Abstract
Supporting evidence and intervention resources for addressing childhood trauma are growing, with schools indicated as a potentially critical system for service delivery. Multiple points for prevention and intervention efforts in schools are possible, but in this manuscript, we review evidence on trauma-specific interventions targeted to students exhibiting negative symptoms. Trauma-specific interventions with evidence and utility for school-based delivery are highlighted, along with key considerations in selection. In addition, we discuss the potential to maximize the impact of trauma-specific interventions for individual students when delivered as part of a school-wide trauma-informed approach that incorporates system-level prevention and intervention strategies. Future directions for research on trauma-specific interventions and trauma-informed approaches in school settings are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Childhood trauma is increasingly recognized as an epidemic (Blaustein, 2013), with strong associations between increased adverse childhood experiences and the likelihood of negative outcomes such as mental health challenges, lower cognitive abilities and academic achievement, and difficulties in school (Copeland, Keeler, Angold, & Costello, 2007; Nooner et al., 2012; Perfect, Turley, Carlson, Yahanna, & Saint Gilles, 2016). Although indications of long-term negative consequences associated with adverse childhood experiences have a long history (e.g., Anda et al., 2006; Felitti et al., 1998), only in more recent years has cross-disciplinary interest in childhood trauma exploded, thrusting school systems to the forefront of efforts to put in place a continuum of prevention and intervention efforts. The purpose of this paper is to review evidence on trauma-specific interventions targeted to students exhibiting negative symptoms, offering key considerations in selection. Additional guidance is provided regarding how school systems might incorporate trauma-informed practices into a comprehensive system of service delivery.
To begin, definitions are needed as terms such as trauma exposure, traumatic experience, toxic stress, and adverse experiences have all been associated with childhood trauma. In the landmark Centers for Disease Control-Kaiser Permanente Adverse Childhood Experiences Study (see Felitti et al., 1998), questions regarding adverse experiences prior to age 18 years are grouped into three primary categories: (1) abuse (physical, sexual, psychological), (2) neglect (emotional, physical), and (3) household challenges (mother treated violently, household substance abuse, mental illness in household, parental separation or divorce, criminal household member). In addition to these types of adversities, symptoms as a result of traumatic experience can also occur through exposure to events such as acts of terrorism, natural disasters, and war or refugee experiences (American Psychiatric Association, 2013). Combining these various exemplars and incorporating the recent definition provided by the Substance Abuse and Mental Health Services Administration (SAMHSA, 2014), childhood trauma can be described as occurring based on an event that poses a threat, which may be experienced by the child as harmful (physically or emotionally); the child’s reaction to the traumatic experience may have enduring effects on functioning and well-being. In Fig. 1, we present a visual to illustrate this cycle of exposure, reaction, and consequence, providing points of opportunity for school-based intervention efforts. As shown, the antecedent (trigger) to behavior (symptomology) is comprised of a combination of (a) exposure to a traumatic event and (b) setting event(s) that establish individual interpretation of and reaction to the event. Features of the exposure to the traumatic event, including predictability, duration, intensity, and consequences, can play an important role in individual reaction (see Brock, Reeves, & Nickerson, 2014), yet are not the only influence. Setting event(s) are established through multiple factors (personal, environmental, history of prior trauma exposure) and can serve to buffer against or exacerbate negative interpretation and reaction. Together, the combination of exposure to an event and individual interpretation and reaction lead to the observed behavior (social, emotional, behavioral, and/or physical symptomology). The consequence, or reaction by others to that behavior, can serve to reinforce individual interpretation and reaction as new situations are presented. These defining characteristics of childhood trauma are important in interpreting prevention and intervention efforts—that is, although we acknowledge that childhood exposure to potentially traumatic events are undesirable, not all individuals react in the same way. Thus, a one-size fits all intervention approach may not be appropriate due to a combination of internal and external factors, and thus, determining the most appropriate point(s) for intervention is critical.
In acknowledging the need for greater understanding of childhood trauma, extension of intervention efforts beyond the individual has burgeoned, and thus, a wider view of approaches has been advocated. Specifically, trauma-informed and trauma-sensitive approaches have been referenced within the literature with regard to system-wide attention to childhood trauma and its impact in schools. Our view is consistent with SAMHSA (2014) in that trauma-informed approaches represent a continuum of efforts that foster a system-wide response to the needs of those exposed to trauma (Chafouleas, Johnson, Overstreet, & Santos, 2016). In school-wide service delivery, prevention efforts form a first point for intervention and should focus on removing, minimizing, or neutralizing the exposure to a traumatic event. For example, positively focused, proactive practices should be implemented by all school staff to foster a safe and supportive climate. In a second point for intervention, school staff should be prepared to create safe and supportive classrooms that reduce the likelihood of triggering events through their (a) realization about trauma and its effects, (b) recognition of trauma signs—and also should be ready for (c) response in a way that embraces trauma understanding, and (d) resistance of inadvertent re-traumatization (SAMSHA, 2014). Yet another point for intervention is focused on the student who is exhibiting maladaptive interpretation of or reaction (social, emotional, behavioral, physical symptoms) to the event, with efforts defined as trauma specific and delivered by specially trained personnel in small group or individual formats. These examples of points for intervention in school-wide service delivery align with Cole, Eisner, Gregory, and Ristuccia (2013)’s description of a trauma-sensitive school, thus incorporating both educational and behavioral perspectives on childhood trauma to both meet individual need for treatment and create a system-wide culture that embraces the impact of trauma on learning and works to ensure all students feel safe and supportive.
In summary, a wider view regarding features to a trauma-informed approach acknowledges that trauma-specific intervention may be provided to some students within the school setting, but all school personnel are expected to facilitate learning through the creation of safe and supportive classrooms. Consistent with this view, we define trauma-specific interventions as individually focused interventions that typically target amelioration of symptomology and are delivered by specially trained personnel. The need for specially trained personnel is aligned with the 2015 National Child Traumatic Stress Network position statement outlining expected areas of clinical competency in order to deliver trauma-specific intervention. In this paper, we focus on review and selection of trauma-specific interventions delivered to individual students with intent to target improvement of symptoms and long-term trauma recovery, not those interventions that address immediate crisis response (e.g., psychological first aid) or address other points for intervention (i.e., prevention or response efforts).
Overview of the Impact of Childhood Trauma on Schools
Childhood trauma is associated with risk factors for multiple aspects of health and life quality throughout the life course (see Fig. 2). Although evidence to date hails primarily through retrospective studies with adults, emerging work substantiates this life-course framework through documentation of the frequency and chronicity of adverse experiences in childhood, thus providing implications for school-based service delivery. Recent results from trauma screening conducted in school settings support substantial numbers of students who report experiencing traumatic stress symptoms at elevated levels. For example, one study found traumatic stress symptoms reported at clinical or subclinical levels in 13.5% of participating middle school students (Woodbridge et al., 2016), and another study found moderately elevated or clinically significant levels in 35.5% of their elementary sample (Gonzalez, Monzon, Solis, Jaycos, & Langley, 2016). Clearly, students are coming to school with exposure to a potentially traumatic event and may be presenting with symptoms stemming from those experiences, but the impact on relevant school outcomes has yet to be fully understood. In a retrospective study of a sample from an urban community with high violence exposure, one study found that the majority of participants had some exposure to adverse childhood experiences and that report of 4 or more different types of adverse childhood experiences (ACES) was associated with increased risk of learning/behavior problems as well as obesity (Burke, Hellman, Scott, Weems, & Carrion, 2011). For example, learning/behavior problems were found in 3% of participants with 0 ACES, 20.7% for those reporting 1–3 ACES, and 52.2% for those with 4 or more ACES. In a recent study, Porche, Costello, and Rosen-Reynoso (2016) found that children exposed to higher numbers of adverse family experiences were more likely to have more mental health diagnoses, which also led to decreased engagement at school and a greater likelihood of retention and placement in special education services. In summary, the current literature supports that schools are comprised of a substantial volume of children who have been exposed to potentially traumatic events, with many of these students presenting behavior suggestive of traumatic stress reactions, and that exposure with more substantial intensity, frequency, and/or duration increases likelihood of negative school-relevant outcomes. Next, we provide more detailed review of impact at the level of (a) the student and (b) the school.
Impact at the Student Level
As noted, evidence has converged regarding the long-term and enduring negative consequences for individuals who experience childhood trauma. More recent reviews (e.g., Perfect et al., 2016) have attempted to disaggregate impacts of exposure to traumatic events and traumatic stress symptoms specifically related to educational outcomes. Next, we summarize this literature, separating content into psychosocial and academic impact, as done in the systematic review by Perfect et al. (2016).
Psychosocial
One aspect of the review focused on identifying teacher-reported social, emotional, and behavioral functioning of students who have experienced a traumatic event. The authors identified 24 studies including teacher ratings/observations of social functioning. Results of the systematic review broadly indicated elevated teacher-rated behavior symptomatology for children with trauma exposure. Studies included in the review also reported on internalizing symptomatology (Perfect et al., 2016). Across the studies, the authors found patterns of elevated symptoms of withdrawal, depression, and anxiety across different traumatic event types. Consistent findings related to elevated teacher-rated externalizing symptoms were also found, with greater externalizing symptoms (e.g., aggression, hyperactivity, impulsivity, and oppositional defiant behaviors) across different types of traumatic events such as natural disasters, sexual abuse, maltreatment, and neglect. In summary, a review of the evidence supports greater psychosocial challenges in classroom settings for those children with trauma exposure.
Academic
Perfect et al. (2016) also synthesized the literature on the effects of trauma on academic functioning; the authors identified 34 articles that measured outcomes in this domain. Interestingly, more studies used rating scales to evaluate academic functioning rather than standardized assessment or other permanent products (Perfect et al., 2016). Across the group of studies, results largely indicated a relationship between traumatic event exposure and poorer academic achievement. Several studies compared children with trauma exposure or posttraumatic stress disorder (PTSD) to controls, finding that these students demonstrated lower performance in both math and reading (De Bellis, Hooper, Spratt, & Woolley, 2009; De Bellis, Woolley, & Hooper, 2013; Eckenrode, Laird, & Doris, 1993; Saigh, Mroueh, & Bremner, 1997). In addition, three studies found that students with trauma exposure were more likely to be retained and repeat a grade (Eckenrode, Rowe, Laird, & Brathwaite, 1995; Shonk & Cichetti, 2001; Wodarski, Kurtz, Gaudin, & Howing, 1990). In summary, although further work is needed to tease apart the specific mechanisms impacting academic outcomes, available evidence suggests a relationship between trauma exposure and academic achievement.
Impact at the School (Classroom and District) Level
The review conducted by Perfect et al. (2016) also evaluated other school-related outcomes that can have substantial impact at the systems level, such as school-wide climate and disciplinary practices. For example, several studies looked at discipline patterns for students with trauma exposure; one study found that children with trauma exposure had more discipline issues and referrals than control students (Eckenrode et al., 1993), and another found that students with trauma exposure were more likely to be suspended than non-trauma-exposed students (Lansford et al., 2002). In addition, a relationship between trauma exposure and attendance was well documented in the review; several studies indicated that those students who experienced trauma were more likely to miss school (Fantuzzo, Perlman, & Dobbins, 2011; Hurt, Malmud, Brodsky, & Giannetta, 2001; Lansford et al., 2002; Mathews, Dempsey, & Overstreet, 2009; Shonk & Cicchetti, 2001; Wodarski et al., 1990). Another large-scale study included in the review found that students with trauma exposure experienced greater mobility or school transfers than comparison students and found that mobility significantly contributed to the relationship between trauma exposure and academic achievement (Eckenrode et al., 1995). In summary, each of these indicators has negative consequences not only for individual students but school systems as school personnel are challenged to maintain the learning environment while dedicating resources to respond to a potentially ever-changing context. Thus, the full impact of childhood trauma at the systems level may be determined based on a combination of individual student factors as well as resources used in preparedness and response to resulting challenging behaviors.
Evidence-Based Treatment and Impact on School-Relevant Outcomes
The results of systematic reviews and meta-analyses evaluating trauma-specific interventions provide some of the most compelling evidence that informs our understanding of school-based interventions for childhood trauma. We identified three key reviews in the last 10 years (2006 to 2016) focused on treating child trauma (Dorsey et al., 2017; Jaycox, Morse, Tanielian, & Stein, 2006; and Rolfsnes & Idsoe, 2011). Several key findings inform the way we understand school-based trauma treatment. First, schools have been among the most common settings for intervention delivery. For example, the review by Dorsey et al. (2017) revealed that schools were the most frequent setting for trauma-specific interventions, comprising 10 of the 37 reviewed studies. Second, results of these reviews indicate that trauma-specific interventions delivered in schools can be effective. For example, the meta-analysis conducted by Rolfnes & Idsoe (2011) for treatment of PTSD symptomatology in school-based settings indicated relatively large effects (0.68, SD = 0.41). Third, evidence for school-based interventions for childhood trauma extends across developmental levels and populations. For example, the reviews provided support for school-based trauma interventions that span across developmental levels, although only one intervention (i.e., trauma-focused CBT) was indicated as having “promise” in preschool settings (see Jaycox et al., 2006). In addition, school-based interventions also demonstrate evidence for use in a range of populations, including international populations of children and children exposed to natural disasters, war, and terrorism abroad (Dorsey et al., 2017; Jaycox et al., 2006; Rolfnes & Idsoe, 2011).
An important point with regard to the body of evidence behind interventions for childhood trauma relates to the theoretical approach. In their review of 37 studies focusing on child and adolescent trauma treatment across settings (not necessarily only in schools), Dorsey et al. (2017) categorized each intervention according to the evidence supporting its use, from treatments with questionable efficacy to well-established treatments. Of the treatments categorized as well established or probably efficacious, only one was not based in cognitive behavioral therapy (CBT). According to their review, group-based CBT (a frequently utilized mode of school intervention for individual students identified at risk) was a well-established treatment, along with individually delivered CBT with and without parent involvement. In addition, the authors concluded that for those individual interventions that met the well-established criteria, almost all included a combination of the following six components: (1) psychoeducation about trauma and the intervention; (2) emotion regulation training; (3) imaginal exposure; (4) in vivo exposure; (5) cognitive processing; and (6) problem solving—all of which are aligned with CBT approaches. In sum, it appears that CBT-focused strategies and treatments are among most effective interventions available for treating childhood trauma.
Evidence exists for a variety of interventions targeting childhood trauma, with many indicating promise for delivery in school-based settings and also offering overlap in content and approach. However, given variations in features across interventions, selection of an intervention appropriate for a particular context requires attention to key considerations. The National Child Traumatic Stress Network (NCTSN) created a series of steps when reviewing and selecting interventions, which can apply to school-based delivery of trauma-specific interventions. In particular, a list of core components to consider, separated by intervention objectives and practice components, can be helpful in reviewing “fit” of a particular intervention. See Table 1 for a summary.
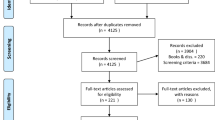
Next, we have selected a few school-based trauma-specific interventions deemed as promising, walking more specifically through the evidence related to social, academic, and other school-relevant outcomes in order to facilitate decisions about optimal selection of a specific intervention. The interventions included in Table 2 were selected by reviewing the NCTSN Empirically Supported Treatments and Promising Practices (2016) and the Substance Abuse and Mental Health Services Administration’s (SAMHSA) National Registry of Evidence-Based Programs and Practices (NREPP) for school-based trauma-specific interventions. We selected interventions based on the following criteria. First, we selected interventions from NREPP and NCTSN with the highest standard of evidence available, which we defined as interventions with at least one study with a control condition (control group, wait-list design, or multiple baselines); treatments or interventions relying on anecdotal, case study, or pilot study evidence alone were excluded. Thus, we acknowledge that of the many interventions available for review on NREPP and NCTSN, few studies available included rigorous design (e.g., randomized control trial). Although random assignment is often not an option in this work, clinicians are encouraged to adhere to the highest standard of evidence available, and thus, our presentation includes those trauma-specific interventions with the most rigorous evidence available. Second, we selected interventions that we considered most feasible for school-based implementation. Specifically, we omitted treatments that were family-focused or required parent/caregiver participation as a key element (e.g., trauma-focused CBT: Cohen, Mannarino, & Deblinger, 2006; for a review of TF-CBT for school-based practitioners, see Fitzgerald & Cohen, 2012). Although involving family systems can be effective in trauma-specific interventions, it may not always be feasible for school-based practitioners to center intervention delivery on family therapy given competing resource demands (Langley, Gonzalez, Sugar, Solis, & Jaycox, 2015). Third, given the previous note indicating that CBT-based interventions have the strongest evidence of efficacy, we chose to select only those programs with CBT-based components. Finally, we attempted to present interventions with school-relevant indicators, such as academic outcome measures or implementation by school-based professionals. In Table 2, a summary of selected interventions, including effects on the selected outcomes, is presented. Note that for those studies that did not report effect sizes, we provide the value calculated by Rolfsnes and Idsoe (2011) in their meta-analytic review. Table 2 also includes the approximate length/number of sessions for each intervention.
Cognitive Behavioral Intervention for Trauma in Schools (CBITS)
CBITS is one of the most well-documented school-based treatments for childhood trauma. Delivered by a school mental health professional, the intervention occurs primarily in small groups of 6–8 students with each session lasting about an hour (Jaycox, Kataoka, Stein, Langley, & Wong, 2012). As its name implies, CBITS is cognitively and behaviorally oriented and includes psychoeducation and behavioral modification training in an attempt to identify traumatic events and modify thought processes surrounding these events (see Jaycox et al., 2012 for a full description of the intervention). The CBITS program also seeks to promote generalization of skills outside of the treatment setting by assigning homework (e.g., challenging negative thoughts in everyday life). CBITS is student-focused as intervention is planned around a student-selected traumatic event that is most salient or problematic for them; the student’s specific trauma experience is further discussed in 1–3 individual sessions that occur separately from the group sessions. In addition, the program also includes a teacher information session and 2–3 optional parent sessions. The program seeks to proactively address barriers to implementation by providing suggestions in the manual for how school-based practitioners can respond to issues like student non-compliance.
A strength of the CBITS program is its cultural responsivity; the manual has been translated into five different languages: Spanish, Korean, Russian, Armenian, and Japanese (NCTSN, 2015), and there are several studies documenting the efficacy of the program in Native American students (Morsette et al., 2009; Goodkind, LaNoue, & Milford, 2010; Morsette, van den Pol, Schuldberg, Swaney, & Stolle, 2012) and immigrant populations (Kataoka et al., 2003). In addition, CBITS has some of the strongest empirical evidence of available school-based trauma interventions, given that randomized control trials or wait-list studies have been conducted (Kataoka et al., 2003; Stein et al., 2003). See Table 2.
CBITS has also been adapted into another program called Support for Students Experiencing Trauma (SSET; Jaycox et al., 2009) which is designed to be implemented by school staff without explicit clinical training such as teachers and school counselors. Although only pilot data are available to date, it represents a promising practice for school-based practitioners, perhaps as a consultation-based intervention.
Bounce Back
Bounce Back is a CBT-based, group delivered intervention designed for children ages 5–11. The creators of the intervention sought to combine the two most effective treatments for trauma, TF-CBT and CBITS, to target an intervention to younger, elementary-aged children (Langley et al., 2015). The authors noted that although TF-CBT has the strongest evidence available for the treatment of trauma reactions, it is not necessarily feasible for implementation in schools given that it requires a high level of parent involvement. The authors consulted with the creators of TF-CBT and CBITS along with other experts to select the key elements of each program to be adapted into this new program. Elements selected from each program include psychoeducation, exposure to avoided stimuli, narrative retelling of the traumatic event, relaxation strategies, and cognitive coping. The intervention was adapted for younger students including developmental scaffolding of activities, such as learning to identify feelings as a foundational activity before connecting feelings, thoughts, and behaviors in a therapeutic manner.
Bounce Back is delivered by a school-based clinician; all interventionists in the study evaluating the program’s efficacy were master’s level psychologists or social workers (Langley et al., 2015). See Table 2. The intervention consists of 10 group sessions lasting 50–60 min consisting of the aforementioned CBT-based approaches. Bounce Back also includes an additional 2 to 3 individual sessions lasting for 20–30 min each; the primary focus of these sessions is narrative retelling of the traumatic event experience by the child to gradually reduce adverse reactions related to the memory of the actual event. The program also includes 1–3 parent sessions which less involvement than the original TF-CBT intervention, which the authors describe as being much more feasible for school-based practitioners and working parents.
Modular Approach to Therapy for Children with Anxiety, Depression, Trauma, or Conduct Problems (MATCH-ADTC)
The MATCH intervention provides practitioners with tools to address symptoms and other diagnoses that often appear concurrently with negative reactions to trauma exposure and addresses common comorbidities that practitioners are likely to see in the field. Unlike some of the other common school-based trauma treatments, MATCH is provided to students individually rather than in a group format. The materials include modules for different client presentations such as anxiety, depression, or conduct problems, and then guidance if symptoms of other disorders arise throughout the course of treatment. School-based clinicians can select different modules for that are appropriate for the individual student with whom they are working. The number of sessions and duration of treatment depends on the type and number of modules selected by the practitioner, so each student’s experience will likely be unique.
In Table 2, a summary of outcomes related to the MATCH intervention is provided. However, the evidence supporting MATCH should be interpreted in light of the limitations that these studies were conducted in clinic-based settings and not in schools. In the studies evaluating the efficacy of MATCH, the providers were primarily social workers and psychologists indicating that school-based mental health providers, including school psychologists and social workers, could be a good fit to implement this intervention (Weisz et al., 2012). Although the MATCH interventions for conduct problems require greater parent involvement, the other modules largely include only the interventionist and the student, making it potentially feasible for school-based implementation. Thus, MATCH might be best described as a promising intervention for school-based practitioners. In addition, participants in available studies were a mixed clinical sample, and there were few participants experiencing PTSD symptoms. It is difficult to evaluate the effects on trauma because the authors did not report on participant traumatic exposure or evaluate PTSD symptomatology as an outcome measure (Chorpita et al., 2013; Weisz et al., 2012). Further research is needed to evaluate the effectiveness of a school-based MATCH intervention and the effects specifically for students with trauma exposure.
Trauma-Focused Coping in Schools (TFC)/Multimodality Trauma Treatment (MMTT)
TFC/MMTT also offers a cognitive behavioral oriented treatment consisting of 14 group sessions, each with a specific goal and skill to teach. The interventionist also meets with each student individually at the midpoint of the intervention duration to assess progress and determine whether adjustments to intervention goals should be made. TFC/MMTT does not include a parental participation component. A strength of the TFC/MMTT program is that it is designed to be adapted for different age levels. The authors of the program initially developed two different manuals—one for elementary students and one of middle/high school age students. In revising the manual, the two manuals were integrated, with different recommendations and guidelines based on developmental levels provided within each session (Amaya-Jackson et al., 2003). The strength of the evidence available for TFC/MMTT includes a multiple baseline design conducted in schools across settings and time (see March, Amaya-Jackson, Murray, & Schulte, 1998), and Amaya-Jackson et al. (2003) evaluated participants engaged in the intervention but did not have a control group. See Table 2.
Summary of Interventions
Of the studies included in Table 2, each measured outcomes in psychosocial domains such as depression, anxiety, and emotional regulation. All of these studies were successful in improvement of functioning in students with exposure to a wide variety of traumatic events. Other than measuring teacher-rated behavior problems (Jaycox et al., 2009, 2010; Stein et al., 2003), studies evaluating the efficacy of CBITS, Bounce Back, MATCH, or TFC/MMTT examined few outcomes related to other school-related factors such as academic achievement, regular school attendance, or discipline. Documented relationships between trauma and these areas exist (Perfect et al., 2016), suggesting that future research includes more robust inclusion of school-related outcomes in addition to psychosocial domains, particularly for school-based projects in which standardized testing, attendance, and discipline data may be readily accessible.
In Table 3, we have separated information about the interventions based on age ranges with demonstrated effects. As noted, many of the CBT-focused, school-based interventions demonstrate effectiveness across developmental levels, although there are few options for preschool-aged children. The lower end of the age range for the Bounce Back intervention is 5 years and thus could have potential for older preschool students if the language is appropriately adjusted to account for developmental level. However, it should be noted that although the Bounce Back intervention is designed for grades K-5, no kindergarteners were included in the study evaluating the efficacy of Bounce Back; the youngest students were in first grade (Langley et al., 2015). The systematic review conducted by Jaycox et al. (2006) found that the only intervention that showed “promising” results for preschool is TF-CBT. As previously stated, given the family involvement required for implementation of TF-CBT, this intervention choice may not always be feasible for school-based practitioners. Further investigation as to the efficacy of school-based trauma-based interventions for the preschool level is needed. Taken together, the summary tables might be used in combination with Table 1 checklist to inform decisions about choice of a particular trauma-specific intervention.
Recommendations for School Mental Health Providers
With regard to trauma-specific intervention delivery, recent guidelines were released to outline expectations for specific training or basic competencies expected of any person engaging in trauma-specific intervention delivery, which includes those working in school-based delivery. Specifically, the 2015 NCTSN position statement outlines expected areas of clinical competency, at a minimum, in order to deliver an NCTSN-endorsed trauma-specific intervention. Broadly, those competencies include skills in assessment (general and risk specific), case conceptualization, and treatment planning, engagement, implementation, and quality monitoring.
In addition, the 2016 NCTSN document on reviewing and selecting interventions provides helpful guidelines that apply to school-based delivery of trauma-specific interventions. A first step includes ensuring review of not only the available evidence for an intervention, but evaluation in consideration of the appropriateness for the intended problem and desired outcomes as well as the population to be served. For example, identification of the type of traumatic event and the level of need for an intervention is needed—such as immediate crisis intervention for a larger community population versus an intervention for individuals who have experienced chronic and persistent levels of abuse. Part of identification and need may include consideration as to how best to identify which students should participate in a school-based trauma-specific intervention; for example, one option may include use of a screening measure to evaluate exposure to or negative response to traumatic events. Although beyond the scope of this review, many factors should be considered when choosing to implement a trauma screening measure, see Eklund et al. (in press) for a full review. Related to both assessment and intervention identification, consideration of use and related evidence for intended developmental levels is important. A second step involves consideration of the fit for the intended service delivery setting as well as broader community. For example, factors such as the local culture and values in the community, settings available for service delivery and other resources that might be leveraged, training and other logistical requirements are essential considerations in planning, adoption, and maintenance. School mental health providers are encouraged to engage in direct and indirect assessment of key intervention usability factors, such as acceptability, feasibility, understand, homeschool collaboration, system climate, and system support (Briesch, Chafouleas, Neugebauer, & Riley-Tillman, 2013). As previously noted, another step involves consideration of the clinical competencies of the intended provider. Finally, the match between the presenting situation and various core components in trauma-specific interventions is needed. And as previously summarized, given substantial overlap in content and approach across existing trauma-specific interventions, the NCTSN (2016) provides a list of core components to consider, separated by intervention objectives and practice elements (see Table 1).
In summary, directions in who, what, where, when, and for how long regarding trauma-specific intervention for individual students are established, and general guidelines for mental health providers are available. Further work is needed to fully understand how best to deliver school-based services at all possible points for intervention (see Table 1). For example, extension of knowledge of mental health providers to professional development and training for school personnel is not fully complete, leaving understanding of procedures that can be proactively deployed across students, classrooms, and schools within a district underdeveloped. Using guiding principles from SAMHSHA (2014) for a trauma-informed approach, a multi-tiered framework for service delivery in schools has been recommended (Chafouleas et al., 2016) in which the focus is on (a) strategies to build positive adaptive systems for all students, (b) incorporating strategies that address psychoeducation about trauma and its impact, reinforcing social support systems, and strengthening self-regulation skills for targeted (at-risk) students, and (c) trauma-specific interventions for select (identified) students. Professional development resources for all school personnel intended to increase awareness and understanding of the impact of trauma on student learning and health (aka “Trauma 101/102”), provide strategies to decrease triggers in the classroom and avoid student re-traumatization, and increase engagement in adult self-care have burgeoned, yet evidence to fully understand the short- and long-term impact on relevant school outcomes is just beginning to emerge. Despite the nascent state of the current evidence for school-relevant impact, the work to date across the country supports interest and engagement in school settings as a critical system for prevention and early intervention of trauma (Overstreet & Chafouleas, 2016), thus providing encouragement that the evidence and ensuing best practice recommendations will be more fully developed within the next decade.
Future Directions
The evidence base for trauma-specific interventions in schools is growing, but many questions remain regarding how best to integrate these interventions into the school setting and to document their impact on school-relevant outcomes. Even larger questions loom when considering the expansion from trauma-specific interventions to trauma-informed approaches that may have the potential to impact the entire school system (Overstreet & Chafouleas, 2016). With acknowledgement of the current status of evidence, we offer recommendations to expand the literature on trauma-specific interventions and trauma-informed approaches at the student and then school and district level.
Trauma-Specific Interventions
As the prevalence and impact of childhood trauma has become increasingly understood (see Perfect et al., 2016, for a review), schools have responded by providing access to trauma-specific treatments. Compelling evidence suggests that when such treatments are provided in schools, students are more likely to complete treatment and demonstrate significant reductions in traumatic stress symptoms (Jaycox et al., 2010; Rolfsnes & Idsoe, 2011). However, much less is known about the impact of trauma-specific treatments on educationally oriented outcomes, such as academic engagement, achievement, and social relationships. In one of the only studies to examine academic performance among students who participated in a school-based trauma treatment, Kataoka et al. (2011) provide important preliminary evidence for a positive impact on grades.
The impact of trauma-specific treatments on academic outcomes is relevant to increase the likelihood that access to intervention in schools is sustained over time (Kataoka et al., 2011; Nadeem & Ringle, 2016). Aligning trauma-specific treatments with the educational missions of school is critical to sustainment of a trauma-informed approach (Nadeem & Ringle, 2016), which includes articulation as to how a trauma-informed approach that includes both trauma-sensitive and trauma-specific practices fits with other initiatives that support student success. Several qualitative studies have identified potentially important factors for the sustainability of trauma-specific treatments in schools beyond demonstrating an impact of the treatments on academic outcomes (Baweja et al., 2016; Langley et al., 2010; Nadeem & Ringle, 2016). For example, Langley et al. (2010) found that teachers who perceived the benefits of trauma-specific treatments were less reluctant to let their students leave class to participate in the intervention. In addition, Baweja et al. (2016) highlight the importance of teacher–clinician consultation as an element of trauma-specific treatments. Consultation may allow teachers to be more invested in the trauma-specific treatment as well as be more capable of managing the behaviors of trauma-exposed students in their classroom, resulting in increased teacher engagement and a more positive classroom environment. Future research should examine whether expansion of treatment models to include teacher training in trauma and teacher–clinician consultation lead to increased teacher buy-in and sustainability of trauma-focused treatments.
There is also a need to identify moderators and mediators of school-based trauma intervention effects, such as intervention components and approaches, developmental level of the child, amount of training provided to the clinician, and dosage. Understanding what accounts for differences in treatment effects and what works best for which children and adolescents will aid in providing the best care for youth struggling with trauma symptoms at school. Finally, few interventions included in these reviews focused on treating childhood trauma associated with neglect and household challenges, such as parental absence or family discord. Often more chronic in nature, these types of events can pose some of the greatest threats to child development and are often commonly experienced by entire populations of youth developing in contexts of persistent poverty. Thus, development of innovative school-based interventions that take a more universal approach to the treatment of chronic stressors may be warranted.
Trauma-Informed Approaches at the Whole School Level
Although several models outline core components and implementation processes for the development of trauma-informed schools (see Chafouleas et al., 2016, for a review), empirical studies have yet to identify factors that lead to the adoption, successful implementation, and sustainment of comprehensive trauma-informed approaches. Furthermore, aside from preliminary data from case studies (e.g., Dorado, Martinez, McArthur, & Leibovitz, 2016), little is known about whether the educational workforce finds trauma-informed approaches acceptable and feasible. Given the rapid push for expansion of trauma-sensitive schools (Overstreet & Chafouleas, 2016), there is a critical need for rigorous research on implementation processes to identify cost-efficient and effective strategies for the adoption and implementation of trauma-informed approaches by schools. A critical opportunity for future work is to establish a crosswalk that aligns related initiatives in supporting student social, emotional, and behavioral success so that a trauma-informed approach is not simply viewed as an add-on to the workload or a temporary initiative. Early reports from uncontrolled studies of trauma-informed schools have reported drastic reductions in suspensions and office referrals (Dorado et al., 2016; Stevens, 2012). However, as noted by Overstreet and Chafouleas (2016), it is not clear: (a) what specific elements of the trauma-informed schools may have contributed to those changes, (b) what short-term outcomes (e.g., changes in classroom management approaches, changes in school discipline policies, changes in student functioning) may have served as precursors to those changes, or (c) whether there are other long-term outcomes that could be expected. As researchers consider long-term outcomes, it will be critical to include teacher and school outcomes, in addition to student outcomes. For example, with an increased understanding of trauma and its effects, teachers may be challenged by secondary traumatic stress, which is characterized by emotional disturbances that often manifest when working with trauma-exposed populations (Figley & Kleber, 1995).
In summary, available resources and supporting evidence for addressing the needs of trauma-exposed students in schools is growing, with established trauma-specific interventions targeted toward individual students experiencing negative symptoms and promising trauma-informed approaches for the entire school that address other points for intervention More research is needed to refine our knowledge on the best implementation approaches, to link our interventions to academic outcomes, and to understand how to sustain these efforts over time.
References
Amaya-Jackson, L., Reynolds, V., Murray, M. C., McCarthy, G., Nelson, A., Cherney, M. S., et al. (2003). Cognitive-behavioral treatment for pediatric posttraumatic stress disorder: Protocol and application in school and community settings. Cognitive and Behavioral Practice, 10, 204–213. https://doi.org/10.1016/S1077-7229(03)80032-9.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., et al. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. https://doi.org/10.1007/s00406-005-0624-4.
Baweja, S., Santiago, C. D., Vona, P., Pears, G., Langley, A., & Kataoka, S. (2016). Improving implementation of a school-based program for traumatized students: Identifying factors that promote teacher support and collaboration. School Mental Health, 8, 120–131.
Blaustein, M. (2013). Childhood trauma and a framework for intervention. In E. Rossen & R. Hull (Eds.), Supporting and educating traumatized students: A guide for school-based professionals (pp. 3–21). New York, NY: Oxford University Press.
Briesch, A. M., Chafouleas, S. M., Neugebauer, S. R., & Riley-Tillman, T. C. (2013). Assessing influences on intervention use: Revision of the usage rating profile-intervention. Journal of School Psychology, 51, 81–96. https://doi.org/10.1016/j.jsp.2012.08.006.
Brock, S. E., Reeves, M. A. L., & Nickerson, A. B. (2014). Best practices in school crisis intervention. In P. Harrison & A. Grimes (Eds.), Best practices in school psychology: System level services (6th ed., pp. 211–230). Bethesda, MD: National Association of School Psychologists.
Burke, N. J., Hellman, J. L., Scott, B. G., Weems, C. F., & Carrion, V. G. (2011). The impact of adverse childhood experiences on an urban pediatric population. Child Abuse and Neglect, 35, 408–413. https://doi.org/10.1016/j.chiabu.2011.02.006.
Chafouleas, S., Johnson, A., Overstreet, S., & Santos, N. (2016). Toward a blueprint for trauma-informed service delivery in schools. School Mental Health, 8, 144–162.
Chorpita, B. F., & Weisz, J. R. (2009). Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems (MATCH-ADTC). Satellite Beach, FL: PracticeWise, LLC.
Chorpita, B. F., Weisz, J. R., Daleiden, E. L., Schoenwald, S. K., Palinkas, L. A., Miranda, J., et al. (2013). Long-term outcomes for the Child Steps randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology, 81(6), 999–1009. https://doi.org/10.1037/a0034200.
Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2006). Treating trauma and traumatic grief in children. New York: Guilford Press.
Cole, S. F., Eisner, A., Gregory, M., & Ristuccia, J. (2013). Creating and advocating for trauma-sensitive schools. Massachusetts Advocates for Children. Retrieved from http://www.traumasensitiveschools.com.
Copeland, W. E., Keeler, G., Angold, A., & Costello, E. J. (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64, 577–584.
De Bellis, M. D., Hooper, S. R., Spratt, E. G., & Woolley, D. P. (2009). Neuropsychological findings in childhood neglect and their relationships to pediatric PTSD. Journal of the International Neuropsychological Society, 15, 868–878. https://doi.org/10.1017/S1355617709990464.
De Bellis, M. D., Woolley, D. P., & Hooper, S. R. (2013). Neuropsychological findings in pediatric maltreatment: Relationship of PTSD, dissociative symptoms, and abuse/neglect indices to neurocognitive outcomes. Child Maltreatment, 18, 171–183. https://doi.org/10.1177/1077559513497420.
Dorado, J., Martinez, M., McArthur, L., & Leibovitz, T. (2016). Health environments and response to trauma in schools (HEARTS): A school based, multi-level comprehensive prevention and intervention program for creating trauma-informed, safe, and supportive schools. School Mental Health, 8, 163–176.
Dorsey, S., Mclaughlin, K. A., Kerns, S. E. U., Harrison, J. P., Lambert, H. K., Briggs, E. C., et al. (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology, 46, 303–330. https://doi.org/10.1080/15374416.2016.1220309.
Eckenrode, J., Laird, M., & Doris, J. (1993). School performance and disciplinary problems among abused and neglected children. Developmental Psychology, 29, 53–62.
Eckenrode, J., Rowe, E., Laird, M., & Brathwaite, J. (1995). Mobility as a mediator of the effects of child maltreatment on academic performance. Child Development, 66, 1130–1142.
Eklund, K., Rossen, E., Koriakin, T., & Chafouleas, S. M. (in press). A systematic review of trauma screening measures for children and adolescents. School Psychology Quarterly.
Fantuzzo, J. W., Perlman, S. M., & Dobbins, E. K. (2011). Types and timing of child maltreatment and early school success: A population-based investigation. Children and Youth Services Review, 33, 1404–1411. https://doi.org/10.1016/j.childyouth.2011.04.010.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8.
Figley, C. R., & Kleber, R. (1995). Beyond the “victim”: Secondary traumatic stress. In R. Kleber, C. R. Figley, & B. P. R. Gersons (Eds.), Beyond trauma: Cultural and societal dynamics (pp. 75–709). NY: Plenum.
Fitzgerald, M. M., & Cohen, J. A. (2012). Trauma-focused cognitive behavior therapy for school psychologists. Journal of Applied School Psychology, 28(3), 294–315. https://doi.org/10.1080/15377903.2012.696037.
Gonzalez, A., Monzon, N., Solis, D., Jaycox, L., & Langley, A. K. (2016). Trauma exposure in elementary school children: Description of screening procedures, prevalence of exposure, and posttraumatic stress symptoms. School Mental Health. https://doi.org/10.1007/s12310-015-9167-7.
Goodkind, J. R., LaNoue, M. D., & Milford, J. (2010). Adaptation and implementation of cognitive behavioral intervention for trauma in schools with American Indian youth. Journal of Clinical Child and Adolescent Psychology, 39, 858–872. https://doi.org/10.1080/15374416.2010.517166.
Hurt, H., Malmud, E., Brodsky, N. L., & Giannetta, J. (2001). Exposure to violence: Psychological and academic correlates in child witnesses. Archives of Pediatrics and Adolescent Medicine, 155, 1351–1356. https://doi.org/10.1001/archpedi.155.12.1351.
Jaycox, L. H., Cohen, J. A., Mannarino, A. P., Walker, D. W., Langley, A. K., Gegenheimer, K. L., et al. (2010). Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress, 23, 223–231. https://doi.org/10.1002/jts.20518.
Jaycox, L. H., Kataoka, S. H., Stein, B. D., Langley, A. K., & Wong, M. (2012). Cognitive behavioral intervention for trauma in schools. Journal of Applied School Psychology, 28, 239–255. https://doi.org/10.1097/CHI.0b013e3181799f19.
Jaycox, L. H., Langley, A. K., Stein, B. D., Wong, M., Sharma, P., Scott, M., et al. (2009). Support for students exposed to trauma: A pilot study. School Mental Health, 1, 49–60.
Jaycox, L. H., Morse, L. K., Tanielian, T., & Stein, B. D. (2006). How schools can help students recover from traumatic experiences: A toolkit for supporting long-term recovery. Retrieved from http://www.rand.org/content/dam/rand/pubs/technical_reports/2006/RAND_TR413.pdf.
Kataoka, S., Jaycox, L. H., Wong, M., Nadeem, E., Langley, A., Tang, L., et al. (2011). Effects on school outcomes in low-income minority youth: Preliminary findings from a community-partnered study of a school trauma intervention. Ethnic Disparities, 21(S1), 71–77.
Kataoka, S. H., Stein, B. D., Jaycox, L. H., Wong, M., Escudero, P., Tu, W., et al. (2003). A school-based mental health program for traumatized Latino immigrant children. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 311–318. https://doi.org/10.1097/00004583-200303000-00011.
Langley, A. K., Gonzalez, A., Sugar, C. A., Solis, D., & Jaycox, L. (2015). Bounce back: Effectiveness of an elementary school-based intervention for multicultural children exposed to traumatic events. Journal of Consulting and Clinical Psychology, 83(5), 853–865. https://doi.org/10.1037/ccp0000051.
Langley, A., Nadeem, E., Kataoka, S., Stein, B. D., & Jaycox, L. H. (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2, 105–113.
Lansford, J. E., Dodge, K. A., Pettit, G. S., Bates, J. E., Crozier, J., & Kaplow, J. (2002). A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrics and Adolescent Medicine, 156, 824–830. https://doi.org/10.1001/archpedi.156.8.824.
March, J. S., Amaya-Jackson, L., Murray, M. C., & Schulte, A. (1998). Cognitive-behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. Journal of the American Academy of Child and Adolescent Psychiatry, 37(6), 585–593. https://doi.org/10.1097/00004583-199806000-00008.
Mathews, T., Dempsey, M., & Overstreet, S. (2009). Effects of exposure to community violence on school functioning: The mediating role of posttraumatic stress symptoms. Behaviour Research and Therapy, 47, 586–591. https://doi.org/10.1016/j.brat.2009.04.001.
Morsette, A., Swaney, G., Stolle, D., Schuldberg, D., van den Pol, R., & Young, M. (2009). Cognitive behavioral intervention for trauma in schools (CBITS): School-based treatment on a rural American Indian reservation. Journal of Behavior Therapy and Experimental Psychiatry, 40, 169–178. https://doi.org/10.1016/j.jbtep.2008.07.006.
Morsette, A., van den Pol, R., Schuldberg, D., Swaney, G., & Stolle, D. (2012). Cognitive behavioral treatment for trauma symptoms in American Indian youth: Preliminary findings and issues in evidence-based practice and reservation culture. Advances in School Mental Health Promotion, 5, 51–62. https://doi.org/10.1080/1754730X.2012.664865.
Nadeem, E., & Ringle, V. A. (2016). De-adoption of an evidence-based trauma intervention in schools: A retrospective report from an urban school district. School Mental Health, 8, 132–143.
National Child Traumatic Stress Network. (2015). National child traumatic stress network position statement: Prerequisite clinical competences for implementing effective, trauma-informed interventions. Retrieved from http://www.nctsn.org/sites/all/modules/pubdlcnt/pubdlcnt.php?file=http://nctsn.org/sites/default/files/assets/pdfs/nctsn_position_statement_on_clinical_competency.pdf&nid=1771.
National Child Traumatic Stress Network. (2016). National child traumatic stress network empirically supported treatments and promising practices. Retrieved from http://www.nctsn.org/resources/topics/treatments-that-work/promising-practices.
Nooner, K., Linares, O., Batinjane, J., Kramer, R., Silva, R., & Cloitre, M. (2012). Factors related to posttraumatic stress disorder in adolescence. Trauma, Violence, & Abuse, 13, 153–166.
Overstreet, S., & Chafouleas, S. M. (2016). Introduction to the special issue. School Mental Heath, 8, 1–6.
Perfect, M. M., Turley, M. R., Carlson, J. S., Yohanna, J., & Saint Gilles, M. P. (2016). School-related outcomes of traumatic event exposure and traumatic stress symptoms in students: A systematic review of research from 1990 to 2015. School Mental Health, 8, 7–43. https://doi.org/10.1007/s12310-016-9175-2.
Porche, M. V., Costello, D. M., & Rosen-Reynoso, M. (2016). Adverse family experiences, child mental health, and educational outcomes for a national sample of students. School Mental Health. https://doi.org/10.1007/s12310-016-9174-3.
Rolfsnes, E. S., & Idsoe, T. (2011). School-based intervention programs for PTSD symptoms: A review and meta-analysis. Journal of Traumatic Stress, 24, 155–165. https://doi.org/10.1002/jts.20622.
Saigh, P. A., Mroueh, M., & Bremner, J. D. (1997). Scholastic impairments among traumatized adolescents. Behaviour Research and Therapy, 35, 429–436. https://doi.org/10.1016/S0005-7967(96)00111-8.
Shonk, S. M., & Cicchetti, D. (2001). Maltreatment, competency deficits, and risk for academic and behavioral maladjustment. Developmental Psychology, 37, 3–17. https://doi.org/10.1097//0212-1649.37.1.3.
Stein, B. D., Jaycox, L. H., Kataoka, S. H., Wong, M., Tu, W., Elliott, M. N., et al. (2003). A mental health intervention for schoolchildren exposed to violence: A randomized controlled trial. Journal of the American Medical Association, 290, 603–611. https://doi.org/10.1001/jama.290.5.603.
Stevens, J. E. (2012). Lincoln High School in Walla Walla, WA tries new approach to school discipline—Suspensions drop 85%. ACEs Too High. Retrieved from http://acestoohigh.com/2012/04/23/Iincoln-high-schooI-in-waIla-walia-wa-tries-new-approach-toschool-discipline-expulsions-drop-85/.
Substance Abuse and Mental Health Services Administration. (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach (HHS Publication No. 14-4884). Retrieved from http://store.samhsa.gov/shin/content/SMA14-4884/SMA14-4884.pdf.
Weisz, J. R., Chorpita, B. F., Palinkas, L. A., Schoenwald, S. K., Miranda, J., Bearman, S. K., et al. (2012). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry, 69, 274–282. https://doi.org/10.1001/archgenpsychiatry.2011.147.
Wodarski, J. S., Kurtz, P. D., Gaudin, J. M., & Howing, P. T. (1990). Maltreatment and the school-age child: Major academic, socioemotional, and adaptive outcomes. Social Work, 35(6), 506–513. https://doi.org/10.1093/sw/35.6.506.
Woodbridge, M. W., Sumi, W. C., Thornton, S. P., Fabrikant, N., Rouspil, K. M., Langley, A. K., et al. (2016). Screening for trauma in early adolescence: Findings from a diverse school district. School Mental Health, 8, 89–105. https://doi.org/10.1007/s12310-015-9169-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chafouleas, S.M., Koriakin, T.A., Roundfield, K.D. et al. Addressing Childhood Trauma in School Settings: A Framework for Evidence-Based Practice. School Mental Health 11, 40–53 (2019). https://doi.org/10.1007/s12310-018-9256-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12310-018-9256-5