Abstract
Summary
A frailty concept that includes psychological and cognitive markers was prospectively shown to be associated with increased risk of multiple falls and fractures among 1,509 community dwelling older adults, especially in those aged 75 and over. The predictive ability of frailty is not superior to falls history.
Introduction
The concept of frailty has been defined with or without psychological and cognitive markers. Falls are associated with multiple risk factors, including cognitive and mood disorders. The purpose of this study was to investigate the association of a comprehensive concept of frailty and its components with falls and fractures in community-dwelling older adults and to compare its predictive ability with having a history of falls.
Methods
One thousand five hundred nine participants in the Longitudinal Aging Study Amsterdam aged ≥65 were assessed to determine fall history and the prevalence of nine frailty markers, including cognitive and psychological factors. The number of falls and time to second fall were prospectively registered for 1 year. Fractures were registered for 6 years.
Results
Frailty was significantly associated with time to second fall: hazard ratio of 1.53 [95 % confidence interval (CI), 1.07–2.18] and area under the receiver operating characteristic curve (AUC) of 0.58 (CI, 0.53–0.62). In participants aged ≥75, frailty was associated with ≥2 falls: odds ratio (OR) of 1.74 (CI, 1.19–2.55) and AUC of 0.62 (CI, 0.55–0.68). Frailty, adjusted for age and sex, was significantly associated with ≥2 fractures: OR of 3.67 (CI, 1.47–9.15). The AUCs for falls history (aged ≥75) ranged from 0.62 (CI, 0.58–0.67) for ≥1 falls to 0.67 (CI, 0.59–0.74) for ≥3 falls.
Conclusions
A concept of frailty including psychological and cognitive markers is associated with both multiple falls and fractures. However, frailty is not superior to falls history for the selection of old persons at increased risk of recurrent falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of frailty in older adults expresses an expectation of increased risk of adverse health outcomes, such as disability, complications, and institutionalisation. Although frailty is a useful concept for both clinical and research purposes in older adults, the definition and methods of assessment are heterogeneous. In 2001, Fried et al. [1] described a phenotype of frailty that has been widely followed in geriatric and gerontological research. They defined frailty as a clinical syndrome that is present in persons who fulfill three or more of the following criteria: unintentional weight loss, self-reported exhaustion, weakness, slow walking speed, and low physical activity. A subsequent debate in the literature has revolved around the question whether or not frailty definitions should include cognitive and mental factors [2].
In the Longitudinal Aging Study Amsterdam (LASA), an ongoing longitudinal study of biological and social aspects of aging, frailty was assessed using similar markers complemented with indicators of psychological and cognitive function. Puts et al. used the following nine markers to define frailty: low body weight, low peak expiratory flow, impaired cognitive function, impaired visual acuity or hearing impairment, incontinence, low mastery, depressive symptoms, and low physical activity. Frailty, thus defined by the LASA frailty instrument, was associated with decline of physical performance and self-reported functional ability after a follow-up of 3 years [3]. Most of these determinants (i.e., low body weight, impaired visual acuity, incontinence, impaired cognitive function, depressive symptoms, and low physical activity) coincide with risk factors for falls and fractures [4–9]. Fall and fracture risk has been demonstrated to be associated with frailty assessed by instruments that do not include aspects of psychological or cognitive functions [10, 11]. To our knowledge, it is not known whether a frailty concept that includes aspects of physical as well as psychological and cognitive functions is also associated with increased fall and fracture risks.
We thus hypothesised that frailty assessed by the LASA frailty instrument is associated with increased fall and fracture risk. In addition, we examined which individual frailty markers were associated with falls and fractures, and we compared the association frailty with that of falls history, an established risk factor for falls and fractures [4–9].
If the association of frailty with falls and fractures is shown to be present, the identification of frailty in an older person might open opportunities for timely initiation of primary fall prevention for those who might benefit most [12]. Furthermore, determination of the frailty markers that contribute to a possible association would help to develop more efficient fall and fracture risk assessment instruments.
Methods
Study design and population
Data for this study were collected in the context of the LASA, an ongoing interdisciplinary cohort study on predictors and consequences of changes in autonomy and well-being in the aging population in The Netherlands [13]. The sampling and data collection procedures have been described in detail elsewhere [14]. In brief, a sample of older men and women (aged 55–85 years), stratified by age and sex, was drawn from the population registries of 11 municipalities in three areas of The Netherlands. In total, 3107 subjects (response rate = 62, 3 %) were enrolled in the baseline examination (1992/1993).
The present study was performed using data from a subsample of the LASA cohort, including 1,509 respondents out of 1,720 eligible, who participated in the second data collection cycle of LASA (1995/1996). A total of 211 people were not interviewed (5 died, 160 refused, 43 were ineligible, and 3 were not contacted). The participants were born in or before 1930 (aged 65 years and older as of January 1, 1996) and were living in the community. A face-to-face interview was performed at home. The interviews were conducted by intensively trained and supervised lay interviewers. All interviews were tape-recorded to monitor the quality of the data [14].
Informed consent was obtained from all respondents, and the study was approved by the Medical Ethics Committee of the VU University Medical Center and conducted according to the principles of the Helsinki declaration.
Assessment of the LASA frailty instrument
The nine frailty markers were as follows: body mass index (BMI) [body weight in kilograms (calibrated bathroom scale) divided by the square of height in meters], peak expiratory flow (Mini-Wright peak flow meter [15]), cognitive functioning (Mini-mental State Examination, MMSE [16]), visual and auditory acuity (“are you able to recognise someone’s face at a distance of 4 meters” and “are you able to follow a conversation with one and four persons”, with glasses or hearing aid if needed), incontinence (unintentional urine loss), sense of mastery (short version Pearlin and Schooler Mastery scale [17]), depressive symptoms (Center for Epidemiological Studies Depression scale, CES-D [18]), and physical activity (LASA Physical Activity Questionnaire [19]) [3].
Participants were assigned one point for each marker for which their score was in the lowest quintile of functioning (peak expiratory flow, mastery, and physical activity) or below or above a literature consensus-based cut-off value (BMI < 23, MMSE < 24, and CES-D ≥ 16). Participants were also assigned one point for answering the questions about visual and auditory acuity with “No, I can’t” and the question concerning incontinence with “yes.” Missing values on frailty markers were not imputed but counted as “not present” in the calculation of the total number of frailty markers present.
The frailty markers were recorded at the start of the fall follow-up. Similar to Fried et al. [1], we considered all participants who scored ≥3 points frail.
Assessment of falls and fractures
Participants were asked to record falls every week on a “fall calendar” and to mail the calendar page to the research institute at 3-month intervals. The participants were contacted by telephone if they were unable to complete the calendar, if the calendar was not returned even after a reminder, or if it was completed incorrectly. Proxies were contacted if participants were not able to respond [9, 20].
A fall was defined as “an unintentional change in position resulting in coming to rest at a lower level or on the ground” [21]. During 1 year of follow-up, the number of falls and the time to the second fall were registered. Prior to the start of the prospective fall registration participants previous falls were assessed with the following question: “did you suffer one or more falls in the previous year?”
During 6 years of follow-up, fractures were registered three monthly and verified using primary care and hospital medical records.
Assessment of covariates
During the home visit, the presence of seven major categories of chronic somatic diseases (lung diseases, cardiac diseases, vascular diseases, joint diseases, cancers, diabetes mellitus, and stroke) and psychiatric diseases, both in the past and present were assessed. Self-report of chronic conditions has been shown to have a moderate to high level of reliability [22, 23]. Functional limitations were assessed with three questions regarding independence with performing three activities: clipping one’s own toe nails, climbing the stairs, and using one’s own or public transport. A composite score was calculated ranging from 0 (no difficulties with the activities) to 3 (difficulties with all of the activities). The highest level of education achieved was recorded. The scores for education ranged from elementary school (low), lower/intermediate general secondary and vocational education (middle), to college and university (high).
Statistical analysis
All analyses were performed using SPSS version 17.0. The level of significance was set at 0.05 unless stated otherwise. The associations of frailty with time to second fall in 1 year and with time to first fracture in 6 years after inclusion were examined using Cox proportional hazards models. Log-binomial regression was performed to analyze the association between frailty and the risk of: ≥1 falls, ≥2, or more ≥3 or more falls in 1 year and of ≥1 and ≥2 fractures in 6 years of follow-up. All analyses were adjusted for age and sex in the first step, and additionally for relevant confounders including number of chronic diseases, functional limitations, and education in the second step. Interaction with age and sex were examined by adding product terms with frailty (e.g., age × frailty) to the models and if significant (p < 0.10) further analyses would be stratified.
If significant associations between frailty and falls or fractures were demonstrated, the same analyses were repeated for the nine frailty markers separately. In these analyses, multiple testing effects were accounted for using a stricter alpha of p ≤ 0.01. Using the six “somatic” frailty components, a somatic frailty index was established using a cut-off of 2 positive markers. For comparison, the association of falls history with falls and fractures was examined. Ultimately, areas under the receiver operating characteristic curves (AUC) were calculated for all relevant frailty indexes, for (combinations of) frailty components, and for outcome of the retrospective falls question.
Results
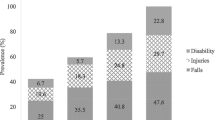
The participants had a median age of 75.6 years (range, 64.8–88.8) and 51.8 % were female. Almost a third of the participants (486, 32.2 %) reported at least one fall in the previous year. One or more falls in the first year of follow-up occurred in 468 (31.0 %) and two or more falls in 174 (11.5 %) participants. At least one fracture within 6 years occurred in 132 (8.7 %) participants. Of these participants, 21 (1.4 %) suffered 2 fractures or more. None of the participants reported sustaining more than one fracture at a single event. A fifth of the participants (n = 312) had three or more frailty markers. A quarter of the participants had two or more of the six somatic frailty markers. Other baseline characteristics are described in Table 1. Prevalence of frailty components and numbers of falls and fractures are described in Tables 2 and 3, respectively.
Falls
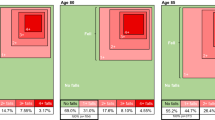
Testing for interactions revealed that frailty interacted with age for the outcomes ≥2 and ≥3 falls (p = 0.03 and p = 0.04, respectively). No interactions with sex were found. Further analyses of the number of falls were therefore stratified for age below or ≥75 years.
After adjustment for age and sex, frailty was significantly associated with fall risk measured by the time to the second fall, hazard ratio (HR) of 2.02 [95 % confidence interval (CI), 1.44–2.83]. Additional adjustment for chronic disease, functional limitations, and education attenuated the association, but it remained significant, HR of 1.53 (CI, 1.07–2.18).
In both age groups, no significant associations were found between frailty and one or more falls (Table 4). In participants younger than 75 years, frailty was not associated with any number of falls. However, in participants aged 75 and over, frailty was significantly associated with having ≥2 falls: odds ratio (OR) of 2.36 (CI, 1.63–3.40). This association remained significant after additional adjustment for chronic diseases, functional limitations, and education OR of 1.74 (CI, 1.19–2.55). Similar associations were found with three or more falls in this age group. The ability of frailty to discriminate between recurrent fallers and nonrecurrent fallers was modest [AUC 0.58 (CI, 0.53–0.62, p = 0.001) in all participants and AUC 0.62 (0.55–0.68) in the participants of 75 years and older].
Fractures
After adjustment for age and sex, frailty was not significantly associated with time to first fracture in 6 years of follow-up (HR, 1.47; CI, 0.98–2.21). Log-binomial analysis of ≥1 fractures resulted in an OR of 1.22 (CI, 0.84–1.79; p = 0.30). However, significant associations were found between frailty and sustaining ≥2 fractures (OR, 3.67; CI, 1.47–9.15). Additional adjustments rendered this association nonsignificant (OR, 1.93; CI, 0.77–4.83). The ability of frailty to identify participants with multiple fractures was statistically significantly better than chance, AUC of 0.66 (CI, 0.53–0.79; p = 0.011; Table 5). Of the participants who sustained more than one fracture, 42.9 % had at least one hip fracture (two of them suffered two hip fractures) and 85.7 % sustained at least one osteoporotic fracture (hip, wrist, upper arm, or vertebral). Of the participants who sustained a maximum of one fracture 25.2 % suffered a hip fracture (p = 0.33) and 69.2 % (p = 0.05) sustained an osteoporotic fracture.
Frailty markers
After adjustment for age and sex, the frailty components incontinence, depression, and (low) mastery were significantly associated with shorter time to second fall (p < 0.001; Table 2). In participants 75 and over, incontinence, depression, and mastery were associated with sustaining ≥2 falls (p < 0.01). For the outcome recurrent falls, the only frailty component with an AUC statistically significant higher than chance was incontinence [in all participants, 0.59 (CI, 0.54–0.65), and in the oldest group, 0.62 (CI, 0.55–0.70)]. Incontinence was also the only frailty marker associated with any fall and ≥3 falls in both age groups (p < 0.01). Defining frailty as having ≥2 out of the three frailty markers that had a significant association with recurrent falls did not lead to a higher AUC. Somatic frailty (i.e., the presence of ≥2 out of six somatic frailty components) did not show significantly higher AUCs than the original frailty index: AUC of 0.60 (CI, 0.53–0.67; p = 0.003) for ≥2 falls in participants aged ≥75. None of the other combinations of the frailty components resulted in significantly higher AUCs than the total frailty index.
None of the frailty components were significantly (p ≤ 0.01) associated with any of the fracture outcomes.
Falls history
Having a history of falls was significantly associated with time to second fall (HR, 2.92; CI, 2.15–3.97) and in the participants aged ≥75 with any number of falls up to three or more: the OR increased from 1.81 (CI, 1.48–2.21) for 1 or more falls to 3.09 (CI, 1.85–5.16) for ≥3 falls, adjusted for all relevant confounders. Accordingly, the AUCs for falls history in participants aged ≥75 ranged from 0.62 (CI, 0.58–0.67) for one or more falls to 0.67 (CI, 0.59–0.74) for ≥3 falls in 1 year. Having sustained a fall in the previous year was also significantly associated with sustaining one or more fractures in 6 years of follow-up: OR, 1.95 (CI, 1.41–2.70) with adjustment for all confounders. The discriminative ability of prior falls for future fractures was modest: AUC of 0.60 (CI, 0.55–0.65).
Discussion
This study confirmed the hypothesis that a concept of frailty, including somatic, psychological, and cognitive markers is associated with increased fall risk and possibly associated with fracture risk in older adults. Frailty was associated with two or more and with three or more falls but only in participants aged 75 years and over. Frailty was also borderline associated with two or more fractures. The frailty markers mastery, incontinence, and depression were individually associated with multiple falls but not with fractures. However, the ability of frailty and each of the frailty markers to distinguish fallers from nonfallers was only modest and not superior to the prognostic value of prior falls.
Many associations with adverse outcomes, including fractures, have been described previously using the original frailty criteria of Fried et al. [24, 25] In our study, the concept of frailty was assessed including cognitive and psychological markers in addition to somatic characteristics to identify older adults at the greatest risk of loss of physical functioning resulting in falls and fractures. The validity of this method of determining frailty was demonstrated by Puts et al. [3]. Avila-Funes et al. [26] showed that adding cognitive impairment to the classical frailty criteria improved the predictive value for adverse outcomes. Comparison of our results with those of studies that used the original frailty criteria was hampered by differences in sample characteristics. However, some general trends can be observed. Ensrud et al. found similar associations with falls and fractures but excluded older adults who could not walk unassisted, resulting in a lower percentage of recurrent fallers than in our study. Using Fried’s frailty criteria and the same outcome measure (recurrent falls in 1 year), she also reported similar AUCs: for recurrent falls, 0.61–0.63 [10, 25].
The frailty markers depression, cognitive impairment, and incontinence were not included in Fried’s frailty criteria. In our study, particularly incontinence contributed strongly to the associations with falls as was demonstrated by the separate associations with the risk of recurrent falls. The relevance of the associations of those frailty markers has previously been demonstrated in other studies with fall risk as primary outcome measure [27–29]. Furthermore, Muir et al. [28] showed that cognitive impairment was also associated with increased risk of distal radius fractures. This finding could not be reproduced in our study.
The finding that frailty as measured with the LASA frailty instrument is not associated with less than two falls supports the notion that the majority of the older adults who fell only once suffered an unfortunate incident, which they were able to avoid thereafter. The association of frailty with risk of multiple fractures was significant, despite the low number of participants with multiple fractures. We used negative binomial regression to analyze this association. With this technique, loss to follow-up and death cannot be accounted for. If an association can nevertheless be demonstrated, it is probably a relevant association because minor associations are not likely to be significant as a result of the inability to account for loss to follow-up. The association of frailty with risk of multiple fractures may nevertheless be due to chance, but the theoretical plausibility that multiple fractures are most likely to occur in frail older adults is high. Furthermore, the association of frailty with time to first fracture is borderline significant. Lack of significance may be due to a too small number of fractures during follow-up. However, the direction and size of the effect are comparable with that of the significant association between frailty and risk of sustaining two or more fractures.
The strength of our study lies in the use of a comprehensive and validated frailty instrument that included psychological and cognitive markers in addition to somatic markers. The added value of mastery and depression is demonstrated by their individual significant associations with falls.
Furthermore, we measured falls prospectively using a fall calendar in a representative sample of the older population. In contrast, in the study of Ensrud et al. [10, 25], a four monthly postcard or telephone survey was performed to measure falls prospectively. This may have resulted in some loss of information.
A limitation of our study is the fact that frailty was assessed once at baseline before the start of the follow-up of falls and fractures. It is therefore possible that the frailty characteristics changed over time resulting in transitions in frailty status. However, transition of a frail to a nonfrail state is a very rare event and therefore unlikely to relevantly influence our results. It is safe to conclude that demonstrating the presence of frailty once is an indicator of increased falls and fracture risk regardless of the subsequent development of frailty in the years that follow.
Unfortunately, we were not able to reconstruct “physical” frailty according to Fried because all but two of the somatic components in the LASA frailty concept differed from Fried’s. Therefore, we could not directly compare Fried’s physical frailty concept and the LASA concept that includes psychological and cognitive components. To examine whether differences in findings were explained by the psychological and cognitive components in the LASA concept, analyses were repeated for the somatic components only. This resulted in similar AUCs for recurrent falls showing that the predictive ability of the LASA frailty concept did not only result from the psychological and cognitive markers.
The fact that the LASA frailty instrument was not developed to distinguish between three levels of frailty like Fried’s criteria (frail, prefrail and nonfrail) could be considered a disadvantage. However, we studied the value of the LASA frailty criteria to predict falls and fractures and did not aim to develop a new fall risk or fracture risk instrument. Frailty in itself is a relevant concept only when it predicts functional outcomes. The LASA frailty criteria have been developed to do this. Puts et al. [3] showed that values above the cut-off that we have used are associated with several measures of functional decline. Although the cut-off was determined at three out of nine frailty markers, we found a prevalence rate of frailty defined by the LASA criteria in our population of 20.7 %. This is higher than the prevalence rate of frailty (6.9 % for three out of five frailty markers) and lower than the prevalence of a prefrail state (46.6 % for two out of five) as found by Fried et al. [1] in a comparable population.
Although the LASA frailty instrument is associated with falls and fractures its discriminative ability is not superior to a simple assessment of falls in the previous year. Taking into account the burden of the measurements for participants and health care personnel the use of the frailty instrument as a tool to predict fall or fracture risk is not recommended. As directing fall prevention interventions at individuals with the highest risk of falls has been demonstrated to be mostly ineffective, new strategies to select those who will benefit most from prevention are desperately needed [30]. Our findings confirm the results of previous studies reporting that a very short clinical impression of an older person can be at least as effective for predicting falls and fractures as most frailty instruments are [31, 32]. Because the currently available frailty instruments have predominantly been developed with prognostic purposes, future research needs to address the question whether these instruments are more fit to select those who will benefit from interventions to prevent adverse outcomes like falls and fractures [33].
Abbreviations
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
95 % confidence interval
References
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Morley JE, Perry HM III, Miller DK (2002) Editorial: something about frailty. J Gerontol A Biol Sci Med Sci 57:M698–M704
Puts MT, Lips P, Deeg DJ (2005) Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol 58:1188–1198
Nevitt MC, Cummings SR, Kidd S, Black D (1989) Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 261:2663–2668
Nevitt MC, Cummings SR, Hudes ES (1991) Risk factors for injurious falls: a prospective study. J Gerontol 46:M164–M170
Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF (2002) A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol 55:1088–1094
Tromp AM, Smit JH, Deeg DJ, Bouter LM, Lips P (1998) Predictors for falls and fractures in the longitudinal aging study Amsterdam. J Bone Miner Res 13:1932–1939
Tromp AM, Ooms ME, Popp-Snijders C, Roos JC, Lips P (2000) Predictors of fractures in elderly women. Osteoporos Int 11:134–140
Pluijm SM, Smit JH, Tromp EA, Stel VS, Deeg DJ, Bouter LM, Lips P (2006) A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: results of a 3-year prospective study. Osteoporos Int 17:417–425
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, Hillier TA, Cauley JA, Hochberg MC, Rodondi N, Tracy JK, Cummings SR (2008) Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 168:382–389
Romero-Ortuno R, Cogan L, Foran T, Kenny RA, Fan CW (2011) Continuous non-invasive orthostatic blood pressure measurements and their relationship with orthostatic intolerance, falls, and frailty in older people. J Am Geriatr Soc 59:655–665
Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T (1996) Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT group. Frailty and injuries: cooperative studies of intervention techniques. J Am Geriatr Soc 44:489–497
Huisman M, Poppelaars J, van der Horst M, Beekman A, Brug J, van Tilburg T, Deeg D (2011) Cohort profile: the longitudinal aging study Amsterdam. Int J Epidemiol 40:868–876
Deeg DJ, van Tilburg T, Smit JH, de Leeuw ED (2002) Attrition in the longitudinal aging study Amsterdam. The effect of differential inclusion in side studies. J Clin Epidemiol 55:319–328
Cook NR, Albert MS, Berkman LF, Blazer D, Taylor JO, Hennekens CH (1995) Interrelationships of peak expiratory flow rate with physical and cognitive function in the elderly: MacArthur Foundation studies of aging. J Gerontol A Biol Sci Med Sci 50:M317–M323
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Pearlin LI, Schooler C (1978) The structure of coping. J Health Soc Behav 19:2–21
Radloff LS, Teri L (1986) Use of the center for epidemiological studies-depression scale with older adults. Clinical Gerontology 5:119–136
Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P (2004) Comparison of the LASA physical activity questionnaire with a 7-day diary and pedometer. J Clin Epidemiol 57:252–258
Stel VS, Pluijm SM, Deeg DJ, Smit JH, Bouter LM, Lips P (2003) A classification tree for predicting recurrent falling in community-dwelling older persons. J Am Geriatr Soc 51:1356–1364
Kellogg International Work Group on the Prevention of Falls by the Elderly (1987) The prevention of falls in later life. Dan Med Bull 34(4):1–24
Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ (1996) Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients' self-reports and on determinants of inaccuracy. J Clin Epidemiol 49:1407–1417
Oksanen T, Kivimaki M, Pentti J, Virtanen M, Klaukka T, Vahtera J (2010) Self-report as an indicator of incident disease. Ann Epidemiol 20:547–554
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, Tracy JK, Hochberg MC, Rodondi N, Cawthon PM (2007) Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 62:744–751
Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, Dam TT, Marshall LM, Orwoll ES, Cummings SR (2009) A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc 57:492–498
Avila-Funes JA, Amieva H, Barberger-Gateau P, Le GM, Raoux N, Ritchie K, Carriere I, Tavernier B, Tzourio C, Gutierrez-Robledo LM, Dartigues JF (2009) Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: the three-city study. J Am Geriatr Soc 57:453–461
Eggermont LH, Penninx BW, Jones RN, Leveille SG (2012) Depressive symptoms, chronic pain, and falls in older community-dwelling adults: the Mobilize Boston Study. J Am Geriatr Soc 60:230–237
Muir SW, Gopaul K, Montero Odasso MM (2012) The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 41(3):299–308
Yamashita T, Jeon H, Bailer AJ, Nelson IM, Mehdizadeh S (2011) Fall risk factors in community-dwelling elderly who receive Medicaid-supported home- and community-based care services. J Aging Health 23:682–703
de Vries OJ, Peeters GM, Elders PJ, Muller M, Knol DL, Danner SA, Bouter LM, Lips P (2010) Multifactorial intervention to reduce falls in older people at high risk of recurrent falls: a randomized controlled trial. Arch Intern Med 170:1110–1117
Gerdhem P, Ringsberg KA, Magnusson H, Obrant KJ, Akesson K (2003) Bone mass cannot be predicted by estimations of frailty in elderly ambulatory women. Gerontology 49:168–172
Gerdhem P, Ringsberg K, Akesson K, Obrant KJ (2004) Just one look, and fractures and death can be predicted in elderly ambulatory women. Gerontology 50:309–314
de Vries NM, Staal JB, van Ravensberg CD, Hobbelen JS, Olde Rikkert MG, Nijhuis-van der Sanden MW (2011) Outcome instruments to measure frailty: a systematic review. Ageing Res Rev 10:104–114
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Vries, O.J., Peeters, G.M.E.E., Lips, P. et al. Does frailty predict increased risk of falls and fractures? A prospective population-based study. Osteoporos Int 24, 2397–2403 (2013). https://doi.org/10.1007/s00198-013-2303-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2303-z