Abstract
Esophageal atresia-tracheoesophageal fistula (EA-TEF) is one of the common congenital anomalies occurring in newborns. Over the last eight decades, various technical modifications have been proposed in the surgical repair of EA-TEF. Preservation of azygos vein is one such modification that has gained considerable attention. However, a consensus statement regarding the superiority of its preservation over its division is lacking. We aim to compare the outcomes of surgery between the two groups of newborns, i.e., those undergoing repair with and without azygos vein preservation, in terms of its complications. The authors systematically searched the databases PubMed, EMBASE, Web of Science, and Scopus through December 2020. The incidence of anastomotic complications and chest infection was compared among the two groups of newborns, i.e., those undergoing surgical repair with (group A) and without azygos vein preservation (group B). Statistical analysis was performed using a fixed-effects model, and pooled risk ratio (RR) and heterogeneity (I2) were calculated. The methodological quality of the studies was assessed using the Downs and Black scale. Six comparative studies, consisting of a total of 671 newborns, were included in the meta-analysis. As compared to group B, newborns belonging to group A showed a significantly lower incidence of pneumonitis in the postoperative period (RR 0.31; 95% CI 0.17–0.57, p = 0.0001). However, no significant difference in the incidence of anastomotic complications including anastomotic leak (RR 0.73; 95% CI 0.48–1.12, p = 0.15) and stricture (RR 0.63; 95% CI 0.36–1.09, p = 0.10) was observed between the two groups. The average Downs and Black scale scores ranged from 20 to 24. The risk of bias was low (n = 1) and moderate (n = 5) in the included studies. Kappa statistics showed a value of 0.902 (p < 0.001), highlighting an almost perfect agreement among the two observers. The present meta-analysis revealed the superiority of surgical repair of EA-TEF performed with preservation of azygos vein in terms of the incidence of postoperative chest infection. However, no significant difference in the occurrence of anastomotic leak and stricture was observed between the two groups. The level of evidence of the published comparative studies is limited. Therefore, well designed, randomized controlled trial utilizing a standardized operative approach on a larger sample-size needs to be conducted for optimal comparison between the two approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal atresia-tracheoesophageal fistula (EA-TEF) is one of the common congenital anomalies occurring in newborns. The first successful repair of EA-TEF was performed almost eight decades ago [1]. Since then, numerous technical modifications have been introduced by surgeons across the globe. However, the basic principles of this surgery remain unchanged [2]. Some of the common modifications include the utilization of clips/hemlocks for fistula clipping, esophageal repair done without transanastomotic tube, avoidance of chest tube placement in the postoperative period, thoracoscopic assisted primary repair instead of thoracotomy, etc. [2]. Preservation of azygos vein (PV) is yet another modification that has gained considerable attention. It has been demonstrated that newborns undergoing repair with PV are associated with a significantly lower incidence of postoperative complications such as anastomotic leak, pneumonitis, stricture, etc. as compared to those where the azygos vein was divided (DV) [3,4,5]. On the contrary, various other studies have shown no difference in the occurrence of anastomotic complications and chest infection between the two groups [6, 7]. Due to these conflicting results, a consensus statement regarding the superiority of PV over DV is lacking. This systematic review and meta-analysis aims to compare the outcomes of surgery between the two groups of newborns, i.e., those undergoing repair with PV or DV, in terms of its complications. We hypothesize that surgical repair of EA-TEF performed with PV is associated with a lower incidence of chest infection. However, the occurrence of anastomotic complications is multifactorial and should not depend upon whether PV or DV approach was preferred.
Materials and methods
Search strategy and inclusion criteria
An exhaustive preliminary search in the PubMed database was conducted by two authors (DK and SA) independently to identify any published literature on the topic and confirm the absence of any systematic reviews and meta-analysis. Subsequently, both the authors systematically searched the databases PubMed, EMBASE, Web of Science, and Scopus through December 2020. The keywords used were esophageal atresia OR tracheoesophageal fistula OR esophageal atresia-tracheoesophageal fistula OR EA OR TEF OR EA-TEF and azygos vein. Once identified, removal of the duplicates studies was performed. The remaining records were further screened to select the relevant studies highlighting the role of azygos vein preservation in newborns with esophageal atresia-tracheoesophageal fistula (EA-TEF).
Inclusion and exclusion criteria
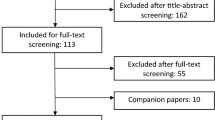
The inclusion criteria were based on: participants: all newborns diagnosed with esophageal atresia-tracheoesophageal fistula (EA-TEF); intervention: preservation of the azygos vein (PV) during operative repair; comparison: patients where the azygos vein was ligated and divided or only ligated or clipped (DV); outcome: the proportion of children developing anastomotic complications such as anastomotic leak and stricture; and proportion of children developing chest infection were assessed separately. The cohort was divided into two groups, i.e., groups A and B included children with PV and DV, respectively. Studies including children with pure esophageal atresia (Type A) or H-type tracheoesophageal fistula (Type E) were excluded. Besides this, those with unavailable full-texts or in which outcomes of interest were not reported were also excluded. The type of operative approach (open or thoracoscopic) was not considered an explicit exclusion criterion. A detailed PRISMA flow diagram of the search strategy is included in Fig. 1.
Data extraction
After the selection of the relevant studies, data extraction was performed by two independent observers (SA and DK). Information on the author, design of the study, year of publication, number of patients per study, and number of patients in each sub-group was extracted along with the data on the abovementioned outcomes in an extraction table using MS Excel (Version 15.24). Any discrepancies among the observers were resolved through consensus and consultation with the senior author (MB).
Quality assessment
The methodological quality of the studies was independently assessed by two observers (SA and AS) utilizing the Downs and Black scale [8]. This hybrid 27-question scale, providing a total score out of 32 points, was adopted to also include non-randomized studies. The risk of bias was categorized as low (score of 24 to 32), moderate (16 to 23), or high (0 to 15). Subsequently, the kappa statistics were used for the measurement of the inter-observer agreement [9]. Based on the kappa values, the level of agreement was defined as almost perfect (0.81–1.00), substantial (0.61–0.80), moderate (0.41–0.60), fair (0.21–0.40), slight (0.00–0.20), and poor (< 0.00).
Statistical analysis
The meta-analysis was performed using RevMan 5.4 (Cochrane Collaboration, London, UK). As all the outcomes were dichotomous, the risk ratio (with 95% CI) was calculated for all of them. The pooled risk ratio was estimated utilizing the Mantel–Haenszel (M–H) method. The I2 statistic was used to estimate the heterogeneity across the included studies. A random-effects model was used if the heterogeneity was significant (I2 > 50%). As per the recommendations of the Cochrane handbook, a funnel plot was drawn when at least ten studies were included in the meta-analysis [10]. A p value of < 0.05 was considered statistically significant.
Results
Study characteristics
A total of 72 studies were identified using the search strategy (Fig. 1). After the removal of the duplications, 56 abstracts were screened. Of these, 45 records were excluded, and only 11 studies were eligible for full-text review. Two of these were excluded as one was a case report and the other had compared two operative approaches (open versus thoracoscopic approach) for the repair of EA-TEF [11, 12]. Nine studies were found relevant and were included in the qualitative synthesis [3,4,5,6,7, 13,14,15,16]. Of these, only six were included in the final meta-analysis (Table 1). The remaining three were excluded due to the absence of a control group [14, 15] and cohort overlap [16]. The study designs of the included studies were randomized clinical trials (n = 3), prospective study (n = 2), and retrospective study (n = 1). A total of 671 subjects, 242 and 429 in groups A and B, respectively, were recruited in the included studies.
The baseline characteristics of the newborns are summarized in Table 1. None of the studies showed a significant difference in the average age or average body weight of newborns among the two groups. Apart from one study [4], no significant difference was observed upon comparing the presence of associated congenital anomalies among the two groups. The information on the gap between the two esophageal ends was presented by four out of six studies [4, 5, 7, 13], and showed no significant difference between the two groups.
Methodological quality assessment
The detailed Downs and Black scoring by the independent observers for each study is depicted in Table 2. The average scores ranged from 20 to 24. The risk of bias was low (n = 1) and moderate (n = 5) in the included studies. Kappa statistics showed a value of 0.902 (p < 0.001), highlighting an almost perfect agreement among the two observers.
Meta-analysis of outcomes
-
a)
Anastomotic leak
All studies reported the incidence of anastomotic leak. The pooled risk ratio (Fig. 2) for the occurrence of leak within group A versus group B was 0.73 (95% CI 0.48–1.12, p = 0.15). The estimated heterogeneity was not significant (p = 0.09; I2 = 51%) for this outcome.
-
b)
Esophageal stricture
The incidence of esophageal stricture was reported by three studies only. The pooled RR (Fig. 3) for stricture within group A compared to group B was 0.63 (95% CI 0.36–1.09, p = 0.10. No significant heterogeneity was observed among the studies for the occurrence of esophageal stricture (p = 0.28; I2 = 22%).
-
c)
Chest infection
A similar selective reporting of the occurrence of chest infection was observed, with only four studies reporting this outcome. The pooled risk ratio (Fig. 4) for chest infection within group A compared to group B was 0.31 (95% CI 0.17–0.57, p = 0.0001). No significant heterogeneity was observed among the studies for the occurrence of chest infection (p = 0.42; I2 = 0%).
Discussion
Following the first successful repair of esophageal atresia-tracheoesophageal fistula (EA-TEF) by Cameron Haight in 1941, numerous technical modifications have been suggested by surgeons across the globe to improve the outcomes [17]. Preservation of the azygos vein (PV) is one such modification that has gained significant attention and has shown interesting results. The azygos vein, formed by the union of right ascending lumbar veins and right subcostal veins, is an essential unpaired vein that connects the superior and the inferior vena cava forming the cavo-caval anastomosis. This venous system (azygos vein and its tributaries) not only drains blood from the bronchus, mediastinum, esophagus, and pericardium; but also receives some collateral lymphatic vessels of the thoracic duct directly [3, 5, 13].
PV has been shown to offer several advantages. First, it maintains the venous drainage of the esophagus [4]. Based on this, it was hypothesized that dividing the azygos vein results in edema and congestion of the esophageal ends, further leading to a higher incidence of anastomotic complications such as leak and stricture. Xu Cui et al. have shown a significantly higher incidence of both these complications in newborns who have undergone azygos vein mutilation [5]. Similarly, Sharma et al. have depicted a significantly higher proportion of postoperative anastomotic leaks in the subset undergoing azygos vein ligation [3]. On the contrary, various studies have demonstrated no significant difference in the occurrence of anastomotic complications among children of both groups [4, 6, 7, 13]. In fact, ligation of the azygos showed no difference in the incidence of anastomotic leak on a regression model [4]. The findings of our meta-analysis reveal a lower incidence of anastomotic complications in newborns belonging to group A. However, the difference could not reach statistical significance. This is because, apart from venous congestion and early tissue edema due to azygos division, several other independent factors are responsible for the occurrence of anastomotic complications. These include anastomosis done under tension, long-gap between the esophageal ends, improper tissue handling, presence of cyanotic heart disease, sepsis, etc. [18]. Hence, PV might reduce the incidence of anastomotic complications, but it is not an independent predictor of the occurrence of these complications.
The second advantage with PV is a significant reduction in the incidence of postoperative pneumonitis or chest infection [4, 13]. Consistent results were observed in the present meta-analysis. Although the exact cause behind this finding is unknown, it is believed that the higher incidence of chest infection in group B is possibly due to a transient impairment in the bronchial function following azygos division. The bronchial veins and capillaries remain congested after azygos arch division, thus contributing to the disruption in the mucociliary function of the mainstem bronchi. However, this effect is transient and lasts till the direction of blood flow is reversed, i.e., the blood finds a downhill course to the inferior vena cava (IVC) [19].
Although further experimental studies are needed to support our hypothesis of transient bronchial dysfunction, previous studies do highlight the occurrence of mediastinal congestion following azygos division [4, 5, 13]. Upadhyaya et al. [13] have demonstrated the trends of cardio-respiratory instability (raised heart rate and respiratory rate) following the surgical repair of EA-TEF. While this instability settled early in newborns belonging to the PV group, the mean heart rate and respiratory rate in the DV group remained elevated till postoperative day 7 due to mediastinal congestion. Therefore, preservation of the azygos vein during thoracic surgeries not only preserves the normal anatomy but offers a major advantage of early restoration of the human physiology in the postoperative period. Lastly, the preserved azygos vein might also reduce the incidence of recurrent tracheoesophageal fistula by preventing the overlap of the esophageal and tracheal suture lines [5].
A systematic review of the available literature was performed for comparison of technical difficulty, operative time, duration of NICU stay, and duration of hospitalization between the two approaches. It was observed that PV neither significantly increased the technical difficulty nor the operative time [3, 6, 7, 13]. Also, apart from the study by Xu Cui et al. [5], no significant differences in the duration of NICU stay, and hospitalization were observed between the two patient groups [3, 6, 13]. However, it must also be noted that all of these variables were selectively reported and need further testing for a comprehensive comparison of the two techniques.
There are few limitations to this meta-analysis. First, the sample size of the included studies was small and the majority of them had a moderate risk of bias. Second, apart from anastomotic leak, a non-uniform reporting of other outcomes was observed among these studies. Chest infection and esophageal stricture were reported by four and three studies, respectively. Third, a similar selective reporting of the baseline details such as associated congenital anomalies, the gap between the esophageal ends, preoperative pulmonary condition, etc. was also observed. At last, it is well-known that numerous factors can affect the surgical outcomes of newborns with EA-TEF. This includes anastomosis done under tension, improper tissue handling, presence of cyanotic heart disease, sepsis, etc. The meta-analysis includes newborns operated by different surgeons under different settings. Therefore, well designed, randomized controlled trial utilizing a standardized operative approach on a larger sample-size needs to be conducted for optimal comparison between the two approaches.
This systematic review and meta-analysis is the first to highlight the impact of preservation of azygos vein during operative repair of EA-TEF, in terms of its complications including anastomotic leak, esophageal stricture, and chest infection. Given the available comparative studies, the level of evidence is limited. The strengths include reporting and external validity while the weaknesses were power and internal validity of the included studies.
Conclusions
The current meta-analysis highlights the superiority of EA-TEF repair performed with preservation of azygos vein in terms of the incidence of postoperative chest infection. However, no significant difference in the occurrence of anastomotic complications including anastomotic leak and stricture was observed between the two approaches. The level of evidence of the published comparative studies is limited. Therefore, well designed, randomized controlled trial utilizing a standardized operative approach on a larger sample-size needs to be conducted for optimal comparison between the two approaches.
References
Foker JE, Linden BC, Boyle EM Jr, Marquardt C (1997) Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg 226:533–543
Iacona RV, Saxena AK (2020) Thoracoscopic repair of esophageal atresia with distal tracheoesophageal fistula (Type C): systematic review. Surg Laparosc Endosc Percutan Tech 30:388–393
Sharma S, Sinha SK, Rawat JD, Wakhlu A, Kureel SN, Tandon R (2007) Azygos vein preservation in primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 23:1215–1218
Soyer T, Öztorun C, Fırıncı B, Durakbaşa ÇU, Bahadır GG, Karaman A et al (2020) The effect of azygos vein preservation on postoperative complications after esophageal atresia repair: results from the Turkish Esophageal Atresia Registry. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2020.12.008 (Epub ahead of print, PMID: 33353739)
Cui X, He Y, Chen L, Lin Y, Wang Y, Zhang J et al (2020) Clinical analysis of azygos vein preservation under thoracoscope in the operation of type III esophageal atresia. J Laparoendosc Adv Surg Tech A 30:448–452
Fathi M, Joudi M, Morteza A (2015) Evaluating necessity of azygos vein ligation in primary repair of esophageal atresia. Indian J Surg 77(Suppl 2):543–545
Rashid KA, Maletha M, Khan TR, Wakhlu A, Rawat J, Kureel SN (2012) Esophageal anastomosis medial to preserved azygos vein in esophageal atresia with tracheoesophageal fistula: restoration of normal mediastinal anatomy. J Neonatal Surg 1:50
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. Available from http://www.training.cochrane.org/handbook. Accessed 11 Mar 2021
Rozeik AE, Elbarbary MM, Saleh AM, Khodary AR, Al-Ekrashy MA (2020) Thoracoscopic versus conventional open repair of tracheoesophageal fistula in neonates: a short-term comparative study. J Pediatr Surg 55:1854–1859
Evans WN, Kogut K, Acherman RJ (2014) Preserving the azygos vein when repairing esophageal atresia and tracheoesophageal fistula accompanied by interrupted inferior vena cava. Pediatr Surg Int 30:345–347
Upadhyaya VD, Gangopadhyaya AN, Gopal SC, Upadhyaya A, Sharma SP, Gupta DK et al (2007) Is ligation of azygos vein necessary in primary repair of tracheoesophageal fistula with esophageal atresia? Eur J Pediatr Surg 17:236–240
Fonte J, Barroso C, Lamas-Pinheiro R, Silva AR, Correia-Pinto J (2016) Anatomic thoracoscopic repair of esophageal atresia. Front Pediatr 4:142
Patkowsk D, Rysiakiewicz K, Jaworski W, Zielinska M, Siejka G, Konsur K et al (2009) Thoracoscopic repair of tracheoesophageal fistula and esophageal atresia. J Laparoendosc Adv Surg Tech A 19(Suppl 1):S19-22
Tandon RK, Sharma S, Sinha SK, Rashid KA, Dube R, Kureel SN et al (2008) Esophageal atresia: factors influencing survival—experience at an Indian tertiary centre. J Indian Assoc Pediatr Surg 13:2–6
Haight C (1944) Congenital atresia of the esophagus with tracheoesophageal fistula: reconstruction of esophageal continuity by primary anastomosis. Ann Surg 120:623–652
Dey S, Jain V, Anand S, Agarwala S, Dhua A, Srinivas M et al (2020) First-year follow-up of newborns operated for esophageal atresia in a developing country: just operating is not enough! J Indian Assoc Pediatr Surg 25:206–212
Sukiara M, Kaneko K, Shinozuka N, Taguchi Y, Omoto R (1990) Hemodynamic changes of azygos venous flow after ligation of the azygos arch. Vasc Surg 24:548–552
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kainth, D., Anand, S., Singh, A. et al. Impact of preservation of the azygos vein during surgical repair of esophageal atresia-tracheoesophageal fistula (EA-TEF): a systematic review and meta-analysis . Pediatr Surg Int 37, 983–989 (2021). https://doi.org/10.1007/s00383-021-04913-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04913-2