Abstract
Background
Lateral pelvic lymph node dissection (LLND) combined with removal of the internal iliac vessels is a challenging surgical procedure in minimally invasive surgery. We herein report our dissection approach and short-term outcomes.
Methods
We conducted a study on rectal cancer patients who underwent laparoscopuic LLND combined with removal of the internal iliac vessels at our institution in March 2017–December 2019. In performing the surgery, we identified and dissected along the three pelvic sidewall fasciae (ureterohypogastric, umbilical prevesical and parietal pelvic fascia), located the internal ilial vein at the level of the common iliac vessels and carried out our dissection along the medial anterior surface of the internal iliac before transecting the vein. The duration of LLND was recorded as was the blood loss.
Results
There were 16 patients (10 males, mean age 65.4 ± 10.8 years). Five patients had primary surgery, and 11 had surgery for recurrence. The median blood loss of LLND was 10 ml (range, 0–250 ml), the median operating time was 173 min (range, 65–358 min), and post-operative complications were relatively mild. Seven of 16 patients (43.8%) were diagnosed with positive lateral nodes. The 2-year local recurrence-free and disease-free survival rates were 87.5% and 58.0%.
Conclusion
Recognizing the pelvic anatomical points illustrated in the present study contributes to the surgical safety of LLND combined with removal of the internal iliac vessels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The significance of selective lateral pelvic lymph node dissection (LLND) following chemoradiotherapy (CRT) has been discussed, and several studies have shown LLND to be useful for achieving local control in patients with suspected node metastasis [1,2,3,4,5,6]. However, nodes that are positive after CRT are radio-resistant, and drastic LLND is sometimes required to achieve R0 resection, such as dissection combined with the removal of the internal iliac vessels. The difficulty of this surgical approach is well-reported, and a thorough understanding of the pelvic anatomy and careful surgical techniques are required for success.
We herein report our dissection approach and the short-term outcomes of laparoscopic LLND combined with removal of the internal iliac vessels in rectal cancer.
Materials and methods
We conducted a study on rectal cancer patients who underwent laparoscopuic LLND combined with removal of the internal iliac vessels at our institution in March 2017–December 2019.
The indication of LLND for non-CRT patients was T3,4 lower rectal cancer located below the peritoneal reflection, according to the Japanese clinical guidelines, and that for CRT patients was a lateral node size > 7 mm at the short axis at initial staging [7]. At our institution, CRT was indicated for cases with main tumors involving the mesorectal fascia and/or cases in which LLND combined with the removal of the internal iliac vessels was planned. The indication of LLND combined with the removal of the internal iliac vessels was clinically positive lateral nodes attached to or invading the internal iliac vessels at initial staging. In all cases with the combined removal of the internal iliac vessels, both the internal iliac arteries and veins were ligated. The initial imaging findings of the main tumor and lateral lymph nodes are shown in Fig. 1a–f.
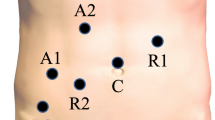
Surgical procedure (right side) shown in the supplemental video
Step 1. Dissection of ureterohypogastric fascia (inner border) (Fig. 2a) (Video; 0:00–0:22).
Surgical procedure. a Dissection of the ureterohypogastric fascia (inner border). The yellow triangle indicates the ureterohypogastric fascia. b Dissection of the parietal pelvic fascia (outer border). The yellow triangle indicates the parietal pelvic fascia. c Dissection of the umbilical prevesical fascia. d Dissection of the internal iliac vein (inner side). The yellow triangle indicates the internal iliac vein. e Dissection of the internal iliac vein (outer side). The yellow triangle indicates the superior gluteal vein. f Dissection of the internal iliac vein (ventral side). The yellow dotted line indicates the incision line on the umbilical prevesical fascia. g Ligation of the common trunk of the internal pudendal and inferior gluteal veins/arteries at infrapiriformis foramen. h Ligation of the internal iliac vein. i Dissection around the sciatic nerve. The yellow triangle indicates the sciatic nerve. j Ligation of the inferior vesical vessels. The yellow triangle indicates the inferior vesical vessels. k Picture after LLND combined with removal of the internal iliac vessels
The ureterohypogastric fascia wraps around the hypogastric nerve, pelvic plexus and ureter as a single membrane and sits adjacent to the total mesorectal excision (TME) plane on the inside. The ureterohypogastric fascia can be recognized by dissecting the ureter from the outside, forming the inner border of LLND.
Step 2. Dissection of the parietal pelvic fascia (outer border) (Fig. 2b) (Video; 0:22–0:47).
Adipose tissue is dissected from the external iliac vessels, psoas and internal obturator muscle, and the parietal pelvic fascia is exposed to determine the outer border. The dissection landmark of this fascia on the caudal side is the vas deferens in men and the uterine cord in women. By means of this procedure, the dissection area of the inner border (ureterohypogastric fascia; Step 1) and outer border (parietal pelvic fascia; Step 2) is determined, and the internal iliac vessels can be seen running into the adipose tissue.
The obturator nerve runs over the sacroiliac joint, between the internal and external iliac vessels, and reaches the obturator foramen. The obturator nerve is dissected from the adipose tissue.
Step 3. Dissection of the umbilical prevesical fascia (Fig. 2c) (Video; 0:47–1:16).
Dissection of the cranial side is performed from the bifurcation of the external and internal iliac artery, and the umbilical artery is identified. The umbilical artery is visible through the visceral peritoneum as a medial fold running towards the navel. There is a fascia between the umbilical artery and internal iliac artery called the umbilical prevesical fascia. This fascia is important because the ventral (visceral) branches of the internal iliac artery (superior and inferior vesical artery, middle rectal artery, internal pudendal artery, deferential artery [male] and uterine artery [female]) run along the inner side of the fascia, while the somatic branches (lateral sacral artery, obturator artery and superior and inferior gluteal artery) run along the outer side.
Step 4. Dissection of the internal iliac vein (inner side) (Fig. 2d) (Video; 1:16–1:47).
The most important point when performing LLND combined with removal of the internal iliac vessels is to understand the route of the internal iliac veins and their branches. The best location for identifying the route of the internal iliac vein is at the common iliac vessels. At this point, the vein is located on the dorsal side of the artery. Thus, by dissecting the dorsal side of the common iliac artery, the common iliac vein can be confirmed. In addition, it is rare for the internal iliac vein to have a ventral (visceral) branch inward (toward the TME area) from the main trunk; thus, dissecting the medial anterior surface of the internal iliac vein helps clarify the route of the vein without injuring the branch veins.
Step 5. Dissection of the internal iliac vein (outer side) (Fig. 2e) (Video; 1:47–2:01).
After confirming the route of the internal iliac vein from the inner side, it is important to encircle the internal iliac vein before the transection of the vein. When dissecting the outer side of the internal iliac vein, careful dissection of the internal iliac vein somatic branch is important (Fig. 2e). The key points to consider when determining the vein branch type are as follows: the superior gluteal vein runs between the L5 and S1 nerve roots and exits into the suprapiriform foramen; the inferior gluteal vein exits into the infrapiriform foramen, although there are various branch variations; the obturator vein exits into the obturator foramen, and an accessary obturator vein, which is a branch of the external iliac vein, is confirmed in some cases.
Step 6. Dissection of the internal iliac vein (ventral side) (Fig. 2f) (Video; 2:01–2:47 min).
The umbilical prevesical fascia connects with the umbilical artery and internal iliac arteries. Thus, by incising this fascia, the internal iliac arteries can be identified from internal and external views. The umbilical prevesical fascia is dissected below the superior vesical artery to maintain the flow to the bladder. As described above, it is important to identify the proximal internal iliac vein and encircle it from the inner side (Fig. 2d), outer side (Fig. 2e) and ventral side (Fig. 2f).
We routinely preserve the umbilical artery for two reasons. First, the superior vesical artery, which branches from the umbilical artery, can maintain the blood flow to the bladder. Second, the umbilical prevesical fascia is divided between the lateral pelvic components and the bladder, and the landmark of this fascia is the umbilical artery. However, it is acceptable to ligate the umbilical artery in these cases to maintain the flow to the bladder, such as by preserving the internal iliac vessels or in unilateral cases.
Step 7. Ligation of the common trunk of the internal pudendal and inferior gluteal veins/arteries at infrapiriformis foramen (Fig. 2g) (Video; 2:47–3:06).
After the ligation of the internal iliac artery, the common trunk of the internal pudendal and inferior gluteal veins/arteries are ligated at the infrapiriformis foramen to block the inflow of the internal iliac vein (Fig. 2g). The infrapiriformis foramen is formed by the piriformis muscle, coccygeus muscle and obturator muscle, and the common trunk of the internal pudendal and inferior gluteal veins/arteries pass through this canal. The infrapiriformis foramen is located on the ventral side of the ischial spine, which is located at the S4 level. Thus, dissection of the pelvis sidewall proceeds from the lateral side (Step 2) and cranial side (Step 5).
Step 8. Ligation of the internal iliac vein (Fig. 2h, i) (Video; 3:06–3:37).
After ligation of the common trunk of the internal pudendal and inferior gluteal veins/arteries, the internal iliac vein is ligated (Fig. 2h). The sciatic nerve passes through the anterior surface of the sacroiliac joint and the piriformis and exits the pelvis through the infrapiriformis foramen. During dissection around the sciatic nerve, the parietal fascia should be attached to the sciatic nerve, without the nerve being directly exposed, to prevent nerve pain (Fig. 2i).
Step 9. Ligation of the inferior vesical vessels (Fig. 2j) (Video; 3:37–3:50).
Continuing on from dissection between the umbilical prevesical fascia and bladder, the inferior vesical vessels can be identified. After ligating those vessels, en bloc dissection of LLND can be performed.
Step 10. Picture after LLND combined with removal of the internal iliac vessels (Fig. 2k) (Video; 3:50–4:22).
Statistical analyses
The short-term outcomes of patients with LLND combined with removal of the internal iliac vessels are shown in Tables 1 and 2. The time to recurrence was measured from the date of surgery, and the 2-year local recurrence-free survival (LFS), disease-free survival (DFS) and overall survival (OS) rates were calculated using the Kaplan–Meier method. The data were analyzed using the JMP 13.0 software program (SAS Institute Inc., Cary, NC, USA).
Results
Short-term outcomes (Tables 1, 2)
From April 2017 to December 2019, 16 patients (10 males, mean age 65.4 ± 10.8 years) underwent LLND combined with removal of the internal iliac vessels (Table 1). Of these 16 patients with combined removal, 11 were undergoing surgery for recurrence, and 6 of these 11 patients had central-type recurrence while 5 had LLN recurrence. These 5 patients with LLN recurrence did not have LLND at the initial surgery; 4 of them underwent LLND, and 1 underwent combined removal of the bladder and prostate due to tumor invasion of the ureter and bladder. Fourteen of the 16 patients with combined removal received CRT, while 2 did not because they received CRT at the initial surgery. Seven of the 16 patients (43.8%) with combined removal were diagnosed with positive lateral nodes, including 1 with extramural tumor deposits and 1 with a high degree of cancer cell degeneration as a result of CRT. R0 resection was performed in 15 of 16 patients (93.8%). Regarding post-operative complications, approximately 40% of the patients suffered from urinary dysfunction and nerve pain; however, no patients suffered from severe nerve pain during long-term follow-up. Self-catheterization was performed in 3 patients (20.0%).
The operating time and blood loss in LLND are shown in Table 2. Of the 16 patients, 3 underwent combined removal of the bilateral internal iliac vessels, so a total 19 cases were analyzed. The operating time and blood loss were measured from the beginning of LLND to the removal of the lateral pelvic lymph nodes. The median time and blood loss were 173 (range 65–358) min and 10 (range 0–250) ml, respectively.
The median follow-up period was 18 (range 3–37) months. The 2-year LFS, DFS and OS rates (removal and preservation) were 87.5%, 58.0% and 87.5%, respectively (Fig. 3).
Discussion
The main aim of this complex procedure was en bloc resection of the lateral pelvic components without exposing the metastatic lymph nodes that abutted or invaded the vessels. We hypothesized that this approach would reduce the risk of local recurrence in select highly advanced cases, which is the main benefit of the present approach.
It should be noted that extensive surgery is associated with an increased risk of post-operative complications. Therefore, care should be taken to prevent these complications. One potential complication is sciatic nerve pain. To prevent this, the route of the sciatic nerve should be recognized to prevent the injury. When performing dissection around the sciatic nerve, the sciatic nerve should be covered with the parietal pelvic fascia and not be directly exposed (Fig. 2i). After surgery in the present study, non-steroidal anti-inflammatory drugs (NSAIDs), antineuralgic agents, opioids and adjuvant drugs (e.g. antidepressants, antiseizure drugs) were prescribed by pain physicians. In addition, ultrasound-guided sciatic nerve block was used in cases of severe pain. From our experience, these treatments are sufficient to manage the nerve pain. As we were able to successfully preserve the S2 and upper level of the sacral nerve, no patients in the present study had any weakness of the lower limbs due to motor dysfunction of the sciatic nerve.
Another potential post-operative complication is ischemic cystitis, especially in patients who undergo bilateral LLND combined with the removal of the internal iliac vessels. In this region, four blood vessels (right and left superior and inferior vesical arteries) flow into the bladder. We routinely preserve the superior vesical arteries, and none of the patients included in this study required additional treatment due to ischemic cystitis. Another potential complication is urinary and sexual dysfunction. It is well known that LLND is associated with increased rates of urinary dysfunction and sexual dysfunction [8]. However, some data have demonstrated the significance of pelvic nerve preservation in LLND, and this approach did not adversely affect the functional outcomes [9]. Thus, when there are no signs of tumor invasion, we routinely preserve the pelvic plexus, even when performing combined removal of the internal iliac vessels.
Several limitations associated with the present study warrant mention. First, the study was retrospective in nature, included a relatively small population and had a short follow-up period. Second, the patients who were included in this study were thinner than Western patients, limiting generalizability. Third, more than half of the patients were found to have negative nodes despite being assigned such extensive surgery. Our surgical procedure was determined based on the initial staging, which might have increased the rate at which we performed LLND combined with the removal of the internal iliac vessels and reduced the incidence of lateral LN positivity. In cases in which good LN shrinkage can be obtained by CRT, it might be possible to preserve the vessels. However, further studies will be required to answer this question. Finally, LN invasion to the internal iliac vessels was not pathologically diagnosed. Making a pathological diagnosis of LN invasion would underscore the significance of this approach.
Conclusion
Recognizing the pelvic anatomical points illustrated in the present study will help improve the surgical safety of LLND combined with removal of the internal iliac vessels.
Code availability
None.
References
Ogura A, Konishi T, Cunningham C, Garcia-Aguilar J, Iversen H, Toda S, Lee IK, Lee HX, Uehara K, Lee P, Putter H, van de Velde CJH, Beets GL, Rutten HJT, Kusters M; Lateral Node Study Consortium (2019) Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low ct3/4 rectal cancer. J Clin Oncol 37:33–43
Malakorn S, Yang Y, Bednarski BK, Kaur H, You YN, Holliday EB, Dasari A, Skibber JM, Rodriguez-Bigas MA, Chang GJ (2019) Who should get lateral pelvic lymph node dissection after neoadjuvant chemoradiation? Dis Colon Rectum 62:1158–1166
Ishihara S, Kawai K, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, Morikawa T, Watanabe T (2017) Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative. Chemoradiotherapy 60:469–476
Perez RO, São Julião GP, Vailati BB, Fernandez LM, Mattacheo AE, Konishi T (2018) Lateral node dissection in rectal cancer in the era of minimally invasive surgery: a step-by-step description for the surgeon unacquainted with this complex procedure with the use of the laparoscopic approach. Dis Colon Rectum 2018(61):1237–1240
Kawada K, Yoshitomi M, Inamoto S, Sakai Y (2019) Indocyanine green fluorescence-guided laparoscopic lateral lymph node dissection for rectal cancer. Dis Colon Rectum 62:1401
Malakorn S, Ouchi A, Sammour T, Bednarski BK, Chang GJ (2018) Robotic lateral pelvic lymph node dissection after neoadjuvant chemoradiation: view from the West. Dis Colon Rectum 61:1119–1120
Japanese Society for Cancer of the Colon and Rectum: General Rules for Clinical and Pathological Studies on Cancer of the Colon, Rectum, and Anus (9 th edn). Tokyo, Kanehara Shuppan, 2018.
Hajibandeh S, Hajibandeh S, Matthews J, Palmer L, Maw A (2020) Meta-analysis of survival and functional outcomes after total mesorectal excision with or without lateral pelvic lymph node dissection in rectal cancer surgery. Surgery S0039–6060(20):30282–30288
Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y et al (2018) Urinary dysfunction after rectal cancer surgery: results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212. Eur J Surg Oncol 44:463–468
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval
Ethics committee approval from our institution was obtained.
Consent to participate
Consent to participate from each patient was obtained.
Consent for publication
Consent for publication was obtained.
Availability of data and material
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 163028 KB)
Rights and permissions
About this article
Cite this article
Beppu, N., Jihyung, S., Takenaka, Y. et al. Laparoscopic lateral pelvic lymph node dissection combined with removal of the internal iliac vessels in rectal cancer: how to standardize this surgical procedure. Tech Coloproctol 25, 579–587 (2021). https://doi.org/10.1007/s10151-020-02387-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02387-3