Abstract
N-myc downstream regulated gene 1 (NDRG1) is a member of the N-myc downstream regulated gene family which belongs to the alpha/beta hydrolase superfamily. Earlier studies have shown its association with inhibition of tumor metastasis. However, its function in malignant tumors is not fully enunciated. Recently there was increasing evidence that NDRG1 is involved in stress responses. In the current study, we examined the expression of NDRG1 and its correlation with clinicopathological factors and microvessel density (MVD) in non-small cell lung cancer (NSCLC) using immunohistochemistry (IHC). NDRG1 expression in NSCLC (71/115, 61.7%) was higher than that in normal lung tissues (32/115, 27.8%) (p < 0.05). NDRG1 expression in NSCLC cells was found in cytoplasm (63/115, 54.8%), nuclear (24/115, 20.9%) and cell membrane (13/115, 11.3%). NDRG1 expression in NSCLC with advanced T stages (T2-4) (63/84, 75.0%) was significantly higher than that with T1 stage (8/31, 25.8%) (P < 0.05). No other clinicopathological factors including lymph node metastasis were found to be associated with NDRG1 expression (p > 0.05). Moreover increased NDRG1 expression was associated with lower MVD in NSCLC (P < 0.05). MVD in adenocarcinoma (33.4 ± 8.4/HP) was significantly higher than that in squamous cell carcinoma (SCC) (19.3 ± 8.1/HP) (P < 0.05). No other clinicopathological factors were associated with MVD in NSCLC (p > 0.05). The present findings indicate an increase of NDRG1 expression with the progress of tumour extent which may be due to unbalanced tumor oxygenation on account of poor vascularization in NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
N-myc downstream regulated gene 1 (NDRG1) is known as a differentiation-related gene that plays important roles in cell differentiation and organ formation [1–3]. Diverse pathological conditions such as neoplasia modulate NDRG1 transcription, mRNA stability, and translation [4–6]. The expression of NDRG1 gene is induced by nickel which may create hypoxia-like conditions in cells and induce hypoxia-responsive genes [7, 8]. Thus NDRG1 is likely to be another gene induced by hypoxia. The process of tumor expansion is characterized by rapid growth of cancer cells as the tumor establishes itself in the host. Accompanying this rapid growth are alterations in the cancer cell microenvironment, typically caused by an inability of local vasculature to supply enough oxygen and nutrients to the rapidly dividing tumor cells. This makes hypoxia one common feature of solid tumors. Exploration of NDRG1 protein expression patterns in various tissues showed that NDRG1 protein was overexpressed in cancers compared to normal tissues, but it’s clinical significance including effect on tumor metastasis remains controversial [9–12]. Furthermore significance of NDRG1 expression in non-small cell lung cancer (NSCLC) tissues is not clearly documented. In the current study, we aim to investigate NDRG1 expression and analyze its association with clinicopathological factors and vascularization in NSCLC.
Materials and Methods
Tissue Samples
Tumor specimens including NSCLC tissues and paired non-tumor portion (with >5 cm distance from the primary tumor’s edge) from 115 patients with NSCLC were obtained between 2001 and 2005 following surgical resection at the First Affiliated Hospital of China Medical University. None of the patients had received radiotherapy, chemotherapy, or immunotherapy prior to tumor excision. Of the patients, 72 are male and 43 are female, creating a 1.67:1 ratio of male to female. Patients’ ages at the time of surgery ranged from 22 to 79, with an average age of 58.7 years old. The tumors were classified according to the TNM stage revised by the International Union Against Cancer (UICC) in 2002 [13]. All specimens were re-evaluated for diagnosis following the criteria for classification of lung cancer by the World Health Organization (WHO) [14], and 47 squamous cell carcinomas (SCCs), 61 adenocarcinomas, 5 large cell carcinomas and 2 adenosquamous carcinomas were confirmed. This study was conducted under the regulations of the Institutional Review Board of China Medical University. Informed consent was obtained from all enrolled patients prior to surgery.
Immunohistochemistry (IHC)
Formalin-fixed, paraffin-embedded specimens were cut into 4 μm-thick sequential sections. The sections were dewaxed in xylene and rehydrated stepwise in ethanol. Then the sections were boiled in citrate buffer (pH 6.0) for 90 s within an autoclave. Endogenous peroxidase activity and non-specific binding were blocked with 3% H2O2 and non-immune sera, respectively. The sections were then incubated with primary rabbit anti-human NDRG1 polyclonal antibody (ab63989, Abcam, Cambridge, UK; dilution 1:100) and mouse anti-human CD34 monoclonal antibody (ab8536, Abcam, Cambridge, UK; dilution 1:100) overnight at 4°C. Thereafter, the catalyzed signal amplification system (Maixin Biotechnology, Fuzhou, Fujian, China) was used for NDRG1 and CD34 staining according to the manufacturer’s instructions. The antibodies were detected by a standard avidin-biotin complex method with a biotinylated rabbit anti-mouse antibody (Maixin) and an avidin-biotin complex (Maixin), and developed with diaminobenzidine. Counterstaining was done lightly with hematoxylin, and the sections were dehydrated in alcohol before mounting. Appropriate negative (obtained by omission of the primary antibodies) and positive (obtained by experiments on slides of human hepatocellular carcinomas under the same conditions above at the same time) controls were used throughout.
The sections were assessed by three observers (CF Fan, JH Yu and Y Liu) who had no knowledge of the patients’ clinical status. Cases with discrepancies were jointly re-evaluated by the investigators, and a consensus was obtained. Scoring of immunohistochemistry was based on two parameters: the proportion of immunopositive cells and their intensity of immunoreactivity. The proportion of immunopositive cells was categorized as follows: 0: <10%; 1: ≥10% to <25%; 2: ≥25% to <50%; 3: ≥50% to <75% and 4: ≥75%. The staining intensity was categorized by relative intensity as follows: 0: no positivity; 1: weak; 2: moderate and 3: strong. A final immunoreactivity score of each section was obtained by multiplying the two individual scores. To obtain final statistical results, a final score less than 2 was considered as negative, while scores of 2 or more were considered as positive.
Assessment of Microvessel Density (MVD)
MVD of the 115 NSCLC tissues was determined using CD34 antibody by IHC. MVD was assessed according to Weidner et al. [15]. The hot spots were selected under a microscope (40×), then individual microvessel counts were made under 200× field (Olympus BH-2 microscope, 0.74 mm2 per field). The average counts in 5 fields were recorded. Any single highlighted endothelial cell or endothelial cell cluster clearly separated from adjacent microvessel, and distinct clusters of brown-stained endothelial cells were counted as separate microvessels. Vessel lumens were not the sole criteria in identifying a microvessel. The vessels with area more than the diameter of 8 red cells, and the vessels with thick tunica media were not considered microvessel.
Statistical Analysis
The Pearson’s Chi-Square test was used to analyze the relationship between NDRG1 expression and clinicopathological factors. The McNemar’s test was used to compare NDRG1 expression in normal lung tissues and lung cancer tissues. T test and Chi-Square test were used to analyze the association between NDRG1 expression and MVD in NSCLC. T test was used to analyze the relationship between MVD and clinicopathological factors. SPSS statistical software package version 13.0 (SPSS Inc., Chicago, IL, USA) was used for all analyses. P-values of <0.05 were considered statistically significant.
Results
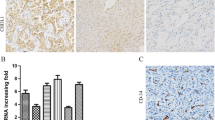
NDRG1 Expression in Normal Lung Tissues and NSCLC
Normal lung tissue cells (including alveolar Type 2 cells and bronchial epithelial cells examined) and NSCLC cells both showed cytoplasm, cell membrane and nuclear staining of NDRG1 (Fig. 1). Total positive rate of NDRG1 expression in normal lung tissues was 27.8% (32/115), with a positive rate of 18.3% (21/115) in alveolar Type 2 cells and 25.2% (29/115) in bronchial epithelial cells. NDRG1 was positive in both alveolar Type 2 cells and bronchial epithelial cells in 18 cases. NDRG1 expression in NSCLC (71/115, 61.7%) was higher than that in normal lung tissues (p < 0.05). Separately, NDRG1 expression in SCC (32/47, 68.1%) was higher than that in bronchial epithelial cells, while NDRG1 expression in adenocarcinoma (37/61, 60.7%) was higher than that in alveolar Type 2 cells (both p < 0.05). NDRG1 expression in cytoplasm of NSCLC cells (63/115, 54.8%) was higher than that in nuclear (24/115, 20.9%) and cell membrane (13/115, 11.3%) (p < 0.05). NDRG1 expression in cytoplasm of cancer cells was associated with that in nuclear and cell membrane respectively (both p < 0.001) but NDRG1 expression in nuclear was not associated with that in cell membrane (p > 0.05). All 13 cases with positve cell membrane stain were also with cytoplasm stain but in the 24 cases with positive nuclear stain there were 8 cases without cytoplasm stain of NDRG1. There were 3 cases of NSCLC showing all cytoplasm, cell membrane and nuclear stain of NDRG1.
NDRG1 expression in normal lung tissues and non-small cell lung cancer tissues. a in alveolar Type 2 cells (cytoplasm stain). b in bronchial epithelial cells (mainly in cytoplasm and membrane with weak stain in some nuclears). c, d in squamous cell carcinoma. Positive stain was seen in cytoplasm and membrane (c); cytoplasm and nuclear (d). e, f in lung adenocarcinoma. Positive stain was seen in cytoplasm and membrane (e); cytoplasm, nuclear and membrane (f). (×400)
Relationship Between NDRG1 Expression and Clinicopathological Factors in NSCLC
The relationship between NDRG1 expression and different clinicopathological factors in NSCLC is shown in Table 1. NDRG1 expression in NSCLC with advanced T stages (T2-4) (63/84, 75.0%) was significantly higher than that with T1 stage (8/31, 25.8%) (P < 0.05). When we analyzed NDRG1 expression in cytoplasm in NSCLC a similar significant correlation between it and T stages was also found (67.9% (57/84) versus 19.4% (6/31), P < 0.05). No other clinicopathological factors including lymph node metastasis were found to be associated with NDRG1 expression (P > 0.05). There was no significant association between NDRG1 expression in nuclear or membrane and any of the clinicopathological factors in NSCLC.
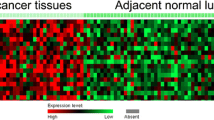
MVD and Association with Clinicopathological Factors and NDRG1 Expression in NSCLC
Brown-stained CD34 protein expression was located in the microvessels (Fig. 2). Distribution of microvessels in sections of NSCLC was illustrated in Fig. 3. The average MVD in 115 cases of NSCLC was 27.1 ± 8.2/HP (ranged from 6.4 to 54.6). Relationship between MVD and different clinicopathological factors in NSCLC is shown in Table 2. MVD in adenocarcinoma (33.4 ± 8.4/HP) was significantly higher than that in squamous cell carcinoma (19.3 ± 8.1/HP) (P < 0.05). No other clinicopathological factors were associated with MVD in NSCLC (p > 0.05). A significant negative correlation was found between NDRG1 expression and MVD in NSCLC. The NDRG1 expression rate in cases with MVD below median MVD (27.1/HP) was significantly higher than that in cases with MVD equal to and over median MVD (P < 0.05) (Table 3). The value of MVD in NDRG1(+) cases (23.8 ± 9.6/HP) was significantly lower than that in NDRG1(-) cases (32.5 ± 7.3/HP) (P < 0.05) (Table 3 and Fig. 4)
Discussion
In earlier studies NDRG1 expression was found to be reduced in some malignant tumors including prostate cancer and breast cancer compared to the non-cancerous tissues of the same origin [16, 17]. Paradoxically, findings relating to the expression of NDRG1 are not always consistent with this tenet. Mei-Sze et al. [12] found that NDRG1 was significantly highly expressed in hepatocellular carcinoma compared to nontumor liver. In many other malignant tumors such as oral squamous cell carcinoma NDRG1 expression was also found to be upregulated [9, 10]. In our study, we also found NDRG1 expression in NSCLC was higher than that in relevant normal lung tissues. Expression of NDRG1 may be tissue- or cell-type specific. The controversy may be attributed in part to the fact that NDRG1 expression is highly influenced by pleiotropic factors and stimuli, including various metal ions, hypoxia, oncogenes, tumorsuppressor genes, hormones, and vitamins. For example, NDRG1 expression in prostate cancer cells is influenced by androgens [18], whereas that in breast cancer cells depends primarily on estradiols [17].
Hypoxia is a common characteristic and a key stimulus in the pathophysiology of many solid tumors including NSCLC. Kokame et al. [19] demonstrated that the sulfhydryl group-containing amino acid, homocysteine, upregulates the expression of NDRG1 which indicates a link of this gene to stress-response. Sonja et al. [11] found that hypoxia increases cytoplasmic expression of NDRG1 in human hepatocellular carcinoma. These findings lend further insights to understanding of the high level of NDRG1 expression in many solid tumors. In the present study, we found NDRG1 was highly expressed in NSCLC compared to adjacent normal lung tissues. To find out whether the high expression of NDRG1 may be cosequence of hypoxia in NSCLC, we also investigated vascularization and its correlation with NDRG1 expression. It is commonly believed that the stroma carries the blood supply and is crucial to the growth of the neoplasm. Therefore the vascular distribution directly determins the conditon of oxygen supply in the neoplasm. There are several reports that have linked NDRG1 expression with neovascularization in malignant tumors. Shin et al. [20] found high NDRG1 expression was closely associated with high angiogenic activity in cervical adenocarcinoma. In the study they found a positve relationship between NDRG1 and vascular endothelial growth factor in the tumor. While in Maruyama et al’s study they found NDRG1 overexpression was associated with reduced tumor-induced angiogenesis in pancreatic cancer [21]. In our study we found a negative correlation between NDRG1 expression with MVD in NSCLC. Though tumor growth depends on the angiogenesis, its rate often fails to keep pace with tumor growth. Therefore, many solid tumors have subpopulations of hypoxic cells. The upregulation of NDRG1 expression due to poor vascularization in tumor is consistant with the findings that NDRG1 is involed in stress response caused by many stimuli, such as metal ions which may create hypoxia-like conditions [7, 8]. It is reasonable to consider the upregulated expression of NDRG1 in NSCLC in our study as a response to hypoxia in cancer tissues. But whether NDRG1 has a role to affect angiogenesis in NSCLC in vivo still needs further investigation.
Bandyopadhyay et al. [16] found the level of NDRG1 expression was inversely related with the Gleason grade of prostate cancer. The author [17] also found a negative correlation between NDRG1 expression and metastasis in breast cancers. Guan et al. [22] reported higher NDRG1 mRNA levels in primary colon cancers than their metastases. These findings indicate NDRG1 may play important roles in inhibition of cancer metastasis. However, the function of NDRG1 associated with tumor metastasis remains contraversial. In Mei-Sze et al’s study [12] overexpression of NDRG1 was found to be an indicator of poor prognosis in hepatocellular carcinoma. In their study, they demonstrated using IHC that hepatocellular carcinomas with vascular invasion express elevated levels of NDRG1 protein compared to those without vascular invasion. Actually in our current study we found that the tumors with lymph node metastasis had lower NDRG1 expression though it was not statistically significant (p = 0.062). As metastasis of malignant tumors is dependent on angiogenesis, poor vascularization which leads to hypoxic conditions in tumors is not favourable for metastasis. As we didn’t investigate lymphatic microvessel density in our study so we don’t know if it is associated with MVD. Actually several studies have shown that highly vascularised tumors have a significantly higher likelihood to present with loco-regional lymph node metastasis than those that are poorly vascularised [23–25]. We can only assume that lymphatic microvessel density may have similar alterations in NSCLC like MVD. Thus we can infer from our findings that the upregulation of NDRG1 expression which is associated with poor vascularization in NSCLC is not enough to be an evidence that NDRG1 has a role related to tumor metastasis supressor but may be consequence of stress response to hypoxia due to poor vascularization which is not favorable for metastasis.
In many studies MVD was investigated to assess it’s clinical significance in neoplasm including NSCLC [23–31]. Some studies found that increasing neovascularization was correlated with an increased rate of local and distant metastasis [23–25, 27, 28]. Our results show that NSCLC with lymph node metastasis has higher MVD though it’s not significant (p = 0.058). Like many other reports we didn’t find significant association between MVD and tumor extent in NSCLC. But actually in our study MVD in NSCLC with T1 stage was higher than that in advanced T stages (p = 0.085). Eberhard et al. [27] have shown that in glioblastomas, renal cell carcinomas, colon carcinomas, mammary carcinomas and lung carcinomas, the microvessel density of the tumors was lower than that of the corresponding nongrowing normal tissues. Sardari et al. [31] found that growth index was independent of microvessel density in non-small cell lung carcinomas. These findings indicate that microvessel density levels do not reflect growth rate though it frequently increases during tumor progression to accommodate an increased metabolic demand. There may be some distinct molecular mechanism in neoplasm different from normal tissues protecting tumor cells against hypoxia. On the other hand, as unbalanced angiogenesis is often seen in neoplasm and poor vascularization may reflect frequent hypoxic conditions which can lead to necrosis during tumor growth, higher MVD in earlier T stage of NSCLC indicates that this size range may be an ideal condition for tumors to receive nutritional supply from the circulation.
Tumor cells are known to tolerate oxygen deprivation and to be resistant to apoptosis under hypoxic conditions. Whether and how NDRG1 may be involed in the mechanism is becoming a new focus in research work relating to this gene. In recent studies, NDRG1 was also found to play certain roles in apoptosis. Zheng et al. [32] found that ectopic expression of NDRG1 could delay the apoptosis of leukemic cells treated by camptothecin analog. Theses results give more proofs to the suggestion that NDRG1 may play a cytoprotective role upon exposure to conditions such as hypoxia that lead to stress response. Whether NDRG1 expression can promote tumor growth remains controversial [12, 21, 33]. In this study we found a positive correlation between NDRG1 expression and tumor extent in NSCLC, but it can not lead to conclusion that NDRG1 may directly promote tumor growth. As MVD in NSCLC was not significantly associated with tumor extent in our study, we can’t attribute the increasing NDRG1 expression completely to tumor growth. On the other hand, our findings support the assumption though not enough to prove it that increasing NDRG1 expression may have positive effect on tumor growth which may be due to a possible cytoprotective role of NDRG1 in stress response. There are reports showing that NDRG1 expression is translocated within cells in response to exogenous stimuli [11, 33]. In our study increased NDRG1 expression was mainly found in cytoplasm of NSCLC cells. While NDRG1 expression in membrane and nuclear of NSCLC cells was associated with that in cytoplasm. Whether NDRG1 expression in membrane and nuclear has function in neoplasm is yet unknown, though we didn’t find any significant association between it and clinicopathological factors in NSCLC.
In conclusion, our findings suggest that the overexpression of NDRG1 was a common abnormality in NSCLC and could be consequence of hypoxia in NSCLC tissues. Moreover upregulated NDRG1 expression in NSCLC may in turn be favorable for tumor growth. However how NDRG1 expression in malignant tumors is modulated and functions still needs more investigations. Future studies on the regulation of NDRG1 and its potential role in the stress response of NSCLC will be helpful for further understanding of the progress of this malignant tumor.
Abbreviations
- NDRG1:
-
N-myc downstream regulated gene 1
- MVD:
-
Microvessel density
- NSCLC:
-
Non-small cell lung cancer
- IHC:
-
Immunohistochemistry
- UICC:
-
International Union Against Cancer
- WHO:
-
World Health Organization
- SCC:
-
Squamous cell carcinoma
References
Lachat P, Shaw P, Gebhard S et al (2002) Expression of NDRG1, a differentiation-related gene, in human tissues. Histochem Cell Biol 118:399–408
Taketomi Y, Sugiki T, Saito T et al (2003) Identification of NDRG1 as an early inducible gene during in vitro maturation of cultured mast cells. Biochem Biophys Res Commun 306:339–346
Wakisaka Y, Furuta A, Masuda K et al (2003) Cellular distribution of NDRG1 protein in the rat kidney and brain during normal postnatal development. J Histochem Cytochem 51:1515–1525
Rutherford MN, Bayly GR, Matthews BP et al (2001) The leukemogenic transcription factor E2a-Pbx1 induces expression of the putative N-myc and p53 target gene NDRG1 in Ba/F3 cells. Leukemia 15:362–370
Angst E, Sibold S, Tiffon C et al (2006) Cellular differentiation determines the expression of the hypoxia-inducible protein NDRG1 in pancreatic cancer. Br J Cancer 95:307–313
Echaniz-Laguna A, Degos B, Bonnet C et al (2007) NDRG1-linked Charcot-Marie-Tooth disease (CMT4D) with central nervous system involvement. Neuromuscul Disord 17:163–168
Zhou D, Salnikow K, Costa M (1998) Cap43, a novel gene specially induced by Ni2+ compounds. Cancer Res 58:2182–2189
Salnikow K, Blagosklonny MV, Ryan H et al (2000) Carcinogenic nickel induces genes involved with hypoxic stress. Cancer Res 60:38–41
Hakan C (2004) Hypoxia upregulates the expression of the NDRG1 gene leading to its overexpression in various human cancers. BMC Genet 5:27
Joseph TC, Hung-Ming W, Ku-Wei C et al (2005) Identification of differentially expressed genes in oral squamous cell carcinoma (OSCC): Overexpression of NPM, CDK1 and NDRG1 and underexpression of CHES1. Int J Cancer 114:942–949
Sonja S, Vincent R, Adrian K et al (2007) Hypoxia increases cytoplasmic expression of NDRG1, but is insufficient for its membrane localization in human hepatocellular carcinoma. FEBS Lett 581:989–994
Mei-Sze C, Hongbo S, Siu TC et al (2007) Overexpression of NDRG1 is an indicator of poor prognosis in hepatocellular carcinoma. Mod Pathol 20:76–83
Sobin DHWC (2002) International Union Against Cancer (UICC): TNM Classification of Malignant Tumors, 6. Wiley-Liss, New York
Travis WDBE, Muller-Hermelink HK, Harris CC (2004) World health organization classification of tumors: pathology and genetics of tumors of the lung, pleura, thymus and heart. IARC, Lyon
Weidner N, Semple JP, Welch WR et al (1991) Tumor angiogenesis and metastasis-correlation in invasive breast carcinoma. N Engl J Med 324:1–8
Bandyopadhyay S, Pai SK, Gross SC et al (2003) The Drg-1 gene suppresses tumor metastasis in prostate cancer. Cancer Res 63:1731–1736
Bandyopadhyay S, Pai SK, Hirota S et al (2004) Role of the putative tumor metastasis suppressor gene Drg-1 in breast cancer progression. Oncogene 23:5675–5681
Ulrix W, Swinnen JV, Heyns W et al (1999) The differentiation-related gene 1, Drg1, is markedly upregulated by androgens in LNCaP prostatic adenocarcinoma cells. FEBS Lett 455:23–26
Kokame K, Kato H, Miyata T (1996) Homocysteine-respondent genes in vascular endothelial cells identified by differential display analysis. GRP78/BiP and novel genes. J Biol Chem 271:29659–29665
Shin N, Kimio U, Naotake T et al (2008) Cap43/NDRG1/Drg-1 is a molecular target for angiogenesis and a prognostic indicator in cervical adenocarcinoma. Cancer Letters 264:36–43
Maruyama Y, Ono M, Kawahara A et al (2006) Tumor growth suppression in pancreatic cancer by a putative metastasis suppressor gene Cap43/NDRG1/Drg-1 through modulation of angiogenesis. Cancer Res 66:6233–6242
Guan RJ, Ford HL, Fu Y et al (2000) Drg-1 as a differentiation-related, putative metastatic suppressor gene in human colon cancer. Cancer Res 60:749–755
Macchiarini P, Fontanini G, Hardin MJ et al (1992) Relation of neovascularisation to metastasis of non-small cell lung cancer. Lancet 340:145–146
Fontanini G, Bigini D, Vignati S et al (1995) Microvessel count predicts metastatic disease and survival in non-small cell lung cancer. J Pathol 177:57–63
Maeda K, Chung YS, Takatsuka S et al (1995) Tumor angiogenesis as a predictor of recurrence in gastric carcinoma. J Clin Oncol 13:477–481
Yamazaki K, Abe S, Takekawa H et al (1994) Tumor angiogenesis in human lung adenocarcinoma. Cancer 74:2245–2250
Anne E, Sebastian K, Valentin G et al (2000) Heterogeneity of angiogenesis and blood vessel maturation in human tumors: implications for antiangiogenic tumor therapies. Cancer Res 60:1388–1393
Fumihiro T, Hiroki O, Kazumasa T et al (2003) Glomeruloid microvascular proliferation is superior to intratumoral microvessel density as a prognostic marker in non-small cell lung cancer. Cancer Res 63:6791–6794
Guo J, Higashi K, Ueda Y et al (2006) Microvessel density: correlation with 18F-FDG uptake and prognostic impact in lung adenocarcinomas. J Nucl Med 47:419–425
Trivella M, Pezzella F, Pastorino U et al (2007) Microvessel density as a prognostic factor in non-small-cell lung carcinoma: a meta-analysis of individual patient data. Lancet Oncol 8:488–499
Sardari NP, Stessels F, Pezzella F et al (2003) Growth index is independent of microvessel density in non-small cell lung carcinomas. Hum Pathol 34:959–960
Zheng Y, Wang LS, Xia L et al (2009) NDRG1 is down-regulated in the early apoptotic event induced by camptothecin analogs: the potential role in proteolytic activation of PKC delta and apoptosis. Proteomics 9:2064–2075
Kurdistani SK, Arizti P, Reimer CL et al (1998) Inhibition of tumor cell growth by RTP/rit42 and its responsiveness to p53 and DNA damage. Cancer Res 58:4439–4444
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fan, C., Yu, J., Liu, Y. et al. Increased NDRG1 Expression is Associated with Advanced T Stages and Poor Vascularization in Non-small Cell Lung Cancer. Pathol. Oncol. Res. 18, 549–556 (2012). https://doi.org/10.1007/s12253-010-9294-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-010-9294-2