Abstract
Purpose
Patients with myocardial infarction (MI) often report lower health-related quality of life (HRQoL) than those without MI. Interventions can affect HRQoL of these patients. The purpose of this review was to identify effective strategies for improving HRQoL among individuals with MI.
Methods
Three electronic databases were searched and limited to articles peer-reviewed and published in English between 1995 and 2015. We screened titles and abstracts of the retrieved articles for studies that examined effectiveness of interventions to improve HRQoL in patients with MI.
Results
Twenty-three studies were found that examined the effects of behavioural interventions—cardiac rehabilitation programmes (CRP), education and counselling programmes, and other psychological and cognitive interventions—to improve HRQoL in patients with MI. The studies included were mainly randomised controlled trials (14 studies) with a wide age range of participants (18–80 years) and a mean age group of 50–70 years. CRPs, including home- and hospital-based CRPs, regular weekly aerobic training programmes, and group counselling mostly resulted in improvement of HRQoL in patients with MI.
Conclusion
Most CRPs and other interventions were beneficial to MI patients. Therefore, patients with MI should be encouraged to participate in programmes that can help promote their HRQoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the leading cause of death globally [1]; mortality from heart disease increased worldwide between 2000 and 2012 [2]. In particular, myocardial infarction (MI) is a life-threatening event caused by a complete blockage in a blood vessel that supplies blood, oxygen, and nutrients to the heart muscle [3]. The survival of patients with MI has remarkably improved as the result of timely use of thrombolysis and primary percutaneous coronary intervention (PCI) that help restore the flow of the culprit vessels [4]. Yet, these patients frequently experience negative physiological effects such as depression and uncertainty as well as other adverse effects such as a disrupted daily life associated with persistent and/or reoccurring disease symptoms [5]. As a result of MI, patients often report reduced health-related quality of life (HRQoL), which is increasingly recognised as a critical outcome measure in health care [6].
HRQoL is a multidimensional concept that encompasses self-reported measures of physical and mental health [7]. The American Heart Association recommends assessment of HRQoL as an integral part of patient-reported health status assessment in patients with cardiovascular disease [8]. HRQoL has been found to be an independent predictor of death and future cardiac events in patients with MI [5]. In the acute phase of MI, the focus is often placed on physical health; however, after discharge from hospital or considering the long-term effects, HRQoL becomes a significant factor reflecting the impact of the disease on diverse aspects of the patient’s life [5]. Patients with MI and their health care providers often discuss HRQoL to develop a shared view of the disease and treatment outcomes [5, 9]. Some studies [10, 11] suggest HRQoL as an indicator of therapeutic response. This understanding is important to help optimise the management of MI and assist patients to return to a normal active life and to obtain required lifestyle changes.
Health professionals are in a unique position to intervene and support patients as they recover from MI. While medical interventions, thrombolytic therapy, and coronary angioplasty have important roles in survival of patients with MI [12], interventions that improve patients’ recovery after discharge also need to be developed and used to help promote patients’ overall health status, wellbeing and quality of life (QoL). Currently, there is no comprehensive literature review to examine the evidence on QoL interventions for patients with MI. This study aims to review the effectiveness of behavioural interventions to improve the HRQoL of patients with MI.
Methods
Literature Search
Relevant studies were identified by searching the electronic databases including MEDLINE, CINAHL, and PsycINFO. Key search terms included: health-related quality of life/quality of life/HRQoL/QoL and myocardial infarction/heart attack/MI. At the stage of screening, only studies that focused on behavioural interventions were included. Search was limited to English-language and peer-reviewed articles published from 1995 to October 2015. Management of patients with MI has significantly improved over the last couple of decades. Thus, the search was limited to the last 20 years to ensure that the interventions were still relevant.
Study Selection
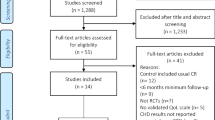
A total of 2523 articles were found from the search, and 1996 were retained after duplicates were removed. Firstly, 1996 articles were screened by titles and abstracts if they reported original data on HRQoL in patients exclusively with MI. 1879 studies were excluded due to irrelevant study subjects, irrelevant dependent variables, and validation studies of measurements. Scientific letters or posters were also excluded, as well as studies of applied qualitative methods were excluded. Articles for which full texts were not available were also excluded. Table 1 describes the inclusion and exclusion criteria of the study. Following the screening of the titles and abstracts, 116 potential articles were selected for further screening. A hand search of the reference lists of relevant published articles was done and resulted in 16 additional articles. Among 132 studies screened by full texts, 109 studies were excluded due to non-interventional studies or studies on medical procedures such as PCI. Finally, 23 studies on HRQoL of MI patients combined with the effects of a particular intervention were included in the present review (Fig. 1).
Results
Participants and setting
Table 2 summarises the characteristics of each study included in the review. Out of 23 articles, 9 studies were conducted in Europe (the UK, Norway, and the Netherlands, 2 studies each, and Finland, Italy, and Ireland, 1 study each). The remaining studies were carried out in North and South America (2 studies in Brazil, and 1 study in the US), Asia (3 studies in Japan, 2 studies in Iran, and 1 study each in Hong Kong, South Korea, Turkey, and China), and Australia (2 studies). The included studies were mainly randomised controlled trials (RCT; 14 studies), followed by prospective studies. Two of the reviewed studies also considered cost-effectiveness as an outcome measure [13, 14], and one study analysed the cost-effectiveness of the programme in an additional separate article [15]. The reviewed studies included a wide age range of participants (18–80 years), with a mean age group of 50–70 years. More male participants were recruited in most of the studies, and one study targeted male patients exclusively [16]. The reviewed studies recruited between 46 and 2481 participants.
Assessment of HRQoL
A number of QoL measures were used to assess HRQoL in the reviewed studies. These included the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), the Sickness Impact Profile (SIP), EuroQol-5D (EQ-5D), the World Health Organization Quality of Life Questionnaire Brief Version (WHOQOL-BREF), the 8-item Life Satisfaction Scale (LSS), a 1–10 ladder technique (Ladder of Life, LOL), the Time Trade-off instrument, and Quality of life, which is a short 10-item visual analogue scale [17], as a generic measurement. SF-36 was one of the most widely used generic tools to measure HRQoL in this patient population [18], used in 11 reviewed studies conducted by Hanssen et al. [19, 20], Hawkes et al. [15], Izawa, Hirano, et al. [21], Izawa, Yamada, et al. [22], Mendes de Leon et al. [23], Uysal and Özcan [24], Wang et al. [18], West et al. [25], Yonezawa et al. [26], Yu et al. [14]. It was a global QoL tool addressing eight domains, including physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health, which were also classified with two psychometrical dimensions—physical component summary (PCS) and mental component summary (MCS) [15]. The measurement was scored from 0 to 100 with lower scores indicating lower HRQoL and higher scores representing better HRQoL [22].
Other studies used disease-specific tools, such as the MacNew Heart Disease HRQoL Instrument (MacNew), the Myocardial Infarction Dimensional Assessment Scale (MIDAS), or the Quality of Life Index (QLI)–Cardiac Version III. Among these specific tools, the MacNew questionnaire was the most commonly used tool to assess HRQoL. MacNew was an improved version of Quality of Life after Myocardial Infarction (QLMI) Questionnaire, consisting of 27 items including physical, emotional, social function domains and five items about symptoms. Each item was scored within a range of 1–7, with higher total scores indicating better HRQoL [27]. In three retrieved studies [18, 24, 28], researchers used both generic and disease-specific QoL instruments.
Interventions to improve the HRQoL of patients with MI
Twenty-three studies were found that examined the effects of behavioural interventions—cardiac rehabilitation programmes (CRP), education and counselling programmes, and other psychological and cognitive interventions—to improve HRQoL in patients with MI. Heterogeneity of the interventions was observed across the reviewed studies; as the result, the studies were grouped and discussed according to the type of intervention. The assessment points of HRQoL of MI patients were mostly comparison between the intervention group and the control group by asking with various patient-reported QoL questionnaires as well as dimensions of HRQoL that were improved after the interventions.
Cardiac rehabilitation programmes
Cardiac rehabilitation programme (CRP) is a comprehensive intervention for improvement of HRQoL in patients who have heart disease. Among the studies reviewed, 11 studies applied CRP, including exercise, education or counselling and monitoring by health professionals, and two studies applied exercise programmes only.
In the present study, CRPs have shown promising results on HRQoL scores of patients with MI. Yu et al. [14] examined the effects of a cardiac rehabilitation and prevention programme on HRQoL of patients with MI, within an age range of 53–75 years. In this RCT, the control group was given standard care without an exercise component. Compared to the control group, participants in the intervention group had significantly higher HRQoL in four domains at the phase 3, and in five domains: the same four domains at the phase 3 plus vitality, at the 2-year follow-up (p < 0.005). The control group reported increased physical pain and no improvement in any of the HRQoL dimensions by phase 2. Only four dimensions of SF-36 were slightly improved at the end of the study period [14].
A supervised exercise-based CRP at the hospital seemed to better improve the QoL of MI patients compared to a home-based unsupervised exercise programme. For example, researchers from Korea compared the effectiveness of a supervised exercise-based CRP with a self-administered home-based exercise programme. The study found that patients in the supervised exercise-based group showed greater improvements in overall QoL scores after 8 weeks (p < 0.0001) compared to the home-based comparison group [29]. These findings imply that the social support and formal structure offered by the supervised programme played an important role in improving QoL.
Findings of a recent study, conducted by Peixoto et al. [30], were also in line with past studies. A significant improvement was observed particularly in the physical and emotional domains in the intervention group, which underwent a 1-month exercise-based CRP (p < 0.001), compared with the control group [30]. Moreover, other 3-month follow-up studies [21, 28] reported positive results in promoting HRQoL among MI patients. In one of these two studies, Japanese participants who completed a CRP had superior HRQoL in four of the eight subscales of the SF-36 (p = 0.000, p = 0.03) to the control group [21]. In the other study, Iranian patients also scored higher in the physical domain of the MacNew (p < 0.05) and the WHOQOL (p < 0.05) after completing a 40-session hospital-based CRP than participants who did not participate in the programme [28].
In Marchionni’s study, participants who attended either a hospital- or home-based CRP for 8 weeks showed better HRQoL than those who did not participate in any of the programmes. Although both interventions were similarly effective in a range of p < 0.001 to p < 0.01, the home-based intervention was more cost-effective than the hospital-based CRP [13]. Likewise, a 6-week home-based CRP using a self-help manual, which contained information about Tai Chi, Qi Gong and Chinese diet, was effective in improving the HRQoL of Chinese patients at 6 weeks and 6 months post-MI (p < 0.05) compared to the control group who received only instructions on taking medications, information leaflets about cardiac risk factors, a healthy diet, and smoking cessation, and a follow-up appointment [18]. Varnfield et al. compared the effectiveness of a 6-week CRP using the smartphone-based Care Assessment Platform Cardiac Rehabilitation (CAP-CR) programme with traditional centre-based CRP. They found that patients in the CAP-CR had higher HRQoL median scores as measured by EQ-5D (p < 0.001). In addition, the CAP-CR group had a low dropout rate with 80 % of participants completing the programme compared to 47 % of the centre-based CRP group [31].
There were two studies that followed up participants, using the SF-36 over a 6-month period [22, 26]. In Izawa, Yamada, et al.’s study [22], the CRP group had significantly higher QoL than the control group in seven domains of the SF-36 at 6 months (p < 0.001); no improvement was observed in social functioning, however. In Yonezawa et al.’s study, the CRP led to significant differences only in bodily pain and social functioning (both p < 0.05) at 6 months [26]. Comparison of the intervention group with the control group among Japanese patients after MI revealed the contrast of the social functioning subscale between these two studies.
A regular weekly aerobic training programme, alone, to the intervention group resulted in greater improvements in HRQoL in patients after MI (p < 0.001) compared with the control group [17]. Changes in HRQoL scores seemed to be affected by the intensity of exercise. Benetti et al. [16] conducted a prospective case–control study and assigned patients into either a 12-week high-intensity physical training or a 12-week moderate-intensity training. Patients in both groups showed significant improvement in HRQoL from baseline (p < 0.05), yet the higher-intensity training resulted in slightly superior HRQoL than the moderate-intensity training and the control group [16]. However, different from the earlier mentioned studies, a study by West et al., which evaluated the long-term effects of an 8-week CRP, failed to show a significant difference between the intervention group and the control group in a 1-year follow-up [25].
Patient education and counselling
Three studies used patient education and counselling to improve HRQoL in post-MI patients [15, 19, 20]. Hawkes et al. examined the effects of a telephone-delivered secondary prevention programme over 6 months including three weekly sessions, three fortnightly sessions, and four monthly sessions. The programme significantly improved the mental component (p = 0.02), the social functioning (p = 0.04), and role-emotional (p = 0.03) subscales of the SF-36 [15].
To assess the long-term effects of an education and counselling intervention via telephone, Hanssen et al. [20] applied weekly phone calls for the first 4 weeks and subsequent calls at 6, 8, 12, and 24 weeks after discharge from MI. The phone follow-ups aimed to help patients solve their common problems or queries after discharge from hospital and to assist patients with their risk factor modification. The results of this RCT showed that the telephone follow-up intervention was effective in increasing HRQoL of patients at a 6-month follow-up compared to the control group [19]. However, the positive effects of the telephone follow-up intervention on HRQoL disappeared at an 18-month follow-up [20].
More recently, the effects of six-session face-to-face interpersonal counselling on HRQoL scores of MI patients were examined [32]. The intervention included a brief introduction by a trained nurse to the framework of the interpersonal counselling, strategies about role transition, and management of therapeutic gains and depressive symptoms. This study found no significant difference in mean HRQoL scores between patients who received interpersonal counselling and the control group. The interpersonal counselling, however, only had a moderate effect on HRQoL of a subgroup of patients aged less than 60 years at either follow-up point [32]. On the other hand, in the study by Uysal and Özcan [24], individual patient education plus counselling positively affected HRQoL of patients after MI. Visual materials were used to provide 1-hour individual training on healthy life after MI in the programme, which was delivered before discharge from hospital. The intervention also included two sessions of telephone counselling on cardiovascular risk-reducing strategies and addressing the patients’ queries in week 14th and 18th following discharge from hospital. The study found greater improvements in HRQoL of patients who participated in the programme (p ≤ 0.000) [24]. It is not, however, clear whether the authors had controlled for cardiac rehabilitation participation as a covariate factor. In line with other counselling interventions, group counselling has also shown promising effects on HRQoL scores. In a study, group counselling resulted in greater HRQoL scores (p < 0.001) at a 1-month follow-up compared to the control group [33].
Other psychological and cognitive interventions
Additional intervention programmes included goal attainment, expressive writing, psychosocial intervention, and short-term humanistic-existential psychotherapy. For example, Boersma et al. [34] assessed the effect of the attainment of three self-selected mid-level goals on HRQoL of patients with MI. These goals were related to health promotion, social activities, and open domain for the coming year. The goal attainment intervention had a positive effect on the social dimension of HRQoL of MI patients (p = 0.05) [34]. Furthermore, there was a unique study, which used language as a means of intervention. Over a period of the study, the intervention group were asked to express their thoughts and feelings about their MI in writing, while the control group were asked to write objectively about their daily events, as they occurred during the year before heart attack. Patients in the expressive writing group showed superior overall HRQoL scores to the control group (p < 0.05). This intervention was cost-effective as it costed only for pens, paper, and envelopes, and had 68 % of response rate [35].
Psychological interventions were also applied to MI patients in the ENRICHD clinical trial [23] and the STEP-IN-AMI trial [36]. The counselling programmes are usually similar to education or questioning and answering; on the other hand, the psychosocial intervention of ENRICHD trial was composed of cognitive behavioural therapy for MI patients who had at least one previous episode of major depression, pharmacotherapy for patients with severe depression, and training of strategies to help with social skill deficits and automatic thoughts or self-talk. The study found significant differences in the mental components of the SF-36 between the intervention group and the control group (2.2; 95 % confidence interval 1.2–3.2); however, no differences were found in the physical components (0.8; 95 % confidence interval −0.5 to 2.0) [23]. In consistent with the above study, a short-term humanistic-existential psychotherapy (STP) used in the STEP-IN-AMI trial enhanced the physical dimension of the MacNew instrument (p = 0.03). The intervention consisted of three to ten 1-hour individual sessions, which focused on patient personal history, body language insights, and relaxation techniques, as well as five group sessions over 3 months. The group sessions included information about MI, cardiac risk factors, lifestyle changes, music-guided breathing and muscular relaxation, comprehension of body signals, elements of oneiric language, and attention to specific partner/relationship issues. The study found that the physical domain of HRQoL was significantly improved in the intervention group compared to the control group. Also, positive trends in the social domain and overall HRQoL in the favour of the intervention were found [36].
Discussion
Overall, the studies included in this review showed promising results in improving HRQoL of MI patients. The studies included heterogeneous behavioural interventions, with cardiac rehabilitation programmes being the most commonly reported [28, 29]. Patients who participated in either hospital-based or home-based CRP showed higher HRQoL than those who did not participate in any CRP [13, 28]. This finding is in line with other studies which demonstrated positive effects from CRP on HRQoL of patients with coronary heart disease [37, 38]. Supervised hospital-based CRPs were shown to be superior to unsupervised home-based programmes. However, if supervised, home-based CRPs showed only little difference with hospital-based cardiac rehabilitations [13, 39]. The positive effects of CRPs on HRQoL of MI patients were found to be independent from the cost and duration of these programmes [32]. Similarly, a systematic review that compared home- versus hospital-based CRPs suggested that home-based CRPs are safe and effective on many patient and disease outcomes of cardiac patients including quality of life [40]. Moreover, a study that conduced cost analysis on CRPs found that hospital-based CRP costed an average US$21,298, while the cost for home-based CRP and no programme was estimated to be US$13,246 and US$12,433, respectively [13]. Therefore, home-based CRPs may be a better option for some patients.
In addition, the available evidence suggests that exercise is an important element of CRPs, which positively affects HRQoL of patients with MI [16, 39]. Similarly, a systematic review revealed that most of the exercise-based cardiac rehabilitation programmes promised improvements in QoL of patients with coronary heart disease including patients with MI [37]. In particular, Tai Chi exercise had positive effects on post-menopausal female patients with coronary heart disease, as this exercise is designed similarly to walking exercises with low–moderate intensity [41]. Therefore, it is important that cardiac rehabilitation programmes be based upon moderate-intensity exercise. However, the effects of exercise intensity on HRQoL in patients with MI need further investigation. While Benetti et al. [16] demonstrated a superior effect from high-intensity exercise, a more outdated study conducted by Worcester et al. [42] suggested no significant difference in HRQoL scores between patients who participated in low-intensity and high-intensity exercises. In their study, Worcester et al. [42] described the high-intensity exercise programme as consisting of three 1-hour sessions per week delivered by a teacher of physical education and a doctor, while the low-intensity exercise programme included two 1-hour sessions per week of light calisthenics and intermittent exercise [42]. To sum up, although there is no strong evidence to support or reject the effects of exercise intensity on HRQoL, exercise is crucial for successful interventional programmes.
Other behavioural interventions including patient education and counselling, psychological, and cognitive interventions also showed potential to improve QoL of patients with MI. Goal setting and goal attainment [34], telephone individual patient counselling [32], group counselling [33], and expressing writing [35] were found to positively affect QoL of MI.
The studies reviewed mainly used a generic tool to assess HRQoL in the target patient population. This is in line with the overall fact that specific instruments are less likely to be used than generic tools [29]. Generic tools have the advantage of being applied to a wider range of individuals from full health to death. This feature enables comparison of QoL scores across diseases and the normal population. Nevertheless, disease-specific measurements are apt for assessing HRQoL in a specific population [43]. These tools are more sensitive to treatment effects among a specific population group [44]. Although it is found that the SF-36 and the Mac New Quality of Life Questionnaire were found to be the most commonly used generic and disease-specific tools, respectively, for measuring HRQoL of patients with MI [45], the disease-specific instruments can better reflect the effects of interventions on HRQoL in this patient population. Thus, their use should be encouraged in studies that aim to follow the changes in HRQoL of MI over time or evaluate the effects of a particular intervention or treatment.
The findings of this review indicate that interventions usually improve some, not all, dimensions of the HRQoL, suggesting that a combination of interventions may be necessary to improve multiple dimensions of HRQoL. Additionally, there is a need for development of interventions that can result in a sustainable improvement in HRQoL of patients with MI. Long-term supportive programmes, as opposed to one-off interventions, might lead to a superior and long-lasting improvement in HRQoL of MI patients.
In this review, the studies evaluated CRP and other interventions with a range of duration from 1 to 18 months. Most interventions lasted a short term up to 6 months and usually showed positive effects on HRQoL of participants with MI [19]. Likewise, in a systematic review about QoL among CHD patients, most of the exercise-based cardiac rehabilitation programmes promised improvements with duration of programmes ranging from 1 to 12 months, where the frequency differed from one to seven sessions per week of 20–90 min length [37]. The included studies mostly examined the short-term effects of behavioural interventions on HRQoL of patients with MI and found positives results. The long-term effects of these interventions are unclear, however. Future studies should focus on evaluating the long-term effects of the cardiac rehabilitation programmes, counselling, and other behavioural interventions on HRQoL of patients with MI.
The effects of behavioural interventions on quality of life of MI patients were predominately studied on male participants. This is consistent with the fact that the incident rate of MI is higher in males than in females [46]. However, several studies reported that female patients showed more impaired HRQoL than their male counterparts within the first year after MI [47–50]. It is necessary to understand the reasons why women report poorer HRQoL than men and whether particular dimensions of HRQoL are more affected in women. This understanding is required to develop and test targeted invitations aiming to reduce gender disparities in the experience of QoL in patients with MI.
Since HRQoL is subjective, studies rely on self-report measurements and must be aware of potential bias based on self-assessment [13, 51]. In addition, there were several limitations such as the small sample size, the considerable proportion of excluded patients, and the absence of a blinded condition. For instance, the effectiveness of expressive writing has not yet been widely proved, and thus, assessment of various interventions should be conducted with a larger sample size of the patient population.
Limitations
Despite our comprehensive methods, it is difficult to ascertain how many studies we did not include in this review. Additionally, limiting our search strategy to English-language articles and excluding grey literature may have resulted in under-representation of research from regions outside English-speaking countries.
This narrative review cannot quantify the effect size of QOL interventions for patients with MI. Therefore, the review is not able to recommend what is the best intervention to improve QoL in these patients. A rigorously conducted meta-analysis is needed to determine the precise effects of the available interventions [52].
Conclusion
Most CRPs and other behavioural interventions improved the HRQoL of patients with MI. Interventions that help increase patients’ functional and psychosocial wellbeing should be introduced before long after discharge from hospital to promote patients’ overall health and quality of life.
Implications
Patients with MI should be encouraged to participate in programmes that can help promote their HRQoL.
References
World Health Organisation (2015). Fact sheet N°317: Cardiovascular diseases (CVDs). http://www.who.int/mediacentre/factsheets/fs317/en/viewed. February 2015.
World Health Organisation (2014). Fact sheet N°310: The top 10 causes of death. http://www.who.int/mediacentre/factsheets/fs310/en/viewed. February 2015.
Thygesen, K., Alpert, J. S., Jaffe, A. S., White, H. D., Simoons, M. L., Chaitman, B. R., et al. (2012). Third universal definition of myocardial infarction. Journal of the American College of Cardiology, 60(16), 1581–1598.
Runge, M. S., Stouffer, G., & Patterson, C. (2010). Netter’s cardiology. Philadelphia, PA: Elsevier Health Sciences.
Eriksson, M., Asplund, K., Hochwälder, J., & Svedlund, M. (2013). Changes in hope and health-related quality of life in couples following acute myocardial infarction: A quantitative longitudinal study. Scandinavian Journal of Caring Sciences, 27(2), 295–302.
Foxwell, R., Morley, C., & Frizelle, D. (2013). Illness perceptions, mood and quality of life: A systematic review of coronary heart disease patients. Journal of Psychosomatic Research, 75(3), 211–222.
Centres for Disease Control and Prevention (2012). Health-related quality of life (HRQOL). http://www.cdc.gov/hrqol/Retrieved. 26 September 2014.
Rumsfeld, J. S., Alexander, K. P., Goff, D. C., Graham, M. M., Ho, P. M., Masoudi, F. A., et al. (2013). Cardiovascular health: The importance of measuring patient-reported health status a scientific statement from the american heart association. Circulation, 127(22), 2233–2249.
Wingate, S. (1995). Quality of life for women after a myocardial infarction. Heart and Lung, 24(6), 467–473.
Sun, J., Buys, N., & Jayasinghe, R. (2014). Effects of community-based meditative Tai Chi programme on improving quality of life, physical and mental health in chronic heart-failure participants. Aging and Mental Health, 18(3), 289–295.
Dal Boni, A. L. M., Martinez, J. E., & da Silva Saccomann, I. C. R. (2013). Quality of Life of patients undergoing coronary artery bypass grafting. Acta Paulista de Enfermagem, 26(6), 575–580.
Pettersen, K. I. (2008). Health-related quality of life after myocardial infarction: methods for assessment and determinants. PhD, University of Oslo.
Marchionni, N., Fattirolli, F., Fumagalli, S., Oldridge, N., Del Lungo, F., Morosi, L., et al. (2003). Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction results of a randomized, controlled trial. Circulation, 107(17), 2201–2206.
Yu, C. M., Lau, C. P., Chau, J., McGhee, S., Kong, S. L., Cheung, B. M. Y., et al. (2004). A short course of cardiac rehabilitation program is highly cost effective in improving long-term quality of life in patients with recent myocardial infarction or percutaneous coronary intervention. Archives of Physical Medicine and Rehabilitation, 85(12), 1915–1922.
Hawkes, A. L., Patrao, T. A., Atherton, J., Ware, R. S., Taylor, C. B., O’Neil, A., et al. (2013). Effect of a telephone-delivered coronary heart disease secondary prevention program (ProActive Heart) on quality of life and health behaviours: Primary outcomes of a randomised controlled trial. International Journal Of Behavioral Medicine, 20(3), 413–424. doi:10.1007/s12529-012-9250-5.
Benetti, M., Araujo, C. L. P. D., & Santos, R. Z. D. (2010). Cardiorespiratory fitness and quality of life at different exercise intensities after myocardial infarction. Arquivos Brasileiros de Cardiologia, 95(3), 399–404.
Dugmore, L., Tipson, R., Phillips, M., Flint, E., Stentiford, N., Bone, M., et al. (1999). Changes in cardiorespiratory fitness, psychological wellbeing, quality of life, and vocational status following a 12 month cardiac exercise rehabilitation programme. Heart, 81(4), 359–366.
Wang, W., Chair, S. Y., Thompson, D. R., & Twinn, S. F. (2012). Effects of home-based rehabilitation on health-related quality of life and psychological status in Chinese patients recovering from acute myocardial infarction. Heart and Lung: The Journal of Acute and Critical Care, 41(1), 15–25.
Hanssen, T. A., Nordrehaug, J. E., Eide, G. E., & Hanestad, B. R. (2007). Improving outcomes after myocardial infarction: A randomized controlled trial evaluating effects of a telephone follow-up intervention. European Journal of Cardiovascular Prevention and Rehabilitation, 14(3), 429–437.
Hanssen, T. A., Nordrehaug, J. E., Eide, G. E., & Hanestad, B. R. (2009). Does a telephone follow-up intervention for patients discharged with acute myocardial infarction have long-term effects on health-related quality of life? A randomised controlled trial. Journal of Clinical Nursing, 18(9), 1334–1345.
Izawa, K., Hirano, Y., Yamada, S., Oka, K., Omiya, K., & Iijima, S. (2004). Improvement in physiological outcomes and health-related quality of life following cardiac rehabilitation in patients with acute myocardial infarction. Circulation Journal: Official Journal Of The Japanese Circulation Society, 68(4), 315–320.
Izawa, K. P., Yamada, S., Oka, K., Watanabe, S., Omiya, K., Iijima, S., et al. (2004). Long-term exercise maintenance, physical activity, and health-related quality of life after cardiac rehabilitation. American Journal Of Physical Medicine and Rehabilitation/Association Of Academic Physiatrists, 83(12), 884–892.
Mendes de Leon, C. F., Czajkowski, S. M., Freedland, K. E., Bang, H., Powell, L. H., Wu, C., et al. (2006). The effect of a psychosocial intervention and quality of life after acute myocardial infarction: The Enhancing Recovery in Coronary Heart Disease (ENRICHD) clinical trial. Journal of Cardiopulmonary Rehabilitation, 26(1), 9–13.
Uysal, H., & Özcan, Ş. (2012). The effect of individual training and counselling programme for patients with myocardial infarction over patients’ quality of life. International journal of nursing practice, 18(5), 445–453.
West, R. R., Jones, D. A., & Henderson, A. H. (2012). Rehabilitation after myocardial infarction trial (RAMIT): Multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart (British Cardiac Society), 98(8), 637–644. doi:10.1136/heartjnl-2011-300302.
Yonezawa, R., Masuda, T., Matsunaga, A., Takahashi, Y., Saitoh, M., Ishii, A., et al. (2009). Effects of phase II cardiac rehabilitation on job stress and health-related quality of life after return to work in middle-aged patients with acute myocardial infarction. International Heart Journal, 50(3), 279–290.
Höfer, S., Lim, L., Guyatt, G., & Oldridge, N. (2004). The MacNew Heart Disease health-related quality of life instrument: A summary. Health Qual Life Outcomes, 2(1), 3.
Yousefy, A., Keshtiaray, N., Yamani, N., Rabiei, K., & Baghbranian, P. (2009). Quality of life in post myocardial infarction patients with or without cardiac rehabilitation. Research Journal of Biological Sciences, 4(1), 54–58.
Choo, J., Burke, L. E., & Hong, K. P. (2007). Improved quality of life with cardiac rehabilitation for post-myocardial infarction patients in Korea. European Journal of Cardiovascular Nursing, 6(3), 166–171.
Peixoto, T. C. A., Begot, I., Bolzan, D. W., Machado, L., Reis, M. S., Papa, V., et al. (2015). Early exercise-based rehabilitation improves health-related quality of life and functional capacity after acute myocardial infarction: A randomized controlled trial. The Canadian Journal Of Cardiology, 31(3), 308–313. doi:10.1016/j.cjca.2014.11.014.
Varnfield, M., Karunanithi, M., Lee, C.-K., Honeyman, E., Arnold, D., Ding, H., et al. (2014). Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: Results from a randomised controlled trial. Heart, 100(22), 1770–1779. doi:10.1136/heartjnl-2014-305783.
Oranta, O., Luutonen, S., Salokangas, R. K., Vahlberg, T., & Leino-Kilpi, H. (2011). The effects of interpersonal counselling on health-related quality of life after myocardial infarction. Journal of Clinical Nursing, 20(23–24), 3373–3382.
Bagheri, H., Memarian, R., & Alhani, F. (2007). Evaluation of the effect of group counselling on post myocardial infarction patients: Determined by an analysis of quality of life. Journal of Clinical Nursing, 16(2), 402–406.
Boersma, S. N., Maes, S., Joekes, K., & Dusseldorp, E. (2006). Goal processes in relation to goal attainment: Predicting health-related quality of life in myocardial infarction patients. Journal of Health Psychology, 11(6), 927–941.
Hevey, D., & Wilczkiewicz, E. (2014). Changes in language use mediate expressive writing’s benefits on health-related quality of life following myocardial infarction. Health Psychology and Behavioral Medicine, 2(1), 1053–1066.
Roncella, A., Pristipino, C., Cianfrocca, C., Scorza, S., Pasceri, V., Pelliccia, F., et al. (2013). One-year results of the randomized, controlled, short-term psychotherapy in acute myocardial infarction (STEP-IN-AMI) trial. International Journal of Cardiology, 170(2), 132–139. doi:10.1016/j.ijcard.2013.08.094.
Heran, B. S., Chen, J. M., Ebrahim, S., Moxham, T., Oldridge, N., Rees, K., et al. (2011). Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD001800.pub2.
Kim, S. S., Lee, S., Kim, G., Kang, S. M., & Ahn, J. A. (2014). Effects of a comprehensive cardiac rehabilitation program in patients with coronary heart disease in Korea. Nursing and Health Sciences, 16(4), 476–482. doi:10.1111/nhs.12155.
Anderson, L., & Taylor, R. S. (2014). Cardiac rehabilitation for people with heart disease: An overview of Cochrane systematic reviews. International Journal of Cardiology, 177(2), 348–361.
Blair, J., Corrigall, H., Angus, N. J., Thompson, D. R., & Leslie, S. (2011). Home versus hospital-based cardiac rehabilitation: A systematic review. Rural and Remote Health, 11(2), 1–17.
Song, R., Ahn, S., So, H. Y., Park, I. S., Kim, H. L., Joo, K. O., et al. (2009). Effects of Tai Chi exercise on cardiovascular risk factors and quality of life in post-menopausal women. Journal of Korean Academy of Nursing, 39(1), 136–144.
Worcester, M. C., Hare, D. L., Oliver, R. G., Reid, M. A., & Goble, A. (1993). Early programmes of high and low intensity exercise and quality of life after acute myocardial infarction. BMJ, 307(6914), 1244–1247.
Oldridge, N., Gottlieb, M., Guyatt, G., Jones, N., Streiner, D., & Feeny, D. (1998). Predictors of health-related quality of life with cardiac rehabilitation after acute myocardial infarction. Journal of Cardiopulmonary Rehabilitation, 18(2), 95–103.
Bengtsson, I., Hagman, M., & Wedel, H. (2001). Age and angina as predictors of quality of life after myocardial infarction: A prospective comparative study. Scandinavian Cardiovascular Journal: SCJ, 35(4), 252–258.
Dempster, M., Donnelly, M., & O’Loughlin, C. (2004). The validity of the MacNew Quality of Life in heart disease questionnaire. Health and Quality of Life Outcomes, 2, 6. doi:10.1186/1477-7525-2-6.
Brink, E., Karlson, B., & Hallberg, L.-M. (2002). Health experiences of first-time myocardial infarction: Factors influencing women’s and men’s health-related quality of life after five months. Psychology, Health and Medicine, 7(1), 5–16.
Bogg, J., Thornton, E., & Bundred, P. (2000). Gender variability in mood, quality of life and coping following primary myocardial infarction. Coronary Health Care, 4(4), 163–168.
Garavalia, L. S., Decker, C., Reid, K. J., Lichtman, J. H., Parashar, S., Vaccarino, V., et al. (2007). Does health status differ between men and women in early recovery after myocardial infarction? Journal of Women’s Health, 16(1), 93–101.
Norris, C. M., Hegadoren, K., & Pilote, L. (2007). Depression symptoms have a greater impact on the 1-year health-related quality of life outcomes of women post-myocardial infarction compared to men. European Journal of Cardiovascular Nursing, 6(2), 92–98.
Kristofferzon, M. L., Löfmark, R., & Carlsson, M. (2005). Perceived coping, social support, and quality of life 1 month after myocardial infarction: A comparison between Swedish women and men. Heart & Lung: The Journal of Acute and Critical Care, 34(1), 39–50.
Bucholz, E. M., Rathore, S. S., Gosch, K., Schoenfeld, A., Jones, P. G., Buchanan, D. M., et al. (2011). Effect of living alone on patient outcomes after hospitalization for acute myocardial infarction. American Journal of Cardiology, 108(7), 943–948. doi:10.1016/j.amjcard.2011.05.023.
Samartzis, L., Dimopoulos, S., Tziongourou, M., & Nanas, S. (2013). Effect of psychosocial interventions on quality of life in patients with chronic heart failure: A meta-analysis of randomized controlled trials. Journal of Cardiac Failure, 19(2), 125–134.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kyoungrim Kang declares that she has no conflict of interest. Leila Gholizadeh declares that she has no conflict of interest. Sally Inglis declares that she has no conflict of interest. Hae-Ra Han declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kang, K., Gholizadeh, L., Inglis, S.C. et al. Interventions that improve health-related quality of life in patients with myocardial infarction. Qual Life Res 25, 2725–2737 (2016). https://doi.org/10.1007/s11136-016-1401-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1401-8