Abstract
Background
Cardiac positron emission tomography (PET) using 18F-fluorodeoxyglucose (FDG) has been used to diagnose and monitor cardiac sarcoidosis (CS). It is not known whether a reduction in myocardial inflammation, as measured by FDG uptake, is associated with improvement in LV ejection fraction (EF).
Methods
For 23 patients with CS followed by a total of 90 serial PET exams (median 4 per patient), two physicians blinded to EF quantified the maximum of standardized uptake value (SUV) and volume of inflamed tissue above two distinct thresholds to assess the intensity and extent of FDG uptake on each study. Using gated 82Rubidium rest myocardial perfusion images, EF was measured blinded to all clinical and FDG data. To account for clustering and differences in scan frequency, a longitudinal mixed effects model was used to evaluate the relationship between FDG uptake and changes in EF on interval scans.
Results
Among 23 patients with serial PET exams (mean age 49, 74% male, mean baseline EF 43% ± 13%), the median time between the first and last scan was 2.0 years. Overall, 91% were treated with corticosteroids, 78% with ACE/ARB, 83% with beta-blockers, and 83% had ICDs. Longitudinal regression demonstrated a significant inverse linear relationship between maximum SUV and EF with an expected increase in EF of 7.9% per SUV reduction of 10 g·mL−1 (P = .008). Likewise, in an analysis based on volume, there was an increase in EF of 2.1% per 100 cm3 decrease in volume of inflamed tissue using a threshold of 2.7 g·mL−1 (P = .028) and an increase in EF of 3.8% per 100 cm3 decrease (P = .022) using a SUV threshold of 4.1 g·mL−1.
Conclusions
In a longitudinal cohort of CS patients, a reduction in the intensity and extent of myocardial inflammation on FDG PET is associated with improvement in EF. These data suggest serial PET scanning may help guide titration of immunosuppressive therapy to improve or prevent heart failure in CS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a multi-system disease of unknown etiology that is characterized by the formation of noncaseating granulomas in multiple organs.1 At least one-fourth of patients have cardiac sarcoidosis (CS),2 which portends a worse prognosis and accounts for most deaths from this disease. Among those with cardiac involvement, left ventricular ejection fraction (LVEF) and left ventricular diastolic diameter are important determinate of prognosis,3 and thus treatments that may improve these parameters are often used, particularly since in other forms of non-ischemic cardiomyopathy, therapies that improve LVEF and end-diastolic dimension have been linked to enhanced survival.4 Nevertheless, the mechanism of heart failure in CS, which may be either systolic or diastolic, is not well understood.
Limited observational data suggests that among some patients with CS, corticosteroids may improve LVEF5,6 or decrease the burden of ventricular arrhythmias, yet the benefits of corticosteroids have not been consistently demonstrated7 and there is no data regarding the optimal course of treatment. Although such therapies may be effective, long-term exposure to high-dose immune suppression has important side effects, is costly and would probably be most appropriate for patients with CS who are at highest risk of adverse events and disease progression. Yet, in patients with CS, it remains uncertain how best to monitor the treatment response to anti-inflammatory therapies.8
Advanced cardiac imaging modalities can provide important information about myocardial structure and function beyond LVEF and chamber size. In patients with CS, abnormal inflammation, as demonstrated by fluorodeoxyglucose (FDG) uptake on cardiac positron emission tomography (PET), has been associated with risk of death or ventricular tachycardia.9 The intensity of FDG uptake, as measured by the standardized uptake value (SUV), has been used to quantify active inflammation in CS.10 Studies have shown that SUV is often higher in the earlier stages of disease and that there is no overt relationship between SUV at presentation and LVEF.10 Other studies have suggested that FDG uptake may be reduced with steroid therapy.11 However, no studies to date have investigated the longitudinal relationship between FDG uptake and LVEF over serial FDG PET scans in CS. We hypothesized that those who experience reduction in inflammation following immunosuppressive therapy will have an improvement in their LVEF. Therefore, our aim was to evaluate CS patients who underwent serial PET examinations in order to identify whether reduction in the extent and intensity of inflammation are associated with any improvement in LVEF.
Methods
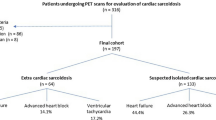
Study Population
The study population was selected from 125 consecutive patients referred for an initial cardiac PET exam at the Brigham and Women’s Hospital (Boston, MA) for the evaluation of known or suspected CS between May 2006 and January 2011. We included all patients with CS who had serial FDG PET scans performed for assessing response to therapy. Two patients with a diagnosis of CAD, defined as prior percutaneous coronary intervention or coronary stenosis >50%, were excluded. One patient was excluded on the basis that his follow-up FDG PET occurred after orthotopic heart transplant, and one patient with a negative baseline PET scan was excluded due to poor quality of the follow-up study. Consequently, a total of 23 patients with CS met criteria for inclusion and those patients had a total of 91 exams. One of the follow-up exams was excluded on the basis of poor quality due to diffuse and intense FDG uptake related to poor preparation. The study was approved by the Partners Healthcare Institutional Review Board and was conducted in accordance with institutional guidelines.
PET Perfusion/Metabolism Protocol
Patients were studied using a whole body PET-CT scanner (Discovery RX Light Speed 64, GE Healthcare, Milwaukee, WI). Non-gated CT imaging was used for attenuation correction. Resting myocardial perfusion was assessed after the intravenous administration of ~50 mCi of 82Rubidium. Following perfusion imaging, 10-12 mCi of 18F-FDG was injected intravenously. After approximately 90 minutes to allow for uptake, dedicated cardiac PET/CT images were performed in the same manner. Last, limited whole body FDG images were obtained from the base of the skull to the mid-thigh. Non-contrast helical CT imaging was performed over the same range without breath-hold for attenuation correction of PET images and for localization of FDG uptake. The average radiation exposure per study was ~15 mSv.
All patients were instructed to follow a high fat, high protein, low carbohydrate diet prior to a fast of at least 3 hours in order to shift normal myocardial metabolism to primary fatty acid utilization and, therefore, suppress the uptake of FDG by normal myocardium. Patients were instructed to avoid any sugar or sugar containing foods.
Image Analysis
Ascertainment of extent and intensity of FDG uptake on cardiac images
The SUV provides a measurement of FDG uptake intensity on cardiac PET. It takes into account the injection dose of FDG, body weight, and rate of decay. SUV is defined as the following and has the units g·mL−1:
Two physicians, blinded to LVEF data, determined the maximum SUV as well as volume of FDG for each scan using commercially available software (Hermes Hybrid Viewer Version 1.4, Hermes Medical Solutions, Stockholm, Sweden) using attenuation-corrected FDG images.
To calculate the volumes of FDG uptake, two separate thresholds were derived. Because quantification of SUV extent requires a threshold SUV measurement above which activity contributes to the measured volume, we used our population of prior PET studies referred for the evaluation of known or suspected CS (n = 125) to define threshold values based on findings in our patient population. The chosen thresholds were SUV values of 2.7 g·mL−1, which represented the smallest value for SUV maximum present among all patients who had focal FDG uptake at our institution, and 4.1 g·mL−1, which represented the minimum value for SUV maximum within the group of patients with known CS based on a positive endomyocardial biopsy.
Using the two thresholds, a volume of interest (VOI) was created which consisted of all myocardial SUV values that exceeded each of the above pre-specified thresholds. A seed tool was used to remove blood pool as necessary, and manual editing was used to exclude any FDG avid extracardiac structures.
Ascertainment of ejection fraction
An experienced cardiologist, who was blinded to all clinical data and to the FDG images as well as the sequence of PET scans (i.e., baseline vs follow-up), calculated LVEF from the rest-gated myocardial perfusion images using commercially available software (Corridor 4DM, INVIA, Ann Arbor, MI). As previously reported by our lab, the inter-observer variability in measurement of EF by 82Rubidium PET imaging is 5.5%.12
In six studies, the EF could not be determined due to gating abnormalities and/or inability to track the endocardium. Each of these patients had a cardiac MRI (n = 1) or echocardiogram (n = 5) within 30 days of the PET scan, and the calculated LVEF from these images was used instead of the PET LVEF. In a sensitivity analysis, removing these six scans did not alter any of the main findings presented in the below results.
Ascertainment of clinical data
Past medical histories including test results and medications were ascertained at the time of the study by review of the electronic medical records. Using all data, we applied the revised guidelines from 2006 for the diagnosis of CS from the Japanese Ministry of Health and Welfare (JMHW) in order to classify patients as JMHW positive or negative.13
Among the subset of patients who underwent endomyocardial biopsy, the findings on cardiac PET exam were compared to the biopsy results. Biopsy of the right ventricular septum was performed via the right internal jugular vein with a disposable bioptome with 4-5 specimens taken per patient. The specimens were fixed in 10% neutral-buffered formalin, processed and then embedded in paraffin. Step sections were taken through the paraffin block, producing three hematoxylin and eosin stained slides with 3-4 levels per slide. Biopsies containing non-necrotizing granulomas were deemed positive for sarcoidosis once other potential etiologies for granulomas were excluded. Polarized light examination was performed to rule out foreign material as a cause of granulomas, and methenamine silver (MSS) and acid-fast bacilli (AFB) stains were used to rule out infection.
All patients were evaluated for death from any cause or documented sustained ventricular tachyarrhythmias (VT). Vital status of all patients was ascertained from the Social Security Death Index. Outcomes were determined by comprehensive review of electronic medical records, defibrillator interrogations, mailed patient questionnaires, and scripted phone interviews. Follow-up was complete for all patients included in this study population.
Statistical Analysis
Patient demographics and baseline characteristics were summarized as mean ± standard deviation for continuous variables and frequencies for dichotomous and ordinal variables.
In order to account for clustering of individual patients and their multiple scans, a mixed effects model was used to evaluate the relationship between changes in SUV intensity and extent and changes in LVEF on serial PET exams. We used changes in maximum SUV, volume above an SUV value of 2.7 g·mL−1, and volume above an SUV value of 4.1 g·mL−1 as fixed effects independent variables with serial LVEF as the dependent outcome. Patient and scan number were treated as random effects.
A separate analysis was performed to determine if there was a difference in EF change based on a patient’s response to treatment during the study. Patients were labeled as responders if the net change in SUV maximum value decreased from baseline to the final PET exam. Conversely, patients were determined to be non-responders if their net SUV maximum increased or remained constant during the study. The median LVEF was determined for both responders and non-responders for the first four serial exams, since only a few patients had greater than four exams. These median values were plotted against scan number, and this plot was used to compare the change in median EF for responders as compared to that for non-responders. A two-tailed P value < .05 was considered to be significant in all analyses. All statistical analyses were performed using commercial software (STATA version 12.0, StataCorp LP, College Station, TX).
Results
Baseline Characteristics
Table 1 shows the complete baseline characteristics of the study population. Among 23 patients with serial PET exams, the median interval between repeat scans was 6.5 months and the median time between the first and last scan was 2.0 years. At baseline, the mean LVEF was 43% ± 13%. Of the 23 patients, 21 (91%) met the JMHW 2006 criteria for diagnosis of CS. The two patients who did not meet criteria were diagnosed by positive extracardiac biopsy and positive MRI in one and positive PET, positive MRI, and occurrence of VT in the other. A total of 9 patients (39%) had positive endomyocardial biopsies. Of the remaining patients, 10 (43%) had positive extracardiac biopsies and 4 (17%) were diagnosed clinically. Overall, 21 (91%) were treated with corticosteroids and 4 (17%) were treated with other immunosuppressive therapies. Both of those never treated with immunosuppression had stable inflammation and EF during the study, and both met the JMHW criteria. When examining medical therapies, 18 (78%) were treated with ACE/ARB, 19 (83%) with beta-blockers, and 8 (35%) with aldosterone inhibitors.
A total of 19 patients (83%) had implantable cardioverter-defibrillators (ICDs). Of these, 12 patients had devices placed prior to their initial scans. The baseline PET results demonstrated normal findings in 2 patients (9%), abnormal perfusion only in 3 patients (13%), abnormal FDG uptake only in 4 patients (17%), and abnormal perfusion and FDG uptake in 14 patients (61%). Those with normal scans both met Japanese Criteria and had positive biopsies (one cardiac and one extracardiac). Right ventricular uptake was noted in 9 (39%) patients.
The patients in this study had a mean of 3.9 PET scans per patient (standard deviation 1.7 scans) with a range of two to seven scans over the follow-up interval. A complete summary is shown in Table 2.
Relationship of Changes in SUV Measures to Change in LV Ejection Fraction
The distributions of the change in both LVEF and SUV maximum in this study are shown in Figure 1 (top left and top right, respectively).
Distribution of changes in ejection fraction and SUV maximum and volume between consecutive exams. Top left distribution of change in ejection fraction. Top right distribution of change in maximum SUV. Bottom left distribution of change in volume with SUV above 2.7 g·mL−1. Bottom right distribution of change in volume with SUV above 4.1 g·mL−1
Using a mixed effects model to examine the association between change in SUV maximum and change in EF, there was a significant inverse relationship with a P value of .008 (Figure 2, top). The model predicts a change of 7.9% in the EF in the opposite direction of a change by 10 g·mL−1 in SUV maximum.
Relationship of change in FDG uptake with change in LV ejection fraction. Top scatterplot of change in maximum SUV with change in LV ejection fraction shown with linear regression obtained via mixed effects modeling with 95% confidence interval (n = 67, P = .008). Bottom scatterplot of change in volume with an SUV above 4.1 g·mL−1 with change in LV ejection fraction shown with linear regression obtained via mixed effects modeling with 95% confidence interval (n = 67, P = .022)
The distributions of changes in SUV volume above thresholds of 2.7 and 4.1 g·mL−1 are shown in Figure 1 (bottom left and bottom right, respectively). A mixed effects model was used to construct a linear regression relating changes in SUV volume above a threshold of 2.7 g·mL−1 (Figure 5 in Appendix) and above a threshold of 4.1 g·mL−1 (Figure 2, bottom) to change in LVEF. The relationship in both of these models was similar as there was a significant inverse relationship with P values of .028 and .022, respectively. The model for volume change above 2.7 g·mL−1 predicts a change of 2.1% in EF in the opposite direction of a change in volume with SUV above 2.7 g·mL−1 of 100 cm3. The model for change in volume of myocardium with FDG uptake above 4.1 g·mL−1 predicts a change of 3.8% in EF in the opposite direction of a change in volume with SUV above 4.1 g·mL−1 of 100 cm3.
The results of one patient’s serial FDG PET exams are shown in Figure 3. This patient had a depressed EF, substantial inflammation, and reduced perfusion at baseline. All three measurements improved over the course of 25 months with corticosteroid treatment.
Serial FDG PET exams showing change in inflammation. The results of three serial studies over 25 months from a 46-year-old man with cardiac sarcoidosis treated with corticosteroids are shown. The color maps demonstrate the intensity of FDG uptake in a coronal view. The grayscale images demonstrate serial perfusion images using 82-rubidium (top) and metabolism images using FDG (bottom) in three distinct axes at approximately the same location. For each scan, the measurements of LV ejection fraction, SUV maximum, and SUV volumes are displayed
Change in Ejection Fraction for Responders and Non-responders
A comparison of the trends in mean LVEF (± standard error) for patients who responded to treatment and for patients who did not respond over serial imaging is shown in Figure 4. The figure demonstrates a significant difference between the two groups with a mean increase in LVEF of 8.6% ± 5.2% for responders vs a mean decrease in LVEF of −5.5% ± 3.4% for non-responders (P = .03). Similar results were found when this analysis was performed using median LVEF values for each group or when using fixed time intervals to define the four longitudinal groups instead of scan number. There was no significant difference in use of ACE/ARBs, beta-blockers, or aldosterone inhibitors between responders and non-responders.
Change in LV ejection fraction according to inflammation response. Line graph demonstrating a significant difference (P = .03) between the mean (± standard error) LV ejection fraction over serial exams, displayed as scan number, in those with (triangles) and without (circles) improvement in inflammation during the study. The numbers adjacent to the data points describe the number of patients contributing to the data at that point for each group
Association of Resting Perfusion Defects with Response to Therapy
The majority of the patients in our study (18 out of 23; 78%) had a resting perfusion defect and correspondingly the median summed rest score was 8 and the median number of segments with resting perfusion defects was 3. There was no difference in response to treatment between patients who had a normal versus abnormal resting perfusion defect (P = .10). When stratifying all patients based on the number of segments with resting perfusion defects on the initial scan, there was a trend for patients with more than 3 abnormal segments not to respond to therapy (P = .06).
Adverse Cardiovascular Events
Of the 23 patients, eleven (49%) experienced VT and two (9%) died during the period of observation. One patient experienced VT prior to death. Therefore, a total of 12 patients (52%) experienced an adverse event. Our study was underpowered to detect differences in adverse events between responders vs non-responders. However, it is noteworthy that, among the eleven patients who did not experience adverse events, five patients had no abnormal FDG uptake on their baseline PET scan. Of the remaining six patients with abnormal baseline FDG uptake, four had reduction in both SUV maximum and volume, one had an increase in FDG uptake and a reduction in LVEF during the study and another had stable FDG uptake during the study.
Discussion
This is the first study to examine the relationship between changes in inflammation and LVEF on serial FDG PET scans in patients with CS. Among 23 patients with known CS who were treated with immunosuppressive therapies guided by serial PET scans, we found that a reduction in both the intensity and extent of inflammation, as quantified by FDG uptake, is associated with an increase in LVEF.
Given that among patients with heart failure, an increase in LVEF is associated with improved prognosis,4 our findings suggest that anti-inflammatory therapy can improve (or in some patients prevent) the severity of heart failure and may improve prognosis. However, since not all patients with CS who are treated with corticosteroid therapy will have a reduction in FDG, it is not yet known whether non-responders should be transitioned to alternative immune suppression in order to maximize the potential for LVEF recovery.14 By the same token, our data reinforce the potential role for using FDG PET to guide down-titration of anti-inflammatory therapy among responders to minimize excessive exposure to potentially toxic therapy.
Our study is underpowered to detect differences in cardiovascular events by response to therapy, similar to other prior studies investigating the association of steroid therapy with outcomes.3 It is increasingly recognized that patients with CS have a high rate of adverse cardiac events,15,16 supported by the fact that half of the patients included in our study experienced death or VT. Therefore, patients with CS warrant consideration for aggressive therapies, in spite of the fact that there are currently no prospective studies to suggest that anti-inflammatory therapy results in any prognostic or symptomatic benefits.
We found a significant inverse relationship between changes in both the intensity (i.e. SUV maximum) and extent (i.e., SUV volume, regardless of selected threshold) of inflammation and changes in LVEF. However, it is noteworthy that the most significant relationship existed between changes in maximum SUV and LVEF. Since maximum SUV is easier to measure and does not rely on any threshold level of activity, our findings support the routine measurement and reporting of this value in patients referred for cardiac PET to assess the response to immunosuppressive therapy.
When examining per patient data, we also showed that patients who had a reduction in SUV maximum from the first to last scan had an improvement in their LVEF. This result supports the hypothesis that inflammation may result in systolic dysfunction and that LVEF may improve with reduction in inflammation. However, there are multiple confounders which may influence LVEF. While we did not detect any differences in use of ACEI/ARB or beta-blockers between responders and non-responders, it is possible that other unmeasured confounders exist.
Our study is not without limitations. Our population was relatively small and thus our results should be viewed as hypothesis generating at this time. A larger study, preferably multicenter, is needed to confirm our findings in order to better establish the relationship noted in this study. We used rest-gated images for measuring LVEF as these occurred on the same day as the PET FDG study; however, other techniques such as MRI or echocardiography may be preferable for serial assessment. Such methods may be especially useful among patients who have a large resting perfusion defect with absent counts, where PET could have limitations in edge detection. We did not measure glucose levels, and it is possible that increased glucose levels in patients treated with steroids could result in decreased FDG uptake.17 However, following a fast of 4-6 hours, fairly uniform plasma glucose levels are expected.18
Another limitation is that we were unable to account for differences in patients’ time course of CS. For instance, patients with more advanced disease, who likely have more scar or fibrosis, are probably less likely to have an improvement in LVEF than who have less advanced disease.5 On the other hand, the presence of focal FDG reflects that at least some degree of inflammation is present, and identifies a group of patients who may benefit from anti-inflammatory therapy. Due to the relatively small number of patients included in our study, we were unable to assess whether the extent or severity of baseline inflammation can be used to further identify sub-groups who are most and least likely to respond. The reduction in FDG observed in our study was attributed to anti-inflammatory therapy, but it is possible that in some cases the decrement in inflammation could be the result of progressive end-stage disease rather than successful treatment. However, such a reduction would be associated with worsening LVEF and thus, the effect of possibly including such patients in our cohort would bias us toward a null finding and minimize the association detected in our study. To that end, excluding patients with advanced disease may demonstrate an even greater benefit of treating active disease.
The results of our study of CS patients evaluated with serial cardiac PET FDG exams support the hypothesis that a reduction in inflammation as measured by the intensity and extent of FDG uptake on cardiac PET correlates with an improvement in LVEF. These data suggest serial PET scanning may help guide titration of immunosuppressive therapy to prevent and treat heart failure in CS.
New Knowledge Gained
Our study is the first to demonstrate that among patients with known CS treated with immunosuppressive therapies, a reduction in the extent and severity of myocardial inflammation is associated with an increase in left ventricular systolic function. Thus, among patients treated with immunosuppressive therapies, serial cardiac PET studies may have a role in guiding the intensity and duration of immunosuppressive therapy in order to minimize the development or progression of systolic dysfunction as well as reduce unnecessary treatment.
References
Iannuzzi MC, Fontana JR. Sarcoidosis: Clinical presentation, immunopathogenesis, and therapeutics. J Am Med Assoc 2011;305:391-9.
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: A clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation 1978;58:1204-11.
Yazaki Y, Isobe M, Hiroe M, Morimoto S, Hiramitsu S, Nakano T, et al. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am J Cardiol 2001;88:1006-10.
Schliamser JE, Kadish AH, Subacius H, Shalaby A, Schaechter A, Levine J, et al. Significance of follow-up left ventricular ejection fraction measurements in the Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation trial (DEFINITE). Heart Rhythm 2013;10:838-46.
Chiu CZ, Nakatani S, Zhang G, Tachibana T, Ohmori F, Yamagishi M, et al. Prevention of left ventricular remodeling by long-term corticosteroid therapy in patients with cardiac sarcoidosis. Am J Cardiol 2005;95:143-6.
Grutters JC, van den Bosch JM. Corticosteroid treatment in sarcoidosis. Eur Respir J 2006;28:627-36.
Nery PB, Leung E, Birnie DH. Arrhythmias in cardiac sarcoidosis: Diagnosis and treatment. Curr Opin Cardiol 2012;27:181-9.
Youssef G, Beanlands RS, Birnie DH, Nery PB. Cardiac sarcoidosis: Applications of imaging in diagnosis and directing treatment. Heart 2011;97:2078-87.
Blankstein R, Osborne M, Naya M, Waller A, Kim CK, Murthy VL, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol 2013. doi:10.1016/j.jacc.2013.09.022.
Okumura W, Iwasaki T, Toyama T, Iso T, Arai M, Oriuchi N, et al. Usefulness of fasting 18F-FDG PET in identification of cardiac sarcoidosis. J Nucl Med 2004;45:1989-98.
Ohira H, Tsujino I, Yoshinaga K. (1)F-Fluoro-2-deoxyglucose positron emission tomography in cardiac sarcoidosis. Eur J Nucl Med Mol Imaging 2011;38:1773-83.
Dorbala S, Vangala D, Sampson U, Limaye A, Kwong R, Di Carli MF. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: A 82Rb PET/CT study. J Nucl Med 2007;48:349-58.
Kida K, Yoneyama K, Kobayashi Y, Takano M, Akashi YJ, Miyake F. Late gadolinium enhancement on cardiac magnetic resonance images predicts reverse remodeling in patients with nonischemic cardiomyopathy treated with carvedilol. Int J Cardiol 2013;168:1588-9.
Lower EE, Baughman RP. Prolonged use of methotrexate for sarcoidosis. Arch Intern Med 1995;155:846-51.
Schuller JL, Zipse M, Crawford T, Bogun F, Beshai J, Patel AR, et al. Implantable cardioverter defibrillator therapy in patients with cardiac sarcoidosis. J Cardiovasc Electrophysiol 2012;23:925-9.
Betensky BP, Tschabrunn CM, Zado ES, Goldberg LR, Marchlinski FE, Garcia FC, et al. Long-term follow-up of patients with cardiac sarcoidosis and implantable cardioverter-defibrillators. Heart Rhythm 2012;9:884-91.
Boellaard R. Need for standardization of 18F-FDG PET/CT for treatment response assessments. J Nucl Med 2011;52:93S-100S.
Boellaard R. Standards for PET image acquisition and quantitative data analysis. J Nucl Med 2009;50:11S-20S.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding
None.
Appendix
Appendix
See Figure 5.
Rights and permissions
About this article
Cite this article
Osborne, M.T., Hulten, E.A., Singh, A. et al. Reduction in 18F-fluorodeoxyglucose uptake on serial cardiac positron emission tomography is associated with improved left ventricular ejection fraction in patients with cardiac sarcoidosis. J. Nucl. Cardiol. 21, 166–174 (2014). https://doi.org/10.1007/s12350-013-9828-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9828-6