Abstract
Coronary CT angiography (CTA) has become a well-accepted imaging modality in the evaluation of coronary artery disease (CAD) due to its high negative predictive value. The ability to exclude CAD in patients presenting with chest pain in a low to intermediate risk population makes it very useful in emergency departments for optimizing resource utilization and reducing expenditure. The limited availability of trained cardiac imagers is a potential obstacle in implementing this strategy. Towards the goal of prompt and accurate interpretation of coronary CTA, there has been a recent interest in the development of automated coronary CTA interpretation and reporting. This article aims to review the current applications and scientific evidence on the utility of automated techniques for interpretation and reporting of coronary CTA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary CT angiography (CTA) has become a well-accepted imaging modality in the evaluation of coronary artery disease. The high negative predictive value of this modality has been demonstrated in several multicenter trials, which makes it very useful in the exclusion of coronary artery disease in low to intermediate risk population [1]. Several centers have implemented coronary CTA to exclude the presence of coronary artery disease in patients presenting with acute chest pain, but with low to intermediate pre-test probability. Coronary CTA has been shown to be useful in the emergency room in establishing the etiology for patients presenting with chest pain, reduce the time to diagnosis, and decrease the duration of hospital stay [2]. The recently published ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial showed the utility of CT in improving resource utilization and reducing expenditure [3]. A negative CT scan also predicts absence of future major adverse cardiovascular outcomes [4]. However, interpretation of coronary CTA requires highly trained cardiac imagers, who may not be routinely available outside normal working hours. Interpretation of coronary CTA may take up to 30–40 minutes since it requires careful analysis of all the segments of the coronary arteries in multiple orientations and possibly several phases of the cardiac cycle.
Computer aided detection (CAD) is being successfully used in several anatomic regions, including mammography for detection of breast lesions, chest CT for detection of lung nodules, and in CT colonography for detection of polyps. Although coronary artery disease is one of the most common medical problems encountered in the western world, computer-aided detection has not yet been utilized on a large scale.
Interpretation of coronary CTA typically requires complex postprocessing, which includes segmentation of coronary arteries, centerline extraction, and evaluation of the coronary arterial wall and lumen. Typically, this is performed using multiple projections, such as multiplanar reconstruction (MPR) in the short axis of the vessel for evaluation of plaque and lumen, curved MPR for evaluation of a tortuous branch in a single 2D image and maximum intensity projections (MIP) for analysis of complex anatomy. Using a combination of multiple techniques and planes, the presence and extent of plaque as well as the presence and severity of luminal stenosis/occlusions can be determined. Because of these complex postprocessing needs, a significant amount of time and a well-qualified reader are often required for interpretation of coronary CTAs.
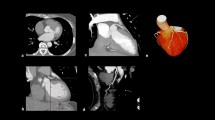
Automated techniques have been used for calcium scoring and semiautomated techniques have been used for segmentation and display of coronary arteries to provide more reproducible measurements and reduce inter and intra observer variability [5–10]. There are several algorithms that are available for automatic centerline extraction of the coronary arteries from CCTA. These algorithms are based on several different techniques including morphologic operators [11], model fitting [12], medialness filter [13], or fuzzy connectedness [14]. Often, these techniques are not completely successful regarding the extraction of the distal coronary arterial tree. More accurate techniques include combination of gradient vector flow and Frangi’s vesselness measure [15–18] or connected component analysis and wave propagation [19]. Another technique is an improved Frangi’s vesselness filter, which uses a discriminator based on local geometric features to decrease false positive responses in Frangi’s vesselness filter [10]. In the last mentioned technique, preprocessing, improved Frangi’s vesselness filter, automatic ostium detection, centerline extraction, branch searching, and centerline refinement are performed with minimal human interaction (Fig. 1). Full description of these algorithms is beyond the scope of this article. The algorithms have been evaluated using Rotterdam Coronary Artery Algorithm Evaluation Framework, which consists of 128 reference centerlines that were used in MICCAI Coronary artery tracking challenge (CAT08) [19]. Most of these techniques require some form of human interaction to correct for incorrect segmentation/centerline extraction,
Semiautomatic centerline extraction and lesion analysis using the algorithm of Yang et al (QAngio CT Research Edition, Medis Medical Imaging Systems, Leiden, The Netherlands) [10]. (A) Image of LAD has been extracted from CTA data and shown as blue curve in 3D and curved MPR on the right. Automatically calculated segment labels and positions are also shown in the 3D view. (B) Initial step of the automatic contour detection showing 4 longitudinal cuts of the stretched MPR stack of the LAD. The lumen (yellow) and vessel (orange) contours are automatically detected. Manual modifications to the contours at this stage can be used to improve the transversal contour detection in the next step. The current transversal slice position is synchronized with the 3 orthogonal views on the side and indicated in the 3D view. (C) After transversal contour detection, the current intersections of the contours with the curved MPR as shown in the left panel. Also the segment labels are shown. The mean diameter of the lumen (yellow) and orange (vessel) contours are show in the graph. The x-axis shows the distance (in mm) from the aorta. (D) Automated lesion analysis in the proximal LAD. The markers in the curved MPR and the graph indicate the lesion definition markers. The markers "S" (green) and "E" (red) indicate the region of interest of the lesion. The reference lines in the graph are calculated based on a regression analysis of the diameters in this region. The "P" and "D" (blue) markers indicate the extent of the lesion. The "O" marker indicates the location of the MLD. Lesion definitions are shown in the full graph. In the transversal lumen contour the minimal diameter is also indicated. Images courtesy of de Graaf MA, Kitslaar PH, Leiden University Medical Center, The Netherlands
Using a fully automated system for the interpretation and reporting of coronary CTA has many potential applications including in the emergency departments. Several studies have recently explored the utility of automated systems in evaluating coronary CTA [20••, 21].
This article aims to review the current evidence on the utility of automated coronary CTA techniques for interpretation and reporting, and the probable limitations.
Techniques
To our knowledge, there are currently 2 computerized automated algorithms for interpretation and reporting of coronary CTA studies. One is the COR Analyzer, (Rcadia, Haifa, Israel) [22] and the other is the Siemens software (Siemens AG, Erlangen, Germany) described by Kelm et al [21]. The COR Analyzer v. 1.8R755 (Rcadia, Auburndale, MA) [23] is approved by the FDA.
The COR Analyzer algorithm performs automated CTA in 3 steps, namely coronary artery segmentation, coronary artery labeling, and detection of stenosis [24]. In the initial step, lungs are detected as air filled areas that are segmented using morphologic filters and distinguished from air outside the body by a set of heuritistics. Mediastinum is segmented as the area between the lungs. Ascending aorta is detected using circular Hough transform, which looks at circular cross sectional within the mediastinum in the axial slices and then segmented using 3D active surface minimization, based on the distinct edges of contrast filled aorta with surrounding structures. Coronary arteries are segmented by following contrast filled areas connected with the ascending aorta and tracked by following tubular components attached to it [20••].
Coronary arteries are then labeled using a probabilistic model that utilizes reference CTA studies that were used to train the algorithm. Main arteries such as the left main (LM), left anterior descending (LAD), left circumflex (LCX), and right coronary artery (RCA) are labeled and validated based on spatial relationships between arteries (Fig. 2). If there is as a variation of the arterial anatomy, such as anomalies where a major artery is missing, it will be read as incomplete segmentation [20••, 22].
Right anterior oblique (A) and left anterior oblique (B) views of the aortic root and coronary arterial tree using the Cor A algorithm, which involved automatic segmentation, centerline extraction, and labeling of branches. With kind permission from Springer Science+Business Media: Goldenberg R, Eilot D, Begelman G, et al. Computer-Aided Simple Triage (CAST) for coronary CT angiography: Fig. 4. Int J Comput Assist Radiol Surg 2012;7:819–827
The labeled coronary arteries are then analyzed following split of the vessels into disjoint segments. The lumen and the wall are delineated using iterative model based variation. Calcified lesions are detected and segmented by hyestersis based adaptive binarization. Noncalcified plaques are detected as hypodense areas without calcium between the vessel wall and the lumen. Each segment is analyzed for cross sectional area (of vessel and lumen), plaque (presence, size), noise, artifacts (presence, extent), bifurcations, and distance from ostium. These features are then matched with characteristic lesions that were used to train the algorithm. Detection marks are placed over significant stenotic areas (>50 %) along an automatically generated curved multiplanar reformation along the centerline of the vessel and warning marks are placed over segments with potential processing failure [20••].
At every step in this algorithm, validation tests are performed to verify the correctness of the process. The system reports a failure if the confidence level of the result is low or it reports a warning if there is a problem in a part of the study. The system determines the adequacy of vessel tracking, abrupt vessel disappearance, imaging artifacts, low likelihood of named vessel to specific coronary artery, and insufficient coverage of AV groove by tracked vessels. The total time for all the above mentioned steps is expected to be 5–7 minutes [20••].
A report is generated with each coronary artery coded with a different color, and significant stenotic areas marked by thick red overlay. An orthogonal set of images with the ability to scroll through coronary vessels to evaluate stenosis identified on color coded coronary tree is also provided. A table showing the interpretation of stenosis for each vessel and branch is also provided.
The second algorithm by Siemens described by Kelm et al has 4 steps, namely vessel tracing, centerline verification, lumen estimation, and stenosis detection and classification [21].
In this algorithm, vessel tracing is performed using multi-scale medialness filters in a graph based algorithm that extracts centerlines of the 4 major arteries (LM, LAD, LCX, RCA) and their major first order branches by computing minimum-cost paths.
Centerline verification is an additional step that is used in this algorithm. Using learning based method, noncoronary portions of the study such as coronary veins, pulmonary vessels, and cardiac chambers are excluded. The algorithm also traces centerlines in vessels completely occluded by non-calcified plaques that have the same attenuation as that of the vessel wall. A cylindrical sampling pattern for feature extraction with its axis aligned to coronary centerline is employed and multiple rotation invariant features are extracted along the entire length of cylinder at varying radii, which are then used to train a random forests (RF) classifier. When a particular coronary artery is extracted, the RF classifier generates a probability that a given point in centerline belongs to a non-vessel structure. Points with scores higher than a particular threshold are then eliminated from further analysis.
Luminal dimensions are estimated along the centerline using an automatic nonlinear regression method to directly estimate the vessel radius and cross sectional area from local image features. Using imaging features and feature vectors of the vessel, a regression tree is evaluated by following its splits from the root to a leaf with an associated radius. This method of luminal estimation using regression analysis is considered significantly faster than luminal segmentation approach [21].
Stenosis is detected and quantified along the lumen as max-min-max triples of baseline-corrected and smoothed radius curve along with an estimation of grade. From the estimated radius, stenosis is identified and estimated. The vessel tree is decomposed into disjoint segments, starting from ostium or vessel bifurcation and subsequently analyzed. Stenosis is graded as significant, >50 % or discarded <50 % or short <0.9 mm or narrow (<1 mm) or close to distal end of vessel (<7.5 mm). Then using probability scores obtained from classifiers, stenosis is classified as calcified, non-calcified, or mixed type [21].
Applications of Automated Coronary CTA Interpretation and Reading
There are several clinical scenarios where an automated coronary CTA interpretation and reading could be useful.
One situation where this system has the highest potential is in emergency department for patients who present with acute chest pain. CTA is increasingly used in emergency departments in patients with suspected acute coronary syndromes who have low to intermediate probability of coronary artery disease, with indeterminate EKG or enzyme findings, to exclude coronary artery disease [3]. As described above, several studies have demonstrated the utility of CTA in this scenario [2]. However, a major obstacle in the implementation of this strategy is the lack of availability of adequately trained cardiac imagers outside normal working hours. Accurate interpretation of coronary CTA require trained cardiac imagers, who will require significant amount of time for evaluation of the entire coronary tree since it requires substantial post processing including multi-planar reconstructions in several projections. Since the primary intention of using CT in this setting is to optimize resource utilization and discharge patients at the earliest, it is imperative to provide a prompt reading. In such a scenario, it might be useful to implement an automated coronary CTA interpretation and reporting algorithm.
After CTA is performed, the images could be sent to a workstation where the software performs a completely automated analysis and give preliminary result on whether there is a significant (>50 %) stenosis or not or if the result is indeterminate. If there is no significant stenosis, the patient can be discharged and a full report can be furnished when an expert radiologist is available. If there is suspicion of a significant stenosis, an expert reader can be alerted to provide a final report and the patient can be admitted to the hospital for further intervention and management. This algorithm would in this way optimize utilization of available resources, providing confidence to less trained personnel for excluding coronary artery disease and utilizing the expert readers only for positive cases.
Another potential use is as a second reader to enhance the interpretation of expert readers. This concept has been used in other anatomical regions such as mammography, CT of lung nodules, and CT colonography for detection of polyps to validate the findings and enhance the diagnostic capabilities of the expert reader. There exists a similar potential in coronary CTA as well, although the only study that evaluated this aspect [25] has not shown any significant benefit. The automated system may also work as a quality assurance tool providing measurable end points in trials.
In summary, there are few scenarios, where the automated CTA algorithm can be employed either as a ‘first reader’ to be followed with an expert manual read or as a ‘second reader’ to enhance the report of an expert reader.
Literature Review
Several studies have been performed on the utility of the automated coronary CTA in various settings (Table 1). Most of these studies have been performed on COR Analyzer software [26•, 27–37] and 1 study by Kelm et al [21] on the Siemens algorithm.
Arnoldi et al correlated the results of automated coronary CTA system with quantitative coronary angiography (QCA) in 59 patients who presented to outpatient cardiology department with atypical chest pain or stress studies (Fig. 3). The algorithm was found to have a sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for predicting stenosis >50 % of 74 %, 83 %, 46 %, and 94 %, respectively, on a per vessel basis and 100 %, 65 %, 58 %, and 100 %, respectively, on a per patient basis. False positive results were seen in 33 patients at a rate of 0.56 per patient, 19 of which were associated with stenosis < 50 % (Fig. 4) and 14 were associated with no stenosis in QCA. False positives were found in studies with motion/stairstep artifacts [3] (Fig. 5) or high image noise (1 case) and in some cases the cause remained unexplained (10 cases). They concluded that the high NPV makes it valuable as a second reader to enhance the confidence in excluding coronary artery stenosis. The false positive rate was also relatively low compared with other modalities. On a per patient basis, there is high performance for diagnosing CAD. On a per vessel basis there is high sensitivity for RCA (70 %) and LAD (94 %), while low sensitivities were found for LM (33 %) and LCX (43 %), which is probably related to low prevalence of CAD in this group (just 3 in LM and 7 in LCX) [22]. Thus the technique is more suitable for excluding CAD in a low to intermediate prevalence population rather than a high prevalence population. This is in line with the current consensus that coronary CTA is appropriate only in low-to-intermediate risk population and not in a high risk group. A limitation of this study is that the CTA was performed on patients who were referred for cardiac catheterization, which will be a high risk population. However, it could be extrapolated that the test will perform better in a low risk population group [22].
Use of Cor A algorithm in a 46-year-old man with atypical chest pain. (A) Following automatic segmentation, labeling, and centerline extraction of the coronary arterial tree, the software places red marks on areas of suspected significant stenosis. Curved multiplanar reconstructed image of LAD shows the areas of significant stenosis, denoted by red arrows. (B) Left anterior oblique view of coronary catheterization study of the same patient shows areas of significant stenosis in the proximal and mid LAD (black arrows). The stenosis in the mid segment (white arrow) is minimal (10 %). With kind permission from Springer Science+Business Media: Arnoldi E, Gebregziabher M, Schoepf JU, et al. Automated computer-aided stenosis detection at coronary CT angiography: initial experience: Fig. 1. European Radiology 2010;2:1160–1167
Curved MPR image of LAD in a 74-year-old man with atypical chest pain shows 2 calcified atherosclerotic plaques. The automated algorithm marked 2 areas as having significant stenosis (red arrows). (B) However cardiac catheterization (right anterior oblique view) did not show any significant stenosis. In this case, software likely overestimated the severity of stenosis due to blooming from calcified plaques. With kind permission from Springer Science+Business Media: Arnoldi E, Gebregziabher M, Schoepf JU, et al. Automated computer-aided stenosis detection at coronary CT angiography: initial experience: Fig. 3. European Radiology 2010;2:1160–1167
False positive interpretation. Curved MPR image of the right coronary artery in a 47-year-old man with exertional chest pain shows red arrows placed in an area, which the software interpreted as an abnormal area. Review of this region shows significant stair-step artifact in the RCA as the cause of this red marker and no significant stenosis was identified in this location on cardiac catheterization (not shown here). With kind permission from Springer Science+Business Media: Arnoldi E, Gebregziabher M, Schoepf JU, et al. Automated computer-aided stenosis detection at coronary CT angiography: initial experience: Fig. 5. European Radiology 2010;2:1160–1167
Halpern et al correlated the results of COR Analyzer interpretation with human expert interpretation for stenosis >50 % in a population of 207 patients. Unlike the study by Alridch et al this study evaluated first order coronary artery branches as well. COR Analyzer had sensitivity, specificity, PPV, and NPV of 92 %, 70 %, 48 %, and 97 %, respectively, on a per patient basis. False positive results were seen in 20 of patients (23 stenoses). This was due to either calcified vessel, blurred vessel, misidentified vessel (misclassification of non-vascular or extracardiac structure as vessel), coronary stents, or myocardial bridges. False negative results were due to small vessels (<1.5 mm), left dominant coronary system with small RCA (<1.5 mm), vessel misidentification and stenosis close to 50 %, failure to include branches, and no obvious explanation. COR Analyzer agreed with the expert interpretation in 75 %. However, this study is limited by absence of correlation with coronary catheterization [23].
Kang et al evaluated the potential of this software in evaluating ED patients presenting with acute chest. This retrospective study correlated the patients with <50 % stenosis in automated coronary CTA with formal radiology report in a group of 398 patients who presented to ED with acute chest pain. Eighteen patients were excluded due to failure of image transmission or insufficient number of image slices. Of the 380 eligible patients, CAD had sensitivity, specificity, PPV, and NPV of 94 %, 63 %, 76 %, and 89 % on a per patient basis. The NPV increased to 93 % after exclusion of 37 cases interpreted as invalid by auto CAD algorithm. The NPV further increased to 97 % after excluding the 75 % of false negative cases that were eventually showed to have non-significant CAD by using coronary angiography. The causes of false negative studies were; high calcium, stent, or previous CABG. False positive studies were associated with severe calcification [15], previous PTCA [8], CABG [4], small RCA [3], calcified plaque [16], myocardial bridge [13], or anomalous RCA origin [9]. Anomalous RCA resulted in failure to correctly track the RCA, which was interpreted as abnormal. The kappa value between auto CAD and radiology report was 0.58. The study also showed that it took 180 ± 30 minutes from the time of acquisition to provide a formal radiology report, while the algorithm provided report in 11 ± 5 minutes after acquisition. This study proved the potential for auto CAD to be used in emergency setting. In addition, it has potential to reduce intra and inter-observer variability and make it more reproducible. However the limitations of this study are that it is retrospective and not all the results were compared with coronary angiography [26•].
Goldenberg et al evaluated the use of CAD as a CAST (Computer aided simple triage) to exclude the presence of coronary artery disease in patients presenting in ED with chest pain. The aim of CAST is to provide a prompt automatic interpretation or wet read indicating presence or absence of the disease. They summarized the results from 14 independent trials, 3 of which have been described above. The other results are summarized in the Table 1. In general, it can be seen that the automated CTA has high NPV and sensitivity (90 %–95 %), while specificity was lower (40 %–70 %). The specificity was particularly lower in those studies where the disease prevalence was high, such as in cardiology outpatients. In this group, mild disease was present in those patients who had negative CAD, which was interpreted as positive by the system, resulting in false positive studies and hence decreased specificity. The system will call a study as negative if there is no disease at all, particularly in the ED population, where the prevalence is less than 20 %, as a result of which the specificity is high, up to 60 %–70 % in this population. The system also performed better with higher quality studies. Higher false positive results were seen in prospective gating due to misregistration artifact, noisy low dose scans, or patients with high heart rate. It can be inferred that the patient selection, patient preparation, scanning parameters, and staff experience all play an important role in the performance of the system. There is an average of 0.72 false positives per study after analysis of all coronary arteries (8 vessels on average) and looking for all types of plaques [20••]. In comparison , the study performed by Kelm et al using the other algorithm had 2.97 false positives per study, while just analyzing 3 major coronary arteries and looking only for noncalcified lesions. If it is assumed that the prevalence is same in both studies and the ratio is the same for both studies between false positives per negative study and per positive study, the average number of false positives per negative study is 0.48 in this study, compared with 2.18 in Kelm et al [20••, 21].
Sansoni et al followed 209 patients who had automated coronary CTA interpreted for a period of 12.8 ± 7 months and found that no adverse events happened in those 78 patients who were reported negative by the system, thus indicating a 100 % NPV. In the 131 positive patients, 40 major adverse events were reported in 28 patients [38].
Anders et al in their recent study, confirmed that the automated technique (COR Analyzer) has high sensitivity, and NPV [25] in the detection of significant coronary artery stenosis (>50 %). In addition, they sought to find out if the automated reading increases the diagnostic accuracy of manual interpretation in the detection of CAD. In 100 patients, with a CAD prevalence of 40 %, they correlated the presence of significant stenosis (>50 %) between manual approach (2 independent readers), automated approach, and expert interpretation aware of automated findings with invasive angiography. Reader 1 read the odd cases and then reviewed the findings after results of COR analyzer were available. Reader 1 valuated the even studies after initial evaluation by COR Analyzer. Reader 2 then read the odd studies, with software first, and even studies, manual interpretation first, blinded to reader 1 [25].
The sensitivity, specificity, PPV, and NPV of automated reading was 89 %, 79 %, 74 %, and 92 %, respectively, on a per patient basis and 82 %, 85 %, 48 %, and 96 % respectively on a per vessel basis. However, the automated segmentation failed in 10 % of patients and 12 % of vessels. This was either due to motion artifacts, insufficient contrast, segmental occlusions or pronounced calcification, or unexplained. This implies the need for additional manual processing in these patients. False negative results were due to tracing of segmental or side branches instead of main vessels in case of ostial occlusions. With expert reading, 100 % of studies were evaluable and sensitivity, specificity, PPV, and NPV of 95 %, 95 %, 93 %, and 97 % was found on a per patient basis and 89 %, 98 %, 88 %, and 98 %, respectively, on a per vessel basis. Knowing the results of the automated approach did not improve the performance of expert readers. With manual reading following automatic reading, sensitivity, specificity, PPV, and NPV were 95 %, 98 %, 98 %, and 97 %, which is comparable with manual interpretation alone. With the expert as the second reader, sensitivity, specificity, PPV, and NPV were 95 %, 95 %, 93 %, and 97 % respectively, which did not improve the initial diagnosis by manual interpretation alone. On a per patient basis, automated detection of stenosis had inferior accuracy compared with manual interpretation, and had little impact on expert readers, either if applied first or second. The 16 (12 false positive, 4 false negative) misdiagnosed patients by automated analysis alone could be reduced to 5 (3 false positive, 2 false negative) by adding the expert read. The limitations of this study are the retrospective nature and a higher prevalence of CAD than typical in this population. Hence, the rate of false negatives in this study might overestimate the false negative rate in a standard clinical setting. However, this study stresses the importance of manual reading, due to the high rate of segmentation failure and false negative rate [25].
Kelm et al evaluated the other available Siemens automated coronary CTA algorithm. In a study of 229 coronary CTAs [21] performed on a variety of scanners, this algorithm was shown to have a sensitivity, specificity and NPV by-vessel of 97 %, 67 %, and 100 %, respectively, and sensitivity of 95 % and false positive of 2.97 % by lesion. The high sensitivity and negative predictive values make it valuable as a second reader, comparable with the CorA system. The authors claim that the total processing time is 1 minute for centerline processing after which 1.8 to 3.9 seconds is required compared with 10 minutes for Rcadia system [21]. The faster time is due to the lumen regression, which is much faster and accurate than lumen segmentation, which takes 21 seconds. The centerline verification system enables the system to cope with tracing errors and low quality vessels.
Challenges and Limitations
With an average specificity of 60 % in the above studies and an estimated prevalence of CAD of 15 % in these studies, at least 51 % of typical patients undergoing coronary CTA will be reported as negative, implying that half of the patients could be discharged or observed safely based on an automated analysis alone. With an NPV of 99 %, only 1 % of patients are expected to be misdiagnosed. However, it should be understood that this automated system is ideal only for a low to intermediate risk population and is not appropriate for use in a high risk population. Final interpretation should be provided by an expert reader, whether it is negative or positive on an automated system. One should also be aware that segmentation fails in some patients. For example, there was a 10 % failure rate in the study published by Anders et al [25], 8 % in Halpern et al [23], and 5 % in Arnoldi et al [22]. Implementing this algorithm in routine practice, particularly in the emergency setting will require adequate training of all the personnel involved, particularly the staff of the emergency department. Workflow should be established after consensus among all the personnel involved on how to manage the patients who are utilizing this algorithm. The cost of implementing this strategy is not insubstantial and lack of reimbursement is a potential obstacle. Prospective multicenter trials need to be performed to evaluate the outcomes of patients who had their initial evaluation performed by an automated coronary CTA system.
Conclusions
Automated coronary artery interpretation and reporting have been shown to provide high sensitivity and negative predictive values in the evaluation of significant coronary arterial stenosis compared with invasive coronary angiography and expert readers. It has high potential as an initial reader to triage patients who present with acute chest pain in the ED and rule out coronary artery disease in patients with low to intermediate probability of coronary artery disease. The limitations of this technique should be understood, particularly the failure of segmentation. Final interpretation by an expert cardiac imager is mandatory in all these studies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Meijboom WB, Meijs MF, Shuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography; a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–44.
Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi slice computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49:863–71.
Blankstein R, Ahmed W, Bambert F, et al. Comparison of exercise treadmill testing with cardiac computed tomography angiography among patients presenting to the emergency room with chest pain: the Rule out Myocardial Infarction Using Computer-Assisted Tomography (ROMICAT) study. Circ Cardiovasc Imaging. 2012;5:233–42.
Schlett CL, Banerji D, Siegel E, et al. Prognostic value of CT angiography for major adverse cardiac events in patients with acute chest pain from the emergency department: 2-year outcomes of the ROMICAT trial. JACC Cardiovasc Imaging. 2011;4:481–9.
Dey D, Schepis T, Marwan M, et al. Automatic 3-dimensional quantification of non-calcified coronary plaque from coronary CT angiography: comparison with intravascular. US Radiol. 2010;257:516–22.
Cline HE, Krishnan K, Napel S, et al. Automated coronary CT angiography plaque-lumen segmentation. Proc SPIE Med Imaging. 2009;7269:726003–10.
Boogers MJ et al. Automated quantification of stenosis severity on 64-slice CT: a comparison with quantitative coronary angiography. JACC Cardiovac Imaging. 2010;3:699–709.
Cordeiro MA, Largo AC, Brito MS, et al. CT angiography in highly calcified arteries: 2D manual vs modified automated 3D approach to identify coronary stenosis. Int J Cardiovasc Imaging. 2006;22:507–16.
Khan MF, Wesarg S, Gurung J, et al. Facilitating coronary artery evaluation in MDCT using a 3D automatic vessel segmentation tool. Eur Radiol. 2006;16:1789–95.
Yang G, Kitslaar P, Frenay M, et al. Automatic centerline extraction of coronary arteries in coronary computed tomographic angiography. Int J Cardiovasc Imaging. 2012;28:921–33.
Bouraoui B, Ronse C, Baruthio J, et al. Fully automatic 3D segmentation of coronary arteries based on mathematic morphology. In: IEEE International Symposium Biomedical Imaging: from nano to macro (ISBI). 2008. 1059–62.
Zambal S, Hladuvka J, Kanitsar A, et al. Shape and appearance models for automatic coronary artery tracking. The Midas Journal; 2008 MICCAI workshop Grand Challenge Coronary Artery tracking. 2008. http://hdl.handle.net/10380/1430. Accessed 1 Feb 2013.
Tek H, Gulsun M, Laguitton S, et al. Automatic coronary tree modeling. The Midas Journal; 2008 MICCAI workshop Grand Challenge Coronary Artery tracking. 2008. http://hdl.handle.net/10380/14326. Accessed 1 Feb 2013.
Wang C, Smedby O. An automatic seeing method for coronary artery segmentation and skeletonization in CTA. The Midas Journal; 2008 MICCAI workshop Grand Challenge Coronary Artery tracking. 2008. http://hdl.handle.net/10380/1434. Accessed 1 Feb 2013.
Bauer C, Bischof H. Edge based tube detection for coronary artery centerline extraction. The Midas Journal; 2008 MICCAI workshop Grand Challenge Coronary Artery tracking. 2008. http://hdl.handle.net/10380/1403. Accessed 1 Feb 2013.
Xu C, Prince JL. Snakes, shapes and gradient vector flow. IEEE Trans Image Process. 1998;7:359–69.
Frangi AF, Niessen WJ, Vincken KL, et al. Multiscale vessel enhancement filtering. In: Proceedings of Medical Image Computer Assisted Intervention (MICCAI). Lecture notes in computer science. 1998;1496:130–7.
Kitslaar PH, Frenay M, Oost E, et al. The Midas Journal; 2008 MICCAI workshop Grand Challenge Coronary Artery tracking. 2008. http://hdl.handle.net/10380/1460. Accessed 1 Feb 2013.
Schaap M, Metz C, et al. Standardized evaluation methodology and reference database for evaluating coronary artery centerline extraction algorithms. Med Image Anal. 2009;13:701–14.
•• Goldenberg R, Eilot D, Begelman G, et al. Computer-Aided Simple Triage (CAST) for coronary CT angiography. Int J Comput Assist Radiol Surg. 2012;7:819–27. Good summary on various studies performed using CorA algorithm.
Kelm BM, Mittal S, Zheng Y, et al. Detection, grading, and classification of coronary stenosis in computed tomography angiography. Med Image Comput Comput Assist Interv. 2011;14(Pt 3):25–32.
Arnoldi E, Gebregziabher M, Schoepf JU, et al. Automated computer-aided stenosis detection at coronary CT angiography: initial experience. Eur Radiol. 2010;2:1160–7.
Halpern EJ, Halpern DJ. Diagnosis of coronary stenosis with CT angiography comparison of automated computer diagnosis with expert readings. Acad Radiol. 2011;18:324–33.
Begelman G, Goldenberg R, Levanon S, et al. Creating a blood vessel tree from imaging data. US Patent. 2011;7:893,459.
Anders K, Achenbach S, Petit I, et al. Accuracy of automated software-guided detection of significant coronary artery stenosis by CT angiography: comparison with invasive catheterization. Eur Radiol. 2012; doi:10.1007/s00330-012-2717-6.
• Kang KW, Chang HJ, Shim H, et al. Feasibility of an automatic computer-assisted algorithm for the detection of significant coronary artery disease in patients presenting with acute chest pain. Eur J Radiol. 2012;81:3640–6. Good study on the feasibility of automated algorithms in the emergency setting.
Weisman J, Yuz M. Fully automated coronary CTA analysis. Proceedings of the 8th SCCT meeting. Orlando, USA. July 2008.
Lopez CT, Weissman G, Joshi S, et al. Automatic computerized evaluation of 64 multislice coronary CTA. A comparison between COR Analyzer II software and visual evaluation. Proceedings of the 8th SCCT meeting. Orlando, USA. July 2008.
Poon M. The role of computed aided diagnosis in the management of acute chest pain. Proceedings of the 8th SCCT meeting. Orlando, USA. July 2008.
Malhotra V. COR Analyzer diagnostic performance analysis. Proceedings of the 9th SCCT meeting. Orlando, USA. July 2009.
Tyagi G, et al. Segmental accuracy of an automated analyzer of coronary CT angiography (CCTA) in ED patients: (Initial experience). Proceedings of the RSNA Meeting. Chicago, USA. Dec 2009.
Daubert M, Malhotra V, Ferrao S, et al. Computed aided analysis of 64-slice coronary computed tomography angiography: a comparison with manual interpretation. Proceedings of the 10th SCCT meeting. Las Vegas, USA. July 2010.
Malhotra V, Poon M, Krishnan U, et al. Computed aided detection for coronary CT angiography in low to intermediate risk population. Proceedings of the 10th SCCT meeting. Las Vegas, USA. July 2010.
Mehta C, et al. Validation of automated cardiac CT angiography analysis system: initial experience at an academic center. Proceedings of the 10th SCCT meeting. Las Vegas, USA. July 2010.
Henzler T, Meyer M, Apfaltrer P, et al. Computer-aided stenosis detection on coronary CT angiography in chest pain patients with an intermediate pre-test likelihood for acute coronary syndrome. Proceedings of the ECR Annual Meeting. Vienna, Austria. March 2012.
Tyagi G. Accuracy of an automated coronary CTA analyzer in ED patients. Proceedings of the ASER, 2009, Orlando, USA. Oct 2009.
Zhang S, et al. Automated diagnosis of stenosis on coronary CT angiography. Presented at ARRS, 2009, Boston, USA. Apr 2009.
Sansoni E, Schoepf U, Nance J, et al. Computer aided detection of coronary artery disease. CT based triage of acute chest pain patients: validation by patient outcome. Presented at RSNA, 2010. Chicago, USA. 2010.
Conflict of Interest
Prabhakar Rajiah declares no conflict of interest. Paul Schoenhagen declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajiah, P., Schoenhagen, P. Automated Interpretation and Reporting of Coronary CT Coronary Angiography. Curr Cardiovasc Imaging Rep 6, 282–291 (2013). https://doi.org/10.1007/s12410-013-9201-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12410-013-9201-9