Abstract
The aim of this study is to report a series of patients with the Azygos vein preserved during the surgery for esophageal atresia with tracheoesophageal fistula (EA&TEF), highlighting the advantages in terms of survival and prevention of anastomotic leak. Ninety-six neonates with EA&TEF, admitted to the Department of Pediatric Surgery, King George Medical University between 2004 and 2006, were reviewed prospectively; the babies were randomly allocated to two groups: Group A (n = 46) in which the Azygos vein was preserved and Group B (n = 50), wherein it was ligated. The two groups were comparable in respect to sex, weight, prematurity, associated anomalies, Waterston classification, Spitz classification and distance between the pouches after mobilization. Anastomotic leak occurred in three cases (6%) in Group A and ten cases (20%) in Group B and was responsible for mortality in one (2%) case in Group A and six cases (12%) in Group B. Preservation of Azygos vein resulted in significant reduction in the number of anastomotic leaks. We propose that preservation of the Azygos vein prevents early postoperative edema of the esophageal anastomosis by maintaining the venous drainage and thus may form an additional protective factor against anastomotic leaks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal atresia (EA) has been referred to as “the epitome of modern surgery” [1]. Though this condition is now treated successfully all over the world, there is still some morbidity and mortality associated with EA surgery. Anastomotic leak is one of the most significant postoperative complications [2]. In the standard technique for repair of EA and tracheoesophageal fistula (TEF), the Azygos vein is ligated and divided early in the operation. The Azygos vein collects blood from the posterior intercostal veins on the right side, with the exception of the first. It also receives the hemiazygos and accessory hemiazygos veins (draining esophagus) together with several esophageal, mediastinal and pericardial veins [3]. It is our hypothesis that preservation of the Azygos vein would reduce early postoperative edema at the anastomosis and perhaps result in a decreased rate of anastomotic leak in these patients. This report describes the comparison of two randomly operated groups of patients in terms of anastomotic leak; one with preservation of the Azygos vein and the other with ligation of azygos vein, in the surgery for esophageal atresia.
Materials and methods
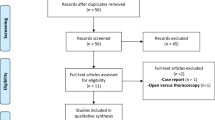
All patients who underwent primary definitive surgery for esophageal atresia with tracheoesophageal fistula in Department of Pediatric Surgery at King George Medical University, Lucknow, India from February 2004 to May 2006 were included in the study. The patients with long gap esophageal atresia without tracheoesophageal fistula (13) and patients who expired before surgery (8) were excluded. The babies were allocated by computer-generated random number table to one of two groups: in Group A—the Azygos vein was preserved during operation and in Group B—the Azygos vein was ligated. The two Groups were compared with respect to sex, weight, prematurity, associated anomalies, Waterston, Spitz classification and distance between the pouches after mobilization. All patients were operated by extra pleural approach through a right posterolateral thoracotomy. A retropleural drain was placed in only two patients in Group A ands all patients in Group B according to the preference of the operating surgeon, whereas a trans-anastomotic tube was placed in all patients (in both groups) and used for postoperative feeding. Both Groups received the same preoperative and postoperative treatment. Oral feeds were started in both groups after a contrast swallow to rule out anastomotic leak usually after the seventh postoperative day. In patients in whom a retropleural drain was placed, anastomotic leaks were detected either by observing the saliva in the drain or by contrast swallow. Minor leaks were identified by appearance of frothy saliva in the retropleural drain with no accompanying deterioration in the general condition. The leak was confirmed by administering oral methylene blue and observing its appearance in the retropleural drain. Major leaks were clinically suspected by the profuse contents in the retropleural drain with accompanying deterioration in general condition of the patient. In patients in whom no retropleural drain was placed, leaks were clinically suspected by increased respiratory distress, fever and sepsis or plain X-ray chest showing pneumothorax and pneumonitis and confirmed by contrast study of esophagus. The incidence of anastomotic leak in the two groups was noted. Minor leaks were managed expectantly, whereas major leaks were treated by re thoracotomy and cervical esophagostomy with gastrostomy.
Results
A total of 117 patients were admitted with esophageal atresia with tracheoesophageal fistula during study period; 91 in Spitz group I ,25 in Spitz group II and 1 in Spitz group III. Out of these, 96 neonates who underwent primary repair were included in the study. Thirteen patients with long gap esophageal atresia with tracheoesophageal fistula and eight patients who expired before surgery were excluded. Group A had 46 patients and Group B has 50 patients. The comparison between two groups in term of sex, weight, prematurity, associated anomalies, Waterston and Spitz classification are given in Table 1. Associated congenital anomalies were present in 12 patients in group A and 14 patients in group B (Table 2). Anastomotic leak occurred in three cases (6%) in Group A and ten cases (20%) in Group B. In group A, there were one major and two minor leaks whereas in group B, there were eight major and two minor leaks. The distance between the pouches after mobilization had no influence on anastomotic leakage in either group. Major anastomotic leak was responsible for mortality in one (2%) case in Group A and six cases (12%) in Group B. The other causes of mortality were associated malformations and sepsis (Table 3).
Discussion
In the standard technique for repair of EA&TEF, the Azygos vein is ligated and divided early in the procedure to facilitate access to the lower pouch fistula and esophageal anastomosis. Holder et al. [4] have described preservation of the Azygos vein. For preservation of the Azygos the first one or two tributaries coming off the ribs are cauterized. Dissection of the lower pouch is done after retracting the vein superiorly to access the fistula (Figs. 1, 2). Esophageal anastomosis is done anterior or posterior to the vein as may be convenient (Fig. 3). We found that preserving the Azygos vein increased neither the operating time nor technical difficulty. Our hypothesis is that, due to its draining the esophagus, preservation of Azygos vein can benefit the patient by preventing early postoperative edema at the anastomotic site. It is not our intention to state that sparing of the Azygos is the only factor in preventing anastomotic leak, but it can offer additional benefit. Moreover the Azygos is a major vein in the body and if it can be preserved without adding to patient morbidity then it should be done. Review of literature showed that there is a definite incidence of anastomotic leakage associated with the surgery for esophageal atresia. Konkin et al. [2] in a study of 144 cases reported anastomotic leak in 8% of cases. McKinnon et al. [5] in their series of 62 patients of EA&TEF have reported anastomotic leak in 21% cases. Major anastomotic leaks have significant morbidity and most of them need re operation and sometimes abandonment of esophagus. Chittmittrapap et al. [6] reported anastomotic leakage following surgery for esophageal atresia in 17% of 199 neonates. Seven (3.5%) of these were major anastomotic disruptions. All Infants with major leak required early re-operation, necessitating abandonment of the esophagus in six. Sarin et al. [7] reported anastomotic leakage in 19% of 80 neonates with EA&TEF, who underwent end-to-end esophageal anastomosis with mortality rates of about 90% after leak. In view of these figures we feel that any measure that offers protection from anastomotic leakage without producing additional patient morbidity should be adopted. Preservation of the Azygos vein is one such step. In our patients preservation of Azygos vein was responsible for reduction in the number of anastomotic leaks. We propose that preservation of the Azygos vein prevents early postoperative edema of the esophageal anastomosis by maintaining the venous drainage and thus may form an additional protective factor against anastomotic leaks.
References
Myers NA (1974) Oesophageal atresia: the epitome of modern surgery. Ann R Coll Surg Engl 54:277–287
Konkin DE, O’hali WA, Webber EM, Blair GK (2003) Outcomes in esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 38:1726–1729
Gabella G (2000) Veins of the thorax. In: Williams PI (ed) Gray’s anatomy: the anatomical basis of medicine and surgery. Churchill Livingstone, London, pp 1593
Holder TM (1993) Esophageal atresia and tracheoesophageal malformations. In: Ashcraft KW, Holder TM (eds) Pediatric surgery. W.B. Saunders, Philadelphia, pp 249–269
McKinnon LJ, Kosloske AM (1990) Prediction and prevention of anastomotic complications of esophageal atresia and tracheo-esophageal fistula. J Pediatr Surg 25:778–816
Chittmittrapap S, Spitz L, Brereton RJ et al (1992) Anastomotic leakage following surgery for esophageal atresia. J Pediatr Surg 27:29–32
Sarin YK, Nambirajan L (1996) Anastomotic leakage following repair of esophageal atresia and tracheo-esophageal fistula. Indian J Pediatr Surg 1:83–85
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, S., Sinha, S.K., Rawat, J.D. et al. Azygos vein preservation in primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 23, 1215–1218 (2007). https://doi.org/10.1007/s00383-007-2008-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-2008-5