Abstract
Objective
To evaluate the performance of a computer-aided algorithm for automated stenosis detection at coronary CT angiography (cCTA).
Methods
We investigated 59 patients (38 men, mean age 58 ± 12 years) who underwent cCTA and quantitative coronary angiography (QCA). All cCTA data sets were analyzed using a software algorithm for automated, without human interaction, detection of coronary artery stenosis. The performance of the algorithm for detection of stenosis of 50% or more was compared with QCA.
Results
QCA revealed a total of 38 stenoses of 50% or more of which the algorithm correctly identified 28 (74%). Overall, the automated detection algorithm had 74%/100% sensitivity, 83%/65% specificity, 46%/58% positive predictive value, and 94%/100% negative predictive value for diagnosing stenosis of 50% or more on per-vessel/per-patient analysis, respectively. There were 33 false positive detection marks (average 0.56/patient), of which 19 were associated with stenotic lesions of less than 50% on QCA and 14 were not associated with an atherosclerotic surrogate.
Conclusion
Compared with QCA, the automated detection algorithm evaluated has relatively high accuracy for diagnosing significant coronary artery stenosis at cCTA. If used as a second reader, the high negative predictive value may further enhance the confidence of excluding significant stenosis based on a normal or near-normal cCTA study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Successful interpretation of coronary CT angiography (cCTA) requires considerable experience [1] as there are various challenges and pitfalls, which may result in missed detection of significant stenosis or overestimation of non-obstructive lesions as significant [2–4]. Therefore, for interpreters at the beginning of their learning curve, an automated system with constant performance for coronary artery stenosis detection appears desirable.
Automated computer-aided detection and diagnosis algorithms have been developed for and applied to a multitude of disease states within and outside of medical imaging [5–9]. However, descriptions of the application of such systems to coronary artery disease are scarce [10–12], which stands in contrast to the socioeconomic importance of this disease. Specifically computer-aided detection of coronary artery stenosis at cCTA to our knowledge has not been previously described in the clinical literature. We evaluated the performance of a computer-aided algorithm for automated, without human interaction, detection of significant stenosis at cCTA, using quantitative coronary angiography (QCA) as the reference standard.
Materials and methods
Study population
The study protocol was approved by our institutional human research committee, and all patients gave written informed consent. The study population consisted of 59 consecutive patients without known coronary artery disease who were referred to our cardiology service for coronary catheter angiography because of symptomatic chest pain or prior abnormal nuclear myocardial perfusion study. Patients in unstable clinical condition, previous revascularization, serum creatinine above 2.0 mg/dl, or known allergy to iodinated contrast material were not eligible for the study.
cCTA image acquisition
On the morning before their coronary catheter angiography all patients underwent cCTA using 64-slice CT (Somatom Sensation™, Siemens, Forchheim, Germany) in 30/59 patients and dual-source CT (Somatom Definition™, Siemens) in 29 patients. Standard parameters were used. Briefly, 64-slice cCTA studies comprised 64 × 0.6 mm collimation, pitch 0.2, 120-kV tube voltage, and 700-mAs tube current. Dual-source CT used 2 × 32 × 0.6 mm collimation, pitch 0.2–0.43, 120-kV tube voltage, and 560-mAs tube current. Contrast enhancement was achieved with 60–80 ml of a non-ionic contrast medium (Isovue; 370 mg I/ml iopamidol; Bracco, Princeton, NJ) injected at 5–6 ml/s, followed by a 50 ml saline chaser bolus using a dual-syringe injector (Stellant D, Medrad, Pittsburgh, PA). Image reconstruction was performed during the RR interval with the least cardiac motion using a medium soft-tissue convolution kernel (B25f) and a section thickness of 0.75 mm with an increment of 0.3 mm.
cCTA analysis
cCTA data were processed using an automated computer-aided coronary artery stenosis detection algorithm (COR Analyzer™, Rcadia, Haifa, Israel). Without human interaction, this algorithm analyzed the four major coronary arteries—left main (LM), left anterior descending (LAD), left circumflex (LCx), and right coronary artery (RCA)—for the presence and location of significant (50% or more) coronary artery stenosis. For visualization of results, the computer algorithm deploys detection marks indicating candidate lesions on an automatically generated curved multiplanar reformation along the centerline of the target vessel. The algorithm also deploys warning marks indicating potential processing failure, which were treated as positive detection marks for the statistical analysis.
Computer-aided detection algorithm
Coronary tree segmentation
The processing starts from the detection of the ascending aorta, which is identified by its typical circular cross-sectional shape within the mediastinum. The aorta is segmented based on the relatively distinct edges of the contrast medium filled aorta within the surrounding anatomy. The algorithm proceeds with the localization of the coronary artery ostia as contrast medium filled structures connected to the aorta. To build the coronary tree tubular components are tracked. The resulting coronary artery tree is then pruned of erroneously connected structures, e.g., coronary veins and pulmonary vessels.
Coronary artery identification
Identifying major vessels is important for validating the robustness of the segmentation (i.e., absence of an artery may indicate incomplete segmentation) and for assigning lesions to a specific artery. Identification of the three major coronary arteries uses a probabilistic anatomical model based on several hundred cCTA studies that had been used to train the algorithm. This model allows computation of the likelihood of a given path to be RCA, LM, LAD, or LCX which is then validated using features such as the spatial relationships between the arteries; e.g., RCA and LCX should reside in the same atrio-ventricular plane.
Stenosis detection
The reconstructed coronary artery tree is split into disjoint vessel segments and analysis is performed for each segment separately. External boundaries and the lumen of the artery are delineated using an iterative model-based variation approach. Calcified lesions are detected and segmented. Non-calcified plaque is detected as a hypo-attenuating area between the external vessel boundary and lumen without calcium. A set of parameters is extracted for every cross section of the vessel segment including vessel and lumen cross-sectional area, presence and size of atherosclerotic plaque, bifurcations, noise level, presence, and extent of artifacts (e.g., motion, misregistration), and distance from the ostium. The algorithm then matches the extracted features to the characteristics of lesions that were used to train the algorithm and deploys a detection mark if the features of the lesion are likely to indicate significant stenosis.
Quantitative catheter angiography (QCA)
QCA was performed using conventional Judkins’ technique with at least four views of the left and two views of the right coronary artery. Studies were interpreted for stenosis by consensus of two experienced cardiologists who performed quantitative assessment of stenosis severity using a grading tool with automated distance and scale calibration (Axiom-Artis, Siemens).
Statistical analysis
All analyses and graphs were performed with statistical software (SAS/STAT software, version 9.2; SAS Institute, Cary, NC). Categorical variables were presented as percentages, and continuous variables were presented as means and ranges. Detection marks deployed by the automated algorithm indicating significant stenosis at cCTA were compared with findings at QCA on a per-vessel and per-patient basis using logistic regression.
Results
Patient demographics
The population consisted of 64% (38/59) male patients with a mean age of 58 ± 12 years and an average body weight of 83 ± 28 kg.
Per-vessel analysis
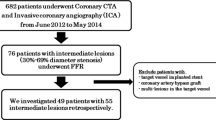
The data sets of all 59 patients were successfully processed by the automated algorithm. Warning marks indicating potential processing failure were deployed on 12 vessel segments, which were treated in the same manner as positive detection marks during data analysis. In the 59 patients, coronary catheter angiography revealed 3 patients with significant (50% or more) stenosis in the LM, 18 with significant LAD stenosis, 7 with significant LCx stenosis, and 10 patients with significant RCA stenosis. The automated algorithm correctly identified 1/3 patients (33%) with LM stenosis, 17/18 (94%) with stenosis in the LAD, 3/7 (43%) with stenosis in the LCx, and 7/10 (70%) with stenosis in the RCA (Fig. 1). Detailed performance indices of the automated detection algorithm are provided in Table 1.
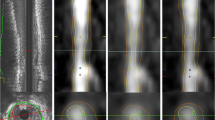
Contrast-enhanced 64-slice cCTA study in a 46-year-old man with atypical chest pain. a 3D coronary artery tree segmentation result generated by the automated algorithm. Red detection marks indicating significant stenosis are deployed in the LAD and LCx. b Left Curved multiplanar reformation of the LAD generated by the algorithm. Detection marks (red arrows) indicating significant stenosis in the proximal and mid vessel were automatically deployed. Right Coronary catheterization (left anterior oblique [LAO] view) confirms stenosis of 50% or more in proximal LAD and mid LAD (black arrows). The more proximal lesion (white arrow) in mid LAD is non-significant (30%) on QCA
Per-patient analysis
Based on QCA, 19/59 patients had significant coronary artery stenosis of 50% or more (Fig. 2), whereas in 40 patients stenosis of 50% or more was excluded (Fig. 2). The automated algorithm correctly identified 19/19 patients with significant stenosis in any vessel (Fig. 1), and correctly excluded significant stenosis in 26/40 patients (Fig. 2). Thus, on a per-patient basis, the automated algorithm had 100% sensitivity, 65% specificity, 76% accuracy, 100% NPV, and 58% PPV compared with QCA (Table 1).
Left Contrast-enhanced dual-source cCTA study in a 67-year-old man with substernal chest pressure. The algorithm’s analysis results displayed as curved multiplanar reformations indicate absence of significant stenosis in LM/LAD (a), LCx (b), and RCA (c). Right Coronary catheterization [a and b right anterior oblique [RAO] view; c LAO view] confirms patency of all four vessels
False positive analysis
In the 59 patients a total of 33 false positive detection marks were deployed by the automated algorithm resulting in an average of 0.56 per patient. Of 33 false positive detection marks, 19 (58%) were associated with stenotic atherosclerotic lesions that did not exceed the 50% or more threshold on QCA (Fig. 3); and 14 did not have an atherosclerotic surrogate. These 14 false positive detection marks were associated with high overall image noise (n = 1) (Fig. 4), stair-step artefacts from ECG-misregistration and patient-related motion (n = 3) (Fig. 5), or had no obvious explanation (n = 10). On a per-patient basis, the automated algorithm falsely identified a total of 14/59 subjects (24%) as positive for significant stenosis of 50% or more. Accounting for the 19 detection marks that were deployed on stenotic lesions of less than 50% and considering only the detection marks that were not associated with an atherosclerotic surrogate as false positives, the number of false-positive patient studies was reduced to 5 (9%).
Left Contrast-enhanced dual-source cCTA study in a 74-year-old man with atypical chest pain. The algorithm deployed two detection marks (red arrows) indicating significant stenosis on eccentric calcified plaques with associated blooming artefact on curved multiplanar reformats of the LAD. Right Coronary catheterization (RAO view). The lesions indicated by the algorithm did not exceed the 50% or more threshold on QCA
Left Contrast-enhanced 64-slice cCTA study in a 49-year-old man with a body mass index of 38 kg/m2 and prior abnormal nuclear myocardial perfusion study. Image quality is limited by high image noise. The algorithm deployed a detection mark (red arrow) indicating significant stenosis on the distal RCA displayed as curved multiplanar reformations. Right Coronary catheterization (LAO view) shows patency of the vessel
Left Contrast-enhanced 64-slice cCTA study in a 47-year-old man with exertional chest pain. The algorithm deployed a detection mark (red arrow) indicating significant stenosis on a stair-step artefact in the mid RCA displayed as curved multiplanar reformations. Right Coronary catheterization (LAO view) shows patency of the vessel
Discussion
Automated computer-aided detection and diagnosis has been introduced for various diagnostic applications and use of such systems is increasingly gaining importance in clinical practice [5–9]. Considering that coronary artery disease is the most important socioeconomic healthcare problem in the westernized world, the application of such techniques to this disease state is surprisingly rare. Our literature search identified an early attempt using computer-aided systems to detect stenosis at coronary catheterization [10]. Computer-aided image analysis, detection, and risk quantification have been applied to CT coronary artery calcium scoring [11] and the use of advanced visualization techniques has been shown to improve cCTA-based diagnosis of coronary artery disease [12]. However, to our knowledge ours is the first description in the peer-reviewed clinical literature of automated computer-aided coronary artery stenosis detection at cCTA.
Relative to early algorithmic stages and even commercial releases of computer-aided detection applications for other pathologies [13–17] the performance of the algorithm evaluated here is comparatively high: particularly, the high NPV, in the range of 91–97% per vessel and 100% per patient, appears promising. Similarly, the comparatively low rate of false-positive detection marks sets this algorithm apart from computer-aided detection applications in other organ systems, which have traditionally struggled to find the right balance between high sensitivity and low false-positive rates [14, 15, 17]. Furthermore, we found relatively high performance for diagnosing significant coronary artery stenosis on a per-patient level. However, per-vessel sensitivities showed considerable variation, with lower values than typically observed with human interpretation [18]. Lowest sensitivities were found for the LM (33%) and the LCx (43%) compared with relatively high values for the RCA (70%) and the LAD (94%). The low sensitivity for the evaluation of LM and LCx disease may be explained by the low prevalence (3 in LM, 7 in LCx) of significant lesions in these vessels and thus may not adequately reflect the performance of the algorithm. The deposition of detection marks on non-obstructive lesions of less than 50% combined with frank false-positive findings resulted in low PPVs of 20–30% for all major vessels except for the LAD (81%). This performance reflects the results of comparison studies between cCTA and coronary catheterization based on human interpretation that almost uniformly demonstrate lower specificity and PPV value than sensitivity and NPV [18].
Considering these findings, the algorithm in its current state appears more suitable for aiding the exclusion of significant coronary artery stenosis in patient populations with low likelihood and prevalence of disease, rather than establishing a diagnosis of significant coronary artery stenosis in populations with high likelihood and prevalence of obstructive lesions. As such the performance characteristics of the algorithm align with the current recommendations for the appropriate use of cCTA [19] which consider performance of cCTA in high likelihood patients not indicated. Prospective use of such automated algorithms may further enhance the confidence of excluding significant coronary artery stenosis based on a normal or near-normal cCTA study in low and intermediate likelihood patients, which is considered appropriate use [19]. In actual clinical practice such algorithms may aid inexperienced readers to gradually acquire confidence for ruling out significant stenosis, particularly in patients with low likelihood of disease. Using the algorithm as a second reader, the interpreter may find reassuring verification of her/his exclusion of significant stenosis based on a normal or near-normal cCTA study. This may be particularly helpful in on-call situations where relatively inexperienced trainees are increasingly called upon to rule out significant coronary artery stenosis in patients with acute chest pain [20–22], using CT.
The sole use of QCA, while eliminating human interaction, to evaluate the performance of the computer-aided detection algorithm is a strength of our study, but also incurs limitations. QCA, although not perfect, is ordinarily considered a stronger reference standard compared with subjective visual interpretation of coronary catheter angiograms because of its greater objectivity and quantitative nature and naturally is a more relevant comparison than human interpretation of cCTA data. However, because we studied patients who were clinically referred for coronary catheterization, our findings are subject to the same biases as previous comparison studies and cannot easily be extrapolated to the low or intermediate likelihood patient population who ordinarily undergoes cCTA in clinical practice. According to the above considerations, however, the performance of the algorithm would likely be better. More importantly, the effect on the eventual performance of human interpreters if this algorithm is used as a second reader was beyond the scope of this initial technical evaluation and will have to be evaluated by future investigations along with the exact role of such algorithms in clinical practice. Further refinements of the algorithm along with more precise delineation of the coronary arteries by ongoing improvements in CT technology [23, 24] can be expected to enhance the robustness and clinical utility of automated stenosis detection.
Conclusion
Despite these limitations we believe that we could successfully demonstrate the relatively high accuracy of computer-aided detection for diagnosing significant stenosis at cCTA compared with QCA. Thus, our preliminary findings may indicate a promising future role of such algorithms for enhancing the confidence of human interpreters for excluding significant stenosis based on a normal or near-normal cCTA study.
References
Pugliese F, Hunink MG, Gruszczynska K et al (2009) Learning curve for coronary CT angiography: what constitutes sufficient training? Radiology 251:359–368
Choi HS, Choi BW, Choe KO et al (2004) Pitfalls, artifacts, and remedies in multi-detector row CT coronary angiography. Radiographics 24:787–800
Hoe JW, Toh KH (2007) A practical guide to reading CT coronary angiograms—how to avoid mistakes when assessing for coronary stenoses. Int J Cardiovasc Imaging 23:617–633
Nakanishi T, Kayashima Y, Inoue R, Sumii K, Gomyo Y (2005) Pitfalls in 16-detector row CT of the coronary arteries. Radiographics 25:425–438
Wormanns D, Fiebich M, Saidi M, Diederich S, Heindel W (2002) Automatic detection of pulmonary nodules at spiral CT: clinical application of a computer-aided diagnosis system. Eur Radiol 12:1052–1057
de Vries AH, Jensch S, Liedenbaum MH et al (2007) Does a computer-aided detection algorithm in a second read paradigm enhance the performance of experienced computed tomography colonography readers in a population of increased risk? Eur Radiol 19:941–950
Das M, Muhlenbruch G, Helm A et al (2008) Computer-aided detection of pulmonary embolism: influence on radiologists’ detection performance with respect to vessel segments. Eur Radiol 18:1350–1355
Tanaka T, Nitta N, Ohta S et al (2009) Evaluation of computer-aided detection of lesions in mammograms obtained with a digital phase-contrast mammography system. Eur Radiol. doi:10.1007/s00330-009-1505-4
Koss LG, Sherman ME, Cohen MB et al (1997) Significant reduction in the rate of false-negative cervical smears with neural network-based technology (PAPNET Testing System). Hum Pathol 28:1196–1203
Sugahara T, Yamagihara Y, Sugimoto N, Kimura K, Awano K, Azumi T (1992) Computer-aided interpretation of coronary cineangiograms. Accuracy of automatic detection of stenotic lesions. Acta Radiol 33:6–9
Isgum I, Rutten A, Prokop M, van Ginneken B (2007) Detection of coronary calcifications from computed tomography scans for automated risk assessment of coronary artery disease. Med Phys 34:1450–1461
Reimann AJ, Tsiflikas I, Brodoefel H et al (2009) Efficacy of computer aided analysis in detection of significant coronary artery stenosis in cardiac using dual source computed tomography. Int J Cardiovasc Imaging 25:195–203
Das M, Muhlenbruch G, Mahnken AH et al (2006) Small pulmonary nodules: effect of two computer-aided detection systems on radiologist performance. Radiology 241:564–571
Schoepf UJ, Schneider AC, Das M, Wood SA, Cheema JI, Costello P (2007) Pulmonary embolism: computer-aided detection at multidetector row spiral computed tomography. J Thorac Imaging 22:319–323
Zhou C, Chan HP, Patel S et al (2005) Preliminary investigation of computer-aided detection of pulmonary embolism in three-dimensional computed tomography pulmonary angiography images. Acad Radiol 12:782–792
Summers RM, Johnson CD, Pusanik LM, Malley JD, Youssef AM, Reed JE (2001) Automated polyp detection at CT colonography: feasibility assessment in a human population. Radiology 219:51–59
Taylor SA, Iinuma G, Saito Y, Zhang J, Halligan S (2008) CT colonography: computer-aided detection of morphologically flat T1 colonic carcinoma. Eur Radiol 18:1666–1673
Hamon M, Morello R, Riddell JW (2007) Coronary arteries: diagnostic performance of 16-versus 64-section spiral CT compared with invasive coronary angiography—meta-analysis. Radiology 245:720–731
Hendel RC, Patel MR, Kramer CM et al (2006) ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 48:1475–1497
Hoffmann U, Nagurney JT, Moselewski F et al (2006) Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation 114:2251–2260
Hoffmann U, Bamberg F, Chae CU et al (2009) Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 53:1642–1650
Sato Y, Matsumoto N, Ichikawa M, Kunimasa T et al (2005) Efficacy of multislice computed tomography for the detection of acute coronary syndrome in the emergency department. Circ J 69:1047–1051
Arnoldi E, Johnson TR, Rist C et al (2009) Adequate image quality with reduced radiation dose in prospectively triggered coronary CTA compared with retrospective techniques. Eur Radiol. doi:10.1007/s00330-009-1411-9
Achenbach S, Marwan M, Schepis T et al (2009) High-pitch spiral acquisition: a new scan mode for coronary CT angiography. J Cardiovasc Comput Tomogr 3:117–121
Conflict of Interest
UJS is a medical consultant for and receives research support from Bayer-Schering, Bracco, General Electric, Medrad, and Siemens. RG is an employee of Rcadia Medical Imaging Ltd. PLZ receives research support from Boehringer-Ingelheim, Bristol Myers Squib, Bracco, and Siemens. PC is a medical consultant for Bracco and receives research support from Siemens.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arnoldi, E., Gebregziabher, M., Schoepf, U.J. et al. Automated computer-aided stenosis detection at coronary CT angiography: initial experience. Eur Radiol 20, 1160–1167 (2010). https://doi.org/10.1007/s00330-009-1644-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1644-7