Abstract
Background
Left ventricular mechanical dyssynchrony (LVMD) induced by exercise stress was reported to be clinically useful in detecting multivessel coronary artery diseases. The aim of this study was to compare the prognostic value of LVMD induced by pharmacological stress with that induced by exercise stress.
Methods
We retrospectively examined 918 consecutive patients who underwent exercise (N = 310) or pharmacological stress (N = 608) 99mTc-tetrofosmin single-photon emission computed tomography (SPECT) with normal myocardial perfusion. LVMD was evaluated by phase analysis as the indices of phase bandwidth and phase standard deviation (PSD).
Results
During the follow-up period (2.2 ± 1.9 years), 74 major cardiac events (MCEs) occurred (7 cases of cardiac death, 17 cases of heart failure, and 50 cases of coronary intervention). In global patients, the indices of LVMD on rest images were significantly greater in patients with MCEs (bandwidth (°): 51 ± 31 vs 37 ± 21, P = .001, PSD: 14 ± 9 vs 10 ± 6, P = .001). The exercise stress bandwidth was significantly higher in patients with MCEs (62 ± 37° vs 42 ± 21°, P = .026), as was the pharmacological stress bandwidth (57 ± 35° vs 43 ± 24°, P = .006). Multivariate analysis demonstrated the exercise stress bandwidth to be an independent predictor of MCEs (HR 1.017, CI 1.003 to 1.032, P = .019), but the pharmacological stress bandwidth had no influence on MCEs.
Conclusions
LVMD induced by exercise stress was an independent predictor of MCEs in patients with normal perfusion SPECT, whereas that induced by pharmacological stress had no association with further events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular mechanical dyssynchrony (LVMD) is a conduction disturbance characterized by a wide QRS duration on electrocardiography. The degree of LVMD was analyzed by tissue Doppler imaging (TDI) assessed by echocardiography. Myocardial perfusion single-photon emission computed tomography (SPECT) (MPS) is able to analyze LVMD quantitatively by phase analysis.1 The indices of LVMD, such as phase standard deviation (PSD) and phase bandwidth, are well correlated with those measured by tissue Doppler imaging.2,3,4 The prognostic value for major cardiac events (MCEs) of LVMD was previously demonstrated in asymptomatic women,5 patients with systolic heart failure,6 and in those with acute coronary syndrome.7
Normal stress MPS findings are associated with low-cardiac event risk.8 Myocardial perfusion sometimes globally reduces in patients with multivessel coronary artery diseases (CAD). Thus, there are some underestimated cases when MPS has no signs of cardiac ischemia. In those cases LVMD induced by exercise stress has diagnostic value in the detection of multivessel CAD.9 However, it is unknown whether LVMD induced by pharmacological stress (hyperemic drugs) is associated with future events. In this study, we retrospectively investigated whether LVMD induced by exercise or pharmacological stress has prognostic value in patients with normal myocardial perfusion.
Methods
Study Population
We retrospectively examined 918 consecutive patients who underwent exercise (N = 310) or pharmacological stress (N = 608) 99mTc-tetrofosmin SPECT. All patients were scheduled to undergo stress-rest ECG-gated MPS due to possible or definite CAD. Patients with bundle branch block on electrocardiography and abnormal MPS (summed stress score ≥ 3) were excluded from this study. The endpoint was the incidence of MCEs consisting of cardiac death, non-fatal myocardial infarction, hospitalization due to heart failure, and coronary intervention due to acute coronary syndrome or worsening symptom of angina. The presence of cardiac events was followed up in all patients after MPS. The study was conducted in accordance with the standards of the local ethics committee. For this retrospective study design, formal consent was not required.
Myocardial Perfusion SPECT Study
Pharmacological (adenosine) or exercise stress 99mTc-tetrofosmin SPECT was performed for each patient using a 1-day protocol. The dose of 99mTc-tetrofosmin was 296 MBq at stress imaging and 596 MBq at rest imaging. Stress was induced by ergometer and was stopped when the patient’s heart rate reached more than 85% of the maximum predictive heart rate. Horizontal or downsloping ST-segment depression (≥ .1 mV) on electrocardiogram was considered as positive exercise test. Pharmacological stress by adenosine with low-dose exercise (25 W) was used for patients with a low exercise tolerance. Patients were instructed not to consume caffeine for 24 hours before pharmacological stress. 99mTc-tetrofosmin was injected 1 minute before the end of exercise or 3 minutes after the start of adenosine (120 µg/min and total 6 minutes). Stress and rest images were acquired 30 minutes after 99mTc-tetrofosmin injection. Four hours later, the rest image was acquired after re-injection of 99mTc-tetrofosmin.
SPECT Acquisition Protocol
Stress and rest images were acquired on a dual-detector gamma camera (Siemens Medical Solutions, Erlangen, Germany) using a low-energy, high-resolution collimator. The gamma camera rotated, collecting 64 projections over 180° for 40 seconds per projection. The projection data were reconstructed into 64 × 64 matrix images using the filtered back projection method. The quantitative-gated SPECT (QGS) software (Cedars Sinai Medical Center, CA, USA) was used for analysis of the left ventricular functional parameters [left ventricular ejection fraction (LVEF) and end diastolic (EDV)/systolic volume (ESV)].
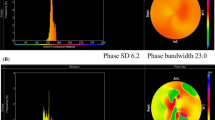
Quantitative Data Analysis of Perfusion SPECT
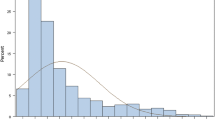
The SPECT images were divided into 17 segments and scored visually using a 5-point scale. The summed stress and rest scores (SSS and SRS) were calculated by adding the scores of these segments of the left ventricle. The summed difference score (SDS) was calculated by SSS minus SRS. Normal myocardial perfusion SPECT was defined as an SSS of less than 3. To evaluate the degree of LVMD, we calculated two indices, the phase standard deviation (PSD) and bandwidth, by phase analysis using Heart Function View software (Nihon Medi-Physics. Co. Ltd., Tokyo, Japan). A phase distribution of the mechanical contraction onset at each regional left ventricular wall was generated, and the histogram bandwidth and PSD were calculated.9
Statistical Analysis
Variables are expressed as the mean ± standard deviation. Normally distributed parameters were compared by t tests and non-normally distributed data were analyzed by the Mann–Whitney U test. Categorical data were compared using the Chi-square test. Multivariate analysis was performed by Cox proportional regression analysis, into which age, gender, LVEF, SSS, bandwidth at stress and combination with other cardiac diseases were entered. Event-free curves were calculated with Kaplan–Meier estimates and differences between two curves were evaluated using a log-rank test. A P value < .05 was considered significant.
Results
Clinical Characteristics of the Patients
The characteristics of the study population are shown in Table 1. The mean age was 70 ± 12 years and the mean LVEF was 71 ± 11%. SSS, SRS, and SDS were .3 ± .7, .2 ± .6, and .2 ± .6, respectively. The QRS duration on electrocardiography was 98.0 ± 9.5 ms. Based on these results, all patients had neither evidence of cardiac ischemia on MPS nor notable LVMD on electrocardiography.
Comparison Between Exercise and Pharmacological Stress
The characteristics of patients with exercise and pharmacological stress are shown in Table 2. Those with pharmacological stress were older (P < .001), had a lower eGFR (P = .004), and a higher EDV (P < .001) and ESV (P = .015). The proportion of male patients was larger in the exercise stress group (P = .001). In both groups, the patients had a normal LVEF by QGS and no evidence of LVMD by phase analysis.
Cardiac Events During Follow-up
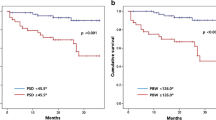
During the follow-up period of 2.2 ± 1.9 years, 74 MCEs occurred. Seven patients had cardiac death, 17 patients were hospitalized due to worsening heart failure, and 50 patients required coronary intervention due to acute coronary syndrome or worsening symptom of angina. The Kaplan–Meier event-free curve revealed that there was no significant difference in cardiac events between pharmacological and exercise stress (P = .108) (Figure 1). The comparison of the data with and without MCEs is shown in Table 3 ((A) global patients (N = 918), (B) pharmacological stress (N = 608), (C) exercise stress (N = 310)). The patients with MCEs were older (P < .001), and had lower LVEF (< .001) and greater SSS (P < .001) although all patients had no evidence of cardiac ischemia (SSS < 3) nor decreased cardiac function (Table 3A). The indices of LVMD on rest images were significantly greater in patients with MCEs (bandwidth (°): 51 ± 31 vs 37 ± 21, P = .001, PSD: 14 ± 9 vs 10 ± 6, P = .001). Similarly, the indices of LVMD on stress images were significantly greater in patients who experienced cardiac events in both pharmacological (bandwidth (°): 57 ± 35 vs 43 ± 24, P = .006; PSD: 16 ± 10 vs 12 ± 7, P = .011) and exercise (bandwidth (°): 62 ± 37 vs 42 ± 21, P = .026; PSD: 17 ± 12 vs 12 ± 6, P = .040) stress groups (Table 3B, C).
Univariate and Multivariate Analyses
In global patients, the bandwidth at rest (P = .013), age (P < .001), gender (P = .043), LVEF (P = .003), and SSS (P = .004) were independent predictors of cardiac events (Table 4A). In patients with pharmacological stress, the bandwidth at stress (P = .004), age (P = .002), LVEF (P < .001), and SSS (P = .008) were univariate predictors of cardiac events (Table 4B). However, based on multivariate analysis, age (P = .002) and LVEF (P < .001), but not bandwidth, were independent predictors of cardiac events. In patients with exercise stress, the bandwidth at stress (P = .002), LVEF (P = .013), and SSS (P < .001) were univariate predictors of cardiac events (Table 4C). Bandwidth at stress was also an independent predictor of cardiac events in multivariate analysis (P = .019).
Discussion
This is the first study to describe the prognostic value of bandwidth on exercise stress as an index of LVMD in patients with no evidence of cardiac ischemia. LVMD induced by exercise stress was associated with further cardiac events, whereas that induced by pharmacological stress was not.
LVMD is evaluated by the QRS duration on electrocardiography or by TDI assessed by echocardiography. Phase analysis on MPS is also one of the methods for evaluating LVMD. Heart Function View evaluates the phase distribution and regional left ventricular onset of mechanical contraction.10 LVMD is quantitatively assessed by the indices such as PSD and bandwidth. The reference values in normal subjects of this software to evaluate the degree of LVMD were described in the previous report.11 Normal upper limits of bandwidth and phase SD at rest images were 38° and 10°, respectively. In our study, mean values of bandwidth and phase SD in patients without cardiac events at rest images were 37° and 10°, respectively (Table 3A). Thus, normal cut-off values of bandwidth and phase SD based on the previous report might be applicable. LVMD assessed by MPS was previously reported to be well correlated with that assessed by TDI.2 The assessment of LVMD is important to select patients for cardiac resynchronization therapy (CRT). TDI was prevalent as the evaluation method of LVMD because of its non-invasive nature, but CRT guided by TDI had negative results due to lack of reproducibility.12,13 Phase analysis on MPS just after CRT can predict the CRT response.14
Normal stress MPS findings in the Japanese population are associated with low-cardiac event risk.8 However, 74 patients (8.1%), including 50 with coronary intervention, had cardiac events in our study. No focal perfusion defect was observed because of a global reduction in patients with left main or 3-vessel CAD. LVMD induced by exercise stress was reported in patients with multivessel CAD.9 LV ischemic myocardium induced by exercise stress contracts weaker than the other non-ischemic wall. The strong wall pushes out the weaker wall, which leads to delayed contraction of the weak wall. Accordingly, LVMD may develop in association with cardiac ischemia induced by exercise stress even with a pseudo-normal MPS and multivessel CAD. On the other hand, adenosine increases the volume of microvascular circulation and it is not considered to induce actual myocardial ischemia despite the development of reversible perfusion defects. No significant stress-induced alteration within the indices of mechanical dyssynchrony using phase analysis was observed in the majority of patients (70%) evaluated under pharmacological stress.15 However, there are conflicting results about LVMD induced by pharmacological stress. A previous report demonstrated that the maximum difference in time to end-systole, which was defined as the index of LVMD in that study, in the 17 segments increased after adenosine loading in CAD patients, but not in normal subjects.16 That study suggested that adenosine has the ability to induce LVMD, but LVMD was evaluated by the time volume curve, not by phase analysis. Dobutamine has also been used for pharmacological stress. In patients with heart failure, the severity of LVMD increases in accordance with dobutamine stress, and a good response of CRT was achieved in patients with LVMD induced by dobutamine.17 Regardless of adenosine, dobutamine increases oxygen demand of the myocardium via β1 stimulation and causes cardiac ischemia in patients with CAD. Accordingly, LVMD induced by dobutamine may be via to the same mechanism as that by exercise stress.
Previous reports showed that LVMD had an association with cardiac function.18 In multivariate analysis of our study, bandwidth at rest was one of the independent predictors of cardiac events in global patients (P = .013). Although in our study MPS had no signs of cardiac ischemia (SSS < 3) and mean LVEF was within normal range (71 ± 11%), LVEF was significantly smaller (P < .001) and SSS was significantly greater (P < .001) in patients with MCEs (Table 3A). A reduced LVEF and severity of myocardial scar on SPECT imaging were reported to be independent predictors of LVMD.19 Accordingly, it was natural that bandwidth at rest also had the ability as a predictor for future cardiac events, similarly to LVEF or SSS.
MPS has been established as a tool to diagnose CAD, but in contrast to the other morphological approaches, such as coronary angiography or computed tomography, exercise or pharmacological stress is necessary for an accurate diagnosis of CAD. Although pharmacological stress is considered when patients have a low exercise tolerance, MPS by pharmacological stress is known to have the same sensitivity and specificity for the diagnosis of CAD as exercise stress.20,21 Pharmacological stress patients had a higher mortality rate than exercise stress patients even though they had no evidence of cardiac ischemia based on stress MPS 22 because they were older, and had a higher prevalence of diabetes and hypertension. In our study, pharmacological stress patients were also older (P < .001), had a lower eGFR (P = .004), and higher prevalence of hypertension (P < .001), but there was no significant difference in cardiac events between pharmacological and exercise stress SPECT (P = .108, Figure 1). One of the reasons may be that patients were classified as low-cardiac risk based on MPS. All patients had no evidence of cardiac ischemia on MPS (SSS < 3). The annual event rate for cardiac events was reported to be low in patients with a normal scan.8,23 As mortality is influenced by other clinical factors, such as age, gender, or renal function, age was an independent predictor in pharmacological stress patients in our study.
Limitations
First, this study was a retrospective, non-randomized study. The patients who had pharmacological stress were significantly older because of their lower physical activity. Age has a strong impact on the prognosis of elderly people. The cardiac event rate did not differ between the exercise and pharmacological stress groups. If the patients with pharmacological stress were younger, the cardiac event rate may have been lower in our study cohort. Therefore, LVMD is less likely to be an independent predictor in patients with pharmacological stress. Second, in this study, coronary intervention due to acute coronary syndrome or worsening symptom of angina included major cardiac events because all patients had no evidence of cardiac ischemia on MPS. Thus, the cardiac event rate was higher (8.1%) than that in previous reports. Third, Cox proportional regression analysis could not be employed for multivariate analysis with gender as a variable in separate groups because the number of cardiac events was relatively low and especially in exercise stress group all patients with events were male. Bandwidth at stress had significant strong correlations with that at rest both in exercise (r = .985, P < .001) and pharmacological stress (r = .986, P < .001). For these reasons bandwidth at rest could not be added to the variables at both exercise and pharmacological stress groups. When bandwidth at rest was included as variables instead of that at stress, it was not an independent predictor both in exercise (P = .0644, CI .999 to 1.036) and pharmacological (P = .109, CI .998 to 1.016) stress. Thus, the indices of LVMD at stress might be more useful as a prognostic marker than those at rest, especially in exercise stress.
New Knowledge Gained
Each index of the phase analysis of exercise stress MPS was related to cardiac events even though MPS demonstrated no evidence of cardiac ischemia. Pharmacological stress is suitable for elderly patients who have a low exercise tolerance, but the information provided by exercise stress is greater than that by pharmacological stress in the clinical setting.
Conclusions
LVMD induced by exercise stress was an independent predictor of cardiac events in patients with normal perfusion SPECT, whereas that induced by pharmacological stress had no association with further events.
Abbreviations
- LVMD:
-
Left ventricular mechanical dyssynchrony
- SPECT:
-
Single-photon emission computed tomography
- PSD:
-
Phase standard deviation
- MCEs:
-
Major cardiac events
- TDI:
-
Tissue Doppler imaging
- MPS:
-
Myocardial perfusion SPECT
- CAD:
-
Coronary artery diseases
- QGS:
-
Quantitative-gated SPECT
- LVEF:
-
Left ventricular ejection fraction
References
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol. 2005;12:687-95.
Henneman MM, Chen J, Ypenburg C, Dibbets P, Stokkel M, van der Wall EE, et al. Phase analysis of gated myocardial perfusion SPECT compared to tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol. 2007;49:1708-14.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Real-time 3-dimensional echocardiography as a novel approach to quantify left ventricular dyssynchrony: a comparison study with phase analysis of gated myocardial perfusion single photon emission computed tomography. J Am Soc Echocardiogr. 2008;21:801-7.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Left ventricular dyssynchrony assessed by two 3-dimensional imaging modalities: phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging. 2008;35:166-73.
Sharma RK, Volpe G, Rosen BD, Ambale-Venkatesh B, Donekal S, Fernandes V, Wu CO, Carr J, Bluemke DA, Lima JA. Prognostic implications of left ventricular dyssynchrony for major adverse cardiovascular events in asymptomatic women and men: the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2014. https://doi.org/10.1161/JAHA.114.000975.
Penicka M, Bartunek J, Lang O, Medilek K, Tousek P, Vanderheyden M, De Bruyne B, Maruskova M, Widimsky P. Severe left ventricular dyssynchrony is associated with poor prognosis in patients with moderate systolic heart failure undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2007;50:1315-23.
Sato M, Toyama T, Kasama S, Hoshizaki H, Oshima S, Kurabayashi M. Left ventricular mechanical dyssynchrony after acute myocardial infarction assessed by CardioGRAF analysis is a predictor of subsequent cardiac events. Ann Nucl Cardiol. 2017;3:20-8.
Matsuo S, Nakajima K, Horie M, Nakae I, Nishimura T. Prognostic value of normal stress myocardial perfusion imaging in Japanese population—a study based on the J-ACCESS study. Circ J. 2008;72:611-7.
Hida S, Chikamori T, Tanaka H, Igarashi Y, Shiba C, Usui Y, Hatano T, Yamashina A. Diagnostic value of left ventricular dyssynchrony after exercise and at rest in the detection of multivessel coronary artery disease on single-photon emission computed tomography. Circ J. 2012;76:1942-52.
Nakae I, Hayashi H, Matsumoto T, Mitsunami K, Horie M. Clinical usefulness of a novel program “Heart Function View” for evaluating cardiac function from gated myocardial perfusion SPECT. Ann Nucl Med. 2014;28:812-23.
Nakajima K, Okuda K, Matsuo S, Kiso K, Kinuya S, Garcia EV. Comparison of phase dyssynchrony analysis using gated myocardial perfusion imaging with four software programs: Based on the Japanese Society of Nuclear Medicine working group normal database. J Nucl Cardiol. 2017;24:611-21.
Chung ES, Leon AR, Tavazzi L, Sun J-P, Nihoyannopoulos P, Merlino J, et al. Results of the predictors of response to CRT (PROSPECT) trial. Circulation. 2008;117:2608-16.
Ruschitzka F, Abraham WT, Singh JP, Bax JJ, Borer JS, Brugada J, et al. Cardiac resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med. 2013;369:1395-405.
Gendre R, Lairez O, Mondoly P, Duparc A, Carrié D, Galinier M, et al. Research of predictive factors for cardiac resynchronization therapy: a prospective study comparing data from phase-analysis of gated myocardial perfusion single-photon computed tomography and echocardiography: Trying to anticipate response to CRT. Ann Nucl Med. 2017;31:218-26.
Aljaroudi W, Koneru J, Heo J, Iskandrian AE. Impact of ischemia on left ventricular dyssynchrony by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol. 2011;18:36-42.
Horigome M, Yamazaki K, Ikeda U. Assessment of left ventricular dyssynchrony in patients with coronary artery disease during adenosine stress using ECG-gated myocardial perfusion single-photon emission computed tomography. Nucl Med Commun. 2010;31:864-73.
Chattopadhyay S, Alamgir MF, Nikitin NP, Fraser AG, Clark AL, Cleland JG. The effect of pharmacological stress on intraventricular dyssynchrony in left ventricular systolic dysfunction. Eur J Heart Fail. 2008;10:412-20.
Atchley AE, Trimble MA, Samad Z, Shaw LK, Pagnanelli R, Chen J, et al. Use of phase analysis of gated SPECT perfusion imaging to quantify dyssynchrony in patients with mild-to-moderate left ventricular dysfunction. J Nucl Cardiol. 2009;16:888-94.
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R, et al. Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol. 2011;18:24-30.
Levine MG, Ahlberg AW, Mann A, White MP, McGill CC, de Leon CM, et al. Comparison of exercise, dipyridamole, adenosine, and dobutamine stress with the use of Tc-99m tetrofosmin tomographic imaging. J Nucl Cardiol. 1999;6:389-96.
Gupta NC, Esterbrooks DJ, Hilleman DE, Mohiuddin SM. Comparison of adenosine and exercise thallium-201 single photon computed tomography (SCPECT) myocardial perfusion imaging. The GE SPECT Multicenter Adenosine Study Group. J Am Coll Cardiol. 1992;19:248-57.
Rozanski A, Gransar H, Hayes SW, Friedman JD, Hachamovitch R, Berman DS. Comparison of long-term mortality risk following normal exercise vs adenosine myocardial perfusion SPECT. J Nucl Cardiol. 2010;17:999-1008.
Galassi AR, Azzarelli S, Tomaselli A, Giosofatto R, Ragusa A, Musumeci S, et al. Incremental prognostic value of technetium-99m-tetrofosmin exercise myocardial perfusion imaging for predicting outcomes in patients with suspected or known coronary artery disease. Am J Cardiol. 2001;88:101-6.
Disclosures
Drs Tomohiko Sakatani, Takeru Kasahara, Daisuke Irie, Yoshinori Tsubakimoto, Akiko Matsuo, Hiroshi Fujita, Keiji Inoue have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Saurabh Malhotra, MD, MPH.
Funding
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sakatani, T., Kasahara, T., Irie, D. et al. Prognostic value of left ventricular mechanical dyssynchrony induced by exercise stress in patients with normal myocardial perfusion single-photon emission computed tomography. J. Nucl. Cardiol. 29, 1–10 (2022). https://doi.org/10.1007/s12350-020-02389-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02389-6