Abstract
Surgery has dramatically improved survival of infants with esophageal atresia. However, early and late complications of these surgeries affect the future life of this population. A probable step toward minimizing such complications is through modifying the technique of surgery. We evaluated two groups of esophageal atresia undergoing surgery with two different techniques including preservation and ligation of the Azygos vein and compared early complications, duration of surgery, and hospital and neonatal intensive care unit (NICU) stay between them. A total number of 24 patients with mean age of 24 to 48 h, who were diagnosed with esophageal atresia, were included in the study. All cases were randomly allocated in two groups: group A (case group) in which patients underwent surgery with preservation of the Azygos vein and group B (control group) in which patients underwent the former surgical method with ligation of the Azygos vein. Incidence of early complications, duration of surgery, and NICU and hospital stay were compared between the two groups. None of the complications occurred in either group. Duration of surgery, NICU stay, and hospital stay were not statistically significant between the groups. Preserving the Azygos vein during esophageal atresia surgery is probably a good modification of the classic technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tracheoesophageal fistula (TEF)—defined as complete disruption in the continuity of the esophagus—is a relatively common congenital condition affecting about 1 in every 3,000 to 4,000 live births [1, 2]. This condition is treated surgically usually on the first or second day of life. The site of entrance is usually the right fourth intercostal space, and the extrapleural approach is the method of choice for entering the thoracic space. Then, the Azygos vein is ligated and anastomosis is done [3, 4]. This technique of surgery has dramatically improved the survival of infants with this condition [1]. However, early [5, 6] and late complications [7–9] affect the future life of this population. A probable step toward minimizing such complications is through modifying the technique of surgery.
In a study published in 2007, the preservation of the Azygos vein during surgery in patients with esophageal atresia and TEF resulted in significant reduction in the number of postoperative anastomotic leaks [10]. In another study, reduction in the rate of postoperative pneumonitis was observed with preservation of the Azygos vein after surgery for TEF [11]. Additionally, pathology in the veins draining cerebrospinal fluid such as the Azygos vein can lead to chronic cerebrospinal venous insufficiency. This condition has been proposed to be associated with the development of multiple sclerosis in recent studies [12–14].
Since the Azygos vein is one of the main parts of the venous system in the human body [10, 11], preserving it is a goal for surgeons. Here, we aim to study the outcome of the primary repair of TEF with and without Azygos vein ligation and compare early complications, duration of surgery, and hospital and NICU stay between them.
Materials and Method
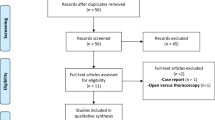
This is a randomized clinical trial which was performed from August 2009 till 2011 at the pediatric center of Mashhad Hospital. A total number of 24 patients aged between 24 and 48 h and who were diagnosed with type III esophageal atresia without other associated congenital anomalies were included in the study. Informed consent was obtained from the patient's parent or guardian. All cases were randomly allocated into the two groups defined as A and B. Randomization was performed using randomized cards and numbers. Group A (case group) consisted of 12 cases that underwent surgery with preservation of the Azygos vein, and group B (control group) consisted of 12 cases that underwent surgery without preservation of the Azygos vein.
Surgical technique was the same as described in the Kinottenbelt et al. study [15] and was performed by the same surgeon in all cases. All patients were under close supervision in the neonatal intensive care unit (NICU) for about 48 h and were followed for about 1 week in hospital after surgery. Ultrasonography, duplex scanning of neck and vertebral vasculature, and two chest X-rays in the first and second days after surgery were performed to control postoperative complications in neonates. Incidence of anastomosis leakage, hemorrhage, and infection; duration of surgery; and NICU and hospital stay were compared between the two groups.
Statistical Analysis
Quantitative data were described by mean ± SD, and qualitative data were described by absolute frequency (percentage). Measured variables were compared using Chi-square and T tests. SPSS version 18 software was applied for statistical analysis. The power of the study was 0.38, calculated using independent sample t test.
Results
During our study, 24 neonates with esophageal atresia were assigned into two groups of case and control (each 12 cases). In group B, the mean age of patients was 34.66 ± 7.49 h with a 6:6 F/M ratio. The weight of patients in this group was 2,224.16 ± 382.46 g. The age and weight of patients in group A was 36.25 ± 7.42 h and 2,359.16 ± 708.67 g, respectively. F/M ratio was 7:5 in this group. Duration of surgery was 60.33 ± 11.45 min in group B and 60.41 ± 5.14 min in group A. None of the assessed complications occurred in each group. Incidence of complications and duration of NICU and hospital stay besides statistical comparisons are summarized in Table 1. None of the assessed factors was significantly different between the two groups.
Discussion
Here, we compared two TEF surgery techniques including Azygos vein preservation and Azygos vein ligation during surgery. Incidence of postoperative infection, hemorrhage, and anastomosis leakage was compared between the two groups. Duration of surgery, NICU stay, and hospital stay were also compared between the two groups. None of the mentioned factors was different between the two groups.
In a similar study by Sharma et al., two groups of about 50 patients with esophageal atresia were selected and were planned for surgery. In one group, the Azygos vein was spared while in the other group, it was ligated. Finally, incidence of anastomosis leakage was significantly lower in patients with spared Azygos vein. A larger size of the study population probably provided a better chance for capturing occurrence of this complication in this study in comparison with our study [10]. In another study by Upadhyayaet al., a similar comparison was performed between two groups of babies with esophageal atresia. A total number of 50 patients were divided into two equal-sized groups. In the group with preservation of the Azygos vein, the rate of postoperative pneumonitis was significantly lower, and they had more stable hemodynamic condition after surgery [11]. In our study, none of the complications occurred in either group. Duration of surgery and NICU and hospital stay were not significantly different between the two groups. These results show that preserving the Azygos vein adds no harm in patients who undergo surgery for esophageal atresia.
Chronic cerebrospinal venous insufficiency, which was first described by Zamboni et al. in 2009 [13], is a syndrome characterized by stenosis of the internal jugular and/or Azygos veins and formation of collateral venous channels. Some studies have shown that prevalence of this condition has been higher in patients with multiple sclerosis using duplex scanning [14, 16–18], while some other studies have shown absence of such an association [19, 20]. In conclusion, the presence of an association between extracranial venous outflow abnormality and development and course of multiple sclerosis is probable.
Since the Azygos vein is a functional important part of the venous system in the human body, it is rational to recommend preserving this vein during surgery for esophageal atresia. Benefits from preserving this vein, which were shown in two mentioned studies, make this modification more favorable in future surgeries. If the hypothesis [12–14] about the association between multiple sclerosis and dysfunction in the venous drainage system of cerebrospinal fluid is correct, it can also emphasize the preservation of the Azygos vein which is naturally a part of this system. The comparable small sample sizes in our study made our judgment about incidence of complications less reliable. But regarding the results of this study and previous similar studies, it seems that preserving the Azygos vein during surgery for esophageal atresia is probably a good modification of the classic technique of surgery.
The principal limitations of the present study were its short-term follow-up duration, small sample size, and low power of study which preclude generalization of the results. Considering these limitations, future case–control studies with larger sample size and longer follow-up are warranted to confirm the results of our study.
References
Goyal A, Jones MO, Couriel JM, Losty PD (2006) Oesophageal atresia and tracheo–oesophageal fistula. Arch Dis Child Fetal Neonatal Ed 91:381–384
Spitz L (2007) Oesophageal atresia. Orphanet J Rare Dis 2:24
Foker JE, Linden BC, Boyle EM Jr, Marquardt C (1997) Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg 226:533–543
Karnak I, Senocak ME, Hiçsönmez A, Büyükpamukçu N (1997) The diagnosis and treatment of H-type tracheoesophageal fistula. J Pediatr Surg 32:1670–1674
Spitz L (2006) Esophageal atresia. Lessons I have learned in a 40-year experience. J Pediatr Surg 41:1635–1640
Konkin DE, O’Hali WA, Webber EM, Blair K (2003) Outcomes in esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 38:1726–1729
Tomaselli V, Volpi ML, Dell'Agnola CA, Bini M, Rossi A, Indriolo A (2003) Long-term evaluation of esophageal function in patients treated at birth for esophageal atresia. Pediatr Surg Int 19:40–43
Little DC, Rescorla FJ, Grosfeld JL, West KW, Scherer LR, Engum SA (2003) Long-term analysis of children with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 38:852–856
Sistonen SJ, Pakarinen MP, Rintala RJ (2011) Long-term results of esophageal atresia: Helsinki experience and review of literature. Pediatr Surg Int 27:1141–1149
Sharma S, Sinha SK, Rawat JD, Wakhlu A, Kureel SN, Tandon R (2007) Azygos vein preservation in primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 23:1215–1218
Upadhyaya VD, Gangopadhyaya AN, Gopal SC et al (2007) Is ligation of azygos vein necessary in primary repair of tracheoesophageal fistula with esophageal atresia? Eur J Pediatr Surg 17:236–240
Zamboni P, Galeotti R, Weinstock-Guttman B, Kennedy C, Salvi F, Zivadinov R (2012) Venous angioplasty in patients with multiple sclerosis: results of a pilot study. Eur J Vasc Endovasc Surg 43:116–122
Zamboni P, Galeotti R, Menegatti E et al (2009) Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 80:392–399
Simka M, Latacz P, Ludyga T et al (2011) Prevalence of extracranial venous abnormalities: results from a sample of 586 multiple sclerosis patients. Funct Neurol 26:197–203
Kinottenbelt G, Skinner A, Seefelder C (2010) Tracheo-oesophageal fistula (TOF) and oesophageal atresia (OA). Best Pract Res Clin Anaesthesiol 24:387–401
Zivadinov R, Marr K, Cutter G et al (2011) Prevalence, sensitivity, and specificity of chronic cerebrospinal venous insufficiency in MS. Neurology 77:138–144
Al-Omari MH, Rousan LA (2010) Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis. Int Angiol 29:115–120
Simka M, Kostecki J, Zaniewski M, Majewski E, Hartel M (2010) Extracranial Doppler sonographic criteria of chronic cerebrospinal venous insufficiency in the patients with multiple sclerosis. Int Angiol 29:109–114
Doepp F, Paul F, Valdueza JM, Schmierer K, Schreiber SJ (2010) No cerebrocervical venous congestion in patients with multiple sclerosis. Ann Neurol 68:173–183
Baracchini C, Perini P, Calabrese M, Causin F, Rinaldi F, Gallo P (2011) No evidence of chronic cerebrospinal venous insufficiency at multiple sclerosis onset. Ann Neurol 69:90–99
Acknowledgments
The authors would like to thank Farzan Science, Research & Technology Institute for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fathi, M., Joudi, M. & Morteza, A. Evaluating Necessity of Azygos Vein Ligation in Primary Repair of Esophageal Atresia. Indian J Surg 77 (Suppl 2), 543–545 (2015). https://doi.org/10.1007/s12262-013-0917-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-013-0917-1