Abstract
We aimed to evaluate para-aortic metastases relative to the level of inferior mesenteric artery (IMA) and to discuss the clinico-pathological features of these patients. A total of 204 patients who underwent systematic pelvic and para-aortic lymphadenectomy up to the level of renal veins for endometrial cancer between January 2007 and August 2013 were included in this study. Of these 204 patients, 44 (21.6 %) had lymph node involvement. From a total of 27 patients with paraaortic lymph node (PALN) metastasis, 11 had only supramesenteric and 4 had only inframesenteric nodal involvement, while 12 had both supramesenteric and inframesenteric metastases. Supramesenteric lymph node metastases were detected in 85.2 % of patients who have para-aortic metastases and in 11.3 % of all patients. Additionally, 5 patients had only supramesenteric lymphatic metastasis. The surgico-pathological characteristics of patients with isolated supramesenteric and inframesenteric metastasis were similar. However, the patients with lymphatic spread in both regions were found to have pelvic lymphatic metastasis and cervical invasion more commonly compared to patients with only supramesenteric or only inframesenteric metastasis. The site of metastatic lymph nodes wasn’t associated with the likelihood and site of recurrence. Lymphadenectomy should be performed up to the level of renal vein in case of the presence of indication for lymphadenectomy in patients with endometrial cancer. Additionally, it is not possible to predict the patients with supramesenteric lymph node involvement by tumor grade, histological type and myometrial invasion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial cancer has been surgically staged according to International Federation of Obstetricians and Gynecologists (FIGO) since 1988 [1]. Disease is usually limited to the uterus. However, 7–12 % of patients had metastatic pelvic and/or paraaortic (PA) lymph nodes without spread outside the pelvis [2, 3]. PA involvement was reported in 3.4–12 % of the patients [4–7].
The extent of surgery in patients with endometrial cancer is still controversial. This controversy was about the necessity of routine lymphadenectomy in staging procedure. Moreover, it isn’t clear whether or not PA lymphadenectomy should be involved when routine lymphadenectomy is performed. Additionally, the extent of PA lymphadenectomy is also controversial. There is no consensus regarding the upper limit of PA lymphadenectomy, inferior mesenteric artery (IMA) or renal vein.
Lymphadenectomy is included in the staging of endometrial cancer with two rationales. One rationale is the definition of the extent of the disease and determination of management and the second one is the achievement of tumoral debulking. National Comprehensive Cancer Network (NCCN) guideline suggests lymphadenectomy in all patients with endometrial cancer with these rationales [8]. On the other hand, lymphadenectomy is known not to improve survival in patients with low-risk disease [9]. However, lymphadenectomy improves survival in patients with intermediate-high risk disease (depth of myometrial invasion ≥1/2, grade 3, cervical invasion, extrauterine spread) [10].
It is clear that only pelvic lymphadenectomy isn’t adequate in patients with intermediate-high risk regarding recurrence. PA involvement is observed in 50–72 % of the patients with endometrial cancer in case of presence of pelvic metastasis [7, 11–14]. Furthermore, PA lymphadenectomy was shown to improve survival in patients with intermediate-high risk endometrial cancer [15–17]. Additionally, FIGO categorized stage IIIC into two groups in respect to the presence of paraaortic metastases in 2009. Therefore, stage IIIC was divided into two substages as stage IIIC1 (only pelvic nodal involvement) and stage IIIC2 (para-aortic nodal involvement) [18]. PA lymph node dissection is obligatory for complete staging in endometrial cancer.
There is no consensus in the answer of the question what the superior border of the PA lymphadenectomy should be, IMA or renal vein. However, in the study by Mariani et al., they showed the presence of metastatic lymph nodes above the level of IMA in 77 % of the patients with pelvic involvement and the presence of lymphatic metastasis only above IMA in more than half of these patients [16]. Additionally, tumor spread above the level of IMA in 70–88 % of the patients with PA metastasis [11, 12, 14]. In our preliminary report that we evaluated the patients with intermediate-high risk for recurrence (grade 2 and 3, non-endometrioid tumor type, depth of myometrial invasion ≥1/2, tumor size >2 cm, cervical invasion, extrauterine metastasis), 14 % of all patients, 61 % of the patients with lymph node metastasis and 91.7 % of the patients with paraaortic metastasis had lymphatic disease above the level of IMA. Furthermore, 4 % of the patients had lymphatic spread only above the level of IMA [19].
In the present manuscript, we aimed to represent the final results of the study, of which we previously presented the preliminary report that evaluated the lymphatic spread prospectively in 78 patients with endometrial cancer.
Material Method
A total of 204 patients who underwent staging surgery with a diagnosis of endometrial cancer between January 2007 and August 2013 were included in the study. Staging was performed according to the FIGO 2009 criteria. PA lymphadenectomy has been performed in our clinic by classifying PA region into 2 as supramesenteric (SM) and inframesenteric (IM) according to the level of IMA for ovarian and uterine cancers since January 2007. We aimed to identify the upper level of lymphatic spread and lymphadenectomy in patients with endometrial cancer in this evaluation.
Pelvic and PA lymphadenectomy was performed including the regions between deep circumflex iliac vein and left renal vein in patients with endometrial cancer who fulfilled the criteria for staging. Patients with uterine sarcoma or sarcomatous component and patients with synchronous tumors were excluded. Serous, clear cell and undifferentiated tumors were defined as FIGO grade 3 tumor. All surgical procedures were performed by gynecologic oncologists. All operations were done by laparotomy.
Frozen/section (FS) is utilized routinely in patients with endometrial cancer in our clinic and staging surgery is performed for the patients whose FS revealed non-endometrioid adenocancer, FIGO grade 2 or 3 disease, the depth of myometrial invasion ≥1/2, cervical involvement and a tumor size >2 cm. Furthermore, patients with a preoperative diagnosis of FIGO grade 3 disease or cell type with high risk undergo staging surgery directly. Staging surgery standardly involves total abdominal hysterectomy + bilateral salpingo-oophorectomy + systematic pelvic and paraaortic lymphadenectomy + omentectomy + cytological evaluation of abdominal washing or ascites when it is present. Cytological sampling is evaluated with hematoxylin eosin. In case of intraoperative identification of macroscopic disease, cytoreductive surgical techniques are used in addition to staging surgery.
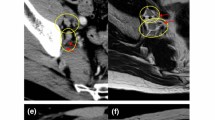
Bilateral pelvic lymphadenectomy was performed to complete skeletonization, with all lymphatic tissue of the common, external and internal iliac vessels and the obturator fossa removed after visualization of the obturator nerve. The superior surgical dissection margin for the pelvic nodes was the aortic bifurcation, and the anterior distal surgical dissection margin was the circumflex iliac vein. The presacral lymphatic tissue was harvested separately. Each of common iliac, external iliac, internal iliac, obturator and presacral regions was included in the pelvic region. The upper limit of paraaortic lymphadenectomy was left renal vein. All lymphatic tissues were then harvested from the precaval, laterocaval, interaortacaval, preaortic and lateroaortic regions up to the renal veins with vessel skeletonization. PA lymphadenectomy was performed by separating this region into 2 according to the level of IMA. The region between left renal vein and IMA was defined as SM region and the region between IMA and aortic bifurcation was defined as IM region. The lymph-node-bearing tissue from the pelvic region, SM region and IM region were submitted for analysis, separately. All surgeries were performed and all pathologic findings were evaluated at a single institution.
In terms of histological evaluation, the uterus was divided into 2 pieces coronally from the cervix to the uterine fundus. The place, size and growth pattern-exophytic or endophytic-of the tumor were evaluated macroscopically. The tissue beginning from the cervix to the fundus was sampled as full-thickness sections. The number of sections taken for microscopic examination ranged between 3 and 5. Myometrial invasion was evaluated by taking 2 full-thickness sections from the tissue involving the tumor where the myometrial invasion was maximum macroscopically. After the lymph nodes were extracted from the tissue covering them, they were sampled by dividing into 2 pieces along the longitudinal axis. All the sections were evaluated after staining with hematoxylin-eosin.
In terms of adjuvant therapy, only radiotherapy or sandwich therapy (3 cycles paclitaxel + carboplatin followed by radiotherapy followed by 3 cycles paclitaxel + carboplatin) or only chemotherapy or chemotherapy followed by radiotherapy or radiotherapy followed by chemotherapy were applied at the discretion of the surgeon and according to the spread of the disease. Radiotherapy was given to pelvic region in case of only pelvic nodal involvement, while it was given as extended-field radiotherapy in patients with paraaortic lymph node metastasis or without sufficient evaluation of the paraaortic lymph nodes.
Patients were followed-up every 3 months for 2 years after adjuvant therapy, every 6 months until the fifth year following treatment and yearly thereafter. In every follow-up, pelvic examination, abdominal ultrasonography, complete blood count and blood chemistry were performed. Chest X-ray was utilized yearly or in case of clinical suspicion. Thoracic and/or abdominal computerized tomography was used when needed. Ca-125 level and Pap-smear test were utilized in the follow-up, even though they weren’t used routinely.
We defined recurrence distal to the pelvic inlet (true pelvis) as pelvic recurrence, recurrence between pelvic inlet and diaphragm as upper abdominal recurrence and all the rest of recurrences as extraabdominal recurrence. While ascites and peritonitis carcinomatosa were accepted as upper abdominal recurrence, recurrence in the liver parenchyma, skin and bone were accepted as extraabdominal recurrence.
Descriptive statistics were performed using the SPSS software version 17.0 (SPSS, Inc, Chicago, III). Chi-square, Anova Table test were used for statistical analysis. The cut-off for statistical significance was set at p < 0.05.
Results
In the study period, 465 patients with endometrial cancer were operated. Among these, 204 patients (44 %) were staged using the criteria mentioned in the “Material and Method” section. The median age of the patients was 60 years (range, 37–92). Stage was IA in 64 patients, IB in 67, II in 20, IIIA in 8, IIIC1 in 15, IIIC2 in 20 and IVB in 10 patients. The median tumor size was 43.7 mm (range, 3–335). Tumor type was endometrioid in 156 patients and 77 patients had grade 3 disease. There was no myometrial invasion in 16 patients, while 105 patients had myometrial invasion ≥1/2. Cervical involvement was observed in 48 patients and 40 of these had cervical stromal invasion. Lymphovascular spread was present in 63 patients. Peritoneal cytology was positive in 9 patients. Omental metastasis was detected in 9 patients and 17 patients had adnexal involvement. Four of the patients had upper abdominal disease other than omental metastasis. Three of these had also omental metastasis and one patient had only liver metastasis. Surgico-pathological data were presented in Table 1 in detail.
Lymph Node Status
The median number of harvested lymph nodes was 69.1 (range, 33–122). The median PA and pelvic lymph node counts were 24.9 (range, 5–55) and 44.1 (range, 19–92), respectively. The median lymph node count from SM region was 15.2 (range, 1–45) and it was 9.8 (range, 1–23) for IM region.
Lymph node involvement was detected in 44 (21.6 %) patients. Among these, 8 (3.9 %) patients had isolated PA metastasis and 17 (8.3 %) patients had isolated pelvic metastasis. Nineteen (9.3 %) patients had both PA and pelvic metastasis. Among 27 patients with PA involvement, 11 (40.7 %) had only SM metastasis, 4 (14.8 %) had only IM metastasis and 12 (44.4 %) patients had both SM and IM lymphatic involvement. In 5 (2.5 %) of the 8 patients having isolated PA metastasis, lymphatic metastasis was only in the SM region, it was only in the IM region in 2 (1 %) and it was in both regions in 1 (0.5 %) patient (Table 2). The median metastatic lymph node count was 4.4 (range, 1–6), 3.3 (range, 1–13) and 5.5 (range, 1–56) for SM, IM and pelvic regions, respectively.
In conclusion, lymphatic metastasis was observed in SM region in 85.2 % (n = 23/27) of the patients with PA metastasis, in 52.3 % (n = 23/44) of the patients with lymph node involvement and in 11.3 % (n = 23/204) of all patients (Table 2). Isolated SM metastasis was detected in 5 patients (with negative IM and negative pelvic spread) meaning that SM spread of the tumor was observed in 18.5 % (n = 5/27) of the patients with PA involvement, in 11.4 % (n = 5/44) of the patients with lymph node metastasis and in 2.5 % (n = 5/204) of all patients.
Lymph Node Status and Surgico-Pathological Factors
When the relation between the site of PA metastasis and surgico-pathological factors were evaluated, these factors were found to be similar in patients with SM and IM metastasis despite the small number of patients in both groups (Table 3). However, the likelihood of pelvic lymph node metastasis and cervical invasion increased in case of the presence of tumor in both regions compared to the presence of only SM or only IM metastasis (Table 4). Furthermore, the patients with both SM and IM metastasis had more grade 3 tumors compared to the patients with only SM or only IM metastasis, even though the difference wasn’t significant (91.7 % vs 53.3 %, respectively, p = 0.074). Additionally, grade 1 tumor was observed in the patients with only SM metastasis. None of the patients with metastasis in both SM and IM regions had grade 1 tumor. Nevertheless, both groups (SM+IM vs SM or IM) were similar in terms of tumor type, depth of myometrial invasion, lymphovascular space invasion, peritoneal cytology, adnexal involvement and omental metastasis. Lymphatic spread was observed in the 4 patients with upper abdominal spread other than omental metastasis. All these 4 patients had PA metastasis, while only 2 of them had pelvic metastasis. Two of these 4 patients had both SM and IM metastasis, 1 had only SM and 1 had only IM spread.
When the 5 patients with isolated SM lymph node metastasis (negative IM and negative pelvic) were assessed, 2 were detected to have endometrioid tumor. These 2 patients would have had stage IA and IB disease according to 2009 FIGO, if the lymphadenectomy didn’t involve SM region (Table 5). Both had grade 1 tumor. The remaining 3 patients had tumor type with high risk. One of these 3 patients had cervical invasion and one had upper abdominal spread. The last one had serous tumor without any other risk factor and the stage of this patient would have been IA according to 2009 FIGO if SM lymphadenectomy wasn’t performed.
Adjuvant Therapy and Recurrence
Adjuvant therapy was applied to 88 (43.1 %) patients. Among these, 36 had only chemotherapy, 27 had only radiotherapy, 11 took chemotherapy followed by radiotherapy, 13 took sandwich therapy and 1 had radiotherapy followed by chemotherapy. Platin-based combinations were used as first-line chemotherapy (paclitaxel + carboplatin, n:54; cisplatin, n:1, paclitaxel, n:1, doxorubicin + cisplatin, n:5). Forty-eight patients completed 6 cycles of chemotherapy.
Eighteen patients were lost to follow-up after surgery, while 6 were lost to follow-up following adjuvant therapy. Additionally, the adjuvant therapy of 1 patient wasn’t completed at the time of analysis. These 25 patients were excluded. The median follow-up time of 179 patients included in the analysis was 17 months (range, 1–87). Recurrence was observed in 18 (10.1 %) of these patients. The median time from surgery to recurrence was 12.6 months (range, 3–38 months) in these 18 patients. Eight (4.5 %) patients had recurrence only in the pelvis, 5 (2.8 %) patients had only extraabdominal recurrence, 1 (0.6 %) had recurrence only in the upper abdomen, 1 (0.6 %) had both pelvic and extraabdominal recurrences and 2 (1.1 %) patients had upper abdominal and extraabdominal recurrences. Recurrence was observed in all pelvic, upper abdominal and extraabdominal regions in only 1 (0.6 %) patient. Five (2.8 %) patients died during follow-up. Three of these died of endometrial cancer and the other 2 died of diseases other than cancer (cardiac failure and cerebrovascular event).
Lymph Node Status and Recurrence
The data is still limited for the evaluation of the association between lymph node status and recurrence. Nevertheless, lymph node involvement was associated with recurrence (Table 6). The likelihood of recurrence increased from 6.3 to 24.3 % in case of the presence of positive lymph nodes (p = 0.001). On the other hand, when the group with lymph node involvement was assessed in the subgroup analysis, any association couldn’t be shown between site of metastasis and recurrence. Isolated PA or SM lymphatic metastasis was similar to lymphatic spread in other regions regarding recurrence.
Discussion
In endometrial cancer, lymphadenectomy is performed in order to detect the lymphatic spread that is important for prognosis and to obtain tumoral lymphatic debulking. However, the necessity and extent of it hasn’t been cleared up. Performance of lymphadenectomy is widely accepted to improve survival in patients with intermediate-high risk for recurrence [10]. Addition of PA lymphadenectomy was shown to be associated with evident survival advantage compared to performance of only pelvic lymphadenectomy [15–17]. Additionally, PA spread of tumor was detected in 50–72 % of the patients with pelvic lymph node metastasis [7, 11–14]. Besides all, PA region should be evaluated for the presence of tumoral spread in order to stage the disease properly according to 2009 FIGO criteria [18]. Therefore, the necessity of the addition of PA lymphadenectomy to the staging procedure is clear.
Choosing IMA that has no functional or anatomical characteristic regarding lymphatic spread as the upper level of PA lymphadenectomy means inadequate tumoral debulking. In the limited number of studies, SM tumoral spread was reported in 70–88 % of the patients with PA metastasis [11, 12, 14]. In the present study, tumor spread was observed above IMA in half of the patients with lymph node involvement (n = 23/44) and in 85.2 % of the patients (n: 23/27) with PA metastasis. If lymphadenectomy didn’t include the region above IMA, adequate debulking wouldn’t have been achieved in 11.3 % of the patients (n: 23/204). In addition, 2.5 % of all patients (n: 5/204) wouldn’t have been staged properly. If lymphadenectomy didn’t include SM region in the 5 patients with only SM metastasis who were shown in Table 5, the stages of the 2 patients with grade 1 endometrioid tumor would have been reported as stage IA and IB according to 2009 FIGO and observation without adjuvant therapy would have been accepted as the proper management for these 2 patients [20]. Observation without adjuvant therapy also would have been suggested to the third patient whose tumor type was serous without myometrial invasion according to NCCN guidelines [21]. Therefore, 3 patients (%1.5) wouldn’t have taken the necessary treatment.
There are 3 known lymphatic pathways from the uterine body. One of these goes to a group of pelvic lymph nodes, one other to the inguinal lymph nodes, and the last one directly connects with PA lymph nodes. Additionally, a direct route may exist that flows from the corpus to the PA node-bearing basins by the lymphatic channels adjacent to the gonadal vessels within the infundibulopelvic ligament [22]. Mariani et al. found that no metastatic disease was observed in the gonadal veins or surrounding soft tissues in the absence of PA lymph node involvement [23]. In the studies identifying sentinel lymph nodes in endometrial cancer, PA sentinel lymph nodes were reported to be above IMA [24, 25]. Therefore, SM region can be stated to be more significant than IM region regarding lymphatic spread.
In this study, any difference couldn’t be found between the patients with only SM or only IM lymphatic spread regarding surgico-pathological factors. Nevertheless, the patients with lymphatic spread in both regions were found to have pelvic lymphatic metastasis and cervical invasion more commonly compared to patients with only SM or only IM metastasis. The likelihood of having lymphatic metastasis in external iliac region was reported to increase from 20.7 to 62 % in case of presence of cervical invasion in our previous study in which lymphatic spread in stage IIIC endometrial cancer was evaluated [26]. This result explains the relation between the presence of lymphatic metastasis in both PA regions and the presence of pelvic lymphatic metastasis and cervical invasion. In addition, the patients with lymphatic metastasis in both PA regions tended to have higher grade tumors in comparison to patients with only SM or only IM metastasis. This may mean that clinically more aggressive tumors spread to pelvic and PA regions sequentially and that the other ones spread to PA, especially to SM region directly earlier via gonadal vascular structures. However, there is no adequate data that supports this concept and that presents the survival of patients with isolated SM lymphatic metastasis (negative IM and negative pelvic). In the presented study, the presence of lymph node metastasis was shown to be associated with recurrence despite the limited number of patients, while the site of metastasis wasn’t observed to be related to the site of recurrence. Whereas, our data is still limited to be able to conclude about survival.
The absence of adequate data related to survival is an important limitation regarding the interpretation of clinical results of this study. Another limitation is that the study population didn’t include all patients with endometrial cancer. The study group included the patients with intermediate-high risk for recurrence, since these patients had the indication for lymphadenectomy. However, performance of the study in a single institution and adequate number of harvested lymph nodes were the advantages of this study.
In conclusion, in this study, if the lymphadenectomy was performed up to the level of IMA, tumoral debulking wouldn’t have been obtained in more than 10 % of the patients with intermediate-high risk for recurrence and 2.5 % of the patients wouldn’t have been staged properly. Eighty-five percent of the patients with PA metastasis had metastasis in SM region. It isn’t possible to predict the patients with SM involvement using surgico-pathological factors. Therefore, IMA that was selected as the upper level of PA lymphadenectomy is an arbitrary border and lymphadenectomy should be performed up to the level of renal vein in patients who were decided to be staged. Additionally, multi-center trials are required to detect the survival of patients with isolated SM metastasis (negative IM and negative pelvic) and to compare the survival of these patients with the patients having isolated IM metastasis, with the patients having IM+SM metastasis and pelvic lymph node metastasis.
References
Announcements (1989) FIGO (the International Federation of Obstetricians and Gynecologists) stages: 1988 revision. Gynecol Oncol 35:125–126
Hoekstra AV, Kim RJ, Small W Jr et al (2009) FIGO stage IIIC endometrial carcinoma: prognostic factors and outcomes. Gynecol Oncol 114(2):273–278
McMeekin DS, Lashbrook D, Gold M, Johnson G, Walker JL, Mannel R (2001) Analysis of FIGO Stage IIIC endometrial cancer patients. Gynecol Oncol 81(2):273–278
Creasman WT, Morrow CP, Bundy BN et al (1987) Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group study. Cancer 60:2035–2041
Hirahatake K, Hareyama H, Sakuragi N et al (1997) A clinical and pathologic study on para-aortic lymph node metastasis in endometrial carcinoma. J Surg Oncol 65:82–87
Mariani A, Keeney GL, Aletti G et al (2004) Endometrial carcinoma: paraaortic dissemination. Gynecol Oncol 92:833–838
Turan T, Hizli D, Sarici S et al (2011) Is it possible to predict para-aortic lymph node metastasis in endometrial cancer? Eur J Obstet Gynecol Reprod Biol 158(2):274–279
National Comprehensive Cancer Network (2006) Clinical practice guidelines in oncology, uterine cancers. Version 1. National Comprehensive Cancer Network, Washington, DC
ASTEC study group, Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK (2009) Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomized study. Lancet 373(9658):125–136
Chan JK, Cheung MK, Huh WK et al (2006) Therapeutic role of lymph node resection in endometrioid corpus cancer: a study of 12,333 patients. Cancer 107(8):1823–1830
Fotopoulou C, Savvatis K, Kraetschell R, Schefold JC, Lichtenegger W, Sehouli J (2010) Systematic pelvic and aortic lymphadenectomy in intermediate and high-risk endometrial cancer: lymph-node mapping and identification of predictive factors for lymph-node status. Eur J Obstet Gynecol Reprod Biol 149(2):199–203
Kumar S, Podratz KC, Bakkum-Gamez JN et al (2014) Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecol Oncol 132(1):38–43
Nomura H, Aoki D, Suzuki N et al (2006) Analysis of clinicopathologic factors predicting para-aortic lymph node metastasis in endometrial cancer. Int J Gynecol Cancer 16(2):799–804
Odagiri T, Watari H, Kato T, et al (2014) Distribution of lymph node metastasis sites in endometrial cancer undergoing systematic pelvic and para-aortic lymphadenectomy: a proposal of optimal lymphadenectomy for future clinical trials. Ann Surg Oncol
Chang SJ, Kim WY, Yoon JH, Yoo SC, Chang KH, Ryu HS (2008) Para-aortic lymphadenectomy improves survival in patients with intermediate to high-risk endometrial carcinoma. Acta Obstet Gynecol Scand 87(12):1361–1369
Mariani A, Webb MJ, Galli L, Podratz KC (2000) Potential therapeutic role of para-aortic lymphadenectomy in node-positive endometrial cancer. Gynecol Oncol 76(3):348–356
Todo Y, Kato H, Kaneuchi M, Watari H, Takeda M, Sakuragi N (2010) Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL study): a retrospective cohort analysis. Lancet 375(9721):1165–1172
Meeting Report (2009) The new FIGO staging system for cancers of the vulva, cervix, endometrium and sarcomas. Gynecol Oncol 115:325–328
Turan T, Yilmaz SS, Hizli D et al (2011) A prospective evaluation of lymphatic dissemination in endometrial cancer: is it adequate to perform lymph node dissection up to the inferior mesenteric artery? Int J Gynecol Cancer 21(5):864–869
Creutzberg CL, van Putten WL, Koper PC et al (2000) Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomized trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet 355(9213):1404–1411
National Comprehensive Cancer Network (2014) Clinical practice guidelines in oncology, uterine cancers. Version 1. National Comprehensive Cancer Network, Washington, DC
Yokoyama Y, Maruyama H, Sato S et al (1997) Indispensability of pelvic and paraaortic lymphadenectomy in endometrial cancers. Gynecol Oncol 64:411–417
Mariani A, Dowdy SC, Cliby WA et al (2008) Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol 109:11–18
Burke TW, Levenback C, Tornos C et al (1996) Intraabdominal lymphatic mapping to direct selective pelvic and paraaortic lymphadenectomy in women with high-risk endometrial cancer: results of a pilot study. Gynecol Oncol 62:169–173
Maccauro M, Lucignani G, Aliberti G et al (2005) Sentinel lymph node detection following the hysteroscopic peritumoural injection of 99mTc-labelled albumin nanocolloid in endometrial cancer. Eur J Nucl Med Mol Imaging 32:569–574
Turan T, Hizli D, Sarici S et al (2012) What is the impact of cervical invasion on lymph node metastasis in patients with stage IIIC endometrial cancer? Arch Gynecol Obstet 285(4):1119–1124
Conflict of Interest
Authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alay, I., Turan, T., Ureyen, I. et al. Lymphadenectomy Should Be Performed Up to the Renal Vein in Patients with Intermediate-High Risk Endometrial Cancer. Pathol. Oncol. Res. 21, 803–810 (2015). https://doi.org/10.1007/s12253-014-9893-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-014-9893-4