Abstract
Objectives
To assess the prognostic value of positron emission tomography (PET) imaging in patients undergoing evaluation for known or suspected cardiac sarcoidosis (CS) while not on active immunotherapy.
Background
Previous studies have attempted to identify the value of PET imaging to aid in risk stratification of patients with CS, however, most cohorts have included patients currently on immunosuppression, which may confound scan results by suppressing positive findings.
Methods
We retrospectively analyzed 197 patients not on immunosuppression who underwent 18F-fluorodeoxyglucose (FDG) PET scans for evaluation of known or suspected CS. The primary endpoint of the study was time to ventricular arrhythmia (VT/VF), or death. Candidate predictors were identified by univariable Cox proportional hazards regression. Independent predictors were identified by performing multivariable Cox regression with stepwise forward selection.
Results
Median follow-up time was 531 [IQR 309, 748] days. 41 patients met the primary endpoint. After stepwise forward selection, left ventricular ejection fraction (LVEF) (HR 0.98, 95% CI 0.96-0.99, P = 0.02), history of VT/VF (HR 4.19, 95% CI 2.15-8.17, P < 0.001), and summed rest score (SRS) (HR 1.06, 95% CI 1.02-1.12, P = 0.01) were predictive of the primary endpoint. Quantitative and qualitative measures of FDG uptake on PET were not predictive of clinical events.
Conclusions
Among untreated patients who underwent PET scans to evaluate known or suspected CS, LVEF, history of VT/VF, and SRS were associated with adverse clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a disease entity characterized by the formation of noncaseating granulomas that can involve multiple organ systems. The most common organ involved is the lung while overt cardiac manifestations are relatively uncommon.1 However, cardiac sarcoidosis is likely under recognized as autopsy series have shown that 16% to 68% of patients with systemic sarcoidosis also have cardiac involvement on histology, depending on ethnicity and region.2,3,4 The prevalence of cardiac sarcoidosis is also rising.5 This is likely due to improved diagnostic imaging, including the use of positron emission tomography (PET) scans to visualize areas of cardiac inflammation and scarring. Patients with cardiac sarcoidosis can present with a broad spectrum of clinical manifestations, ranging from electrocardiographic changes without symptoms, to complete heart block and malignant ventricular arrhythmias with sudden cardiac death.6 With increased recognition of CS in clinical practice, the use of PET to evaluate for signs of inflammation is expanding.
The prognosis of patients with cardiac sarcoidosis is generally not well understood. From an imaging perspective, prior studies have shown that 18F-fluorodeoxyglucose (FDG) uptake (representing active myocardial inflammation) and perfusion defects (representing scar or fibrosis) on PET sarcoid scans are predictors of adverse events independent of ejection fraction.7,8 However, these previous studies have included patients on active immunosuppression, potentially affecting the degree of inflammation seen on PET and thus its prognostic implications.
Better understanding the prognosis of patients with cardiac sarcoidosis may help guide therapy by driving initiation, intensity, and duration of immunosuppression as well as decisions to place implantable cardiac defibrillators (ICD). We sought to explore how clinical characteristics and PET imaging findings are associated with future adverse cardiovascular events in patients not on immunosuppression who underwent PET imaging for the evaluation of known or suspected cardiac sarcoidosis.
Methods
Study Population
We performed a retrospective cohort study on consecutive patients who underwent PET sarcoid scans for evaluation of possible or known cardiac sarcoidosis from June 6, 2015 to June 29, 2018 at the University of Michigan Hospital (Ann Arbor, MI, USA). Studies were identified through screening all cardiac FDG PET scans that were protocolled to assess for sarcoidosis within that time frame. Both rest/stress and rest only perfusion scans were included. Patients on immunosuppressive therapy at the time of the scan and those with a history of coronary artery disease (CAD) were excluded. Additionally, patients with scans considered non-diagnostic due to suspected or confirmed dietary non-compliance were excluded. This study was approved by the Institutional Review Board at the University of Michigan, and waiver of informed consent was granted for this retrospective analysis.
Population Characteristics
Baseline characteristics including pertinent past medical history, results of prior imaging studies, and demographic data were obtained by thorough review of the electronic medical records across multiple health systems. These were recorded from the time of the scan. Advanced heart block was defined as second degree type 2 or third-degree heart block. Left ventricular ejection fraction (LVEF) was recorded from the rest perfusion potion of the PET sarcoid study. Patients were classified by the Japanese Ministry of Health and Welfare (JMHW) criteria which is commonly used for the diagnosis of cardiac sarcoidosis.9 Patients were also classified for cardiac sarcoidosis by the Heart Rhythm Society (HRS) criteria10. If patients had subsequent biopsies (extra cardiac or endomyocardial) as a result of FDG PET scans, the findings were recorded.
PET Patient Preparation and Imaging Acquisition
All patients who underwent cardiac PET/computed tomography (PET/CT) studies at the University of Michigan received a standardized protocol. These methods have been described previously.11 Briefly, patients were instructed to maintain a 36-hour low carbohydrate, high fat, protein permitted diet. After an overnight fast, patients were given a high fat shake on the morning of the FDG rest scan. After at least 3 hours, patients were injected with an average of 8 to 10 mCi of FDG. A total of 30IU/kg of unfractionated heparin was given to each patient, divided into three boluses.
Approximately 1 hour after FDG injection, patients underwent PET/CT imaging, acquired using a whole-body PET/CT scanner (Siemens Biograph mCT, Knoxville, TN). Rest myocardial perfusion images were obtained using rubidium-82. FDG images were acquired for 15 minutes in list mode using 3D ordered subset expectation maximization (3D-OSEM) according to the manufacturer’s recommended protocol. Both attenuated and non-attenuated images were obtained.
Image Analysis
Images were analyzed using Corridor4DM (INVIA Medical Imaging Solutions, Ann Arbor, MI) by board certified nuclear cardiologists. Using the fused CT attenuation corrected FDG images, a 1 cm diameter, circular, 2-dimensional region of interest (ROI) was drawn on fused FDG PET/CT images to measure the mean blood pool standardized uptake value (SUVmean) in the ascending aorta at the level of the pulmonary artery, excluding the vessel wall. The max standardized uptake value (SUVmax) for the myocardium was measured using a circular 2-dimensional ROI drawn in the mid-septal wall and mid lateral wall, avoiding areas of FDG spillover or abnormal FDG uptake. Summed rest scores were calculated as the sum of individual segmental scores on the respective images. SUVindex (SUVmax/SUVmean) was calculated for all patients to standardize the degree of FDG uptake seen in the myocardium to the mean blood pool SUV. Semiquantitative 17-segment visual interpretation of the gated myocardial perfusion images was performed using a standard 5-point scoring system.12 Patients were deemed to have FDG/perfusion mismatch if the PET scan reports specifically mentioned FDG uptake in areas with perfusion defects or if there was overlap in the individually listed myocardial segments. As an additional way to assess predictive value of PET findings, scans were also categorized into three groups described in prior literature:7 normal perfusion and normal metabolism, abnormal perfusion or abnormal metabolism, and abnormal perfusion and metabolism.
Outcomes Analysis
The primary outcome was a composite endpoint including time to first episode of ventricular tachycardia, ventricular fibrillation (VT/VF), or death. VT/VF was defined as sustained ventricular arrhythmia, or a ventricular arrhythmia requiring cardioversion, defibrillation, or anti-tachycardia pacing. These outcomes were adjudicated through detailed review of the electronic medical record including outpatient clinic notes, admission history and physicals, discharge summaries, telephone notes, and device interrogations.
In patients with evidence of FDG uptake on PET imaging, additional data was collected for further analysis, including treatment with high dose immunosuppression (defined as ≥ 30mg of prednisone or use of steroid sparing agent). In those who began immunosuppression as a result of their first scan, data from their follow up PET sarcoid scans (if performed) were collected in the same manner as described above.
Statistical Analyses
Variables of interest were described as median [25th percentile, 75th percentile] and percentages for continuous and categorical variables, respectively. Baseline characteristics were compared between those who did and did not meet the primary endpoint using Mann–Whitney U tests for continuous variables. Pearson’s chi squared analysis were used to compare categorical variables of interest. In patients that were started on high dose immunosuppression and had subsequent PET sarcoid scans, continuous variables of interest were compared using Wilcoxon Signed Rank Test. All statistical tests were two-sided with a 0.05 significance level. Possible predictors for the primary outcome were explored using univariable Cox regression. Multivariable Cox regression was performed using candidate predictors identified in the univariable analysis (P ≤ 0.1). Stepwise regression with a forward selection (P value ≤ 0.05 for inclusion) was performed to identify independent predictors of our primary endpoint. Harrell’s Concordance index was calculated to assess the final model discrimination. We performed additional analysis of the same character on the subgroup of patients who met criteria for CS by HRS as a result of positive PET scans and downstream cardiac/extra cardiac biopsies.
Results
A total of 316 patients were screened for inclusion. After exclusion for coronary disease (N = 25), active treatment with immunosuppression (N = 86), and concern for non-diagnostic scans (N = 8), a total of 197 patients were included in the final analysis (Figure 1). Characteristics and comparisons between those who did and did not meet the primary endpoint can be seen in Table 1. Median age was 58.0 [48.0, 66.0] years, and a majority (58.9%) of the patients were male. The cohort was 76.6% Caucasian, 22.3% African American, and 1% other. Indication for PET scans included VT (22), high grade heart block (24), reduced EF (50), or a combination of these (46), and other (55, including EKG abnormalities, NSVT, imaging findings on MRI etc). Median follow up time was 531 [309, 748] days. The primary endpoint was achieved in 41 (20.8%) patients, including 38 patients with ventricular arrhythmias and 3 deaths. There were 19 patients who met JMHW criteria for cardiac sarcoidosis. 40 patients met criteria for cardiac sarcoidosis using HRS criteria. Some patients underwent additional biopsies after PET imaging. In total, three patients were found to have positive endomyocardial biopsies for cardiac sarcoidosis and five patients were found to have positive extracardiac biopsies. Together with positive PET findings and biopsy results, a total of 52 (26.4%) patients met criteria for cardiac sarcoidosis by HRS criteria (3 definite, 49 probable).
The results of the PET imaging are shown in Table 2. There were 84 total patients (42.6%) with positive FDG uptake, 4 of whom had focal on extensive/diffuse uptake. Of those with RV uptake, 3 had extensive or diffuse rather than focal (N = 14) FDG uptake. The median SRS from perfusion imaging was 1.0 [0.0, 5.0] in the group which did not meet the primary endpoint vs. 4.0 [1.0, 9.5] in the event group (P < 0.001). Combining myocardial perfusion defect and FDG uptake into a 3-category model as described previously7 was not significantly different between the two groups (P = 0.122), nor was tissue FDG SUVindex (P = 0.228) or the presence of myocardial FDG uptake as a categorical variable (P = 0.372). Additionally, the presence of FDG/perfusion mismatch (N = 60) was found to not be significantly different between the two groups (P = 0.34).
Results of the univariable and multivariable analyses are shown in Table 3. Significant univariable associations included LVEF (P < 0.001), history of VT/VF (P < 0.001), and SRS (P < 0.001). Other candidate predictors identified included the presence of atrial FDG uptake (P = 0.068) and right ventricular (RV) FDG uptake (P = 0.061). In multivariable modeling with stepwise forward selection, the following variables remained significant: LVEF (hazard ratio [HR] 0.98, 95% CI 0.96-0.99, P = 0.022), history of VT/VF (HR 4.19, 95% CI 2.15-8.17, P < 0.001), and SRS (HR 1.06, 95% CI 1.02-1.12, P = 0.01). Based on these hazard ratios, an LVEF drop of 10% and an SRS increase of 3-4 points would be approximately associated with a 20% increased risk of meeting the primary endpoint. Harrell’s Concordance index of the final model composed of the three significant predictors was 0.795.
Results of the univariable and multivariable analyses on patients who ultimately met HRS criteria after PET scan are shown in Table 4. After stepwise forward selection, the only variable that remained a significant predictor for our primary outcome was summed rest score (HR 1.082, 95% CI 1.02-1.147, P = 0.009).
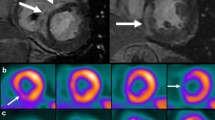
From the cohort of 197 patients, 84 (42.6%) of them had positive FDG uptake. Of these, 39 (46.4%) were treated with immunosuppression within six months of the scan, as compared to 4 (3.5%) of the 113 patients who did not have FDG uptake (P < 0.001). Most were treated with prednisone and a steroid sparing agent. Three patients were treated with more than one steroid sparing agent. The most commonly used steroid sparing agent was mycophenolate mofetil (72.4%). Other agents used included: methotrexate (20.5%), tacrolimus (2.6%), azathioprine (2.6%), and adalimumab (2.6%). Twenty-four patients underwent repeat scans to evaluate treatment response (Figure 2). Median time between scans was 214 [189-260] days. After treatment, SUVindex decreased from a median of 1.70 [1.32, 3.53] to 1.13 [1.02, 1.59] (P = 0.001). Figure 3 further illustrates these findings. Median LVEF before and after treatment were similar (42.0% [29.75, 57.5] to 44.5% [36.25, 54.5], P = 0.080) as were median SRS (7.5 [3.0, 7.5] to 6.5 [2.5, 11.75], P = 0.568).
Visualization of changes in SUVindex (peak myocardial SUV uptake divided by mean blood pool SUV) before and after treatment with immunosuppression. Black lines represent patients with decreased SUVindex on follow-up scans. Gray lines represent patients with increased SUVindex on follow up scans. Values reported as median [25th percentile, 75th percentile]
For those with normal PET scans, final diagnosis included: heart failure with preserved EF (7), idiopathic heart block (6), premature ventricular contractions or related cardiomyopathy (9), non-ischemic cardiomyopathy (19), idiopathic VT (4), quiescent CS (10), no significant cardiac disease (12), and other (6, including hypertrophic cardiomyopathy, mitral valve prolapse, and pericarditis.)
Discussion
To our knowledge, this is the largest cohort of patients who underwent PET scans for known or suspected cardiac sarcoid that have been studied in this fashion. In this retrospective analysis of patients not on immunosuppression undergoing PET sarcoid scans, we found that decreased LVEF, history of VT/VF, and SRS were significant predictors for a composite endpoint of time to VT/VF and death. FDG uptake on PET sarcoid scans (assessed as a continuous variable through SUVindex and a categorical variable) was not a significant predictor of our primary endpoint.
Comparison to Prior Literature
Previous studies have proposed various models for predicting adverse outcomes in patients with cardiac sarcoidosis, including a three-category model based on the presence of FDG uptake and perfusion defects on PET imaging.7,8 In our univariable analysis, this three-category model was not significantly associated with our primary endpoint. In our cohort, neither qualitative nor quantitative measurements of FDG uptake (SUVindex) were predictive, which may have influenced the prognostic value of this model.
There are multiple reasons that could explain these discrepant findings. First, our study excluded patients on immunosuppression at the time of scan, whereas other studies included these patients. This may have led to the significantly lower proportion of patients who met either the JMHW or HRS criteria for CS in our study, as this would lead to exclusion of many patients with known extra cardiac sarcoidosis or known CS. It is likely that our cohort represents a lower risk, more treatment naïve population identified earlier in the disease process compared to cohorts evaluated in prior literature. Additionally, differences in dietary preparation can lead to the incomplete myocardial suppression of FDG uptake and therefore affect the prognostic value of the scan. The patients studied in our cohort underwent a strict dietary preparation, as described in our methods, which has been shown to be highly effective.11 The results could also be confounded by dietary non-compliance as this has been shown to be independently associated with adverse cardiovascular outcomes in those undergoing nuclear stress testing.13 Lastly, there is a possibility that our discrepant findings are due to type II error. This is less likely, given the relatively large cohort and the fact that both LVEF and history of VT were strong predictors as expected.
PET Imaging Variables
As mentioned above, FDG uptake was not found to be predictive of our primary endpoint. It is believed that active inflammation demonstrated by increased FDG uptake and high SUVindex may be a marker of disease reversibility and responsiveness to immunosuppressive therapy. With this, increased inflammation may portend a more benign clinical course while presence of scar would point towards a more fulminant disease process that would be less responsive to immunotherapy. Large studies have shown that FDG uptake has been predictive of adverse cardiovascular outcomes.7,8 As mentioned previously, the difference between these studies and ours may be due to the exclusion of patients on immunosuppression at the time of scan. Ongoing inflammation while on immunotherapy could represent a more treatment resistant disease process which could portend a worse prognosis.
Prior studies have shown that patients treated with prednisone or other immunosuppressive therapy have a decrease in FDG uptake on repeat PET scans.14,15 Improving FDG uptake on serial PET scans has been shown to correlate with clinical improvement and has been used to guide treatment.16,17,18,19 The results of our analysis are congruent with these findings. In the subgroup of patients that underwent follow up PET scans after initiation of immunosuppression, SUVindex significantly decreased. This likely represents improved inflammation, and with this, there was a small but statistically insignificant improvement in LVEF. Furthermore, in our cohort, patients who had evidence of FDG uptake on their PET scans were more likely to be aggressively treated and started on high dose immunosuppression. In a study of 20 patients diagnosed with cardiac sarcoidosis with atrioventricular block and normal LVEF, patients not treated with steroids had worsening LV function, less improvement in their conduction disease and more VT on follow-up compared to those who had early initiation of steroids.20
High SRS was found to be predictive of our primary outcome, independent of both LVEF and history of VT/VF. Furthermore, in the subgroup who ultimately met criteria for CS by HRS, SRS was the only predictor for our primary outcome in the multivariable analysis. In patients with cardiac sarcoidosis and no history of CAD, scarring or fibrosis of the myocardium (represented by a high SRS) may represent previously active disease which has since resulted in permanent myocardial damage. Patients that have more scar have had a more severe disease course and would be more likely to have subsequent adverse cardiovascular events. Malignant ventricular arrhythmias as a result of scar or fibrosis has been previously described as a possible re-entrant circuit in scarred myocardium in patients with cardiac sarcoidosis.21,22,23 Additionally, late gadolinium enhancement on cardiac MRI, a surrogate for replacement myocardial fibrosis, has been shown to be a strong predictor for incident ventricular arrhythmias.24 However, Sperry et al showed that SRS from PET sarcoid scans by itself was not predictive of a composite endpoint including all cause mortality, heart transplantation or ventricular arrhythmia in patients with suspicion for cardiac sarcoidosis after adjusting for key clinical variables. This could be due to a difference in patient population, the fact that a significant proportion of their population were on immunosuppression at the time of their scan, and that their final models were robustly adjusted.8
In the early stages of cardiac sarcoidosis, it has been hypothesized that rest perfusion defects could also be the result of compression of the myocardial microvasculature in areas of active inflammation as opposed to scarring or fibrosis.25 Accordingly, a prior study involving cardiac sarcoidosis patients showed a significant improvement in rest perfusion defects seen on thallium-201 myocardial scans with the administration of dipyridamole, a potent vasodilator.26 Theoretically, aggressive treatment with immunotherapy could decrease inflammation and improve microvasculature compression leading to an improvement in SRS on subsequent scans. However, in our subgroup of patients started on high dose immunosuppression followed by subsequent PET scans, SRS did not decrease significantly even as inflammation improved. This would suggest that the perfusion defects seen on imaging are more consistent with scarring rather than a consequence of potentially reversible inflammation.
Clinical Predictors
Both decreased LVEF and history of prior VT/VF were significantly associated with our primary endpoint. This is consistent with what is known in non-sarcoid cardiomyopathy, as depressed ejection fraction and a prior history of sustained ventricular arrhythmia are strong risk factors for future ventricular tachyarrhythmias.27,28,29 In patients with cardiac sarcoidosis, multiple studies have demonstrated that decreased LVEF is associated with increased mortality.5,19,30 Like non-sarcoid cardiomyopathy, current AHA/ACC/HRS guidelines recommend implantation of ICDs in patients with cardiac sarcoidosis when LVEF is less than 35%.31 However, patients with cardiac sarcoidosis are thought to have an especially high risk for sudden cardiac death as a significant proportion of these patients initially present with ventricular arrhythmias. 5,32 As such, current guidelines also recommend implantation of an ICD in patients with EF greater than 35% with high risk features including syncope, need for a pacemaker, presence of scar on either MRI or PET, or inducible ventricular arrhythmias on electrophysiological study.31 Our study population is similarly high risk in that approximately 21% experienced VT/VF or death over a median follow up period of only 1.7 years.
Non-Left Ventricular Myocardial FDG Uptake
The presence of RV FDG uptake on PET imaging has been previously found to be a predictor of adverse cardiovascular events in patients with known or suspected cardiac sarcoidosis.7,33 In our analysis, although there was a tendency towards worse outcomes with the presence of RV FDG uptake in the univariable analysis, it was not a predictor after adjustment for LVEF, history of VT/VF, and SRS. Interestingly, the presence of atrial FDG uptake was found to be a candidate predictor in the univariable analysis (P = 0.068). After stepwise forward selection that included LVEF, history of VT/VF, and SRS, presence of atrial FDG uptake continued to show a tendency towards being a significant predictor for our primary outcome (P = 0.056), even with only 15 patients exhibiting atrial uptake. A recent study has shown an association between atrial FDG uptake and presence of atrial arrhythmias,34 but to our knowledge no studies have shown a relationship between atrial FDG uptake and VT/VF and death.
Limitations
There are several limitations to this study. First, although our study included patients referred from outside hospital systems, it is still a single center retrospective analysis. In addition, both the proportion of patients who met JMHW criteria for sarcoidosis (10%), and the incidence of primary outcomes (20.8%) was lower in our study than in similar prior studies.7,8 Though the proportion of patients CS criteria as a result of positive PET scans and/or subsequent biopsies did increase (26.4%), this likely indicates that our patient population was lower risk as a whole and/or there may be a lower threshold to order PET imaging at our institution in select patients. The fact that patients on immunosuppression were excluded in our analysis also supports this hypothesis. This may also indicate that some patients had FDG uptake from unclear etiologies. Thus, our conclusions may not be readily generalizable to patients with known sarcoidosis who are already on immunosuppression (who were excluded from the cohort), or for those with biopsy-proven extra cardiac sarcoidosis as only 32.5% of patients fit this demographic. Lastly, the most intense areas of FDG uptake are occasionally not accounted for in the polar maps (i.e. papillary muscles, basal parts of the ventricle); and there may be variabilities between readers for SUV measurements.
Conclusion
Among patients not on immunosuppression who underwent PET cardiac sarcoid scans to evaluate known or suspected cardiac sarcoidosis, decreased ejection fraction, history of VT/VF, and summed rest score were significantly and independently associated with our composite primary endpoint of time to VT/VF and death. FDG uptake was not found to be predictive of the endpoint. Patients who were found to have FDG uptake were more likely to be started on immunotherapy which led to significantly decreased FDG uptake on subsequent follow up scans. Identifying higher risk patients in this population may help guide prognosis discussions as well as treatment intensity.
New knowledge gained: for patients with confirmed or suspected cardiac sarcoidosis undergoing FDG, PET imaging, history of ventricular arrhythmia, reduced LVEF, and high are associated with poor prognosis rather than FDG uptake.
References
Baughman RP, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 2001;164(10 Pt 1):1885-9.
Iwai K, et al. Pathological studies on sarcoidosis autopsy. I. Epidemiological features of 320 cases in Japan. Acta Pathol Jpn 1993;43(7-8):372-6.
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation 1978;58(6):1204-11.
Iwai K, et al. Racial difference in cardiac sarcoidosis incidence observed at autopsy. Sarcoidosis 1994;11(1):26-31.
Kandolin R, et al. Cardiac sarcoidosis: epidemiology, characteristics, and outcome over 25 years in a nationwide study. Circulation 2015;131(7):624-32.
Birnie DH, et al. Cardiac sarcoidosis. J Am Coll Cardiol 2016;68(4):411-21.
Blankstein R, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol 2014;63(4):329-36.
Sperry BW, et al. Prognostic impact of extent, severity, and heterogeneity of abnormalities on (18)F-FDG PET scans for suspected cardiac sarcoidosis. JACC Cardiovasc Imaging 2018;11(2 Pt 2):336-45.
Hiraga H, Yuwai K, Hiroe M. Diagnostic standard and guidelines for sarcoidosis. Jpn J Sarcoidosis Granulomatous Disord 2007;27:89-102.
Birnie DH, et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart Rhythm 2014;11(7):1305-23.
Larson SR, et al. Characterization of a highly effective preparation for suppression of myocardial glucose utilization. J Nucl Cardiol 2019;27:849.
Cerqueira MD, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105(4):539-42.
Banko LT, et al. Incidence of caffeine in serum of patients undergoing dipyridamole myocardial perfusion stress test by an intensive versus routine caffeine history screening. Am J Cardiol 2010;105(10):1474-9.
Osborne MT, et al. Reduction in (1)(8)F-fluorodeoxyglucose uptake on serial cardiac positron emission tomography is associated with improved left ventricular ejection fraction in patients with cardiac sarcoidosis. J Nucl Cardiol 2014;21(1):166-74.
Rosenthal DG, et al. Long-term corticosteroid-sparing immunosuppression for cardiac sarcoidosis. J Am Heart Assoc 2019;8(18):e010952.
Ahmadian A, et al. The response of FDG uptake to immunosuppressive treatment on FDG PET/CT imaging for cardiac sarcoidosis. J Nucl Cardiol 2017;24(2):413-24.
Lee PI, Cheng G, Alavi A. The role of serial FDG PET for assessing therapeutic response in patients with cardiac sarcoidosis. J Nucl Cardiol 2017;24(1):19-28.
Ning N, et al. Serial cardiac FDG-PET for the diagnosis and therapeutic guidance of patients with cardiac sarcoidosis. J Card Fail 2019;25(4):307-11.
Chiu CZ, et al. Prevention of left ventricular remodeling by long-term corticosteroid therapy in patients with cardiac sarcoidosis. Am J Cardiol 2005;95(1):143-6.
Nagai T, et al. Effect of corticosteroid therapy on long-term clinical outcome and left ventricular function in patients with cardiac sarcoidosis. Circ J 2015;79(7):1593-600.
Winters SL, et al. Sustained ventricular tachycardia associated with sarcoidosis: assessment of the underlying cardiac anatomy and the prospective utility of programmed ventricular stimulation, drug therapy and an implantable antitachycardia device. J Am Coll Cardiol 1991;18(4):937-43.
Koplan BA, et al. Refractory ventricular tachycardia secondary to cardiac sarcoid: electrophysiologic characteristics, mapping, and ablation. Heart Rhythm 2006;3(8):924-9.
Furushima H, et al. Ventricular tachyarrhythmia associated with cardiac sarcoidosis: its mechanisms and outcome. Clin Cardiol 2004;27(4):217-22.
Disertori M, et al. Myocardial fibrosis assessment by LGE is a powerful predictor of ventricular tachyarrhythmias in ischemic and nonischemic LV dysfunction: a meta-analysis. JACC Cardiovasc Imaging 2016;9(9):1046-55.
Blankstein R, Waller AH. Evaluation of known or suspected cardiac sarcoidosis. Circ Cardiovasc Imaging 2016;9(3):e000867.
Tellier P, et al. Reversibility by dipyridamole of thallium-201 myocardial scan defects in patients with sarcoidosis. Am J Med 1988;85(2):189-93.
Bardy GH, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005;352(3):225-37.
Moss AJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346(12):877-83.
Antiarrhythmics versus Implantable Defibrillators Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 1997;337(22):1576-83.
Yazaki Y, et al. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am J Cardiol 2001;88(9):1006-10.
Al-Khatib SM, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2018;138(13):e272-391.
Nery PB, et al. Prevalence of cardiac sarcoidosis in patients presenting with monomorphic ventricular tachycardia. Pacing Clin Electrophysiol 2014;37(3):364-74.
Tuominen H, et al. FDG-PET in possible cardiac sarcoidosis: right ventricular uptake and high total cardiac metabolic activity predict cardiovascular events. J Nucl Cardiol 2019;28:199.
Yodogawa K, et al. Prevalence of atrial FDG uptake and association with atrial arrhythmias in patients with cardiac sarcoidosis. Int J Cardiol 2020;313:55.
Disclosures
Vaiibhav N. Patel, Justin A. Pieper, David Kopin, Thomas Cascino, Keith Aaronson and Todd Koelling have no conflicts of interest to disclose. Alexis Poitrasson-Rivière is employed by INVIA. INVIA Medical Imaging Solutions did not provide direct support to this study. Venkatesh L. Murthy owns stock in General Electric, has a research grant from Siemens Medical Imaging, and receives non-monetary research support from INVIA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
V. L. Murthy is supported by 1R01HL136685 from the National, Heart, Lung, Blood Institute and 1RO1AG059729 from the National Institute on Aging.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patel, V.N., Pieper, J.A., Poitrasson-Rivière, A. et al. The prognostic value of positron emission tomography in the evaluation of suspected cardiac sarcoidosis. J. Nucl. Cardiol. 29, 2460–2470 (2022). https://doi.org/10.1007/s12350-021-02780-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-021-02780-x