicarbazone derived from S-limonene. BMC Microbiol 14:1–12. https://doi.org/10.1186/s12866-014-0236-0
Bruno F, Castelli G, Migliazzo A et al (2015) Cytotoxic screening and in vitro evaluation of pentadecane against leishmania infantum promastigotes and amastigotes. J Parasitol 101:701–705. https://doi.org/10.1645/15-736
Bryceson A (2001) A policy for leishmaniasis with respect to the prevention and control of drug resistance. Trop Med Int Heal 6:928–934. https://doi.org/10.1046/j.1365-3156.2001.00795.x
Cataneo AHD, Tomiotto-Pellissier F, Miranda-Sapla MM et al (2019) Quercetin promotes antipromastigote effect by increasing the ROS production and anti-amastigote by upregulating Nrf2/HO-1 expression, affecting iron availability. Biomed Pharmacother 113:108745. https://doi.org/10.1016/j.biopha.2019.108745
Chakravarty J, Sundar S (2010) Drug resistance in leishmaniasis. J Glob Infect Dis 2:167. https://doi.org/10.4103/0974-777x.62887
Chandrasekaran S, Dayakar A, Veronica J et al (2013) An in vitro study of apoptotic like death in Leishmania donovani promastigotes by withanolides. Parasitol Int 62:253–261. https://doi.org/10.1016/j.parint.2013.01.007
Chouhan G, Islamuddin M, Want MY et al (2015) Apoptosis mediated leishmanicidal activity of Azadirachta indica bioactive fractions is accompanied by Th1 immunostimulatory potential and therapeutic cure in vivo. Parasit Vectors 8:1–24. https://doi.org/10.1186/s13071-015-0788-3
Cragg GM, Newman DJ (2013) Natural products: a continuing source of novel drug leads. Biochim Biophys Acta Gen Subj 1830:3670–3695. https://doi.org/10.1016/j.bbagen.2013.02.008
Croft SL, Sundar S, Fairlamb AH (2006) Drug resistance in leishmaniasis. Clin Microbiol Rev 19:111–126
da Silva Rodrigues JH, Miranda N, Volpato H et al (2019) The antidepressant clomipramine induces programmed cell death in Leishmania amazonensis through a mitochondrial pathway. Parasitol Res 118:977–989. https://doi.org/10.1007/s00436-018-06200-x
da Silva RRP, da Silva BJM, Rodrigues APD et al (2015) In vitro biological action of aqueous extract from roots of Physalis angulata against Leishmania (Leishmania) amazonensis. BMC Complement Altern Med 15:1–10. https://doi.org/10.1186/s12906-015-0717-1
Dantas AP, Barbosa HS, De Castro SL (2003) Biological and ultrastructural effects of the anti-microtubule agent taxol against Trypanosoma cruzi. J Submicrosc Cytol Pathol 35:287–294
Dar P, Faisal M, Dar A, Waqas U (2018) Journey describing biological activities and chemical constituents in the leaves, stem bark and seed of putranjiva roxburghii. Curr Tradit Med 4:263–278. https://doi.org/10.2174/2215083805666181206104450
Das A, Das MC, Das N, Bhattacharjee S (2017) Evaluation of the antileishmanial potency, toxicity and phytochemical constituents of methanol bark extract of Sterculia villosa. Pharm Biol 55:998–1009. https://doi.org/10.1080/13880209.2017.1285946
Das R, Roy A, Dutta N, Majumder HK (2008) Reactive oxygen species and imbalance of calcium homeostasis contributes to curcumin induced programmed cell death in Leishmania donovani. Apoptosis 13:867–882. https://doi.org/10.1007/s10495-008-0224-7
Dayakar A, Chandrasekaran S, Veronica J et al (2015) In vitro and in vivo evaluation of anti-leishmanial and immunomodulatory activity of Neem leaf extract in Leishmania donovani infection. Exp Parasitol 153:45–54. https://doi.org/10.1016/j.exppara.2015.02.011
De MacEdo Silva ST, Visbal G, Godinho JLP et al (2018) In vitro antileishmanial activity of ravuconazole, a triazole antifungal drug, as a potential treatment for leishmaniasis. J Antimicrob Chemother 73:2360–2373. https://doi.org/10.1093/jac/dky229
Monte-Neto de RL, Coelho AC, Raymond F et al (2011) Gene expression profiling and molecular characterization of antimony resistance in Leishmania amazonensis. PLoS Negl Trop Dis. https://doi.org/10.1371/journal.pntd.0001167
El-Khadragy M, Alolayan EM, Metwally DM et al (2018) Clinical efficacy associated with enhanced antioxidant enzyme activities of silver nanoparticles biosynthesized using moringa oleifera leaf extract, against cutaneous leishmaniasis in a murine model of leishmania major. Int J Environ Res Public Health 15:1037
Essid R, Rahali FZ, Msaada K et al (2015) Antileishmanial and cytotoxic potential of essential oils from medicinal plants in Northern Tunisia. Ind Crops Prod 77:795–802. https://doi.org/10.1016/j.indcrop.2015.09.049
Forni C, Facchiano F, Bartoli M et al (2019) Beneficial role of phytochemicals on oxidative stress and age-related diseases. Biomed Res Int. https://doi.org/10.1155/2019/8748253
Gannavaram S, Bhattacharya P, Ismail N et al (2016) Modulation of innate immune mechanisms to enhance Leishmania vaccine-induced immunity: role of coinhibitory molecules. Front Immunol 7:1–10. https://doi.org/10.3389/fimmu.2016.00187
Ghorai N, Ghorai N, Chakraborty S et al (2012) Estimation of total Terpenoids concentration in plant tissues using a monoterpene, Linalool as standard reagent. Protoc Exch. https://doi.org/10.1038/protex.2012.055
Goyal DK, Keshav P, Kaur S (2021a) Adjuvanted vaccines driven protection against visceral infection in BALB/c mice by Leishmania donovani. Microb Pathog. https://doi.org/10.1016/j.micpath.2021.104733
Goyal DK, Keshav P, Kaur S (2021b) Immune induction by adjuvanted Leishmania donovani vaccines against the visceral leishmaniasis in BALB/c mice. Immunobiology. https://doi.org/10.1016/j.imbio.2021.152057
Guerin PJ, Olliaro P, Sundar S, et al (2002) Visceral leishmaniasis: Current status of control, diagnosis, and treatment, and a proposed research and development agenda. Lancet Infect Dis 2:494–501. https://doi.org/10.1016/S1473-3099(02)00347-X
Gunjan S, Singh SK, Sharma T et al (2016) Mefloquine induces ROS mediated programmed cell death in malaria parasite: plasmodium. Apoptosis 21:955–964. https://doi.org/10.1007/s10495-016-1265-y
Gupta M (2016) A review of pharmacological properties, pharmacognosy and therapeutic actions of Putranjiva roxburghii Wall. (Putranjiva). Int J Herb Med 4:104–108
Hammi KM, Essid R, Tabbene O et al (2020) Antileishmanial activity of Moringa oleifera leaf extracts and potential synergy with amphotericin B. South Afr J Bot 129:67–73. https://doi.org/10.1016/j.sajb.2019.01.008
Harborne J (1973) Phytochemical methods in: a guide to modern techniques of plant analysis. Chapman and Hall Ltd, London
Hefnawy A, Berg M, Dujardin JC, Muylder GD (2017) Exploiting knowledge on Leishmania Drug resistance to support the quest for new drugs. Trend Parasitol 33:167–174
Islamuddin M, Sahal D, Afrin F (2013) Apoptosis-like death in Leishmania donovani promastigotes induced by eugenol-rich oil of Syzygium aromaticum. J Med Microbiol 63:74–85. https://doi.org/10.1099/jmm.0.064709-0
Kathuria M, Bhattacharjee A, Sashidhara KV et al (2014) Induction of mitochondrial dysfunction and oxidative stress in leishmania donovani by orally active clerodane diterpene. Antimicrob Agents Chemother 58:5916–5928. https://doi.org/10.1128/AAC.02459-14
Kaye PM, Cruz I, Picado A et al (2020) Leishmaniasis immunopathology—impact on design and use of vaccines, diagnostics and drugs. Semin Immunopathol 42:247–264. https://doi.org/10.1007/s00281-020-00788-y
Kumar N (2020) Phytochemistry and medicinal value of putranjiva roxburghii wall. In: Advances in pharmaceutical biotechnology: recent progress and future applications, p. 133–144.https://doi.org/10.1007/978-981-15-2195-9_11
Lee SJ, Zhang J, Choi AMK, Kim HP (2013) Mitochondrial dysfunction induces formation of lipid droplets as a generalized response to stress. Oxid Med Cell Longev. https://doi.org/10.1155/2013/327167
Magalhães LS, Bomfim LGS, Mota SG et al (2018) Increased thiol levels in antimony-resistant leishmania infantum isolated from treatment-refractory visceral leishmaniasis in Brazil. Mem Inst Oswaldo Cruz 113:119–125. https://doi.org/10.1590/0074-02760170289
Misra P, Kumar A, Khare P et al (2009) Pro-apoptotic effect of the landrace Bangla Mahoba of Piper betle on Leishmania donovani may be due to the high content of eugenol. J Med Microbiol 58:1058–1066. https://doi.org/10.1099/jmm.0.009290-0
Molnár J, Engi H, Hohmann J et al (2010) Reversal of multidrug resitance by natural substances from plants. Curr Top Med Chem 10:1757–1768
Montrieux E, Perera WH, García M et al (2014) In vitro and in vivo activity of major constituents from Pluchea carolinensis against Leishmania amazonensis. Parasitol Res 113:2925–2932. https://doi.org/10.1007/s00436-014-3954-1
Monzote L, Perera Córdova WH, García M et al (2016) In-vitro and in-vivo activities of phenolic compounds against cutaneous leishmaniasis. Rec Nat Prod 10:269–276
Mukherjee D, Singh CB, Dey S et al (2016) Induction of apoptosis by zerumbone isolated from Zingiber zerumbet (L.) Smith in protozoan parasite Leishmania donovani due to oxidative stress. Brazil J Infect Dis 20:48–55. https://doi.org/10.1016/j.bjid.2015.10.002
Ogungbe IV, Erwin WR, Setzer WN (2014) Antileishmanial phytochemical phenolics: molecular docking to potential protein targets. J Mol Graph Model 48:105–117. https://doi.org/10.1016/j.jmgm.2013.12.010
Onal G, Kutlu O, Gozuacik D, Emre SD (2017) Lipid droplets in health and disease. Lipids Health Dis. https://doi.org/10.1186/s12944-017-0521-7
Owczarczyk-Saczonek A, Lahuta LB, Ligor M et al (2018) The healing-promoting properties of selected cyclitols—a review. Nutrients 10:1–20. https://doi.org/10.3390/nu10121891
Park YS, Jung ST, Kang SG et al (2008) Antioxidants and proteins in ethylene-treated kiwifruits. Food Chem 107:640–648. https://doi.org/10.1016/j.foodchem.2007.08.070
Pintaudi B, Di Vieste G, Bonomo M (2016) The Effectiveness of Myo-Inositol and D-Chiro inositol treatment in type 2 diabetes. Int J Endocrinol. https://doi.org/10.1155/2016/9132052
Ponte-Sucre A, Gamarro F, Dujardin JC et al (2017) Drug resistance and treatment failure in leishmaniasis: a 21st century challenge. PLoS Negl Trop Dis 11:1–24. https://doi.org/10.1371/journal.pntd.0006052
Pramanik PK, Paik D, Pramanik A, Chakraborti T (2019) White jute (Corchorus capsularis L.) leaf extract has potent leishmanicidal activity against Leishmania donovani. Parasitol Int 71:41–45. https://doi.org/10.1016/j.parint.2019.03.012
Purkait B, Kumar A, Nandi N et al (2012) Mechanism of amphotericin B resistance in clinical isolates of Leishmania donovani. Antimicrob Agents Chemother 56:1031–1041. https://doi.org/10.1128/AAC.00030-11
Reanmongkol W, Noppapan T, Subhadhirasakul S (2009) Antinociceptive, antipyretic, and anti-inflammatory activities of Putranjiva roxburghii Wall. leaf extract in experimental animals. J Nat Med 63:290–296. https://doi.org/10.1007/s11418-009-0336-6
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta Mol Cell Res 1863:2977–2992. https://doi.org/10.1016/j.bbamcr.2016.09.012
Rezvan H, Moafi M (2015) An overview on Leishmania vaccines: a narrative review article. Vet Res forum an Int Q J 6:1–7
Rohloff J, Hymete A, Tariku Y (2013) Plant-derived natural products for the treatment of leishmaniasis, 1st edn. Copyright © 2013 Elsevier B.V. All rights reserved.
Roy S, Dutta D, Satyavarapu EM et al (2017) Mahanine exerts in vitro and in vivo antileishmanial activity by modulation of redox homeostasis. Sci Rep 7:1–16. https://doi.org/10.1038/s41598-017-03943-y
Sales MDC, Costa HB, Fernandes PMB et al (2016) Antifungal activity of plant extracts with potential to control plant pathogens in pineapple. Asian Pac J Trop Biomed 6:26–31. https://doi.org/10.1016/j.apjtb.2015.09.026
Sen N, Banerjee B, Das BB et al (2007) Apoptosis is induced in leishmanial cells by a novel protein kinase inhibitor withaferin A and is facilitated by apoptotic topoisomerase I-DNA complex. Cell Death Differ 14:358–367. https://doi.org/10.1038/sj.cdd.4402002
Sharma U, Velpandian T, Sharma P, Singh S (2009) Evaluation of anti-leishmanial activity of selected Indian plants known to have antimicrobial properties. Parasitol Res 105:1287–1293. https://doi.org/10.1007/s00436-009-1554-2
Strober W (2001) Trypan blue exclusion test of cell viability. Curr Protoc Immunol Appendix 3:2–3. https://doi.org/10.1002/0471142735.ima03bs21
Sundar S, Singh A, Singh OP (2014) Strategies to overcome antileishmanial drugs unresponsiveness. J Trop Med. https://doi.org/10.1155/2014/646932
Tan H, Wang N, Li S et al (2016) The reactive oxygen species in macrophage polarization: human diseases. Oxid Med Cell Longev 2016:1–16. https://doi.org/10.1155/2016/2795090
Tomiotto-Pellissier F, Alves DR, Miranda-Sapla MM et al (2018) Caryocar coriaceum extracts exert leishmanicidal effect acting in promastigote forms by apoptosis-like mechanism and intracellular amastigotes by Nrf2/HO-1/ferritin dependent response and iron depletion: leishmanicidal effect of Caryocar coriaceum leaf ex. Biomed Pharmacother 98:662–672. https://doi.org/10.1016/j.biopha.2017.12.083
Varma A, Alok S, Jain SK (2011) Hypoglycemic activity of Putranjiva roxburghii Wall. in alloxan induced diabetic rats. Int J Pharm Sci Res 2:160–164. https://doi.org/10.13040/IJPSR.0975-8232.2(1).160-64
Zhou SH, Fang ZX, Lü Y et al (2009) Phenolics and antioxidant properties of bayberry (Myrica rubra Sieb. et Zucc.) pomace. Food Chem 112:394–399. https://doi.org/10.1016/j.foodchem.2008.05.104
Acknowledgements
The authors are thankful to the Department of Botany, Panjab University Chandigarh for identifying the plant material. Sophisticated Analytical Instrument Facilities (SAIF)/Central Instrumentation Laboratory (CIL), Panjab University, Chandigarh is acknowledged for GC-MS analysis.
Funding
This work was financially supported by University Grants Commission, New Delhi under UGC-JRF/SRF Fellowship (3643/NET-DEC.2012) and UGC-CAS (F.4–28/2015/CAS-II) (SAP-II).
Author information
Authors and Affiliations
Contributions
PK and DKG carried out the experimental work and wrote the manuscript. PK, DKG, and SK designed the study. SK supervised the experimental study and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors hereby declare that they have no conflicts of interest.
Ethics approval
Ethics committee approval was received for this study from the scientific committee of the Faculty of Science, Panjab University, Chandigarh.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keshav, P., Goyal, D.K. & Kaur, S. GC–MS screening and antiparasitic action of Putranjiva roxburghii leaves against sensitive and resistant strains of Leishmania donovani. J Parasit Dis 45, 1002–1013 (2021). https://doi.org/10.1007/s12639-021-01388-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12639-021-01388-9