Abstract
Purpose
The purpose of this study was to assess the feasibility of sentinel lymph node (SLN) detection in endometrial cancer patients with a dual-tracer procedure after hysteroscopic peritumoural injection.
Methods
Twenty-six women with previously untreated endometrial adenocarcinoma underwent the hysteroscopic injection of 111 MBq 99mTc-Nanocoll and blue dye administered subendometrially around the lesion. On the same day, all 26 patients underwent lymphoscintigraphy, followed 3–4 h later by hysterotomy with bilateral salpingo-oophorectomy and pelvic lymphadenectomy. Para-aortic lymphadenectomy was also performed in cases of either serous or papillary carcinoma (n=7/26). All SLNs were removed and examined with haematoxylin and eosin staining and immunohistochemical techniques.
Results
The procedure was well tolerated by patients, only two experiencing transient vagal symptoms. The sensitivity of this technique for correct identification of SLNs was 100%. Lymph node metastases were found in 4 out of the 26 patients (15%), bilaterally in the external iliac region (n=1), unilaterally in the external iliac region (n=1), unilaterally in the common iliac region (n=1) and unilaterally in the para-aortic region (n=1). In all four cases, nodal metastases were located within SLNs detected by lymphoscintigraphy. Only 10 of the 26 patients (38%) had significant blue dye staining. All blue-stained SLNs were radioactive.
Conclusion
In patients with endometrial cancer, it is feasible to use lymphatic mapping and SLN biopsy to define the topographic distribution of the lymphatic network and also to accurately detect lumbo-aortic and pelvic metastases within SLNs. In the majority of patients with early stage endometrial cancer, this procedure may avoid unnecessary radical pelvic lymphadenectomy. It may also guide para-aortic lymph node dissection on the basis of the SLN status.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In many tumours, lymph node staging is performed using various nuclear medicine procedures, including sentinel lymph node (SLN) biopsy and emission tomography. SLN biopsy has an established role in malignant melanoma [1] and its use is increasingly being validated in patients with gynaecological tumours that give rise to lymph node metastases, such as breast cancer [2], vulvar cancer [3] and cervical carcinoma [4]. The assessment of lymph nodes by lymphoscintigraphy and SLN biopsy may also be of interest in endometrial cancer for several reasons. This is the most frequent cancer among post-menopausal women and is the fourth most common gynaecological cancer in the USA and Europe. In patients with such tumours, lymph node status is the most important predictor for survival. The 5-year diseasefree survival in stage I patients with positive pelvic nodes has been reported to be 54%, as against 90% for those with negative nodes [5]. Metastatic nodal involvement may affect pelvic and para-aortic lymph nodes. To date, pelvic lymph node dissection has been performed on a routine basis, while para-aortic lymphadenectomy is not systematically carried out [6, 7]. In addition, in early stage endometrial cancer, the frequency of lymph node metastases is low (i.e. 6.8–18%), and the surgical morbidity is not negligible. However, only a few studies [8–14] have assessed the feasibility of lymphoscintigraphy and SLN biopsy in women with endometrial carcinomas. In these series, varying methodologies have been used with different results. The aim of the present study was to assess the feasibility of SLN detection in patients with proven endometrial cancer by use of a dual-tracer injection based on a subendometrial hysteroscopy technique as pioneered by Niikura et al. [15].
Materials and methods
Study population
Twenty-six previously untreated, consecutive patients with endometrial cancer (mean age 54 years, range 46–67) without any clinical evidence of lymphatic metastases and no concurrent and/or previous cancers, were enrolled in the study between 2002 and 2004. The study focussed on patients with early stage disease and a low probability of lymph node metastases. In these patients there is an indication for pelvic lymph node dissection but not for lumbo-aortic dissection. The exclusion criteria were preoperative histological diagnosis of clear cell carcinoma or serous papillary adenocarcinoma, risks related to anaesthesia, and preoperative and intra-operative evidence of distant metastasis. However, when the histological diagnosis of clear cell carcinoma or serous papillary adenocarcinoma was made at surgery, as occurred in 7 of the 26 patients examined, data were retained and are reported. The clinical diagnosis of endometrial cancer was achieved by a hysteroscopic examination. Lymphoscintigraphy was performed on the same day as surgery to identify the deep lymphatic basins that could not be recognised solely on the basis of clinical examination.
Technique
Tracer injection
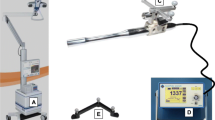
The radiopharmaceutical and blue dye (Monico S.p.A., Venezia/Mestre, Italy) were injected by hysteroscopy (Solima-Zupi hysteroscope; Wolf, Knitlingen, Germany) in the subendometrial layer of the uterine wall within 2–3 mm of the visible edge of the tumour. The radiopharmaceutical consisted of albumin nanocolloid particles ranging in size from 5 to 80 nm [16], labelled with 99mTc (Nanocoll; Nycomed Amersham Sorin S.r.l., Saluggia, Italy). Approximately 111 MBq of 99m Tc-Nanocoll in 5 ml of saline was administered in the subendometrial layer. The total dose of 111 MBq was established by starting from 37 MBq [17, 18] and then increasing this initial activity first two- and then threefold in the first three patients until the image quality and the nodal activity during the surgical procedure (in which a gamma probe was used) were deemed adequate. The injection was performed through a 23-gauge, 30-cm-long needle (code 6522IT; Bard Ltd., Crawley, Sussex, UK) to minimise the endometrial trauma. The depth of needle placement was assessed by visualisation of the endometrial elevation during injection. Penetration of the myometrium by the needle was avoided by paying attention to pain elicitation and to the increase in resistance to injection. The number of injections was three or four depending on the lesion site and shape, and the injections were placed around the cancer at approximately 90° or 120° to each other. After the administration of radiocolloid, a total volume of 8 ml of blue dye was injected in the peritumoural area at the same site as the radiopharmaceutical injection. Radiopharmaceutical and blue dye were injected concurrently, by means of separate injections and volumes, because the two tracers have a different kinetic behaviour and because transitory impairment of visibility at hysteroscopy may be observed following injection of blue dye owing to leakage into the uterus. No anaesthesia was used during the entire procedure.
Imaging
After administration, a 15-min dynamic planar acquisition was performed in the anterior view with a gamma camera (Prism 1000 XP; Picker, Cleveland, OH, USA) equipped with a low-energy general-purpose collimator; the acquisition window was set at 140 keV [19–22]. This initial acquisition was followed by sequential static imaging every 5 min for up to 1 h or until two or three SLNs had been identified. For dynamic images, the matrix size was 125×125, while for the static images it was 256×256. The static images in the anterior view included the entire pelvis. Posterior and/or oblique projections and lateral views were acquired after the last anterior projection acquisition in order to better identify the depth of the SLNs. Transmission images were acquired in the anterior view with a 57Co flood source [23] to assist in lymph node localisation. Finally, to facilitate the surgical resection, a reference mark was placed on the skin, corresponding to the position of the SLN visualised by lymphoscintigraphy with the help of the 57Co marker.
Surgical technique
Within 3–4 h of lymphoscintigraphy, patients underwent a hysterectomy with bilateral salpingo-oophorectomy and systematic pelvic lymphadenectomy. The pelvic lymphadenectomy entailed removal of the pelvic nodes from the common iliac vessels to the deep obturator fossae. If the tumour histology was found at surgery to be of either the serous or the clear cell type,para-aortic lymphadenectomy was performed; this event occurred in seven cases. The lymph nodes were isolated from the fatty tissue without freezing or preservation.
Gamma-detecting probe and lymph node biopsy
Following hysterectomy and bilateral salpingo-oophorectomy, but prior to lymphadenectomy, a crystal scintillator (CsI) gamma probe (C-Track System; Care-Wise, CA, USA) [24–26] was used intraoperatively to confirm the location of the SLN as seen on scintigraphy and using the images and skin mark as guides. The lymph node emitting the highest signal was recorded and identified as an SLN and then isolated for pathological examination. Following dissection, all surgical specimens were scanned by the probe to identify residual hot spots in the abdomen or in the lymphadenectomy specimen. In the event of focal accumulations of radioactivity, specimens were sent in separately as SLNs with progressive identification numbers. The threshold level was set at 80% of the radioactivity of the hottest SLN if the lymph node was close to the hottest node, and at 30% if the lymph node was far from the hottest node, in another lymphatic basin. All surgically removed lymph nodes were re-examined with the gamma probe ex vivo.
Pathological examination
All lymph nodes were removed from the fatty tissue without freezing or preservation and were examined using haematoxylin and eosin staining; in the case of serous papillary and clear cell tumours, the nodes were also examined immunohistochemically using anti-cytokeratin AE1/AE3 monoclonal antibody of the acidic and basic subfamilies. Nodes of at least 0.5 cm in diameter were dissected, and those smaller than 0.5 cm were fixed and embedded and cut. Three sections were obtained from each node (100–500 μm apart). The tumour was histologically classified according to the FIGO classification of endometrial cancer [27].
Results
The hysteroscopic procedures were considered satisfactory in visualising the uterine cavity before and during the injection of the tracers. The mean duration of the hysteroscopic procedure was 8 min (range 5–9 min). Patient compliance with the procedure was acceptable in all but two cases. Both of the latter patients presented a mild vagal reaction which resolved spontaneously. The tumour site distribution is shown in (Table 1). Eighteen patients (69%) had an endometrioid adenocarcinoma, four (16%) had a serous papillary adenocarcinoma, and three (11%) had a clear cell adenocarcinoma; one case (4%) was considered unclassifiable since while the diagnosis was supported by a biopsy sample, the final histological analysis revealed only necrotic tissue (Table 2). A total of 921 lymph nodes were dissected.
Scintigraphic results
Scintigraphy successfully identified SLNs in all patients (identification rate 100%) (Figs. 1, 2). In all patients, drainage to more than one lymphatic basin was observed, and the mean number of SLNs detected was three (range two to four). Sixty-five SLNs were first detected by lymphoscintigraphy and then using the radio-guided probe. The location and number of SLNs detected by radio-guided surgery are reported in Table 3. During surgery the SLN was consistently identified by both the radionuclide procedure and the patent blue dye technique in only ten patients (38%). No patients presented blue dye uptake in combination with negative 99m Tc-Nanocoll findings, and no cases of blue dye uptake in the para-aortic nodes were observed.
In only two cases were the SLNs identified with difficulty during surgery, as lymphoscintigraphy revealed at most very faint uptake of radioactivity. In one of these cases the injected activity was not sufficient, at less than 37 MBq, while in the other, bleeding occurred during the tracer injection, suggesting possible venous injection of the tracer. In the remaining cases, tracer uptake was sufficient to identify the SLN during surgery, though the uptake varied from 10 to 2,000 counts per second (cps). No correlation was found between the site of the SLN and the site of the tumour. The mean cumulative duration of intraoperative detection of the SLN and its dissection and removal was 23 min (range 17–31 min). In no case was there contamination of the peritoneum by blue dye or by 99mTc, appearing as tubal leakage of the tracers. No intraoperative complications were recorded. One patient was resubmitted to laparotomy for pelvic pain and pelvic lymphocele 3 weeks after discharge. These complications were related to lymphadenectomy.
Results of pathology
Lymph node metastases were identified in four of the 26 women by pathological examination of the 921 resected lymph nodes. These metastatic lymph nodes were localised bilaterally in the external iliac region in one patient, unilaterally in the external iliac region in one, unilaterally in the common iliac region in one and unilaterally in the para-aortic region in one. In all four cases, the nodal metastases were seen in lymph nodes depicted as SLNs by lymphoscintigraphy (Table 4).
The follow-up of the patients enrolled in the study ranges between 4 and 23 months; no relapses have been observed so far.
Discussion
This study aimed to assess the lymphatic drainage of the uterus and the feasibility of SLN biopsy in patients with endometrial cancer—a type of tumour in which metastases occur in deeply seated nodes and complete lymphadenectomy is usually performed. To this end, we tested a technique for lymphoscintigraphy and SLN detection in endometrial cancer based on the hysteroscopic peritumoural injection of 99mTc-labelled albumin nanocolloid.
The results of this study confirm the feasibility of the SLN technique in patients with endometrial cancer when performed by peritumoural tracer injection, and the possibility of achieving extensive visualisation of the lymphatic drainage and of SLNs. Moreover, it was demonstrated that the technique is applicable with minor patient discomfort during a routine hysteroscopic procedure on the same day as surgery.
In total, 65 SLNs were detected. It is of note that 14 of these 65 SLNs (21%) were found in the para-aortic basin, confirming that this is a primary pathway in lymphatic endometrial drainage and also that its visualisation by lymphoscintigraphy and intraoperative detection using a gamma probe are feasible.
In our series of patients the rate of SLN detection by 99mTc-Nanocoll was 100%, since every SLN seen on lymphoscintigraphy was found by the probe during surgery, whereas the sensitivity of nodal blue dye detection was only 38%. This low sensitivity represents a further limitation to the use of blue dye for SLN detection, over and above the laborious nature of the search for the SLN, which is possible only after peritoneal incision.
Pathological analysis demonstrated five lymph node metastases in 4 of 26 patients. All five metastatic lymph nodes were among the 65 identified as SLNs. Moreover, they were the only metastatic nodes among the 921 resected: no other lymph node was detected by histology as metastatic among those examined following complete lymphadenectomy. This result suggests that the detection and dissection of the SLN to assess the spread of metastases ensures proper nodal staging. Not only was it possible to visualise the para-aortic nodes, but in one patient in our series, who had serous papillary carcinoma, such visualisation led to the detection of the only metastatic lymph node. This result confirms the importance of para-aortic assessment especially in serous papillary carcinoma.
No discomfort was reported by patients during needle placement and tracer injection, probably because of the limited nociceptor distribution in the endometrium, even in the deepest layers. The use of hysteroscopy in patients with endometrial cancer entails potential risk owing to the possibility of tumour cell dissemination through the fallopian tubes and into the peritoneal cavity [28, 29]. To distend the uterine cavity during the hysteroscopic procedure, intrauterine pressure is applied. However, using hydrotubation, Baker and Adamson [30] found that the minimum intrauterine pressure required to distend the uterine cavity during hysteroscopy is less than 40 mmHg, which is lower than the pressure at which spillage from the fallopian tubes occurs (no spill occurred at pressures <70 mmHg). Using this technique, positive peritoneal cytology for neoplastic cells was obtained in only one case; furthermore, positive peritoneal cytology is not clearly recognised as an independent prognostic factor in endometrial adenocarcinoma [31]. Based on these data we believe that our technique is technically safe and does not entail a risk of iatrogenic upstaging that would potentially have a negative impact on the final outcome.
Only a few studies have focussed on SLN detection in endometrial cancer. In the studies of Pelosi et al. [9] and Barranger et al. [14], 99mTc-Nanocoll and blue dye were injected in the pericervical region. Laparoscopic nodal dissection under gamma probe guidance enabled the recognition of SLNs within the pelvic lymphatic system, the sensitivity for SLN detection being 100% in each of the studies. However, use of pericervical injection for all patients, regardless of the tumour location, could have resulted in failure to detect aortic SLNs (and possible lymphatic metastases), i.e. false negative findings may have been acquired in some cases that could have been detected had para-aortic lymph node dissection been performed.
Burke et al. [8] injected the tracer in the uterus trans-serosally at three mid-line sites, irrespective of the tumour site. They used only blue dye and recognised an SLN in just 70% of cases. Niikura et al. [15] were the first to employ hysteroscopic injection, injecting 99mTc-labelled sulphur colloid dissolved with patent blue dye into the peritumoural endometrium on the day preceding surgery. They used blue dye not to detect SLNs but to ensure injection in the subendometrial layer without leakage. They detected SLNs in the para-aortic region in 18 of 25 patients, with a sensitivity and specificity of 100%. The present study confirms and extends our own preliminary results and highlights the importance of peritumoural tracer injection in ensuring that para-aortic SLNs are not overlooked. Our results are in agreement with the findings of Niikura et al. [15], who detected different lymphatic pathways draining from the uterine cervix and the corpus uteri. In the latter case, the para-aortic basin is frequently involved, and tracer injection in the peritumoural area becomes mandatory for assessing the para-aortic nodes. Building on previous work [5, 6, 11], this study demonstrates the possibility of detecting para-aortic SLNs by peritumoural injection, thereby allowing correct disease staging and offering the potential for tailored lymphadenectomy.
This study was conceived to assess the feasibility of a 1-day procedure based on peritumoural radiopharmaceutical injection for the visualisation of the nodal basins in patients undergoing a standardised predefined surgical protocol for endometrial cancer. The intention was to include only patients with early and not very aggressive forms of endometrial cancer. However, some patients with serous papillary or clear cell endometrial cancer were included because the diagnosis was made at surgery. Patients with early stage endometrial cancer have a low incidence of nodal metastases and, given the preoperative assumption of low aggressiveness, it was not anticipated that systematic para-aortic lymphadenectomy would be necessary in our patients. In the event, para-aortic lymph nodes were dissected only in those patients found to have serous papillary and clear cell endometrial cancer. Given that surgical procedures varied among patients owing to differences in the type of disease, this study must be considered preliminary and to have had the principal aim of assessing the feasibility of the procedure rather than its clinical value. Indeed, the findings of the present study do not allow conclusions to be drawn regarding the predictive value of SLN biopsy in endometrial adenocarcinoma. To this end, a multicentre study aimed at systematic assessment of the predictive value of SLN biopsy with respect to para-aortic lymph nodes is in progress.
Conclusion
In patients with endometrial cancer, SLN dissection with hysteroscopic peritumoural tracer injection is feasible in a 1-day procedure. Such a technique may reduce the use of radical pelvic lymphadenectomy while achieving accurate nodal staging with a low morbidity. In addition, the procedure allows the detection of para-aortic lymph node metastases. Prospective multicentre studies with a large number of patients are needed to assess the predictive value of SLN biopsy in endometrial cancer.
References
Estourgie SH, Nieweg OE, Valdes Olmos RA, Hoefnagel CA, Kroon BB. Review and evaluation of sentinel node procedures in 250 melanoma patients with a median follow-up of 6 years. Ann Surg Oncol 2003;10:681–8.
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 2003;349:546–53.
Makar AP, Scheistroen M, van den Weyngaert D, Trope CG. Surgical management of stage I and stage II vulvar cancer: the role of the sentinel node biopsy. Review of literature. Int J Gynecol Cancer 2001;11:255–62.
Dargent D, Martin X, Mathevet P. Laparoscopic assessment of the sentinel lymph node in early stage cervical cancer. Gynecol Oncol 2000;79:411–5.
Lurain JR, Rice BL, Rademaker AW, Poggensee LE, Schink JC, Miller DS. Prognostic factors associated with recurrence in clinical stage I adenocarcinoma of the endometrium. Obstet Gynecol 1991;78:63–9.
Belinson JL, Lee KK, Badger GJ, Pretorius RG, Jarrell MA. Clinical stage I adenocarcinoma of the endometrium—analysis of recurrences and the potential benefit of staging lymphadenectomy. Gynecol Oncol 1992;44:17–23.
Benedetti Panici PL, Scambia G, Baiocchi G, Greggi S, Mancuso S. Technique and feasibility of radical para-aortic and pelvic lymphadenectomy for gynaecologic malignancies: a prospective study. Int J Gynecol Cancer 1991;1:133–40.
Burke TW, Levenback C, Tornos C, Morris M, Wharton JT, Gershenson DM. Intraabdominal lymphatic mapping to direct selective pelvic and paraaortic lymphadenectomy in women with high-risk endometrial cancer: result of a pilot study. Gynecol Oncol 1996;62:169–73.
Pelosi E, Arena V, Baudino B, Belló M, Giusti M, Gargiulo T, et al. Pre-operative lymphatic mapping and intra-operative sentinel lymph node detection in early stage endometrial cancer. Nucl Med Commun 2003;24(9):971–5.
Holub Z, Jabor A, Kliment L. Comparison of two procedures for sentinel lymph node detection in patients with endometrial cancer: a pilot study. Eur J Gynecol Oncol 2002;23:53–7.
Zambo K, Koppan M, Paal A, Schmidt E, Tinneberg HR, Bodis J. Sentinel lymph nodes in gynaecological malignancies: frontline between TNM and clinical staging system? Eur J Nucl Med Mol Imaging 2003;30(12):1684–8.
Fersis N, Gruber I, Relakis K, Friedrich M, Becker S, Wallwiener D, et al. Sentinel node identification and intraoperative lymphatic mapping. First results of a pilot study in patients with endometrial cancer. Eur J Gynaecol Oncol 2004;25(3):339–42.
Gargiulo T, Giusti M, Bottero A, Leo L, Brokaj L, Armellino F, et al. Sentinel lymph node (SLN) laparoscopic assessment early stage in endometrial cancer. Minerva Ginecol 2003;55(3):259–62.
Barranger E, Cortez A, Grahek D, Callard P, Uzan S, Darai E. Laparoscopic sentinel node procedure using a combination of patent blue and radiocolloid in women with endometrial cancer. Ann Surg Oncol 2004;11:344–9.
Niikura H, Okamura C, Utsunomiya H, Yoshinaga K, Akahira J, Ito K, Yaegashi N. Sentinel lymph node detection in patients with endometrial cancer. Gynecol Oncol 2004;92:669–74.
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 2003;349:546–53.
Glass EC, Essner R, Morton DL. Kinetics of three lymphoscintigraphic agents in patients with melanoma. J Nucl Med 1998;38:1185–90.
Morton DL, Wen DR, Wong JH, Economu JS, Cagle LA, Storm FK, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–9.
Giuliano AE, Kirgan DM, Geunther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg 1994;220:391–401.
Alex JC, Krag DN. Gamma probe-guide localization of lymph nodes. Surg Oncol 1993;2:137–43.
Alex JC, Weaver DL, Fairbank JT, Rankin BS, Krag DN. Gamma-probe-guided lymph node localization in malignant melanoma. Surg Oncol 1993;2:303–8.
Van der Veen H, Hoekstra OS, Paul MA, Cuesta MA, Meijer S. Gamma probe-guided sentinel node biopsy to select patients with melanoma for lymphadenectomy. Br J Surg 1994;81:1769–70.
Kapteijn BA, Nieweg OE, Liem I, Mooi WJ, Balm AJ, Muller SH, et al. Localizing the sentinel node in cutaneous melanoma: gamma-probe detection versus blue-dye. Ann Surg Oncol 1997;4:156–60.
Alazraki N, Glass EC, Castronovo F, Olmos RA, Podoloff D. Procedure guideline for lymphoscintigraphy and the use of intraoperative gamma probe for sentinel lymph node localization in melanoma of intermediate thickness 1.0. J Nucl Med 2002;43(10):1414–8.
Zanzonico P, Heller S. The intra-operative gamma probe: basic principles and choices available. Semin Nucl Med 2000;30:33–48.
Kopp J, Wengenmair H, Vogt H, Heidenreich P. Intra-operative gamma-probe: performance of commercially available systems- a comparison. Eur J Nucl Med 1999;26 Suppl 4:S59, S.03.04.
FIGO news. Corpus cancer staging. Int J Obstet 1989;28:190.
Obermair A, Geramou M, Gucer F, Denison U, Graf AH, Kapshammer E, et al. Does hysteroscopy facilitate tumor cell dissemination? Cancer 2000;88:139–43.
Selvaggi L, Cormio G, Ceci O, Loverro G, Cazzolla A, Bettocchi S. Hysteroscopy does not increase the risk of microscopic extrauterine spread in endometrial carcinoma. Int J Gynecol Cancer 2003;13:223–7.
Baker VL, Adamson GD. Threshold intrauterine perfusion pressures for intraperitoneal spill during hydrotubation and correlation with tubal adhesive disease. Fertil Steril 1995;64:1066–9.
Kasamatsu T, Onda T, Katsumata N, Sawada M, Yamada T, Tsunematsu R, et al. Prognostic significance of positive peritoneal cytology in endometrial carcinoma confined to the uterus. Br J Cancer 2003;88:245–50.
Acknowledgements
The authors appreciate the assistance of the technologists Mrs. Monica Testoni and Mrs. Elena Fraigola in the standardisation of the technical procedures. The authors are grateful to Mrs. Annaluisa De Simone Sorrentino for her help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maccauro, M., Lucignani, G., Aliberti, G. et al. Sentinel lymph node detection following the hysteroscopic peritumoural injection of 99mTc-labelled albumin nanocolloid in endometrial cancer. Eur J Nucl Med Mol Imaging 32, 569–574 (2005). https://doi.org/10.1007/s00259-004-1709-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1709-4