Abstract
Background
Participation in coronary heart disease secondary prevention programs is low. Innovative programs to meet this treatment gap are required.
Purpose
To aim of this study is to describe the effectiveness of a telephone-delivered secondary prevention program for myocardial infarction patients.
Methods
Four hundred and thirty adult myocardial infarction patients in Brisbane, Australia were randomised to a 6-month secondary prevention program or usual care. Primary outcomes were health-related quality of life (Short Form-36) and physical activity (Active Australia Survey).
Results
Significant intervention effects were observed for health-related quality of life on the mental component summary score (p = 0.02), and the social functioning (p = 0.04) and role-emotional (p = 0.03) subscales, compared with usual care. Intervention participants were also more likely to meet recommended levels of physical activity (p = 0.02), body mass index (p = 0.05), vegetable intake (p = 0.04) and alcohol consumption (p = 0.05).
Conclusions
Telephone-delivered secondary prevention programs can significantly improve health outcomes and could meet the treatment gap for myocardial infarction patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease (CHD) is a leading cause of death and economic burden in the USA and the rest of the developed world [1]. While advances in treatment have improved survival after an initial cardiovascular event, persons with established CHD are at high risk of subsequent events, poor health-related quality of life (HRQoL), and high health service needs and costs [1, 2].
Clinical trials have shown that persons with CHD can reduce their risk of subsequent events through participation in effective secondary prevention or cardiac rehabilitation programs [1]. Traditional secondary prevention programs are facility-based, structured, time-limited, group-based and include exercise and CHD risk factor education sessions [3]. These programs have led to enhanced HRQoL, improved CHD risk factor profiles and decreased total cardiac mortality (26 %) [1]. As such, secondary prevention programs are recommended (with the highest level of scientific evidence—class I) for the treatment of patients with CHD by the American Heart Association and the American College of Cardiology, the European Society of Cardiology and the Australian Cardiovascular Health and Rehabilitation Association [1, 2, 4, 5]. However, participation rates remain sub-optimal with only 10–30 % of eligible participants taking part in traditional models of secondary prevention [5]. Importantly, those at greatest risk of recurrent disease are least likely to attend [5] and of those that do attend, many do not adhere to the program [6]. Both patient- and provider-level barriers to participation have been identified [7, 8]. Reported patient-level barriers include lack of transport and geographical isolation, early return to work and decreased motivation to attend due to factors such as depression [7, 8]. Provider-level barriers include the degree of automation and assertiveness around securing referrals to secondary prevention programs, poor integration of secondary prevention programs within the hospital setting; as well as clinician, community and capacity constraints [9]. Further, patients who have undergone coronary artery bypass surgery or percutaneous coronary intervention are more likely to attend than myocardial infarction (MI) patients who have not been revascularised [10]. As such, there is a need to develop and evaluate novel and flexible secondary prevention programs to overcome barriers to participation and meet the treatment gap to achieve optimal benefits for MI patients [5].
More recently, telehealth (telephone, Internet and videoconference communication) has emerged as a flexible home-based model of secondary prevention [5, 11–14]. Telephone-delivered interventions have been shown to be convenient and flexible as they can be delivered at a suitable time for the participant in their own home, and they are acceptable to participants [15]. Telephone-delivered programs may improve health outcomes by providing secondary prevention to the majority of patients who are currently not accessing traditional cardiac rehabilitation or secondary prevention programs, and they may also motivate patients to attend traditional programs.
A review of telephone-delivered interventions for CHD patients revealed that at 6–48 months follow-up, compared with usual care (UC) participants, intervention participants reported a trend towards lower body mass index or BMI, a 17 % lower smoking rate and significantly more physical activity [12]. Only two trials used the Short Form-36 (SF-36) to assess HRQoL and both found a significant benefit in the physical component summary score but not in the mental health summary score [12]. In contrast, Worcester and Le Grande reported positive effects on psychological functioning outcomes following participation in secondary prevention [16]. However, it is difficult to quantify the effectiveness of telephone-delivered secondary prevention programs from previous studies due to the disparate methodologies employed [12]. Previous programs have varied in content, duration and intensity. They have included a range of CHD patient subgroups and a wide range of outcome variables have been reported [5, 12]. As such, previous investigators and a recent Cochrane Review conclude that rigorous research is needed in this important and emerging field using validated outcome measures to further investigate the effectiveness of telephone-delivered secondary prevention programs for specific subgroups of CHD patients representative of usual clinical practice [5, 12, 17].
Recent position statements recommend that secondary prevention programs should be designed to maximise participant referral, enrolment and retention. They should be informed by national guidelines, and they should be theory-based and evidence-based [1, 2, 5]. Finally, the program content should include CHD risk factor education, exercise and psychosocial support, and it should be designed to assist participants in achieving individual CHD risk factor goals [1, 2, 5].
The current study involves a unique approach to the delivery of secondary prevention specifically for MI patients and extends the literature on the effectiveness of telephone-delivered secondary prevention interventions for CHD patients. We report a randomised controlled trial of a telephone-delivered secondary prevention program developed specifically for MI patients of two metropolitan hospitals in Australia. The study aimed to achieve significantly greater improvements in HRQoL and health behaviours (physical activity, diet, alcohol intake, BMI and smoking status) for intervention versus UC participants.
Methods
Study Design
We conducted a parallel group, prospective, randomised controlled trial among MI patients in Brisbane, Australia between December 2007 and March 2010. The study protocol and intervention have been described in detail previously [18]. In brief, patients were assigned to receive either a health coaching (HC) intervention or UC. Patients were recruited during their hospital admission and included regardless of whether or not they planned to attend traditional cardiac rehabilitation or secondary prevention programs. This was done for three reasons. First, it was felt inappropriate to deny access to traditional cardiac rehabilitation to UC participants. Second, actual (as opposed to planned) participation in traditional programs can only be determined at least 6 weeks post-discharge. Finally, telephone-delivered interventions may influence attendance and participation in traditional programs. Data were collected at baseline and post-intervention or at 6 months, which was the primary end-point.
Sample Recruitment Procedures
Adult MI patients were recruited from two large metropolitan hospitals from December 2007 to January 2009. Eligibility criteria included a diagnosis of MI [typical rise in serum level of troponin with at least one of the following—ischaemic symptoms, development of pathological Q waves on the electrocardiogram, electrocardiographic changes indicative of ischaemia (ST-segment elevation or depression) or coronary artery intervention [19]], aged 18–80 years, ability to understand English, availability via the telephone during the duration of the trial and no other medical condition that would interfere with optimal participation or produce a significant risk to the patient as defined by the referring specialist.
The intervention commenced within the first 2 weeks of hospital discharge. A letter was mailed to the patient’s primary care provider/s informing them of the aims of the study, the patient’s agreement to participate, and the information that may be required from the patient and the care provider at follow-up. To facilitate comparison of participants and non-participants, de-identified demographic and simple health status data were collected on eligible MI patients identified by the hospital during the study period, and reasons for refusal were collected by the recruitment staff.
Intervention Group
The current study included a novel approach to the delivery of secondary prevention for MI patients through the recruitment and delivery mode, as well as the intervention content. First, participant referral and recruitment to the trial was enhanced by embedding the process within the hospital system. The study had the support of all cardiologists and hospital staff, and participants were recruited pre-discharge by nursing staff. Second, the intervention was delivered by project-trained and highly skilled health professionals (‘health coaches’) over the telephone. The intervention was delivered at a time that was suitable to the participant and was flexible around their schedule. The health coaches were based at a computer-assisted telephone interviewing facility which also provided flexibility around the translation of the intervention in to clinical practice either utilising telehealth lines/helplines available to CHD patients (such as the National Heart Foundation of Australia’s Health Information Service) [20] or through acute clinical settings.
Third, the intervention was grounded in social cognitive theory which has been successfully used across a wide range of health behaviour interventions [21]. The intervention focused on the core determinants of health behaviour including knowledge of the risks and benefits of the behaviour, self-efficacy or confidence that one can engage in the behaviour under various circumstances, outcome expectations and individualised strategies for achieving positive health behaviour change [22]. Finally, the intervention focused on all CHD risk factors including psychosocial support (depression and social isolation) which is often lacking in currently available cardiac rehabilitation programs. There is now strong and consistent evidence for an independent causal association between depression, social isolation and lack of quality social support, and the causes and prognoses of CHD [23]. The intervention was tailored to suit individual participants who were supported to achieve their CHD risk factor goals.
Intervention Delivery
Over a 6-month period, HC participants received up to 10 × 30 min scripted telephone health coaching sessions. This included an introductory session to explain the program and what was expected of the participant, followed by three weekly sessions, three fortnightly sessions and four monthly sessions over 6 months to assist with CHD risk factor management. This structure allowed for more support at the commencement of the program and encouragement of self-management of CHD risk factors towards the end of the program. During the intervention period, participants were guided through a series of steps beginning with an assessment of their CHD risk factor profile at the commencement of the program followed by feedback on their profile consistent with National Heart Foundation of Australia’s guidelines. In collaboration with their health coach, participants were then encouraged to set Specific, Measurable, Achievable, Realistic and Timely (SMART) goals for a CHD risk factor they were most motivated to change which was incorporated into a behaviourally specific action plan. Barriers and enablers were identified, confidence was assessed and problem-solving was discussed if necessary. Subsequent sessions were structured as follows: (1) introduction and identification of any cardiac symptom changes, (2) assessment and health coaching on relevant CHD risk factors, (3) follow-up on progress towards previous actions and goals, and (4) session review, including a summary of actions required and scheduling of the next session. Consistent with the self-management approach underpinning the intervention, participants were encouraged to follow up relevant issues with their usual health care providers.
The health coaching sessions were based on the current guidelines for CHD [24] with a focus on (1) appropriate reduction/management of clinical risk factors (hypercholesterolaemia, hypertension and diabetes), (2) appropriate modification of behavioural risk factors (smoking, nutrition, alcohol, physical activity, weight management), (3) compliance with pharmacological management and (4) management of emotional well-being. Risk factor advice was consistent with the National Heart Foundation of Australia’s guidelines with the goal of achieving the following: total cholesterol <4.0 mmol/L, triglyceride <1.5 mmol/L, HDL cholesterol >1/0 mmol/L, LDL cholesterol <2.0 mmol/L; 130 mmHg systolic and 80 mmHg diastolic blood pressure; fasting plasma glucose <7.0 mmol/L; complete smoking cessation; five servings of vegetables and two servings of fruit per day, <30 % and 10 % of calories from total fat and saturated fat, respectively, <2,300 mg sodium per day and <300 mg dietary cholesterol per day; <2 and <1 standard alcoholic drinks per day for men and women, respectively; 150 min/week over ≥5 sessions of moderate-level physical activity (sufficiently active); BMI 18.5–24.9 kg/m2; and all patients should be assessed for comorbid depression and their level of social support [25].
Recommendations for enhancing emotional well-being included monitoring feeling down/depressed and seeking help when needed, and monitoring support from others and seeking help if needed. The health coach encouraged and recommended the involvement of significant others (i.e. the activation of social and family support), and information sheets were available for partners. They also recommended the activation of community and environmental supports to enhance maintenance of behaviour change (e.g. encouraging participants to utilise local gyms or swimming pools). Participants were encouraged to contact their usual health care providers immediately if there were any medical concerns during the course of the intervention (e.g. changes in cardiac symptoms), and strict protocols were adhered to for participants requiring additional psychosocial support or exhibiting suicidality. Those who were severely distressed were triaged to a helpline based at the Cancer Council Queensland for qualified suicide assessment from a trained counsellor or recommended to contact a national helpline available 24 h a day (Lifeline).
Prior to the commencement of the intervention, participants were posted a ProActive Heart handbook outlining the program goals for CHD risk factors [24], as well as the benefits of improving CHD risk factors, and an existing written educational resource produced by the National Heart Foundation of Australia (‘My Heart My Life’) [26] containing information about CHD and the associated risk factors. During the study period, ‘My Heart My Life’ was provided to all acute coronary syndrome patients hospitalised in Queensland, Australia.
UC Group
UC participants also received the educational resource ‘My Heart My Life’ [26]. In addition, they were sent a quarterly informative newsletter to enhance participant retention which was based on ‘off-the-shelf’ written educational materials.
Measurement
Baseline data were collected from hospital medical records (age, gender, ethnicity, marital status, education, employment, family history of CHD, diabetes, hypertension, lipid profile, blood pressure, height and weight) or by self-report (physical activity, HRQoL, nutrition, alcohol intake and smoking status) through trained computer-assisted telephone interviewers who were blind to study condition. Follow-up data were collected by computer-assisted telephone interview. Participants were also sent a self-reported satisfaction survey at the completion of the study to investigate satisfaction with the ProActive Heart program overall (‘very satisfied’, ‘mostly satisfied’, ‘mildly satisfied’, ‘not satisfied’), satisfaction with the participant handbook (‘excellent’, ‘good’, ‘average’, ‘poor’) and satisfaction with the health coaching sessions (‘useful’, ‘not-useful’). Participants were also asked to identify whether the ProActive Heart program had met their needs (‘met all of your needs’, ‘met most of your needs’, or ‘met some of your needs’, ‘met none of your needs’).
Outcome Variables
HRQoL
The SF-36 Survey Version 2 [27] was used to measure HRQoL, as it is a widely used generic health status measure, demonstrates good reliability and validity within cardiac populations [28], and Australian population norms are available [27]. The SF-36 includes 36 questions that yield an eight-scale profile of functional health (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health) as well as two psychometrically based physical (physical component summary or PCS) and mental health (mental component summary or MCS) summary measures [27]. A mean improvement of three to five points is commonly considered clinically significant [29].
Health behaviours
Physical activity was measured using the Active Australia Survey [30] which has been reported as reliable and of acceptable validity within the Australian population [31] and for older adults [32], and test–retest reliability of the survey is similar to the International Physical Activity Questionnaire [33]. Overall weekly physical activity was calculated by adding together the time spent walking, in other moderate-intensity physical activity and in vigorous intensity physical activity (vigorous activity was double weighted to account for additional energy expenditure) [30].
Other health behaviours included self-reported dietary intake [vegetables, fruit, total fat, saturated fat, sodium, dietary cholesterol and alcohol intake (standard drinks per day)] using a validated food frequency questionnaire [34] that estimates intake of most nutrients accurately (within 10 %) and does not systematically under- or over-estimate against weighted records [34], BMI (normal weight, overweight/obese) and smoking status (current smoker).
Study Integrity/Randomisation
The study protocol was approved by the ethics committees of Monash University (2007/0584MC), Royal Brisbane and Women’s Hospital (2007/049) and The Prince Charles Hospital (EC2738) in 2007. The study was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12607000595415). The study design was guided by the CONSORT statement [35, 36]. To ensure fidelity of intervention delivery, the intervention protocol was manualised, and all intervention calls were audio-taped with 10 % reviewed against a session checklist based on the objectives for each session. The sessions were also reviewed by a second rater to investigate inter-rater reliability, with 98 % agreement between reviewers. Finally, the health coaches met with study investigators with expertise in behaviour change for bi-weekly supervision sessions. Project staff, who were tracking data collection, were blinded to the study group. Treatment allocation was stratified by gender to allow for the expected higher proportion of males in the study sample. Randomisation occurred following the completion of baseline assessment using a separate block randomisation list for each stratum. Randomisation was undertaken by the study manager and concealed from investigators.
Statistical Analyses
Sample size analysis indicated that 129 subjects per group (HC and UC) or a total of 258 were required to detect, with 90 % power and type I error of 5 % (two-tailed), an absolute intervention effect of 20 % or greater based on a primary outcome variable of undertaking the recommended level of physical activity. However, sample size was significantly increased above 258 to allow for participant drop-out and sub-group analyses at follow-up.
Descriptive statistics are presented as mean (standard deviation) for continuous variables and as n (%) for categorical variables. We assessed differences at baseline between participants and non-participants, between HC and UC groups, as well as differences at follow up between individuals with complete data and individuals who withdrew or were lost to follow-up using independent sample t tests for continuous variables and Fisher’s exact tests for categorical variables. We compared outcomes at follow-up between the HC and UC groups using linear regression models, with treatment-group and baseline score for the outcome under investigation included as covariates. Results are presented as mean difference (95 % confidence interval).
Health behaviours were also assessed relative to the national guidelines (outlined above). We calculated the proportion of participants in each treatment group who met the guidelines at baseline and follow-up and compared the HC and UC groups using logistic regression analysis. Treatment-group and baseline status for the outcome under investigation were included as covariates in the model. Results are expressed as an odds ratio (95 % CI). Using the likelihood ratio test, we investigated the interaction between HC and participation in other cardiac rehabilitation programs during the intervention period on study outcomes. Statistical significance was set at p ≤0.05. Only individuals with complete data were included in the analyses and all patients were analysed according to their random allocation to group, using Stata statistical software (StataCorp, College Station, TX, USA).
Results
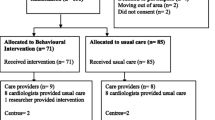
As shown in Fig. 1, a total of 1,333 MI patients were assessed for eligibility in hospital and 550 were eligible and agreed to be contacted by project staff to be involved in the study. Of those 550 patients, 430 were randomised in equal numbers to the HC or UC group (49 did not meet the eligibility criteria as they were no longer available by telephone during the study period, three were deceased and 68 declined to participate further). Six-month assessments were completed by 78 % (n = 337) of participants. There were no significant differences in available baseline characteristics between participants and non-participants (p >0.05). There was also no differential attrition between the study groups or significant differences between completers and non-completers at follow-up in terms of baseline characteristics or outcomes (p > 0.05).
Overall, 83 % of all participants randomised to receive HC received at least five of 10 possible telephone sessions. The median number of sessions was 8 (range 0–10) and the mean (SD) call length was 26 (9.3) min. We found that 95 % of participants were highly satisfied with the ProActive Heart program (78 % were ‘very satisfied’ and 17 % were ‘mostly satisfied’). In total, 98 % of participants stated that the handbook was ‘excellent’ or ‘good’ (52 % and 46 %, respectively), and 98 % of participants stated that the health coaching sessions were ‘useful’. Finally, 98 % of participants said ProActive Heart met their needs (59 % had all of their needs met and 39 % had most of their needs met).
A comparison of demographic and health characteristics at baseline revealed no significant differences between the treatment groups (Table 1). The sample included middle-aged and older adults (mean age = 60.6, SD = 11.8) and 74.7 % (n = 321) were male. Overall, 39 (18.1 %) participants in the HC group and 45 (20.9 %) of participants in the UC group participated in another cardiac rehabilitation program during the intervention period, and this difference between the groups was not significant (p > 0.05). Also, 96 % vs. 97 % of HC and UC participants respectively were taking CHD-related medications at baseline and again this difference was not significant (p > 0.05).
The sample were characterised by poor health characteristics at baseline with 65.1 % (n = 280) reporting a family history of CHD, 22.3 % (n = 96) were diabetic, 55.9 % (n = 236) were hypertensive, mean (SD) total cholesterol was 4.6 (1.2), LDL cholesterol was 2.8 (1.1) and HDL cholesterol was 1.0 (0.4) (Table 1). Across the two HRQoL summary scores and eight sub-scales, mean (SD) scores were below average (<50) at baseline (Table 2). The majority of participants did not meet CHD risk factor guidelines for physical activity, BMI and nutrition (vegetable intake, fruit intake, total fat intake and saturated fat intake). Also, approximately 30 % of participants did not meet the sodium, dietary cholesterol or alcohol recommendations, and approximately 30 % were current smokers (Table 3).
Investigation of intervention effects at follow-up (adjusted for baseline) revealed that the HC group achieved a significantly higher HRQoL score compared with the UC group for MCS (mean difference = 2.7, 95 % CI = 0.5, 4.9, p = 0.02), and for the social functioning (mean difference = 2.3, 95 % CI = 0.1, 4.5, p = 0.04) and role-emotional (mean difference = 2.7, 95 % CI = 0.2, 5.2, p = 0.03) subscales. Also, at follow-up, the HC and UC groups achieved significant improvements in MCS and PCS scores as well as all SF-36 sub-scales except general health. These improvements approached clinical significance (three- to five-point improvement) [29]. The HC and UC groups significantly improved their mean physical activity levels from baseline to follow-up by 49 (232.1) min and 40 (213.1) min, respectively, and there was no significant difference between the treatment groups at follow-up (Table 2).
Investigation of the odds of meeting the recommended guidelines (Table 3) at follow-up (adjusted for baseline) revealed that, compared with UC participants, HC participants were significantly more likely to be sufficiently active (OR = 1.7, 95 % CI = 1.1, 2.7, p = 0.02), to maintain a healthy weight (OR = 2.1, 95 % CI = 1.0, 4.7, p = 0.05), to eat ≥5 serves of vegetables per day (OR = 1.7, 95 % CI = 1.0, 2.8, p = 0.04) and to drink ≤2 standard alcoholic drinks per day (OR = 1.8, 95 % CI = 1.0, 3.2, p = 0.05). Overall, there were no interaction effects between HC and participation in other cardiac rehabilitation programs during the intervention period on the study outcomes (p > 0.14). There was also no significant difference in the proportion of HC (90 %) and UC (88 %) participants taking CHD medications at 6 months (p > 0.05).
Discussion
There is a need for innovative secondary prevention interventions for patients with CHD as participation in traditional programs is low. This study extends the research on the effectiveness of novel secondary prevention programs for CHD patients, reporting on the effect of a telephone-delivered program for MI patients on HRQoL and health behaviours (physical activity, dietary intake, alcohol intake, BMI and smoking status). High levels of intervention delivery were achieved with the HC group experiencing significantly greater improvements in a number of HRQoL subscales compared with the UC group. The HC group were also more likely to be sufficiently active, achieve normal weight, and meet the recommended vegetable and alcohol intake at follow-up, compared with the UC group. Finally, overall, participants were highly satisfied with the ProActive Heart program including the handbook and health coaching sessions, and the program met all or most of their needs.
Only two trials have investigated the effectiveness of telephone-delivered secondary prevention programs on HRQoL using the SF-36 health survey [12] and both found a significant benefit in PCS but not in MCS [12]. From baseline to follow-up, we observed a significant improvement in PCS for the HC and UC groups, but this difference was not significant between groups. However, we observed a significant intervention effect in MCS and in the SF-36 subscales social functioning and role-emotional which approached clinical significance. These results add to the emerging literature supporting the effectiveness of secondary prevention programs offering exercise, education and behavioural interventions on patients’ psychological outcomes [16]. Additional analyses are currently underway to investigate the predictors of the observed improvement in psychological functioning; however, the positive impact may be attributable to the focus of the intervention on psychosocial support for depression and social isolation. In particular, the improvement in social functioning may be a result of the regular telephone contact with the health coach during the intervention period. Also, participation in regular aerobic exercise is an effective treatment for post-MI depression [37], hence improved physical activity may have impacted on the observed improvement in psychological functioning.
Some investigators have reported positive effects of telephone-delivered secondary prevention programs on physical activity, but it has been difficult to draw conclusions due to the variation in reporting and measurement [12, 38]. For example, Vale et al. [38] reported an improvement in physical activity post-intervention; however, they measured whether participants reported ‘taking up walking since discharge’ and subsequently found no intervention effect on the actual duration of walking [38]. In the current study, we used a valid and reliable physical activity measure and found that HC participants were significantly more likely to be sufficiently active at follow-up compared with UC participants. Further, both HC and UC participants reported a significant improvement in mean physical activity at 6 months’ follow-up of 49 and 40 min per week, respectively, and importantly the degree of change in both groups was significant from a public health perspective [39].
The reason for the improvement in physical activity in the UC group is unclear, although observed improvements in physical activity among control group participants in lifestyle intervention trials is not uncommon [40]. There are a number of potential explanations including the recruitment of a highly motivated sample [41], social desirability [42], regression to the mean (a problem associated with intra-participant variation and measurement error, which can occur in trials using pre- and post-intervention measurements, particularly when behavioural screening is employed to select an inactive sample) [43] or the effects of measurement (when measurement alone produces a change in behaviour) [44]. A recent study also found that certain socio-demographic characteristics (being retired and having a secondary school education) predicted an increase in physical activity amongst usual care participants [41].
Compared with UC participants, HC participants were more likely to maintain a healthy weight at follow-up. Previous investigators have demonstrated a trend towards lower BMI in intervention participants compared with controls [12, 38], although they have not reported whether participants were in the healthy weight range post-intervention consistent with the national recommendations for those with CHD [38].
Finally, HC participants were more likely to meet the recommended guidelines for vegetable and alcohol intake at follow-up compared with UC participants. Few studies have reported nutritional status post-intervention and only one has reported a significant change [38]. Vale et al. [38] demonstrated a significantly greater reduction in dietary intake of total fat, saturated fat and cholesterol. However, again it is difficult to interpret the impact of these results as the authors did not report whether intervention participants had met the national recommendations for dietary intake.
The results of this study suggest that the ProActive Heart program is an effective secondary prevention program for MI patients. In addition, the program was highly acceptable to MI patients as program uptake and adherence was very good, program satisfaction levels were very high and the program met all or most of participants’ needs. The telephone-delivered ProActive Heart program can overcome many of the patient-related barriers to participation in traditional secondary prevention such as geographical isolation, lack of transport, poor mobility or early return to work and could thus meet the treatment gap for a number of CHD patients. Further research is required to determine whether it would be effective for other subgroups of CHD patients or other chronic disease groups, although our positive findings suggest that the ProActive Heart program may be acceptable amongst other chronic disease patients vulnerable to non-participation in secondary prevention programs. Additional publications from this study will report the cost-effectiveness of the intervention as well as correlates of the observed improvement in HRQoL and health behaviours post-intervention.
Our study strengths include the well-defined subgroup of CHD patients with the recruitment of MI patients, the high consent rate, the randomised controlled trial design, the comprehensive assessment of HRQoL and behavioural end points using validated measures, the comparison of the study findings with national recommendations and the limited loss to follow-up for a 6-month intervention trial. Importantly, patients who participated in facility-based cardiac rehabilitation programs were not excluded from the study, and participation rates were similar for the HC and UC groups. Also, the treatment benefits of the intervention were similar for those that had participated in such programs and those that had not. Study limitations include the use of self-reported data that may have been limited by recall error and social desirability. Data was also collected by telephone interview which limited our ability to collect objective biomedical data. However, the study outcomes were consistent with those reported in previous trials and all measures have been routinely used in population-based epidemiological and intervention research [30, 34, 45]. Also, the control group received a level of intervention that was more intensive than usual care to reduce the likelihood of differential attrition; the inclusion of a no-treatment control group may have assisted the interpretation of the study findings.
Conclusions
Telephone-delivered CHD secondary prevention programs, such as the ProActive Heart program, are acceptable and can improve HRQoL and CHD risk factor profiles for MI patients. Importantly, this study investigated whether participants had met the national recommendations for reducing risk of CHD and found a significant positive intervention effect across a range of CHD risk factors.
References
Smith Jr SC, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 Update: endorsed by the national heart, lung, and blood institute. Circulation. 2006;113(19):2363–72. May 16, 2006.
Piepoli MF, Corrà U, Benzer W, Bjarnason-Wehrens B, Dendale P, Gaita D, et al. Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the cardiac rehabilitation section of the European association of cardiovascular prevention and rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17(1):1–17. 0.1097/HJR.0b013e3283313592.
Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–72. November 1, 2005.
Joliffe J, Rees K, Taylor R, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Review In: The Cochrane Library. 2003(1):1–41.
Briffa T, Kinsman L, Maiorana AJ, Zecchin R, Redfern J, Davidson PM, et al. An integrated and coordinated approach to preventing recurrent coronary heart disease events in Australia. MJA. 2009;190:683–6.
Davies P, Taylor F, Beswick A, Wise F, Moxham T, Rees K, et al. Promoting patient uptake and adherence in cardiac rehabilitation. The Cochrane Library. 2010(7).
Scott IA, Lindsay KA, Harden HE. Utilisation of outpatient cardiac rehabilitation in Queensland. Med J Aust. 2003;179(7):341–5.
Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002;17:8–17.
Gurewich D, Prottas J, Bhalotra S, Suaya JA, Shepard DS. System-level factors and use of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2008;28(6):380–5.
British Heart Foundation. National Audit of Cardiac Rehabilitation 2011: an annual, BHF funded report into the provision and uptake of cardiac rehabilitation across England, Wales and Northern Ireland. 2011.
Allen JK, Dennison CR. Randomized trials of nursing interventions for secondary prevention in patients with coronary artery disease and heart failure: systematic review. J Cardiovasc Nurs. 2010;25(3):207–20. doi:10.1097/JCN.0b013e3181cc79be.
Neubeck L, Redfern Ju, Fernandez R, Briffa T, Bauman A, Freedman SB. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. J Cardiovasc Risk. 2009;16(3):281–9. June 1, 2009.
Blair J, Corrigal H, Angus NJ, Thompson DR, Leslie S. Home versus hospital-based cardiac rehabilitation: a systematic review. Rural Remote Heal. 2011;11(2):1532–49. Apr–Jun Epub Apr 6.
Redfern J, Briffa T, Ellis E, Freedman SB. Patient-centered modular secondary prevention following acute coronary syndrome: a randomized controlled trial. J Cardiopulm Rehabil Prev. 2008;28(2):107–15. quiz 16–7.
Stewart S, Inglis S, Hawkes A. Chronic cardiac care: A guide to specialist nurse management. London: Blackwell BMJ Books; 2006.
Worcester MUC, Le Grande MR. The role of cardiac rehabilitation in influencing psychological outcomes. Stress Heal. 2008;24(3):267–77.
Heran BS, Chen JMH, Ebrahim S, Moxham T, Oldridge N, Rees K, et al. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011. doi:1002/14651858.CD001800.pub2. Issue 7. Art. No.: CD001800.
Hawkes AL, Atherton J, Taylor CB, Scuffham P, Eadie K. Houston Miller N, et al. Randomised controlled trial of a secondary prevention program for myocardial infarction patients ('ProActive Heart'): study protocol. Secondary prevention program for myocardial infarction patients. BMC Cardiovasc Disord. 2009;9:16–22.
National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand. Guidelines for the management of acute coronary syndromes. MJA. 2006;184:S1–S30.
The Heart Foundation Australia Website. Available from: http://www.heartfoundation.org.au/Heart_Information/Information_by_Phone/Pages/default.aspx.
Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behaviour research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35:358–62.
Bandura A. Social learning theory. Englewood Cliffs: Prentice Hall; 1977.
Bunker SJ, Colquhoun DM, Esler MD, Hickie IB, Hunt D, Jelinek M, et al. "Stress" and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178:272–6.
National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand. Reducing risk in heart disease: guidelines for preventing cardiovascular events in people with coronary heart disease. National Heart Foundation of Australia; 2003.
National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand. Reducing risk in heart disease 2007 (updated 2008).
National Heart Foundation of Australia. My Heart My Life: a manual for patients with coronary heart disease. National Heart Foundation of Australia; 2007.
Hawthorne G, Osborne RH, Taylor A, Sansoni J. The SF36 version 2: critical analyses of population weights, scoring algorithms and population norms. Qual Life Res. 2007;16(4):661–73.
Dempster M, Donnelly M. Measuring the health related quality of life of people with ischaemic heart disease. Heart. 2000;83(6):641–4. June 1, 2000.
Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, et al. Functional status and well-being of patients with chronic conditions. JAMA: J Am Med Assoc. 1989;262(7):907–13. August 18, 1989.
Australian Institute of Health and Welfare (AIHW). The Active Australia Survey: a guide and manual for implementation, analysis and reporting. Canberra: AIHW2003.
Timperio A, Salmon J, Crawford D. Validity and reliability of a physical activity recall instrument among overweight and non-overweight men and women. J Sc Med Sport/Sports Med Aust. 2003;6(4):477–91.
Heesch KC, Hill RL, van Uffelen JGZ, Brown WJ. Are active Australia physical activity questions valid for older adults? J Sci Med Sport. 2010;14(3):233–7.
Brown WJ, Trost SG, Bauman A, Mummery K, Owen N. Test–retest reliability of four physical activity measures used in population surveys. J Sci Med Sport/Sports Med Aus. 2004;7(2):205–15.
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G. The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health. 2000;24(6):576–83.
Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726–32.
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ.340.
Hoffman BM, Babyak MA, Craighead WE, Sherwood A, Doraiswamy PM, Coons MJ, et al. Exercise and pharmacotherapy in patients with major depression: one-year follow-up of the SMILE study. Psychosom Med. 2011;73(2):127–33.
Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, et al. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163(22):2775–83. December 8, 2003.
US Department of Health and Human Services. Physical activity and health: a report of the Surgeon General Atlanta, Georgia: US Department of Health and Human Services, Public Health Service, CDC, National Center for Chronic Disease Prevention and Health Promotion 1996.
Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med. 2012;42(1):81–8.
Waters LA, Reeves MM, Fjeldsoe BS, Eakin EG. Characteristics of control group participants who increased their physical activity in a cluster-randomized lifestyle intervention trial. BMC Publ Health. 2011;11:27.
Sjostrom O, Holst D. Validity of a questionnaire survey: response patterns in different subgroups and the effect of social desirability. Acta Odontol Scand. 2002;60(3):136–40.
Shephard RJ. Regression to the mean. A threat to exercise science? Sports Med. 2003;33(8):575–84.
van Sluijs EM, van Poppel MN, Twisk JW, van Mechelen W. Physical activity measurements affected participants' behavior in a randomized controlled trial. J Clin Epidemiol. 2006;59(4):404–11.
Coyne T, Ibiebele TI, McNaughton S, Rutishauser IHE, O'Dea K, Hodge AM, et al. Evaluation of brief dietary questions to estimate vegetable and fruit consumption? Using serum carotenoids and red-cell folate. Public Health Nutr. 2005;8(03):298–308.
Acknowledgments
This study was funded by a National Health and Medical Research Council project grant #443222. Adrienne O’Neil is supported by a Post Graduate Award from the National Heart Foundation of Australia (PP 08 M4079). The funding bodies had no role in the design or conduct of the study, data extraction or data analyses. We thank The Prince Charles Hospital and Royal Brisbane and Women’s Hospital staff for their support of the study, and acknowledge the dedicated work of our health coaches, Dr Dominique Bird, Ms Brigid Hanley and Ms Bernice Kelly, as well as our telephone interviewers. We thank our research investigators, Professor Paul Scuffam, Ms Nancy Houston Miller and Professor John Bett. We are also grateful for Associate Professor Darren Walters’ support of the study.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hawkes, A.L., Patrao, T.A., Atherton, J. et al. Effect of a Telephone-Delivered Coronary Heart Disease Secondary Prevention Program (ProActive Heart) on Quality of Life and Health Behaviours: Primary Outcomes of a Randomised Controlled Trial. Int.J. Behav. Med. 20, 413–424 (2013). https://doi.org/10.1007/s12529-012-9250-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-012-9250-5