Abstract
Background
Data supporting a link between frailty and risk of falls is mostly confined to individuals living in urban centers, where risk factors and lifestyles are different from that of rural settings.
Objective
To assess the association between frailty and risk of falls in older adults living in rural Ecuador.
Design
Population-based cross-sectional study.
Participants
Community-dwellers aged ≥60 years living in a rural Ecuadorian village, in whom frail status and risk of falls were assessed.
Measurements
Frailty was evaluated by the Edmonton Frailty Scale (EFS) and risk of falls by the Downton Fall Risk Index (DFRI). Multivariate models were fitted to evaluate whether frailty was associated with risk of falls (dependent variable), after adjusting for demographics, alcohol intake, cardiovascular risk factors, sleep quality, symptoms of depression, and history of an overt stroke. Correlation coefficients were constructed to assess confounders modifying this association.
Results
A total of 324 participants (mean age: 70.5±8 years) were included. The mean EFS score was 4.4±2.5 points, with 180 (56%) participants classified as robust, 76 (23%) as pre-frail and 68 (21%) as frail. The DFRI was positive in 87 (27%) participants. In univariate analysis, the EFS score was higher among participants with a positive DFRI (p<0.001). The number of frail individuals was higher (p<0.001), while that of robust individuals was lower (p<0.001) among those with a positive DFRI. Adjusted logistic regression models showed no association between frailty and the DFRI. Correlation coefficients showed that age, high glucose levels, and history of an overt stroke tempered the association between frailty and the risk of falls found in univariate analyses.
Conclusions
Frailty is not independently associated with risk of falls in older adults living in a remote rural setting. Further studies are needed to assess the impact of frailty on the risk of falls in these populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a geriatric state of vulnerability or reduced functional reserve, characterized by slow walking speed, muscle weakness, low levels of physical activity and, in some cases, cognitive impairment not related to neurodegenerative disorders (1). This condition has become a major public health problem in older adults, mostly because of its association with increased risks for hospitalization, institutionalization, systemic diseases, and all-cause mortality (2, 3). On the other hand, accidental falls are a leading cause of fatal and non-fatal injuries among older adults, with direct medical costs exceeding $30 billion dollars per year in the US only (4).
There is evidence supporting a link between frailty and risk of falls. A recent meta-analysis of 10 studies showed that the risk of falls in frail community dwelling adults aged ≥65 years is higher than in their robust counterparts (5). Other meta-analyses also showed a significant relationship between frailty status and risk of falls (6, 7). However, all these meta-analyses suffered from limitations due to inconsistencies among the included studies, which were partly related to heterogeneity in study designs (mainly because of the use of different questionnaires to identify frailty, and the confounders used for adjustment in individual studies). Moreover, with the exception of a few studies (8), data came from people living in urban or industrialized centers, where risk factors and lifestyles are totally different from that of rural settings. More information is needed before concluding that frail individuals are at an increased risk of falls in these remote communities. In this study, we aimed to assess whether a frail or pre-frail status is associated with an increased risk of falls among older adults living in rural Ecuador.
Methods
Study population
Atahualpa is a rural Ecuadorian village where previous studies on frailty have been conducted (9, 10). As detailed elsewhere, inhabitants are homogeneous regarding ethnicity, diet, and lifestyles (11). The study population included Atahualpa residents aged ≥60 years — identified during door-to-door surveys — in whom the frail status and the risk of future falls were assessed. The I.R.B. of Hospital-Clínica Kennedy, Guayaquil, Ecuador (FWA 00006867) approved the study.
Frailty assessment
Frailty was evaluated by the use of the Edmonton Frail Scale (EFS), a reliable instrument that consists of 10 domains with 11 items including cognition (the clock drawing test, 2 points), general health status (number of hospitalizations during the past year, 2 points and self-reported health status, 2 points), functional independence (from eight independent activities of daily living, 2 points), social support (count on someone who is willing and able to meet the subject’s needs when the subject needs help, 2 points), medication use (five or more prescription medications, 1 point and forgetfulness for taking medications, 1 point), nutrition (weight loss, 1 point), mood (depression, 1 point), incontinence (1 point), and balance and motility (the “Timed Get Up and Go” test, 2 points) (12). The maximum total score is 17, and individuals were classified into three categories including robust (0 to 4 points), apparently vulnerable or pre-frail (5 to 6 points) and frail (≥7 points) (13). The stratification of the EFS score in the three aforementioned groups was according to the recommendations of the reproducibility of the EFS in a Latin American elderly population (which is closely related to the current study population) (13). Also, same cutoffs have been used in previous studies on the correlates of the EFS conducted by our group (9, 10).
Risk of future falls
The Downton Fall Risk Index (DFRI) was used to assess the risk of future falls. The DFRI is a five-item questionnaire inquiring about history of previous falls, use of specific medications (tranquilizers/sedatives, non-diuretic anti-hypertensives, diuretics, anti-parkinsonians, and antidepressants), sensory or motor deficits (visual impairment, hearing impairment, paresis), gait abnormalities (with or without aid), and confusion (14, 15). Using the DFRI, a score ≥3 is considered positive (high risk of future falls). In a previous study from the Atahualpa Project, we used the DFRI, and conducted sensitivity analysis to assess its reliability in its residents. In that previously published study, we found a reasonable reliability of the DFRI in our population (16).
Covariables investigated
Demographics (age, sex, scholarity), alcohol intake (dichotomized in <50 and ≥50 g per day), cardiovascular risk factors, sleep quality, symptoms of depression, and history of an overt stroke were selected as confounding variables. These relevant confounders were assessed by means of procedures and interviews previously described in the Atahualpa Project. We used the American Heart Association criteria to assess physical activity, the body mass index, blood pressure, and fasting glucose (17, 18). Sleep quality was assessed by the use of the Pittsburgh Sleep Quality Index, which is basically used to differentiate between “good” and “poor” sleepers. The instrument consists of 19 items grouped into seven components (assessment of sleep duration, sleep disturbances, sleep latency, daytime dysfunction due to sleepiness, sleep efficiency, overall sleep quality, and medications needed to sleep), each weighted on a 0 to 3 scale, for a total score of 21 points (19). Symptoms of depression were assessed by the depression axis of the depression-anxiety-stress-21 scale, a validated field instrument that measures dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia (20). To recognize patients with overt strokes, rural doctors screened all participants with the use of a validated field instrument, and then, certified neurologists confirmed the diagnosis with the aid of MRI (21).
Statistical analyses
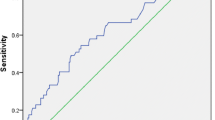
Data analyses are carried out by using STATA version 15 (College Station, TX, USA). In univariate analyses, continuous variables were compared by linear models and categorical variables by x2 or Fisher exact test as appropriate. Logistic regression models, adjusted for relevant confounders, were fitted to assess the association between the continuous EFS score and the frail status (as exposures) and the DFRI (dependent variable). Partial and semi-partial correlation coefficients were constructed to assess confounders affecting the aforementioned associations.
Results
Of 463 individuals aged ≥60 years enrolled in the Atahualpa Project (2012 – 2018), 342 were active at the time of this study (January 2019). Of these, 18 declined consent and were excluded. The mean age of 324 participants was 70.5±8 years (median age: 69 years; age range: 60 to 95 years), 186 (57%) were women, 250 (77%) had primary school education only (mean years of education: 6.5±2.9 years), and 50 (15%) reported high intake of alcohol (all men). Blood pressure levels ≥140/90 mmHg were present in 137 (42%) individuals, a body mass index ≥30 kg/m2 in 75 (23%), fasting glucose ≥126 mg/dL in 98 (30%), poor physical activity in 28 (9%), poor sleep quality in 106 (33%), symptoms of depression in 37 (11%), and an overt stroke in 24 (7%).
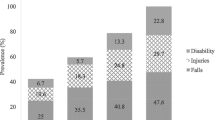
The mean score in the EFS was 4.4±2.5 points, with 180 (56%) participants classified as robust, 76 (23%) as pre-frail and 68 (21%) as frail. The DFRI was positive in 87 (27%) participants. The most common positive component of the DFRI was history of falls (172 cases, 53%), followed by use of medications (142 cases, 44%), sensory or motor deficits (139 cases, 43%), gait abnormalities (55 cases, 17%), and confusion (13 cases, 4%). Table 1 shows characteristics of participants across categories of the EFS and the DFRI. As noted, most of the covariables evaluated — with the exception of a body mass index ≥30 kg/m2, fasting glucose ≥126 mg/dL, and symptoms of depression — were significantly associated with a frail status. In contrast, high alcohol intake was associated with a robust status. This inverse relationship can be an artifact since this covariable was only recorded in men, and men were most often robust than women. Regarding covariables associated with an increased risk of future falls, a positive DFRI was significantly associated with age, blood pressure levels ≥140/90 mmHg, fasting glucose ≥126 mg/dL, poor physical activity, poor sleep quality, symptoms of depression, and an overt stroke.
Also in univariate analysis, the mean EFS score was significantly higher among participants with a positive, than in those with a negative DFRI (5.8±2.9 versus 3.9±2.2; p<0.001). The percentage of frail individuals was higher (40% versus 14%; p<0.001), while that of robust individuals was lower (37% versus 62%; p<0.001) among those with a positive DFRI. However, there were no differences in the percentages of prefrail individuals according to a positive or negative DFRI status (23% versus 24%; p=0.791).
A logistic regression model, adjusted for all the aforementioned covariables, showed no association between the continuous EFS score and the DFRI (Table 2). Then, the most parsimonious model was fitted with variables having p<0.2 significance in the fully-adjusted model. Again, there was no association between the continuous EFS score and the DFRI (Table 3). We then investigated the possibility of having a positive DFRI according to the three categories of frailty (instead of the continuous EFS score) using covariables included in the most parsimonious model, and found no differences in the Odds of having a positive DFRI when prefrail and frail subjects where compared with robust ones (Table 4).
Since age seemed to be a relevant confounder in the association between frailty and risk of falls, we fitted an interaction model with participants stratified according to their median age, but found no significant interaction of age in this association (OR: 0.85; 95% C.I.: 0.25 – 2.87; p=0.793). History of an overt stroke also appeared as a significant confounder in all previous models. Therefore, we fitted a logistic regression model that only included the 300 stroke-free participants. Nevertheless, in this model without stroke as a covariable, the association between the continuous EFS score and the DFRI was also non-significant (OR: 1.06; 95% C.I.: 0.92 – 1.21; p=0.428).
In addition, partial and semi-partial correlation coefficients showed that several confounders together (age, high glucose levels, and history of an overt stroke) took away the association between frailty and the risk of falls found in univariate analyses (Table 5).
Discussion
The relationship between frailty and the risk of falls has not been investigated in remote rural settings, and little is known of the impact of frailty on the risk of falls in these populations. The present study shows a significant association between both variables, but only in univariate analyses. Of note, several of the chosen covariables were significantly associated with both the exposure (frail status) and the outcome (risk of falls). This might explain why the association between frailty and the risk of falls became non-significant when confounders were added to multivariate regression models. This was better demonstrated by the use of partial and semi-partial correlation coefficients, which showed that age, high glucose levels, and history of an overt stroke tempered the significance of the association between frailty and risk of falls.
It is possible that the effect of confounders explains the disparities in the results of some previous studies attempting to assess the relationship between frailty and risk of falls. Another possibility is that instruments used to assess frailty in many of these studies fail to take into account several of the items included in the EFS (22, 23).
There are several factors that increase the risk of falls in older adults, some of which are intrinsic to the individual while others are extrinsic (i.e., related to the environment) (24). In any case, many of the intrinsic factors that increase the risk of falls are components of the frail syndrome (cognitive decline, functional independence, use of medications, depression, and abnormal balance and motility). Therefore, it is not surprising that both conditions are associated. Indeed, results of univariate analyses conducted in the present study strongly suggest that frail individuals are at increased risk of future falls. The problem here are the confounders, that is, the presence of specific circumstances or conditions that make some subjects more prone to developing falls in the follow-up. In the present study, the non-significant association found in multivariate models does not rule out the actual association between frailty and risk of falls. Rather, it means that some frail individuals, particularly those with increasing age, diabetes mellitus, and history of an overt stroke have a greater risk of falls than other frail subjects due to these characteristics. This should be considered in further studies assessing the relationship between frailty and risk of falls in the population at large.
Major strengths of the present study are the unbiased selection of participant subjects and the methods used to assess frailty and the risk of future falls. A potential limitation is its cross-sectional design which does not allow for an assessment of the reliability of the DFRI to predict the actual risk of falls among inhabitants living in rural populations, where environmental factors might be an important cause of falls (in particular, walking throughout uneven non-paved streets). Future longitudinal studies using the Atahualpa Project cohort will be of value to answer this question.
In summary, this study shows that the prevalence of frailty among older adults living in a remote rural community is similar to that reported in industrialized urban centers. In contrast, the risk of falls is somewhat lower according to the DFRI. This discrepancy is probably related to the fact that the DFRI does not take into account distinct environmental conditions that may result in falls. More importantly, frailty is significantly associated with the risk of falls in univariate analyses, but the association disappeared in multivariate models, most likely because increasing age, diabetes mellitus, and history of an overt stroke tempered the statistically significant association between exposure (frailty) and outcome (risk of falls) variables.
References
Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging 2013;17:726–734.
Morley JE, Vellas B, Abellan van Kan G, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392–397.
Bagshaw SM, Stelfox HT, Johnson JA, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43:973–982.
Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults — United States. J Safety Res 2016;58:99–103.
Cheng MH, Chang SF. Frailty as a risk factor for falls among community dwelling people: evidence from a meta-analysis. J Nurs Scholarship 2017;49:529–536.
Kojima G. Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc 2015;16:1027–1033.
Fhon JR, Rodrigues RA, Neira WF, Huayta VM, Robazzi ML. Fall and its association with the frailty syndrome in the elderly: systematic review with meta-analysis. Rev Esc Enferm USP 2016;50:1005–1013.
Gray WK, Orega G, Kisoli A, et al. Identifying frailty and its outcomes in older people in rural Tanzania. Exp Aging Res 2017;43:257–273.
Del Brutto OH, Mera RM, Sedler JM, et al. The effect of age in the association between frailty and poor sleep quality: a population-based study in community-dwellers (The Atahualpa Project). J Am Med Dir Assoc 2016;17:269–271.
Del Brutto OH, Mera RM, Zambrano M, Sedler MJ. Influence of frailty on cognitive decline: a population-based cohort study in rural Ecuador. J Am Med Dir Assoc 2019;20:213–216.
Del Brutto OH, Peñaherrera E, Ochoa E, Santamaría M, Zambrano M, Del Brutto VJ. Door-to-door survey of cardiovascular health, stroke, and ischemic heart disease in rural coastal Ecuador — the Atahualpa Project: Methodology and operational definitions. Int J Stroke 2014;9:367–371.
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing 2006;35:526–529.
Fabricio-Wehbe SC, Cruz IR, Haas VJ, Diniz MA, Dantas RA, Rodrigues RA. Reproducibility of the Brazilian version of the Edmonton Frail Scale for elderly living in the community. Rev Lat Am Emfermagem 2013;21:1330–1336.
Nilsson M, Eriksson J, Larsson B, Odén A, Johansson H, Lorentzon M. Fall risk assessment predicts fall-related injury, hip fracture, and head injury in older adults. J Am Geriatr Soc 2016;64:2242–2250.
Mojtaba M, Alinaghizadeh H, Rydwik E. Downton Fall Risk Index during hospitalization is associated with fall-related injuries after discharge: a longitudinal observational study. J Physiother 2018;64:172–177.
Del Brutto OH, Mera RM, Peinado CD, Sedler MJ. Prevalence, severity, and risk of future falls in Community-dwelling older adults living in a rural Community: The Atahualpa Project. J Community Health 2019, doi: https://doi.org/10.1007/s10900-019-00664-3
Lloyd-Jones D, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion. The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 2010;121:586–613.
Del Brutto OH, Santamaría M, Ochoa E, et al. Population-based study of cardiovascular health in Atahualpa, a rural village of coastal Ecuador. Int J Cardiol 2013;168:1618–1620.
Del Brutto OH, Mera RM, Farfán R, Castillo PR. Cerebrovascular correlates of sleep Disorders — Rational and protocol of a door-to-door survey in rural coastal Ecuador. J Stroke Cerebrovasc Dis 2014;23:1030–1039.
Del Brutto OH, Mera RM, Del Brutto VJ, et al. Influence of depression, anxiety and stress on cognitive performance in community-dwelling older adults living in rural Ecuador: Results of the Atahualpa Project. Geriatr Gerontol Int 2015;15:508–514.
Del Brutto OH, Santamaría M, Zambrano M, et al. Stroke in rural Ecuador: a community-based survey. Int J Stroke 2014;9:365–366.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–M156.
Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 2008;168:382–389.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2913;75:51–61.
Funding
Source of funding: This study was supported by Universidad Espiritu Santo — Ecuador. The sponsor had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standard: None declared by the Authors.
Additional information
Conflicts of interest: No conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Del Brutto, O.H., Mera, R.M., Peinado, C.D. et al. Frailty and Risk of Falls in Community-Dwelling Older Adults Living in a Rural Setting. The Atahualpa Project. J Frailty Aging 9, 150–154 (2020). https://doi.org/10.14283/jfa.2019.36
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2019.36