Abstract
The search for new therapeutic agents from natural sources has been a constant for the treatment of diseases such as leishmaniasis. Herein, in vitro and in vivo pharmacological activities of pure major phenolic constituents (caffeic acid, chlorogenic acid, ferulic acid, quercetin, and rosmarinic acid) from Pluchea carolinensis against Leishmania amazonensis are presented. Pure compounds showed inhibitory activity against promastigotes (IC50 = 0.2–0.9 μg/mL) and intracellular amastigotes (IC50 = 1.3–2.9 μg/mL). Four of them were selected after testing against macrophages of BALB/c mice: caffeic acid, ferulic acid, quercetin, and rosmarinic acid, with selective indices of 11, 17, 10, and 20, respectively. Ferulic acid, rosmarinic acid, and caffeic acid controlled lesion size development and parasite burden in footpads from BALB/c experimentally infected mice, after five injections of compounds by intralesional route at 30 mg/kg every 4 days. Pure compounds from P. carolinensis demonstrated antileishmanial properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leishmaniasis represents a group of neglected diseases caused by infection with protozoan parasites from the genus Leishmania (Trypanosomatidae) (Bañuls et al. 2011; Soong 2012). Since the high increase of cases and the amount of people living at risk of leishmaniasis, prevention of the disease is an urgent need. Given the complexity of the disease, a single-control strategy is not applicable and efforts have been performed on the different levels of control (Bañuls et al. 2011; Sharma and Sing 2008). Reservoir and vector controls are almost infeasible in endemic areas and they are difficult to monitor (Murray 2000). While prophylactic and therapeutic vaccines are in great need, there is currently no effective immunotherapy for any leishmaniasis form.
Antileishmanial drugs have one or more limitations like unaffordable cost, difficulty in administration, toxic side effects, and more importantly the development of drug resistance (Mishra et al. 2007). The pentavalent antimonials, Pentostam® (sodium stibogluconate) and Glucantime® (meglumine antimoniate), became the first-line drugs to treat all types of leishmaniasis with high cure rate and low toxicity (Mishra et al. 2007). Alternative line drugs include pentamidine, amphotericine B (also in lipid formulations), paromomycin, and miltefosine (Kedzierski et al. 2009). Nevertheless, to date, none of them are proven fully effective against Leishmania parasites, and leishmaniasis became a major health problem (Chan-Bacab and Peña-Rodríguez 2001; Mishra et al. 2007). Therefore, the development of new antileishmanial drugs with the lowest cost and toxicity is an urgent need.
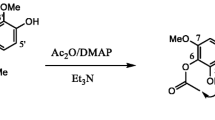
Due to the limited availability of effective pharmaceutical products and the high costs, most of the people living in areas affected by leishmaniasis depend largely of popular treatments and traditional medicine practices. In a previous study, leaf crude extracts from three Cuban Pluchea species (Asteraceae), selected for their ethnomedical uses against skin infections, were evaluated against Leishmania amazonensis (García et al. 2011; Locher et al. 1996; Fatope et al. 2004). In addition, special attention has been focused on the Asteraceae family, where approximately 20 species have been described for their antileishmanial activities (Berger et al. 2001; Fournet et al. 1994; Rocha et al. 2005). Extracts from Pluchea carolinensis (Jacq.) G. Don (Fig. 1) showed the best in vitro and in vivo activities (García et al. 2011). However, as far as we know, the compounds responsible for the antileishmanial activity have not been identified yet. Therefore, in the present study, we report the in vitro and in vivo antileismanial activity of five major compounds that were previously identified in P. carolinensis (Perera 2012): caffeic acid, chlorogenic acid, ferulic acid, quercetin, and rosmarinic acid (Fig. 2).
Material and methods
Parasite
The MHOM/77BR/LTB0016 strain of L. amazonensis was kindly provided by the Department of Immunology, Oswaldo Cruz Foundation (FIOCRUZ), Brazil. Parasites were routinely isolated from the mouse lesions and maintained as promastigotes at 26 °C in Schneider’s medium (Sigma-Aldrich, St. Louis, MO, USA) containing 10 % heat-inactivated fetal bovine serum (HFBS) (Sigma-Aldrich), 100 μg of streptomycin/mL, and 100 U of penicillin/ml.
Tested compounds
Caffeic acid and chlorogenic acid were purchased from Sigma and ferulic acid and rosmarinic acid from Aldrich, while quercetin was purchased from Extrasynthèse. All compounds have >99 % of purity and were dissolved in dimethyl sulfoxide (DMSO) at 2 mg/mL.
Reference drugs
As drug reference, a pentavalent antimonial, meglumine antimoniate (Glucantime®, Rhône-Poulenc Rorer, Mexico), was used at a concentration of 30 mg/mL in sterile distilled water.
Animals
Female BALB/c mice, with body weights of approximately 20 to 22 g, were obtained from The National Centre of Laboratory Animals Production (CENPALAB, Cuba) and maintained according to “Guideline on the Care and Use of Laboratory Animals.” The protocol used for the animal experiments was approved by Ethic Committee from the Institute of Tropical Medicine Pedro Kouri, Havana, Cuba (CEI-IPK 13-10).
In vitro activity
In each well, 50 μL of Schneider’s medium (Sigma, St. Louis, MO, USA) containing 10 % heat-inactivated fetal bovine serum (HFBS), 100 μg of streptomycin/mL, and 100 U of penicillin/mL were added, with an additional 48 μL in the wells of the second column, completed with 2 μL of each compound. Consecutively, ten twofold serial dilutions were carried out, taking 50 μL. Then, 50 μL at 2 × 105 promastigotes/mL were added in each well to evaluate final concentrations of compounds ranging from 0.04 to 20 μg/mL and incubated at 26 °C for 72 h. Colorimetric assays with 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) (Sigma, St. Louis, MO, USA) were used. To cultures, 20 μL of MTT solution (5 mg/mL) in phosphate-buffered saline (PBS), were prepared, filtered, and added in each well. After incubation for an additional 4 h, supernatant was eliminated and the formazan crystals were dissolved by addition of 100 μL DMSO. The optical density was determined using a spectrophotometer Sirio S Reader, 2.4-0 (Italy), at a test wavelength of 560 nm and a reference wavelength of 620 nm (Sladowski et al. 1993). The median inhibitory concentration (IC50) was obtained from concentration-response curves by linear regression. The results were expressed as mean IC50 and standard deviation (SD) of two independent experiments.
The activity against intracellular amastigotes was evaluated following the method previously described by Caio et al (1999). The peritoneal macrophages were harvested and plated in 24-Well Lab-Tek (Costar®, USA) and incubated at 37 °C under an atmosphere of 5 % CO2 for 2 h. Non-adherent cells were removed, and stationary-phase L. amazonensis promastigotes were added in a ratio of 4:1 parasite/macrophage. The cultures were incubated for 4 h and free parasites were removed. Then, 1995 μL of RPMI medium (Sigma, St. Louis, MO, USA) containing 10 % HFBS, 100 μg of streptomycin/mL, and 100 U of penicillin/mL, and 5 μL of the test products dissolved in DMSO were added in duplicate for another 48-h incubation. The cultures were fixed in absolute methanol, stained with Giemsa, and examined under a light microscope. The number of intracellular amastigotes was determined by counting the amastigotes in 100 macrophages per sample and percentage of infected macrophages. Results were expressed as percent of reduction of the infection rate in comparison with the controls. The infection rates were obtained by multiplying the percentage of infected macrophages by the number of amastigotes per infected macrophage. The IC50 values were determined from the linear regression of dose-response curves.
The effect of compounds on the viability of mouse peritoneal macrophages was also determined (Sladowski et al. 1993). Macrophages were collected and incubated as described previously. The medium was removed and 50 μL of RPMI medium (Sigma, St. Louis, MO, USA) containing 10 % HFBS, 100 μg of streptomycin/mL, and 100 U of penicillin/mL was added, with an additional 48 μL in the wells of the second column, completed with 2 μL of each test compound. Then, ten serial dilutions of 1:2 were carried out, and an additional 50 μL of medium was added in each well to obtain final compound concentrations ranging from 0.04 to 20 μg/mL. The plates were incubated at 37 °C for 48 h. Macrophages treated with 1 μL DMSO were included as negative controls. Then, 15 μL of MTT solutions was added and the plate was incubated at same conditions. After 3 h, formazan crystals were dissolved with 100 μL DMSO and optical density was measured. The 50 % cytotoxic concentration (CC50) was determined by dose-response curves. Selectivity indices (SI) were calculated by dividing the CC50 for peritoneal macrophages by the IC50 for L. amazonensis amastigotes.
In vivo activity
On day 0, BALB/c mice were injected subcutaneously in the right hind footpad with 107 stationary-phase L. amazonensis promastigotes. Then, 15 days post-infection (p.i.), the animals were randomly divided into eight groups of eight mice each. Five groups were treated with 0.05 mL of each pure phenolic compounds at a dose of 30 mg/kg dissolved in DMSO: saline solution (20:80, v/v). Two groups were treated with glucantime at 30 mg/kg dissolved in saline solution or vehicle (DMSO: saline solution at 20:80, v/v). Five doses were administered by intralesional route each 4 days. A group of infected and untreated mice was also included.
Animals were observed daily and deaths were recorded. Body weight was monitored weekly. Disease progression was evaluated weekly by measuring footpad swelling of the lesion diameter between 15 and 45 days p.i., using a digital calliper. Average lesion size was calculated as the differences obtained between infected and uninfected footpads. On days 30 and 45 p.i., three animals of each group were killed by cervical dislocation and parasite burden was determined using the culture microtitration method (Buffet et al. 1995). Briefly, a sample of the lesion was excised, weighted, and homogenized in 4 mL of Schneider’s medium. Under sterile conditions, a serial fourfold dilution was prepared in 96-well plates. After 7 days of incubation at 26 °C, plates were examined with an inverted microscope. The final titer was defined as the last dilution for which the well contained at least one parasite. The parasite burden was calculated as follows: parasite burden = (geometric mean of reciprocal titers from each duplicate / weight of homogenized cross section) × 400.
Statistical analyses
Statistical differences between IC50 values of test compounds against promastigotes and amastigotes were demonstrated with the Mann–Whitney test. Data on lesion progression and parasite burden determined by the microtitration method were analyzed for statistical significance by the analysis of variance test, following a post hoc test (LDS test or planned comparison). Significance between groups was classified as p < 0.05 using the STATISTICA for Windows program (release 4.5, StatSoft, Inc. 1993).
Results
In vitro activity
The antileishmanial and cytotoxic activities of five pure compounds from P. carolinensis were first evaluated in vitro. All pure compounds inhibited both promastigotes and intracellular amastigotes, and also showed some cytotoxicity on non-infected peritoneal macrophages (Table 1). The most active compounds against parasites were chlorogenic acid, feluric acid, quercetin, and rosmarinic acid, while the most specific were feluric acid and rosmarinic acid. Glucantime did not cause inhibition of Leishmania promastigotes or BALB/c-mice-derived macrophages.
In vivo activity
In vitro active compounds from P. carolinensis were also evaluated in vivo in an experimental BALB/c mice model of cutaneous leishmaniasis with L. amazonensis. Preliminary studies indicated that intralesional administration of the compounds did not cause death of animals, and no lost of body weight higher than 10 % was observed (Table 2).
Among the compounds evaluated, three of them showed promising results taking into account the gradient of lesion sizes and parasite burden (Fig. 3). Ferulic acid caused the highest and fastest reduction of the lesion size development compared to vehicle or untreated control animals (p < 0.05). In addition, no parasites were observed from infected tissue at 4 weeks p.i., while after 6 weeks p.i., statistical differences (p < 0.05) with respect to control groups were observed. On the other hand, caffeic acid and rosmarinic acid seemed also effective by showing statistical differences (p < 0.05) of lesion size and parasite burden of treated animals compared with vehicle or untreated animals (Fig. 3). The activity of these three pure compounds was also statistically higher (p < 0.05) than glucantime at the end of experiment (week 6 p.i.).
Effect of pure compounds from P. carolinensis on BALB/c mice infected with 107 promastigotes of L. amazonensis in the footpad by subcutaneous route. The results are expressed as mean ± standard deviation. Treatment was started after 2 weeks p.i. Caffeic acid, ferulic acid, quercetin, and rosmarinic acid were administered at a dose of 30 mg/kg dissolved in DMSO:saline solution (20:80, v/v); glucantime at 30 mg/kg dissolved in saline solution at a volume of 0.05 mL. Five doses were administered by intralesional route each 4 days. a Lesion size; b parasite burden. Glucantime is the reference drug; vehicle: 0.05 mL of mix DMSO:saline solution (20:80, v/v); control: infected and untreated mice. Asterisks indicate statistical differences (p < 0.05) with respect to animals treated with vehicle and control
However, quercetin caused a higher lesion size compared to the control animals. After 5 weeks p.i., when the treatment was stopped, the lesion sizes decreased. No statistical difference (p > 0.05) was observed at the end of the experiment. Nevertheless, parasite burdens showed statistical differences (p < 0.05) in 4 and 6 weeks p.i. compared with vehicle or untreated groups, while no difference (p < 0.05) was observed compared to glucantime-treated animals (Fig. 2).
Discussion
For the treatment of leishmaniasis, only a limited number of drugs are available and they possess toxic side effects, and resistance development is still increasing. Therefore, research on new antileishmanial drugs should also focus on natural products (Sales et al. 2012). To overcome some important disadvantages of using plant extracts, like standardization and production process, one can purify the major bioactive compounds. Herein, pure major constituents from P. carolinensis were assayed against L. amazonensis in in vitro and in vivo models.
Chlorogenic acid, quercetin, and rosmarinic acid showed similar antileishmanial activities and were the most effective against promastigotes. However, quercetin and ferulic acid were the most active compounds against intracellular amastigotes. Interestingly, the in vitro values for the antileishmanial activity of the test compounds against both parasite stages showed better results than the reference drug glucantime. Previous studies also demonstrated the activity of other clinical drugs against L. amazonensis. Pentamidine and pentostam showed inhibition of promastigote and amastigote growth with IC50 values of respectively 0.37 μg/mL (García et al. 2012) and 20 μg/mL (Muzitano et al. 2006), while IC50 values of 1.88 μg/mL for ketoconazole and >50 μg/mL for fluconazole against intracellular amastigotes of L. amazonensis have been reported (Kulkarni et al. 2013). In addition, antileishmanial activity of some promising pure compounds isolated from plants has been reported. The antileishmanial potential of the oleanane triterpene saponin (PX-6518), isolated from Maesa balansae, showed IC50 values >50 μg/mL against promastigotes and 1.3 ± 0.4 μg/mL against intracellular amastigotes (Inocencio et al. 2011). In another studies, azadirachtin from Azadirachta indica was inactive against promastigotes and amastigotes of L. amazonensis (Carneiro et al. 2012), while eupomatenoid-5 from Piper rangellii (Vendrametto et al. 2010) and damasine from Ambrosia peruviana (Aponte et al. 2009) showed IC50 values of respectively 13 and 22.6 μg/mL against intracellular amastigotes. Pure compounds isolated from P. carolinensis demonstrated herein better results against promastigote and amastigote growth of L. amazonensis.
In the case of caffeic acid, the antileishmanial activity observed in this study (IC50 = 16.0 ± 1.8 μM) is in concordance with previous results reported: IC50 = 17.8 ± 0.15 μM (Cabanillas et al. 2010). However, in our study, quercetin showed higher activity (IC50 = 4.3 ± 0.3 μM) than previously reported by Fonseca-Silva and collaborators (IC50 = 31.4 μM), which could be related to the strain of L. amazonensis used, as well as different experimental conditions (Fonseca-Silva et al. 2011).
In general, in our study, the inhibitory effect of the test compounds was stronger on promastigotes than on intracellular amastigotes of L. amazonensis. In a promastigote assay, the compounds can interact directly with the parasites growing freely in the culture medium. In an amastigote assay, the compounds need to enter the macrophage before interacting with the parasites. For that reason, in macrophages, compounds can be metabolized or binded to some host cell molecules, resulting in lower antileishmanial activities.
All pure test compounds showed a better activity against the promastigotes and amastigotes than the crude extract of P. carolinensis (IC50promastigotes = 30.4 ± 1.2 μg/mL and IC50amastigotes = 30.9 ± 6.1 μg/mL) (García et al. 2012). This could be explained by the fact that (i) the pure compounds are only present in small quantities in the crude extract or (ii) there is an antagonism action among them in the mixture. Further experiments should be addressed to demonstrate possible interactions between the compounds in the crude extract.
To test the safety of the compounds, non-infected peritoneal BALB/c mice macrophages were treated. The SIs of the test compounds are, in general, low. Nevertheless, they also present a higher selectivity than the crude extract (García et al. 2011). Although quercetin showed the best activity against intracellular amastigotes, the CC50 value was low in comparison to the rest of the test compounds. Since for pure compounds relevant biological efficacy must have a selectivity index of at least 10 (Pink et al. 2005), only four compounds were selected for further evaluation in an animal model. Chlorogenic acid showed a SI < 10 and was therefore not tested in an animal model.
Finally, the effect of the four compounds from P. carolinensis against experimental cutaneous leishmaniasis in BALB/c mice caused by L. amazonensis was evaluated. Administration by intralesional route was selected due to the following: (i) previously in vitro cytotoxicity obtained in our study of the tested products; (ii) absence of previous scientific information related to toxicity of the pure compounds applied in mice by different routes (intravenous, intraperitoneal, or oral); (iii) this technique reduces the dosage of product, as well as the risk of systemic toxicity; and (iv) it is an attractive formulation for the development of new topical drugs for the treatment of cutaneous leishmaniasis (Alkawajah and Larbi 1997; Mishra et al. 2007). In literature, different reports have demonstrated the use of intralesional administration of clinically used drugs, including the glucantime (Salmanpour et al. 2006), sodium stibogluconate (El-Sayed and Anwar 2010), and amphotericin B liposomal (Yardley and Croft 1997).
As preliminary toxicity testing in animals, we desire to comment that evaluated compounds from P. carolinensis did not show body weight loss higher than 10 % and none of the animals died. Ferulic acid presented the highest and fastest control of lesion size growth of infected footpads, compared with vehicle treated or untreated mice. Caffeic acid and rosmarinic acid also showed a promising activity considering the gradient of lesion sizes and parasite burden. Quercetin showed increased values of lesion size during the first 2 weeks of treatment, although statistical differences with respect to the control animals were observed. This could be the consequence of a low absorption of quercetin into subcutaneous tissues. Similar results have been reported for oleo products, such as licochalcona A (Chen et al. 1994) and an essential oil from Chenopodium ambrosioides (Monzote et al. 2007). The three promising compounds selected (caffeic acid, ferulic acid, and rosmarinic acid) showed a better activity when compared with the animals treated with glucantime. In our experiments, glucantime did not demonstrate high antileishmanial effect as a reference drug. However, it is a drug used to treat infections by Leishmania mexicana complex as first option in the New World, and, in our in vitro study, L. amazonensis reference strain was susceptible. Other authors have also reported the low effect of glucantime (Nakayama et al. 2005) in animals experimentally infected with L. amazonensis. This is probably due to the experimental model used in this study, which is extremely susceptible and can be considered a highly stringent model for experimental chemotherapy. BALB/c mice infected with L. amazonensis commonly develop a progressive lesion at the inoculation site, followed by ulceration, visceralization, and metastasis that cause a disseminate infection and “non-cure” and fatal disease (Fournet et al. 1996; Valadares et al. 2012).
In general, the effect of tested compounds in in vivo models could be related with direct antileishmanial activity demonstrated previously, and could also be associated with indirect actions, such as antioxidant, anti-inflammatory, or immunostimulatory activities. For example, Passero and collaborators suggested that fractions with caffeic acid were able to enhance the levels of nitrates that can cause macrophage activation (Passero et al. 2011). Additionally, Kim and collaborators reported that rosmarinic acid could act as an anti-inflammatory compound, which in the context of inflammatory infection diseases, as leishmaniasis, may be relevant (Kim et al. 2008).
Of the test compounds from P. carolinensis, three of them have been selected as potential products to develop new antileishmanial agents according to the in vitro and in vivo results. The most promising compounds were ferulic acid > rosmarinic acid > caffeic acid. Further studies should be performed to develop a formulation with the desired pharmacokinetic and toxicological properties, which could be accessible to endemic population.
Abbreviations
- DMSO:
-
Dimethyl sulfoxide
- HFBS:
-
Heat-inactivated fetal bovine serum
- IC50 :
-
Concentration at which inhibition of the activity was 50 %
- MTT:
-
3-[4,5-Dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide
- PBS:
-
Phosphate-buffered saline
- p.i.:
-
Post-infection
- SD:
-
Standard deviation
- SI:
-
Selectivity indices
- TDR:
-
Tropical Diseases Research
- WHO:
-
World Health Organization
References
Alkawajah AM, Larbi E (1997) Treatment of cutaneous leishmaniasis with antimony: intramuscular versus intralesional administration. Ann Trop Med Parasitol 91:899–905
Aponte JC, Yang H, Vaisberg AJ, Castillo D, Málaga E, Verástegui M, Casson LK, Stivers N, Bates PJ, Rojas R, Fernandez I, Lewis WH, Sarasara C, Sauvain M, Gilman RH, Hammond GB (2009) Cytotoxic and anti-infective sesquiterpenes present in Plagiochila disticha (Plagiochilaceae) and Ambrosia peruviana (Asteraceae). Planta Med 75:1–3
Berger I, Passreiter CM, Cáceres A, Kubelka W (2001) Antiprotozoal activity of Neurolaena lobata. Phytother Res 15:327–330
Buffet PA, Sulahian A, Garin YJ, Nassar N, Derouin F (1995) Culture Microtitration a sensitive method for quantifying Leishmania infantum in tissues of infected mice. Antimicrob Agents Chemother 39:2167–2168
Bañuls AL, Bastien P, Pomares C, Arevalo J, Fisa R, Hide M (2011) Clinical pleiomorphism in human leishmaniases, with special mention of asymptomatic infection. Clin Microbiol Infect 17:1451–1461
Cabanillas BJ, Le Lamer AC, Castillo D, Arevalo J, Rojas R, Odonne G, Bourdy G, Moukarzel B, Sauvain M, Fabre N (2010) Caffeic acid esters and lignans from Piper sanguineispicum. J Nat Prod 73:1884–1890
Caio TSE, Lima MD, Kaplan MAC, Nazareth MM, Rossi-Bergmann B (1999) Selective effect of 2’,6’-dihydroxy-4’methoxychalcone isolated from Piper aduncum on Leishmania amazonensis. Antimicrobial Agents Chemother 43:1234–1241
Carneiro S, Carvalho F, Santana L, Sousa A, Neto J, Chaves M (2012) The cytotoxic and antileishmanial activity of extracts and fractions of leaves and fruits of Azadirachta indica (A Juss.). Biol Res 45:111–116
Chan-Bacab MJ, Peña-Rodríguez MP (2001) Plant natural products with leishmanicidal activity. Nat Prod Rep 18:674–688
Chen M, Christensen SB, Theander TG, Kharazmi A (1994) Antileishmanial activity of licochalcone A in mice infected with Leishmania major and in hamsters infected with Leishmania donovani. Antimicrob Agents Chemother 38:1339–1344
El-Sayed M, Anwar AE (2010) Intralesional sodium stibogluconate alone or its combination with either intramuscular sodium stibogluconate or oral ketoconazole in the treatment of localized cutaneous leishmaniasis: a comparative study. J Eur Acad Dermatol Venereol 24:335–340
Fatope MO, Nair RS, Marwah RG, Al-Nadhiri HHS (2004) New sesquiterpenes from Pluchea Arabica. J Nat Prod 67:1925–1928
Fonseca-Silva F, Inacio JD, Canto-Cavalheiro MM, Almeida-Amaral EE (2011) Reactive oxygen species production and mitochondrial dysfunction contribute to quercetin induced death in Leishmania amazonensis. PLoS One 6:e14666
Fournet A, Barrios AA, Muñoz V (1994) Leishmanicidal and trypanocidal activities of Bolivian medicinal plants. J Ethnopharmacol 41:19–37
Fournet A, Ferreira ME, Rojas A, Torres S, Fuentes S, Nakayama H (1996) In vivo efficacy of oral and intralesional administration of 2-substituted quinolines in experimental treatment of New World cutaneous leishmaniasis caused by Leishmania amazonensis. Antimicrob Agents Chemother 40:2447–2451
García M, Monzote L, Scull R, Herrera P (2012) Activity of Cuban plants extracts against Leishmania amazonensis. ISRN Pharmacology 2012:1–7
García M, Perera WH, Scull R, Monzote L (2011) Antileishmanial assessment of leaf extracts from Pluchea carolinensis, Pluchea odorata and Pluchea rosea.Asian Pacific. J Trop Med 4:836–840
Inocencio R, Vermeersch M, Deschacht M, Hendrick S, Assche T, Cos P, Maes L (2011) In vitro and in vivo prophylactic and curative activity of the triterpene saponin PX-6518 against cutaneous leishmaniasis. J Antimicrob Chemother 66:350–353
Kedzierski L, Sakthianandeswaren A, Curtis JM, Andrews PC, Junk PC, Kedzierka K (2009) Leishmaniasis: current treatment and prospect for new drugs and vaccines. Curr Med Chem 16:599–614
Kim H, Lee J, Lee J, Park Y, Yoon T (2008) Rosmarinic acid down-regulates the LPS-indiced production of monocyte chemoattractant protein-1 (MCP-1) and macrophage inflammatory protein-1α (MIP-1α) via the MAPK pathway in bone-marrow derived dendritic cells. Mol Cells 26:583–589
Kulkarni MM, Reddy N, Gude T, McGwire BS (2013) Voriconazole suppresses the growth of Leishmania species in vitro. Parasitol Res 112(5):2095–2099
Locher CP, Witvrouw M, deBethune MP, Burch MT, Mower HF, Davis H, Lasure A, Pauwels R, deClercq E, Vlietinck AJ (1996) Antiviral activity of Hawaiian medicinal plants against human immunodeficiency virus type-1 (HIV-1). Phytomed 2:259–264
Mishra J, Saxena A, Singh S (2007) Chemotherapy of leishmanisasis: past, present and future. Curr Med Chem 14:1153–1169
Monzote L, Montalvo AM, Scull R, Miranda M, Abreu J (2007) Activity, toxicity and analysis of resistance of essential oil from Chenopodium ambrosioides after intraperitoneal, oral and intralesional administration in BALB/c mice infected with Leishmania amazonensis: a preliminary study. Biomed Pharmacother 61:148–153
Murray HW (2000) Treatment of visceral leishmaniasis (kala-azar): a decade of progress and future approaches. Int J Infect Dis 4:158–177
Muzitano MF, Tinoco LW, Guette C, Kaiser CR, Rossi-Bergmann B, Costa SS (2006) The antileishmanial activity assessment of unusual flavonoids from Kalanchoe pinnata. Phytochem 67:2071–2077
Nakayama H, Loiseau PM, Bories C, Torres S, Schinini A, Serna E, Rojas de Arias A, Fakhfakh MA, Franck X, Figadère B, Hocquemiller R, Fournet A (2005) Efficacy of orally administered 2-substituted quinolines in experimental murine cutaneous and visceral leishmaniases. Antimicrob Agents Chemother 49:4950–4956
Passero LF, Bonfim-Melo A, Corbett CE, Laurenti MD, Toyama MH, de Toyama DO, Romoff P, Fávero OA, dos Grecco SS, Zalewsky CA, Lago JH (2011) Anti-leishmanial effects of purified compounds from aerial parts of Baccharis uncinella C. DC. (Asteraceae). Parasitol Res 108:529–536
Perera W (2012) Isolation and identification of antioxidant phytochemicals from Cuban species of the genera Erythroxylum P. Browne and Pluchea Cass [PhD thesis]. Liege, Belgium: University of Liege, 2012: p 186
Pink R, Hudson A, Mouriés MA, Bendig M (2005) Opportunities and challenges in antiparasitic drug discovery. Nature Rev Drug Discov 4:727–740
Rocha LG, Almeida J, Macedo RO, Barbosa-Filho JM (2005) A review of natural products with antileishmanial activity. Phytomed 12:514–535
Sales D, Silva AL, de Almeida F, de Almeida I, do Socorro M, de Araujo RM (2012) Conventional therapy and promising plant-derived compounds against trypanosomatid parasites. Front Microbiol 3:1–10
Salmanpour R, Razmavar MR, Abtahi N (2006) Comparison of intralesional meglumine antimoniate, cryotherapy and their combination in the treatment of cutaneous leishmaniasis. Int J Dermatol 45:1115–1116
Sharma U, Sing S (2008) Insect vectors of Leishmania: distribution, physiology and their control. J Vector Borne Dis 45:255–272
Sladowski D, Steer SJ, Clothier RH, Balls M (1993) An improve MTT assay. J Immunol Methods 157:203–207
Soong L (2012) Subversion and utilization of host innate defense by Leishmania amazonensis. Front Immunol 3:1–7
Valadares DG, Duarte MC, Ramírez L, Chávez-Fumagalli MA, Lage PS, Martins VT, Costa LE, Ribeiro TG, Régis WCB, Soto M, Fernandes AP, Tavares CAP, Coelho EAF (2012) Therapeutic efficacy induced by the oral administration of Agaricus blazei Murill against Leishmania amazonensis. Parasitol Res 111(4):1807–1816
Vendrametto MC, Oliveira A, Nakamura CV, Prado B, Garcia DA, Ueda-Nakamura T (2010) Evaluation of antileishmanial activity of eupomatenoid-5, a compound isolated from leaves of Piper regnellii var. pallescens. Parasitol Int 59:154–158
Yardley V, Croft SL (1997) Activity of liposomal amphotericin B against experimental cutaneous leishmaniasis. Antimicrob Agents Chemother 41:752–756
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Montrieux, E., Perera, W.H., García, M. et al. In vitro and in vivo activity of major constituents from Pluchea carolinensis against Leishmania amazonensis . Parasitol Res 113, 2925–2932 (2014). https://doi.org/10.1007/s00436-014-3954-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-014-3954-1