Abstract
Between 2002 and 2008, a number of consensus statements and guidelines were developed by various groups around the world to educate healthcare professionals on the treatment of myelodysplastic syndromes (MDS), including the management of transfusional iron overload with iron chelation therapy. Guidelines have been developed by The Italian Society of Hematology, The UK MDS Guidelines Group, The Nagasaki Group, The National Comprehensive Cancer Network, and The MDS Foundation. These guidelines show that the approaches to managing iron overload in patients with MDS are region specific, differing in their recommendations for when iron chelation therapy should be initiated and strategies for the ongoing management of iron overload. The guidelines all agree that red blood cell transfusions are clinically beneficial to treat the symptomatic anemia in MDS, and that patients with low-risk MDS receiving transfusions are the most likely to benefit from iron chelation therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Although the myelodysplastic syndromes (MDS) are a relatively rare condition, the incidence in the general population is similar across the world: about five per 100,000 persons per year. Incidence is linked with age, rising to 20–50 per 100,000 persons per year in patients older than 60 years of age, and a median age at diagnosis of between 60 and 75 years [1–3] In Japan, the median age of diagnosis of MDS is 57 years, younger than in Caucasian patients [4].
Recent developments in the treatment of MDS, and growing evidence of the effects of iron overload on morbidity and mortality, have warranted the development of guidelines to inform physicians on the best available, most current treatment strategies for the management of iron overload [5, 6]. Between 2002 and 2008, a number of consensus statements and guidelines were developed by different groups around the world to educate healthcare professionals on the management of MDS. Although there are limited data on the clinical consequences of iron overload in patients with MDS, the guidelines also discuss management of transfusional iron overload as an important component of treating MDS, and also consider the clinical consequences of iron overload, the need to monitor patients who may be at risk of iron overload, and the need to treat iron-overloaded patients. The approaches to treating iron overload are likely to be region specific, so it is important that healthcare professionals treating transfusion-dependent patients with MDS are aware of best practice in their country.
The guidelines that have been developed include those of The Italian Society of Hematology [7], The UK MDS Guidelines Group [8], The Nagasaki Group, and The National Comprehensive Cancer Network (NCCN) in the USA [9]. This review will summarize the content of these guidelines, comparing relevant factors that influence the diagnosis and treatment of transfusion-dependent, iron-overloaded patients with MDS, including the classification systems used, recommendations for supportive therapy, and management of iron overload with the available iron chelation therapies. The MDS Foundation has also prepared a set of guidelines, with publication anticipated in 2008 [10].
2 Overview of the available guidelines
2.1 The Italian Society of Hematology
In 2001 and 2002, the Italian Society of Hematology commissioned a series of consensus conferences to provide clinical practice recommendations to support the appropriate choice of therapeutic interventions in patients with primary MDS, both of adult and pediatric age [7]. This led to the development of guidelines for the treatment of MDS using evidence-based knowledge and consensus-formation techniques. The guidelines were compiled by an expert panel of ten senior hematologists, and cover therapeutic options for MDS and supportive therapies including iron chelation, with statements graded according to the strength of the supporting evidence. The guidelines cover topics such as which patients are candidates for treatment, the appropriateness of new therapies, and optimizing transfusion and iron chelation therapy.
2.2 The UK MDS Guidelines Group
The UK guidelines group, which published their findings in 2003, included UK-based medical experts in the clinical management of MDS as well as a representative from a District General Hospital [8]. The drafting group met on six occasions, and no recommendations were included without a full consensus. The guidelines cover diagnosis of MDS, classification, the various prognostic scoring systems, and management of MDS.
2.3 The Nagasaki Group
A group of leading hematologists meeting in 2005 in Nagasaki, Japan, were the first to develop a consensus statement on the treatment of iron overload in patients with MDS. The main session was followed by regional discussion groups, and a final discussion on the consensus statement. They discussed fundamental questions such as which cases of MDS should be treated, when it is necessary to initiate treatment, and strategies for the treatment of iron-overloaded patients in continents around the world [11]. The group included healthcare professionals from Asia-Pacific (n = 13), Europe (n = 13), and Latin America (n = 8). The meeting summarized the current practice within each region and developed a consensus statement on the treatment of iron overload in patients with MDS that covers the knowledge at the time.
2.4 The National Comprehensive Cancer Network
The National Comprehensive Cancer Network (NCCN) is an alliance of 21 leading cancer centers, developing treatment guidelines for most cancers to improve the quality and effectiveness of care provided to patients. Each set of guidelines is a comprehensive set of diagnostic, treatment and supportive care recommendations. The guidelines for MDS are a statement of consensus developed by the NCCN Myelodysplastic Panel members and are reviewed annually. They include algorithms that cover the initial evaluation of MDS, the classification systems for de novo MDS, different treatment strategies for each International Prognostic Scoring System (IPSS) category, evaluation and treatment of the related anemia, as well as supportive therapy [9]. Among other therapeutic options covered by the guidelines, the panel recommends management of iron overload resulting from supportive transfusions with iron chelation therapy. This is discussed in greater detail below.
2.5 The MDS Foundation
The MDS Foundation has developed a set of consensus guidelines for the management of iron overload in patients with MDS. The guidelines are the result of discussions that took place during a series of 20 international round-table meetings. The guidelines were finalized at the MDS congress held in Florence, Italy, in May 2007, and are expected to be published in 2008. The main conclusions from the guidelines were presented at the MDS congress and are summarized here [10].
2.6 Japanese Guidelines for the treatment of transfusional iron overload (National Research Group on Idiopathic Bone Marrow Failure Syndromes)
Most recently, a group of Japanese physicians also convened at the MDS congress in Florence in 2007 to develop guidelines for the treatment of iron overload in bone-marrow failure in Japan, and to align Japanese and international guidelines. The group discussed which patients would most benefit from iron chelation therapy, diagnosis of iron overload, when to initiate iron chelation therapy, classification of severity of iron overload, and monitoring and maintaining iron chelation therapy. These guidelines are discussed in further detail in the accompanying manuscript by Dr Ozawa.
3 Guideline recommendations
3.1 The classification of MDS
In order to initiate iron chelation therapy appropriately, an understanding of the various classification systems is required. Understanding the prognosis of the MDS subgroups is equally important for the treatment of iron overload. MDS is a heterogeneous disease and two classification systems have been developed to classify the various subgroups. The French-American-British (FAB) system, developed in 1976 and revised in 1982, divided MDS patients into five subtypes: refractory anemia (RA), refractory anemia with ringed sideroblasts (RARS), refractory anemia with excess blasts (RAEB), refractory anemia with excess blasts in transformation (RAEB-T) and chronic myelomonocytic leukemia (CMML) [12]. The FAB system served as the gold standard for MDS classification for many years.
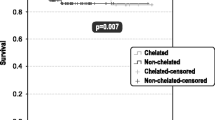
The World Health Organization (WHO) developed its system in 2002, incorporating many of the concepts and definitions of the FAB system, and adding refractory cytopenia with multilineage dysplasia (RCMD), refractory cytopenia with multilineage dysplasia and ringed sideroblasts (RCMD-RS), unclassified myelodysplastic syndrome (MDS-U) and eliminating RAEB-T and CMML. 5q-syndrome, commonly seen in older women with normal or high platelet counts, was considered to be a separate subtype, creating a total of eight subtypes [13]. The 5q-syndrome, RA and RARS subtypes are associated with the best survival rates, and RAEB II is associated with the worst (Fig. 1) [14].
Survival of patients with MDS according to the WHO criteria [14]. Reprinted from Germing U et al. Haematologica 2006;91:1596–1604. With kind permission of the Ferrata Storti Foundation, Pavia, Italy
The IPSS, introduced in 1997, improved on the MDS classification systems by introducing an assessment of the chances of overall survival and risk of transformation to acute myeloid leukemia for individual patients [15]. The IPSS uses a consensus-based approach for evaluating prognosis in MDS and is used in conjunction with the WHO and FAB diagnostic systems. The critical prognostic features of MDS were identified as the proportion of bone marrow blasts, the karyotype and the presence of one or more cytopenias (Table 1) [15].
Not discussed within any of these guidelines is a new prognostic classification system, the WPSS, which was conceived in 2007 by combining the WHO and IPSS systems. While the IPSS assesses prognosis of untreated patients at the time of diagnosis, the WPSS can also be used thereafter to assess risk during the course of a patient’s disease [16].
All the guidelines discussed within this review recommend the use of the IPSS, which they agree is useful for the prognostic stratification of MDS. When the UK MDS guidelines were published, the WHO system had only recently been published and there had been only limited experience with this; therefore, the more familiar FAB system was used [8]. The expert panel preparing the Italian guidelines chose to adopt the WHO classification system and the IPSS risk scores, dispensing with the FAB-classified RAEB-T subgroup [7]. The NCCN guidelines state that the IPSS has markedly improved the prognostic stratification of MDS, and endorse both the FAB and WHO classification systems, noting that the RAEB-T subgroup may be considered for either MDS or AML [9]. The Nagasaki group report that the WHO system is the most commonly used worldwide, although the FAB system is still commonly used in Europe and Latin America [11]. They further comment that the IPSS is widely used to estimate prognosis, particularly in Europe and Asia-Pacific, as well as by about 50% of hematologists in Latin America.
3.2 Supportive therapy for MDS
Supportive care, which includes red blood cell (RBC) transfusions, improves patient quality of life and remains the mainstay of treatment for MDS [9]. All the guidelines highlight the importance of supportive therapy and recommend RBC transfusions for symptomatic anemia as needed. The NCCN guidelines also suggest platelet transfusions for patients with severe thrombocytopenia or thrombocytopenic bleeding.
The guidelines differ on their recommendations for the hemoglobin (Hb) level at which transfusions should be initiated, and recommend taking into account issues such as quality of life, improved oxygenation and cardiac function, as well as risks of infection and iron overload. The Italian Society of Hematology guidelines indicate that all patients with Hb < 8 g/dL should receive RBC transfusions, while recommending that transfusions are rarely indicated in patients with mild anemia (Hb > 10 g/dL) [7]. The Nagasaki group Found that there is a great variation around the world in the Hb threshold that is used to initiate RBC transfusions: in Asia-Pacific, the range of the threshold level is 6–9 g/dL, while in Europe it is 8–10 g/dL, and 7–10 g/dL in Latin America [11]. The UK MDS group guidelines do not suggest a Hb concentration below which transfusions should be initiated, recommending that each individual case needs to be considered separately; however, they note that transfusions should be considered in any patient with symptoms of anemia, and that supportive care is particularly important for patients with good-prognosis MDS and for those with a poor prognosis whose age or performance status precludes them from receiving more intensive forms of therapy [8].
3.3 Management of iron overload
Although RBC transfusions remain an integral part of the management of MDS, chronic transfusions result in iron overload from catabolism of transfused erythrocytes and from plasma iron levels exceeding the binding capacity of transferrin. Iron overload can cause significant damage of the heart, liver and endocrine glands [17]. All the guidelines recommend that iron overload should be treated with iron chelation therapy to achieve a safe iron concentration in tissues and plasma. Likewise, they all recommend that the patients who are most likely to benefit from iron chelation therapy are those who are of low risk (e.g., low or Int-1; RA, RARS or 5q-MDS), and those who will continue to receive long-term RBC transfusions. The Japanese group of physicians meeting in Florence established that there is an issue with iron overload in a wider range of bone-marrow failure syndromes and within those categories set out the criteria for identifying patients who need iron chelation therapy. These recommendations are discussed in further detail in the accompanying manuscript by Dr Ozawa.
The NCCN guidelines recommend that although monitoring of serum ferritin levels is a useful method, it is less precise than superconducting quantum interference device (SQUID) or hepatic magnetic resonance imaging (MRI) [9].
The guidelines mostly recommend iron chelation therapy with deferoxamine (DFO, Desferal®). The UK guidelines recommend that audiometry and ophthalmology should be reviewed prior to DFO therapy and repeated at least annually, and that vitamin C (100–200 mg daily) should be commenced after 1 month of DFO therapy [8]. The Nagasaki group developed their guidelines prior to widespread use of the once-daily oral chelator, deferasirox (Exjade®). These experts based their consensus on knowledge at the time, rather than possible future developments; however, the guidelines explain that a suitable oral chelator would potentially overcome many of the problems associated with administration of subcutaneous infusions of DFO [11].
Based on the summary presented at the MDS congress in Florence, Italy, in May 2007, it is expected that the MDS Foundation guidelines will recommend that iron chelation therapy should be initiated when a patient’s serum ferritin reaches 1,000 μg/L, and/or after the patient has received two units of RBCs/month for at least 1 year. It was agreed that serum ferritin levels should not be the only factor to consider as patients can present with elevated serum ferritin levels as a result of ineffective erythropoiesis or due to inflammatory conditions. Iron chelation therapy was discussed, and should be offered to patients with an anticipated survival of greater than 1 year, and the choice of chelator should be left to the discretion of the physician. To ensure that the goal of therapy is attained, serum ferritin levels should be monitored at least every 3 months during therapy [10].
Table 2 summarizes the recommendations from each set of guidelines for the initiation of iron chelation therapy based on transfusion status, target serum ferritin level and MDS risk score. The table also indicates which iron chelation therapy that each set of guidelines recommends, the target serum ferritin level and techniques for monitoring iron chelation therapy.
4 Conclusions
The classification and scoring systems that have been devised provide a clearer understanding of the heterogeneous MDS diseases and an insight into how to use risk-adapted treatment approaches for MDS. Recent developments in the treatment of MDS allow clinicians to treat patients with a range of new therapies. This has necessitated the development of guidelines to steer healthcare professionals within each region to the available treatments and how to apply these to a complex disease.
The guidelines all concur that RBC transfusions are clinically beneficial to treat the symptomatic anemia in MDS, but caution that iron overload needs to be adequately managed to avoid the clinical consequences of organ damage. The guidelines agree that patients with low-risk MDS receiving RBC transfusions are the most likely to benefit from iron chelation therapy, but differ in their recommendations for when iron chelation therapy should be initiated. The guidelines also differ on the appropriate target serum ferritin level that should be reached to manage iron overload adequately; overall, however, they favor maintaining serum ferritin at <1,000 μg/L. Most of the guidelines recommend DFO for iron chelation, and the Nagasaki guidelines suggest that an oral chelator would be very useful. The NCCN guidelines, revised annually, recommend DFO or deferasirox, also noting that an oral iron chelator would more readily treat iron overload. The Italian and UK guidelines also recommend DFO, and were published prior to the approval of deferasirox in Europe.
Research continues into new approaches for the management of MDS, and there have been a number of developments in the field since publication of the first guidelines. More data are now available regarding the impact of iron overload in MDS and have prompted the development of more recent guidelines specific to this. These will undoubtedly be reviewed and updated as clinical experience in the management of iron overload grows.
References
Cazzola M, Malcovati L. Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med. 2005;352:536–8.
Greenberg PL, Baer MR, Bennett JM, et al. Myelodysplastic syndromes clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2006;4:58–77.
Aul C, Bowen DT, Yoshida Y. Pathogenesis, etiology and epidemiology of myelodysplastic syndromes. Haematologica. 1998;83:71–86.
Matsuda A, Germing U, Jinnai I, et al. Difference in clinical features between Japanese and German patients with refractory anemia in myelodysplastic syndromes. Blood. 2005;106:2633–40.
Gattermann N. Clinical consequences of iron overload in myelodysplastic syndromes and treatment with chelators. Hematol Oncol Clin North Am. 2005;19(Suppl 1):13–7.
Malcovati L, Della Porta MG, Pascutto C, et al. Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J Clin Oncol. 2005;23:7594–603.
Alessandrino EP, Amadori S, Barosi G, et al. Evidence- and consensus-based practice guidelines for the therapy of primary myelodysplastic syndromes: a statement from the Italian Society of Hematology. Haematologica. 2002;87:1286–306.
Bowen D, Culligan D, Jowitt S, et al. Guidelines for the diagnosis and therapy of adult myelodysplastic syndromes. Br J Haematol. 2003;120:187–200.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology—v.1.2008: Myelodysplastic Syndromes. http://www.nccn.org/professionals/physician_gls/pdf/mds.pdf 2008.
Gattermann N. Guidelines on iron chelation therapy in patients with myelodysplastic syndromes and transfusional iron overload. Leuk Res. 2007;31(Suppl 3):S10–S5.
Gattermann N, Porter J, Lopes LF, Seymour J. Consensus statement on iron overload in myelodysplastic syndromes. Hematol Oncol Clin North Am. 2005;19(Suppl. 1):18–25.
Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100:2292–302.
Germing U, Strupp C, Kuendgen A, et al. Prospective validation of the WHO proposals for the classification of myelodysplastic syndromes. Haematologica. 2006;91:1596–604.
Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Malcovati L, Germing U, Kuendgen A, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–10.
Andrews NC. Disorders of iron metabolism. N Engl J Med. 1999;341:1986–95.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gattermann, N. Overview of guidelines on iron chelation therapy in patients with myelodysplastic syndromes and transfusional iron overload. Int J Hematol 88, 24–29 (2008). https://doi.org/10.1007/s12185-008-0118-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-008-0118-z