Abstract
Objectives
To investigate the association between frailty status and risk of fall among middle-aged and older Chinese people.
Design
A nationally representative prospective cohort study.
Setting and Participants
The study included 13,877 community-dwelling participants aged 45 years and above from the China Health and Retirement Longitudinal Study.
Methods
Frailty status was identified by the frailty index of health deficit accumulation. 34 variables at baseline were selected to calculate the frailty index. We excluded participants with incomplete information in construction of the frailty index at baseline. Falls were measured based on the respondents’ self-report. We used a logistic regression model to estimate the associations between the frailty status and risk of fall, and subgroup analyses and sensitivity analyses were further conducted.
Results
Of 13,877 participants, 2310 (16.6%) had falls during the observation period. 9027 (65.0%) participants were classified as robust, 4019 (29.0%) participants were classified as pre-frail, and 831 (6.0%) participants were classified as frail. Our results indicated per 0.01 increment in the frailty index was significantly associated with an increased risk of fall among middle-aged and older participants (OR: 1.52, 95%CI: 1.45–1.60). Such association was stronger when frailty was presented as a categorical variable, with an OR of 1.75 (95%CI: 1.59–1.93) for pre-frail and 3.04 (95%CI: 2.60–3.56) for frail. The area under the curve of the logistic model was 0.612 (95%CI: 0.600–0.625). Each 0.01 increment of the frailty index was association with a higher risk of fall among middle-aged (45–59years) participants (OR: 1.44, 95%CI: 1.29–1.60) than among older (≥60 years) participants (OR: 1.28, 95%CI: 1.16–1.41) at baseline (p=0.015 for interaction).
Conclusion
Frailty was significantly associated with an increased risk of fall among community-dwelling middle-aged and older people in China. It is necessary to screen and recognize frailty status to prevent falls among middle-aged and older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
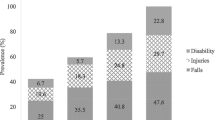
With the population ageing rapidly, falls have become one of the significant public health problem worldwide (1,2). In 2019, 703 million people reached 65 years old or above in the world, and an estimated number of older people is projected to 1.5 billion in 2050 (3). Approximately one-third community-dwelling adults aged 65 years and above and one-half of adults older than 85 years of age are reported falls each year (4). Globally, it was estimated falls as the second leading cause of death from unintentional injuries after road traffic injuries (5). In addition to death, falls can result in limited mobility, fractures, disabilities, and hospitalization (6,7). Moreover, falls are likely to compromise quality of life and cause large consumption of medical resources (8,9). In China, falls are the leading cause of injury death in the elderly (10). According to the Global Burden of Disease Study, the incidence, mortality, and disability-adjusted-life-years for falls among Chinese people increased from 1990 to 2017 (11). Falls have a huge impact on the burden of disease among the middle-aged population, which are the second leading cause of injury deaths among middle-aged people. In addition, a majority of studies on the associations between frailty index and risk of fall were conducted among older people (over 60 years), resulting in limited evidence regarding the middle-aged population. Therefore, it is necessary to investigate the risk factors of falls in the middle-aged and older people.
Frailty is an age-related biological syndrome characterized by a reduction of physiologic reserve and an increase of vulnerability to stressors, which is strongly associated with adverse health outcomes, such as disability, delirium, and hospitalization (12). With the acceleration of aging, frailty, as a comprehensive index to measure the physiology, function and psychology of the elderly, has been as focal points of academic circles. A previous systematic review reported the prevalence of frailty in community-dwelling adults aged 65 years and above was ranging from 4.0% to 59.1% (13). Frailty index is the most widely used method for assessing frailty status, which is also called deficits accumulation index (14).
Previous studies showed an association of frailty with incidence of falls in the elderly (15,16). However, most of these studies were carried out in developed countries. Studies on the association between frailty and falls are scanty in China, and most of them were limited to single-centered (17) and cross-sectional design (18). There is a lack of nationally representative longitudinal studies. Thus, in this study, we aim to investigate the association between frailty index and risk of fall among middle-aged and older adults by using data of the China Health and Retirement Longitudinal Study (CHARLS).
Methods
Study design and Sampling
The study data was obtained from the CHARLS, an ongoing nationally representative cohort study of the residents in mainland China aged 45 years and above. Further details of the study design have been described elsewhere (19). Briefly, a total of 17,708 respondents in 10,257 households were chosen in 28 provinces, 150 country-level units and 450 urban communities/villages, using a multi-stage stratified probability-proportional-to-size random sampling strategy. The baseline survey was conducted in June 2011 with a response rate of 80.5%, and follow-up surveys were carried out every two years subsequently (i.e. wave 2 in 2013, wave 3 in 2015 and wave 4 in 2018, respectively). Face-to-face computer assisted personal interview was adopted by trained staff using a standardized questionnaire on sociodemographic characteristics, lifestyle factors, mental and physical health status, and physical measurements. The CHARLS study had been reviewed and approved by the Institutional Review Board (IRB) at Peking University.
As the study progressed, new samples were added to the study in each wave to ensure the sample fully represent those aged 45 years and above. The CHARLS baseline data was used to calculate the frailty index while fall information was obtained from the CHARLS follow-up data. Because the dates of falls were not available, analyses were performed only using the data for falls during the two or three years of follow-up. We constructed a special dynamic cohort, including three groups. In group I, baseline data were from wave 1 (2011), and fall information was from wave 2 (2013); in group II, new participants were added from the refresher sample in wave 2 (2013), making wave 2 as their baseline data, and fall information was from wave 3 (2015); and in group III, new participants were added from the refresher sample in wave 3 (2015), making wave 3 as their baseline data, and fall information was from wave 4 (2018) (Figure 1).
Measures
Frailty
Frailty status was measured by a frailty index, which was calculated by baseline deficits accumulation in health of each participant. The frailty index was constructed following a standard procedure (20). These deficits associated with health status included the following basic criteria: 1) The deficit covers a range of body systems; 2) the prevalence of the deficit generally increases with age; 3) the baseline prevalence of the deficit is more than 0.5% in the CHARLS study; and 4) the deficit does not saturate too early.
According to the CHARLS data and previous studies (21–23), we selected 34 variables at baseline to calculate the frailty index covering symptoms, body functions, disabilities, medical condition, and activities of daily living (Supplementary Table 1 in the Appendix). The deficit was dichotomized into 0 and 1 if the deficit was binary variables, with ‘0’ referring to no deficit and ‘1’ referring to the maximum deficit. For activities of daily living variable, the deficit was mapped into the 0–1 interval, where we assigned a 0 for the answer ‘have no difficulty’, 0.33 for ‘have difficulty but can still do it’, 0.67 for ‘have difficulty and need help’, and 1 for ‘cannot do it’. For each participant, the frailty index was calculated by dividing the total number of the deficit in a person by 34 deficits considered. For example, if six deficits (each of four deficits scored 1 point and each of two deficits scored 0.67 point) were present in a participant, the frailty index would be (4×1+2×0.67)/34=0.16. Frailty states were divided into three level with the reference of previous study (21,24,25): frailty index ≤0.10 denoted the robust, frailty index >0.1 to <0.25 denoted pre-frail, and frailty index ≥0.25 denotes frail.
Fall
The outcome of interest in the present study was fall in Chinese adults aged 45 years and above, which was assessed by the following single question: ‘have you fallen down in the last two years?’ Participants were asked to answer ‘Yes’ or ‘No’ (coding 1 or 0).
Covariates
Sociodemographic information, lifestyle and health related factors were collected at baseline. Age was categorized as 45–59 and ≥60 years. Educational level was divided into four groups: no formal education, elementary school, middle or high school, and college or above. Marital status was classified as married and other status (divorced, widowed, and single). Lifestyle included smoking (current, past, or never) and drinking status (>1 per month, ≤1 per month, or no). Health related factors included comorbidity, history of medication use (hypertension medications, diabetes medications, psychotropic medications), history of falls, eyesight, hearing, balanced performance (semitandem stand and full-tandem stand) and body mass index (BMI). BMI was calculated as weight in kilograms divided by the square of height in meters.
Statistical analysis
Data were presented as means (standard deviation, SD) for normally distributed continuous variables, and as medians (interquartile range, IQR) for non-normally distributed continuous variables. Categorical variables were presented as frequency with percentage (%). We described and compared the baseline characteristics of participants according to three categories of frailty status (robust, pre-frail, and frail) using the Chi-square test for categorical variables and analysis of variance or the Kruskal-Wallis test for continuous variables where appropriate. We excluded participants with incomplete information in construction of the frailty index and younger than 45 years at baseline. For missing data, it was assumed that the data were missing at random, and then, multiple imputation of chained equations strategy was performed by using other baseline variates. Ten imputed datasets were created and the results were pooled using Stata software version 14.0 command “mi estimate”. To examine the association between frailty index and risk of fall, a series of logistic regression models were applied to calculated the odds ratio (OR) with 95% confidence interval (95% CI), with or without adjustment. Three models were built: in model 1, only frailty was included; in model 2, age and gender were adjusted; in model 3, the variables in model 2 plus residence, educational level, marital status, smoking, alcohol use, comorbidity, history of medication use, history of falls, eyesight, hearing, BMI, balance performance, follow-up period and group were adjusted. The receiver operating characteristic (ROC) curve was constructed to calculated the area under the curve (AUC) in order to evaluate frailty index’s ability to predict risk of fall.
Subgroup analyses were conducted to investigate whether the potential association between frailty and risk of fall was affected by age (middle-aged: 45–59 vs. older: ≥60 years), gender (male vs. female), residence (rural vs. urban), marital status (married vs. others), history of falls (yes vs. no), alcohol use (>1 per month vs. ≤ 1 per month vs. don’t use), hypertension medications use (yes vs. no), diabetes medications use (yes vs. no). We used interaction terms (frailty was regarded as a continuous variable) and generalized hausman test (frailty was regarded as a categorical variable) to evaluate p values for interaction. Sensitivity analyses of different cutoff points of the frailty index (robust: ≤0.1; pre-frail: 0.1–0.21; frail: ≥0.21) were also conducted to evaluate the association results between frailty status and risk of fall.
All statistical analyses were performed using Stata software version 14.0 (Stata Corp, College Station, Texas). P values were two-sided test, with a less than 0.05 to be considered statistically significant.
Results
Baseline characteristics of participants
The ROC curve showed a fair accuracy of frailty index predicted risk of fall with an AUC of 0.612 (95%CI: 0.600–0.625). Of the 13,877 middle-aged and older participants in the analysis, 12,109 from group I, 1528 from group II, and 240 from group III. 9027 (65.0%) adults were classified as robust, 4019 (29.0%) adults were classified as pre-frail, and 831 (6.0%) adults were classified as frail. The mean frailty index was 0.092±0.086. Their mean BMI was 23.51±3.63 kg/m2. The mean age of participants at baseline was 58.71±9.41 years. About three fifths (59.1%) of participants were aged younger than 60 years, and about half (48.6%) of the participants were male. Table 1 illustrated baseline characteristics of participants according to frailty status in this study. Frail persons were more likely to be older, be female, have no formal education, live in rural areas, be unmarried, be former and never smokers, be nondrinkers, have comorbidity, use medication for hypertension, diabetes and psychiatric illnesses, have a history of falls, wear glasses or corrective lenses, have poor hearing, and bad balance performance (keep semi-tandem stand for less than 10s or keep full-tandem stand for less than 30s/60s) at baseline.
Frailty status and risk of fall
Of the 13,877 included participants, 2310 (16.6%) had falls during the observation period. The incidence rate of falls was 13.3% among robust participants, 21.1% among pre-frail participants and 31.8% among frail participants. Table 2 showed that frailty status was significantly associated with risk of fall in all models. In the univariate analysis (model 1), when frailty was regarded as a continuous variable, the OR for risk of fall was 1.52 (95%CI: 1.45–1.60) per 0.01 increment of the frailty index. When frailty was regarded as a categorical variable (frail, pre-frail, and robust), compared with robust group, pre-frail group had a higher risk of fall (OR: 1.75, 95%CI: 1.59–1.93), similar as frail group (OR: 3.04, 95%CI: 2.60–3.56). In the multivariate analysis (model 3), the OR for risk of fall was 1.35 (95%CI: 1.26–1.45) per 0.01 increase of the frailty index. Compared with robust group, pre-frail group and frail group had a 37% and 97% higher risk of fall, respectively (OR: 1.37, 95%CI: 1.21–1.55 for pre-frail group; OR: 1.97, 95%CI: 1.59–2.44 for frail group).
Subgroup analyses
Figure 2 showed the results of the association between frailty status and risk of fall stratified by other potential risk factors. When frailty status was considered as a continuous variable (Figure 2-A), we found that the association was stronger among middle-aged participants (OR: 1.44, 95%CI: 1.29–1.60) than older participants (OR: 1.28, 95%CI: 1.16–1.41) at baseline (p=0.015 for interaction). Frailty status was associated with a higher risk of falls in participants with no history of falls (OR: 1.41, 95%CI: 1.30–1.53), compared with those with a history of falls (OR: 1.23, 95%CI: 1.08–1.39) at baseline (p=0.006 for interaction). However, when frailty status was considered as a categorical variable (Figure 2-B), we could not see any statistically significant heterogeneity in all subgroups (p>0.05 for interaction).
Association between Frailty and Risk of Fall Stratified by Different Factors
OR, odds ratio. 95%CI, 95% confidence interval; Model adjusted age, gender, residence, educational level, marital status, smoking, alcohol use, comorbidity, history of medication use, history of falls, eyesight, hearing, BMI, balance performance, follow up period and group. A: continuous variable. B1 and B2: categorical variable, taking robust as reference.
Sensitivity analyses
In sensitivity analyses, the results had marginal changes after replacing the cutoff point of frailty to 0.21. In the multivariate analysis, the OR for risk of fall was 1.35 (95%CI: 1.26–1.45) per 0.01 increase of the frailty index. Compared with robust group, both pre-frail group (OR: 1.34, 95%CI: 1.18–1.51) and frail group (OR: 1.87, 95%CI: 1.56–2.25) had higher risks of fall (Table 3).
Discussion
This study investigated the association between frailty status and risk of fall in a nationally representative longitudinal study of 13,877 participants aged 45 years and above. At baseline, the prevalence of frailty was 6.2% by using the measurement method of frailty index. At follow up, 16.5% of the participants experienced falls. The major finding of our study showed that there was a statistically significant association between frailty status and risk of fall among middle-aged and older adults in China. Each 0.01 increase of the frailty index was significantly associated with a higher risk of fall among middle-aged participants (45–59 years) than older participants (60 years and older).
The frailty index was developed based on the theory of health deficit accumulation, combing a variety of complex health information into a single indicator, which could break the limitations of describing health status by using a single variable. The frailty index model was widely used in developed countries to evaluate the frailty status of the elderly, which has been proved to be reliable and valid (26). Furthermore, frailty index also had good repeatability. Although different countries used different data to evaluate the frailty status of the elderly by frailty index method, nearly all of the studies got the similar results (27). Previous studies also proved the validity of the frailty index model among adults aged 55 years and older in China (28). There is no international consensus for the health-related variables used to construct frailty index, although 30–40 variables included in an index have been proposed to accurately predict adverse outcomes (29). Hence we selected 34 variables to construct the frailty index. According to different levels of frailty, the general information of participants was analyzed. The results showed a higher level of frailty in female than in male, consistent with the findings of former studies (21,30). Participants who had a history of falls were frailer than those who had not. For example, Fang et al (17) found that the frailty index of the elderly with recurrent falls was significantly higher than those without falls (0.15±0.08 vs 0.09±0.07). The prevalence of frailty was 9.7% in adults aged 60 years and above. A study including seven cities reported similar results to our study, with the overall weighted frailty prevalence of 9.9% among Chinese population in the community aged 60 years and above (31).
In our study, logistic regression was used to analyze the relationship between frailty status and risk of fall. The results showed that frailty was associated with an increased risk of fall, even after adjusting for baseline covariates such as sociodemographic characteristics and lifestyle and health related factors. A Canadian study of nearly 4000 women aged 55 years and over, using 34 health deficits to construct a frailty index, found that per 0.01 increment in the frailty index was significantly associated with an increased risk of fall during short term of follow up (OR:1.02, 95%CI:1.02–1.03) (32), which showed similar results to our study. Moreover, a meta-analysis including 68,723 older individuals also found that frailty (OR:1.84, 95% CI:1.43–2.38) and pre-frailty (OR:1.25, 95%CI:1.01–1.53) were significantly associated with higher risks of fall, respectively (33). The results of the association between frailty index and risk of fall in subgroup analysis showed that frail middle-aged people aged 45–59 years were more vulnerable to fall, which suggested that the middle-aged population should also be the targeted population for frailty intervention in addition to the elderly population. The prevention and treatment of frailty is still in the exploratory stage, and clinical trials of frailty intervention are sparse, such as medication management (34), exercise and nutrition support (35). However, early identification and intervention of frailty are important to prevent falls. Compared with other studies (22,32), the present study used specific cutoff points to define frailty. Sensitivity analysis suggested that the relationship between frailty and risk of fall was not affected by slight fluctuations in cutoff points of frailty. However, the frailty cutoff point of Chinese population is still required to be validated in future research.
The mechanisms that underlie the association of frailty with increased risks of fall have been proposed. Balance and gait disorders are typical features of frailty and are major risk factors for falls (12). Moreover, frailty is often accompanied by muscle weakness, decreased bone mineral density, and chronic disease (36). All of these symptoms are likely to increase the risk of fall (37,38).
There are several strengths in our study. First, this study was a nationally representative prospective cohort study of participants aged 45 years and over. Results in our study could be used as a reference to prevent falls among middle-aged and older people living in community in China. Second, the method of health deficit accumulation was used to calculate the frailty index, and continuous index can be used to analyze the trend association. Third, this study included a new sample from each follow-up, which increased the sample size and ensured the representativeness of the population aged 45 years and older. Considering the heterogeneity among samples in different periods, we adjusted the enrollment year and follow-up period in the analysis to reduce bias. Meanwhile, we acknowledge some limitations. First, similar to previous large-scale studies (32), the data for falls was collected by respondents’ self-report. However, the validity of self-reported fall in the CHARLS study has been confirmed only by examining the relationship of balanced performance and falls (39). Second, some confounding factors of the association of frailty with incident fall, such as physical environment, sarcopenia, and nutrients intake were not adjusted in our study. Because these variables were not available in CHARLS data. In addition, dates for falls and frequency of falls were also unavailable. Finally, the response rate is 80.5% at baseline, which may have slight impact on our findings. However, CHARLS, a first nationally representative survey of the middle-aged and older population, has a high-quality data (19).
Conclusion
In conclusion, the frailty index of deficit accumulation is significantly associated with an increased risk of fall among community-dwelling middle-aged and older people in China. It is necessary to integrate the frailty evaluation in routine clinical practice and community-based physical examination of middle-aged and older people. Timely screening and recognition of frailty are urgent to prevent falls among middle-aged and older adults.
References
World Health Organization. WHO global report on falls prevention in older age. Geneva: World Health Organization. 2008. Available at: https://www.who.int/ageing/publications/Falls_prevention7March.pdf. Accessed February 1, 2021.
Stewart WJ, Kowal P, Hestekin H et al. Prevalence, risk factors and disability associated with fall-related injury in older adults in low- and middle-incomecountries: results from the WHO Study on global AGEing and adult health (SAGE). Bmc Med. 2015;13:147. https://doi.org/10.1186/s12916-015-0390-8.
United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). 2019. Available at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf. Accessed February 3, 2021.
World Health Organization. World report on ageing and health. 2015. Available at: https://www.who.int/ageing/publications/world-report-2015/en/. Accessed February 3, 2021.
Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–1922. https://doi.org/10.1016/S0140-6736(18)32335-3.
Jin J. Prevention of Falls in Older Adults. JAMA. 2018;319(16):1734. https://doi.org/10.1001/jama.2018.4396.
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–93. https://doi.org/10.1016/S0140-6736(05)67604-0.
Pandya C, Magnuson A, Dale W et al. Association of falls with health-related quality of life (HRQOL) in older cancer survivors: A population based study. J Geriatr Oncol. 2016;7(3):201–10. https://doi.org/10.1016/j.jgo.2016.01.007.
Florence CS, Bergen G, Atherly A et al. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018;66(4):693–698. https://doi.org/10.1111/jgs.15304.
Zhiming L, Pengpeng Y, Yuan W, Leilei D, Yuliang E. Characteristics of Falls Among Older People -China, 2018. China CDC Weekly. 2021;3(4):65–68. https://doi.org/10.46234/ccdcw2021.013.
Leilei D, Pengpeng Y, Haagsma JA et al. The burden of injury in China, 1990–2017: findings from the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4(9):e449–e461. https://doi.org/10.1016/S2468-2667(19)30125-2.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. https://doi.org/10.1016/S0140-6736(12)62167-9.
Collard RM, Boter H, Schoevers RA, Oude VR. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92. https://doi.org/10.1111/j.1532-5415.2012.04054.x.
Rockwood K. What would make a definition of frailty successful? Age Ageing. 2005;34(5):432–4. https://doi.org/10.1093/ageing/afi146.
Kojima G. Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2015;16(12):1027–33. https://doi.org/10.1016/j.jamda.2015.06.018.
Vries OJ, Peeters GM, Lips P, Deeg DJ. Does frailty predict increased risk of falls and fractures? A prospective population-based study. Osteoporos Int. 2013;24(9):2397–403. https://doi.org/10.1007/s00198-013-2303-z.
Fang X, Shi J, Song X et al. Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing Longitudinal Study of Aging. J Nutr Health Aging. 2012;16(10):903–7. https://doi.org/10.1007/s12603-012-0368-6.
Cai Y, Xu W, Xiao H, Liu H, Chen T. Correlation between Frailty and Adverse Outcomes Among Older Community-Dwelling Chinese Adults: The China Health and Retirement Longitudinal Study. J Nutr Health Aging. 2020;24(7):752–757.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8. https://doi.org/10.1007/s12603-020-1368-6.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. Bmc Geriatr. 2008;8:24. https://doi.org/10.1186/1471-2318-8-24.
Fan J, Yu C, Guo Y et al. Frailty index and all-cause and cause-specific mortality in Chinese adults: a prospective cohort study. Lancet Public Health. 2020;5(12):e650–e660. https://doi.org/10.1016/S2468-2667(20)30113-4.
Wang X, Chen Z, Li Z et al. Association between frailty and risk of fall among diabetic patients. Endocr Connect. 2020;9(10):1057–1064. https://doi.org/10.1530/EC-20-0405.
Gu Y, Wu W, Bai J et al. Association between the number of teeth and frailty among Chinese older adults: a nationwide cross-sectional study. Bmj Open. 2019;9(10):e029929. https://doi.org/10.1136/bmjopen-2019-029929.
Hoogendijk EO, Afilalo J, Ensrud KE et al. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-6.
Zhang J, Xu L, Sun L, Li J, Qin W. Gender difference in the association of frailty and health care utilization among Chinese older adults: results from a population-based study. Aging Clin Exp Res. 2020;32(10):1985–1991. https://doi.org/10.1007/s40520-019-01410-4.
Apostolo J, Cooke R, Bobrowicz-Campos E et al. Predicting risk and outcomes for frail older adults: an umbrella review of frailty screening tools. JBI Database System Rev Implement Rep. 2017;15(4):1154–1208. https://doi.org/10.11124/JBISRIR-2016-003018.
Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200. https://doi.org/10.1093/ageing/afx162.
Shi J, Song X, Yu P et al. Analysis of frailty and survival from late middle age in the Beijing Longitudinal Study of Aging. Bmc Geriatr. 2011;11:17. https://doi.org/10.1186/1471-2318-11-17.
Mitnitski A, Song X, Skoog I et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc. 2005;53(12):2184–9. https://doi.org/10.1111/j.1532-5415.2005.00506.x.
Schoufour JD, Erler NS, Jaspers L et al. Design of a frailty index among community living middle-aged and older people: The Rotterdam study. Maturitas. 2017;97:14–20. https://doi.org/10.1016/j.maturitas.2016.12.002.
Ma L, Tang Z, Zhang L et al. Prevalence of Frailty and Associated Factors in the Community-Dwelling Population of China. J Am Geriatr Soc. 2018;66(3):559–564. https://doi.org/10.1111/jgs.15214.
Li G, Ioannidis G, Pickard L et al. Frailty index of deficit accumulation and falls: data from the Global Longitudinal Study of Osteoporosis in Women (GLOW) Hamilton cohort. BMC Musculoskelet Disord. 2014;15:185. https://doi.org/10.1186/1471-2474-15-185.
Kojima G. Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2015;16(12):1027–33. https://doi.org/10.1016/j.jamda.2015.06.018.
Herr M, Robine JM, Pinot J, Arvieu JJ, Ankri J. Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol Drug Saf. 2015;24(6):637–46. https://doi.org/10.1002/pds.3772.
Landi F, Cesari M, Calvani R et al. The “Sarcopenia and Physical fRailty IN older people: multi-componenT Treatment strategies” (SPRINTT) randomized controlled trial: design and methods. Aging Clin Exp Res. 2017;29(1):89–100. https://doi.org/10.1007/s40520-016-0715-2.
Makizako H, Kubozono T, Kiyama R et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr Gerontol Int. 2019;19(1):76–80. https://doi.org/10.1111/ggi.13571.
Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327(7417):712–7. https://doi.org/10.1136/bmj.327.7417.712.
Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–9. https://doi.org/10.1111/j.1532-5415.2004.52310.x.
Ouyang P, Sun W. The association between depressive symptoms and fall accidents among middle-aged and elderly people in China. Environ Health Prev Med. 2018;23(1):42. https://doi.org/10.1186/s12199-018-0735-y.
Acknowledgements
None.
Funding
Funding: None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Statement of contribution: Study concept and design: Zhiming Lu, Xiao Deng, Leilei Duan; acquisition of data: Zhiming Lu, Yuliang Er, Xiao Deng; analysis and interpretation of data: Zhiming Lu, Ye Jin, Pengpeng Ye; drafting of the manuscript: Zhiming Lu, Yongle Zhan, Leilei Duan, Ye Jin; critical revision of the manuscript for important intellectual content: Leilei Duan, Pengpeng Ye, Yongle Zhan
Disclosure of Interest Statement: All authors have no declarations of interest to report.
Ethical Standards: All participants provided informed consent, and the protocol was approved by the Ethical Review Committee of Peking University.
Supporting information
Rights and permissions
About this article
Cite this article
Lu, Z., Er, Y., Zhan, Y. et al. Association of Frailty Status with Risk of Fall among Middle-Aged and Older Adults in China: A Nationally Representative Cohort Study. J Nutr Health Aging 25, 985–992 (2021). https://doi.org/10.1007/s12603-021-1655-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1655-x