Abstract
Iron overload remains a concern in myelodysplastic syndrome (MDS) patients especially those requiring recurrent blood transfusions. Whether iron chelating therapy (ICT) is beneficial to the long-term survival of myelodysplastic syndrome is still a controversial issue. Therefore, we conducted a systematic review and meta-analysis to clarify the relationship between ICT and long-term survival in patients with MDS. A total of 14 studies involving 7242 participants were identified; the outcomes revealed that for patients with MDS, ICT resulted in a lower risk of mortality compared to those with no ICT (HR 0.57; 95% CI 0.44–0.70; P < 0.001); what is more, ICT led to a lower risk of leukemia transformation (HR 0.70; 95% CI 0.52–0.93; P = 0.016). Results of subgroup analyses based on adequate ICT or any ICT, low/int-1 IPSS or unclassified IPSS and study types indicated that the ICT had a beneficial role in all these groups of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndrome (MDS) is a group of refractory heterogeneous diseases originating from hematopoietic stem cells and characterized by pathological hematopoiesis and enhanced risk of transformation to acute myeloid leukemia (AML) [1, 2]. Anemia is the most frequent cytopenia diagnosed in patients with MDS [3], and the majority of the patients will require red blood transfusion therapy when anemia appears through the disease course. The short-term benefit of red blood cell (RBC) transfusion is that it can rapidly improve anemia symptoms and life quality of patients [3]. However, iron overload often occurs as an iatrogenic consequence of RBC transfusions in some patients [4]. What is worse, because of ineffective erythropoiesis and consequently unrestrained intestinal iron uptake, iron overload in MDS often appears before patients become transfusion-dependent and the clinical consequences of iron overload include cardiac and/or hepatic failure, endocrinopathies and infection risk [5]. MDS patients showed increased levels of oxidative stress, which was further aggravated by iron overload [6,7,8]. A meta-analysis including 1855 participants underlined worse survival in patients with MDS who had higher SF levels [9].
Iron chelation therapy (ICT) was commonly used in patients with transfusional iron overload in chronic transfusion-dependent anemia, such as sickle cell disease or β-thalassemia, and is also used in some patients with MDS [10,11,12,13,14]. No validated threshold has been established for SF levels, but experts have recommended 1000–2500 ng/mL [15]. ICT was usually recommended for managing iron overload in MDS patients with low/int-1 IPSS score when serum ferritin (SF) levels are above 1000 ng/mL, but the data indicate that SF levels between the upper limit of normal and 1000 ng/mL adversely affect genetic stability [16, 17]. However, these treatment suggestions for ICT in MDS patients are not based on clinical outcomes from prospective randomized trials, and there are different opinions among experts on whether to choose ICT or not for MDS patients with iron overload [18]. In addition, ICT in MDS is sometimes terminated due to adverse events (AEs), and the overall annual discontinuation rates for MDS patients in these trials ranged approximately 40–50% [19,20,21,22]. In a previous meta-analysis concerning ICT for MDS conducted by Mainous et al. in 2014, eight observational studies were included; finally, they concluded that the use of ICT in patients with MDS is associated with a greater median survival time than their counterparts who did not receive ICT [23]. However, only 1562 participants were included in their study and these studies were focused on patients with low IPSS score. In recent years, several new studies with larger sample size and better design have been reported; therefore, a new meta-analysis is needed to evaluate the application value of ICT in MDS, including high IPSS score [23]. To further illustrate whether ICT is beneficial to overall survival (OS) and/or leukemia-free survival (LFS), we performed a new systematic review and meta-analysis of studies focused on the relationship between ICT and OS and/or the rates of transformation to AML.
Materials and methods
Study identification
PubMed, EMBASE, Web of Science and Cochrane Library electronic databases were searched with no language restriction from inception through January 18, 2019, with search terms (MDS OR Myelodysplastic syndrome) AND (iron chelation OR iron chelating) AND (overall survival OR OS). The present meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines [24, 25]. References from the above-selected reports were accordingly searched to include any additional publications. Published abstracts were permitted if the primary outcomes of interest were reported. If the publications were reported from the same cohort, those with the longer follow-up or larger samples were included.
The potentially relevant studies were downloaded and reviewed for the following exclusion criteria: (1) not a clinical study, (2) not reporting data for leukemia-free survival (LFS) and/or overall survival (OS), (3) not reporting original data, (4) the objectives investigated had multiple hematological malignancies including MDS and (5) studies not focused on relationship between ferritin and OS.
Data extraction
The data included in this meta-analysis were extracted from publicly available published articles and were independently extracted from published articles by Hailing Liu and Nan Yang. PRISMA flow diagram is shown in Fig. 1a. We collected key study characteristics, including study design, treatment strategy, sample size, median LFS, median OS and hazard ratios (HRs) with confidence intervals for LFS and OS. This present meta-analysis included 14 studies that fulfilled our eligibility criteria; in total, 7242 patients were included; of these studies, six studies were prospective (one RCT included) and eight studies were retrospective. The main sample characteristics are presented in Table 1.
Study quality
We judged the quality of studies included in the present meta-analysis using Newcastle–Ottawa Scale (NOS) as shown in Fig. 1b. Publication bias of the included literature was assessed with Egger’s regression intercept, as shown in Fig. 2a; there were some elements with the appearance of publication bias (P < 0.001), with smaller studies not being symmetrical around the mean effect size, which suggested that studies with much larger effect size were more likely to be published.
Sensitivity analysis
We performed sensitivity analysis with a pre-planned sensitivity analysis by removing each study and then re-conducted the meta-analysis for the remaining studies to determine the stability of the results (shown in Fig. 2b). The results suggested that the two studies conducted by Zeidan et al. [38] and Angelucci et al. [22] had a great influence on the final results. Subsequently, we further analyzed the reasons why these two studies brought such obvious heterogeneity to this meta-analysis.
Results
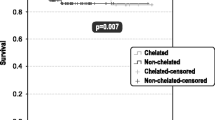
Some studies had tolerability or adverse events (AEs) as their primary end points, and ten included studies reported data on HRs of LFS and OS, while the median OS was not yet reached for several studies. The treatment effect sizes were little greater for OS (HR 0.57; 95% confidence interval (CI) 0.44–0.70; P < 0.001) (Fig. 3) in the ICT group than for LFS (HR 0.70; 95% CI 0.52–0.93; P = 0.016) (Fig. 4).
We conducted subgroup analysis based on adequate ICT or any ICT (Fig. 5a, b), low/int-1 IPSS or unclassified IPSS (Fig. 6a, b) and study type (Fig. 7a, b). The results indicated that ICT exerted a better effect on the OS for different groups of patients with MDS compared to those without ICT treatment.
Discussion
A total of 14 prospective and retrospective studies focusing on ICT and OS and/or LFS of patients with MDS were included in this meta-analysis, and the results indicated ICT was associated with both prolonged OS (HR 0.57; 95% CI 0.44–0.70; P < 0.001) and LFS (HR 0.70; 95% CI 0.52–0.93; P = 0.016). The conclusions were consistent with previous studies of ICT in MDS [23, 39, 40]. There was no statistical difference between two studies regarding the benefits of ICT compared with no ICT for OS of MDS [34, 37]. The study conducted by Angelucci et al. was a randomized placebo-controlled phase II clinical trial, reporting a median OS of 1907 days (95% CI: 1440—not estimable) with ICT and 1509 days (95% CI 1095–1804) with placebo, HR 0.832 (95% CI 0.54–1.28, P = 0.20). A potential OS difference was thought to be diluted because of the young age of the patients and the fact that half of placebo patients dropped out and subsequently received chelation, in addition to the fact that the patient numbers were reduced by two-thirds due to poor enrollment [37]. Clinical practice of ICT in MDS varied fairly in the European countries registered in the EUMDS. Deferasirox was most frequently used in MDS with iron overload, and the frequency ranged from 0 to 25% per country. OS was significantly better when compared with a large control group; besides, OS was longer after treatment with deferasirox than deferoxamine [34].
Sensitivity analysis indicated that the stability of meta-analysis results was greatly affected by two included studies [22, 38]. Small size of the control compared to the ICT group (7 vs. 152) might be one of the factors influencing the final OS [22]. The study conducted by Zeidan A et al. [38] included a large proportion of patients with intermediate IPSS score, so the final treatment effect may also be less significant compared those including a large proportion of low-IPSS patients.
Poor patient adherence to therapy was also a common problem in ICT treatment. High trial discontinuation rates of patients with MDS likely reflected the poor physique with insufficient motivation with regard to the disease and the expected benefits of ICT. Patients with longer duration of disease were more likely to complete the trial, which potentially implied improved patient education and cognition of the disease progression. The advanced age and poor physical condition of patients with MDS may also explain the high incidence of non-treatment-related AEs reported in a previous study. However, no treatment-related deaths, treatment-related grade 4 AEs or dose-limiting toxic effects were observed in the whole study, and the majority of treatment-related AEs were minor [22]. Another study reported a rate of AEs of 47.5% among patients, mainly gastrointestinal and renal toxicity [41]. Nevertheless, ICT is an effective measure in MDS patients with iron overload, even at an earlier stage of the disease. The threshold of ferritin for starting ICT is expected to be explored in future studies.
The studies included in the present meta-analysis did not limit the IPSS risk of patients; therefore, it explored universal applicability of ICT in MDS. We found that although ICT was beneficial to OS (HR 0.57; 95% CI 0.44–0.70; P < 0.001) of patients with any IPSS risk, it was more effective in patients with low/int-1 IPSS (HR 0.48; 95% CI 0.21–0.74; P < 0.001). Therefore, ICT should be recommended in more MDS patients with iron overload. Besides, MDS patients with iron overload receiving deferasirox resulted in increased hemoglobin level from 6 to 44.5%, increased platelet count from 13 to 61% and neutrophil count from 3 to 76% [17, 20, 22, 42, 43], which might be another underlying mechanism to reduce the risk of death by preventing patients from hemorrhage and infection. Hypermethylation of tumor suppresser genes occurs frequently in MDS patients, and these epigenetic abnormalities have been confirmed to be associated with MDS progression and transformation to leukemia. Besides, oxidative stress was correlated with tumor suppressor genes methylation, and iron chelators may reverse tumor suppressor genes hypermethylation by reducing oxidative stress, thereby reducing disease progression and leukemia transformation [44]. Of course, avoiding unnecessary blood transfusion is an important means to reduce iron overload. It has been reported that cyclosporine therapy can make patients achieve blood transfusion independence [45].
Our meta-analysis included only one randomized clinical study, in which the HR (0.832; 95% CI 0.54–1.28; P = 0.20) of ICT for OS seems to have little effect, though this study has limitations as discussed above. Therefore, more well-designed randomized clinical trials are expected to confirm the current results, and further seek measures to reduce treatment-related adverse reactions and explore the threshold of SF for initiating ICT.
References
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. https://doi.org/10.1182/blood-2012-03-420489.
Jabbour E, Takahashi K, Wang X, Cornelison AM, Abruzzo L, Kadia T, et al. Acquisition of cytogenetic abnormalities in patients with IPSS defined lower-risk myelodysplastic syndrome is associated with poor prognosis and transformation to acute myelogenous leukemia. Am J Hematol. 2013;88(10):831–7. https://doi.org/10.1002/ajh.23513.
Waszczuk-Gajda A, Madry K, Machowicz R, Drozd-Sokolowska J, Stella-Holowiecka B, Mital A, et al. Red blood cell transfusion dependency and hyperferritinemia are associated with impaired survival in patients diagnosed with myelodysplastic syndromes: results from the first polish MDS-PALG registry. Adv Clin Exp Med Off Org Wroc Med Univ. 2016;25(4):633–41. https://doi.org/10.17219/acem/62397.
Dreyfus F. The deleterious effects of iron overload in patients with myelodysplastic syndromes. Blood Rev. 2008;22(Suppl 2):S29–34. https://doi.org/10.1016/S0268-960X(08)70006-7.
Shammo JM, Komrokji RS. Clinical consequences of iron overload in patients with myelodysplastic syndromes: the case for iron chelation therapy. Expert Rev Hematol. 2018;11(7):577–86. https://doi.org/10.1080/17474086.2018.1486188.
Ghoti H, Amer J, Winder A, Rachmilewitz E, Fibach E. Oxidative stress in red blood cells, platelets and polymorphonuclear leukocytes from patients with myelodysplastic syndrome. Eur J Haematol. 2007;79(6):463–7. https://doi.org/10.1111/j.1600-0609.2007.00972.x.
Lu WY, Zhao MF, Rajbhandary S, Xie F, Chai X, Mu J, et al. Free iron catalyzes oxidative damage to hematopoietic cells/mesenchymal stem cells in vitro and suppresses hematopoiesis in iron overload patients. Eur J Haematol. 2013;91(3):249–61. https://doi.org/10.1111/ejh.12159.
Chung YJ, Robert C, Gough SM, Rassool FV, Aplan PD. Oxidative stress leads to increased mutation frequency in a murine model of myelodysplastic syndrome. Leuk Res. 2014;38(1):95–102. https://doi.org/10.1016/j.leukres.2013.07.008.
Pileggi C, Di Sanzo M, Mascaro V, Marafioti MG, Costanzo FS, Pavia M. Role of serum ferritin level on overall survival in patients with myelodysplastic syndromes: results of a meta-analysis of observational studies. PLoS ONE. 2017;12(6):e0179016. https://doi.org/10.1371/journal.pone.0179016.
Carreau N, Tremblay D, Savona M, Kremyanskaya M, Mascarenhas J. Ironing out the details of iron overload in myelofibrosis: lessons from myelodysplastic syndromes. Blood Rev. 2016;30(5):349–56. https://doi.org/10.1016/j.blre.2016.04.003.
Yassin MA, Soliman AT, De Sanctis V, Hussein RM, Al-Okka R, Kassem N, et al. Jadenu((R)) substituting exjade((R)) in iron overloaded beta-thalassemia major (BTM) patients: a preliminary report of the effects on the tolerability, serum ferritin level, liver iron concentration and biochemical profiles. Mediterr J Hematol Infect Dis. 2018;10(1):e2018064. https://doi.org/10.4084/mjhid.2018.064.
Bollig C, Schell LK, Rucker G, Allert R, Motschall E, Niemeyer CM, et al. Deferasirox for managing iron overload in people with thalassaemia. Cochrane Database Syst Rev. 2017;8:7476. https://doi.org/10.1002/14651858.cd007476.pub3.
Karami H, Kosaryan M, Amree AH, Darvishi-Khezri H, Mousavi M. Combination iron chelation therapy with deferiprone and deferasirox in iron-overloaded patients with transfusion-dependent beta-thalassemia major. Clin Pract. 2017;7(1):912. https://doi.org/10.4081/cp.2017.912.
Kattamis A, Aydinok Y, Taher A. Optimising management of deferasirox therapy for patients with transfusion-dependent thalassaemia and lower-risk myelodysplastic syndromes. Eur J Haematol. 2018;101(3):272–82. https://doi.org/10.1111/ejh.13111.
Leitch HA, Buckstein R, Zhu N, Nevill TJ, Yee KWL, Leber B, et al. Iron overload in myelodysplastic syndromes: evidence based guidelines from the Canadian consortium on MDS. Leuk Res. 2018;74:21–41. https://doi.org/10.1016/j.leukres.2018.09.005.
Zeidan AM, Griffiths EA. To chelate or not to chelate in MDS: that is the question! Blood Rev. 2018;32(5):368–77. https://doi.org/10.1016/j.blre.2018.03.002.
Gattermann N. Iron overload in myelodysplastic syndromes (MDS). Int J Hematol. 2018;107(1):55–63. https://doi.org/10.1007/s12185-017-2367-1.
Mitchell M, Gore SD, Zeidan AM. Iron chelation therapy in myelodysplastic syndromes: where do we stand? Expert Rev Hematol. 2013;6(4):397–410. https://doi.org/10.1586/17474086.2013.814456.
Porter J, Galanello R, Saglio G, Neufeld EJ, Vichinsky E, Cappellini MD, et al. Relative response of patients with myelodysplastic syndromes and other transfusion-dependent anaemias to deferasirox (ICL670): a 1-yr prospective study. Eur J Haematol. 2008;80(2):168–76. https://doi.org/10.1111/j.1600-0609.2007.00985.x.
List AF, Baer MR, Steensma DP, Raza A, Esposito J, Martinez-Lopez N, et al. Deferasirox reduces serum ferritin and labile plasma iron in RBC transfusion-dependent patients with myelodysplastic syndrome. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(17):2134–9. https://doi.org/10.1200/jco.2010.34.1222.
Gattermann N, Finelli C, Porta MD, Fenaux P, Ganser A, Guerci-Bresler A, et al. Deferasirox in iron-overloaded patients with transfusion-dependent myelodysplastic syndromes: results from the large 1-year EPIC study. Leuk Res. 2010;34(9):1143–50. https://doi.org/10.1016/j.leukres.2010.03.009.
Angelucci E, Santini V, Di Tucci AA, Quaresmini G, Finelli C, Volpe A, et al. Deferasirox for transfusion-dependent patients with myelodysplastic syndromes: safety, efficacy, and beyond (GIMEMA MDS0306 Trial). Eur J Haematol. 2014;92(6):527–36. https://doi.org/10.1111/ejh.12300.
Mainous AG 3rd, Tanner RJ, Hulihan MM, Amaya M, Coates TD. The impact of chelation therapy on survival in transfusional iron overload: a meta-analysis of myelodysplastic syndrome. Br J Haematol. 2014;167(5):720–3. https://doi.org/10.1111/bjh.13053.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA J Am Med Assoc. 2000;283(15):2008–12.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. https://doi.org/10.1136/bmj.g7647.
Leitch HALC, Goodman TA, Wong KK, Wong DHC, Ramadan KM, Rollins MD, Barnett MJ, Galbraith PF, Vickars LM. Improved survival in patients with myelodysplastic syndrome receiving iron chelation therapy. Clin Leuk. 2008;2:205–11.
Rose C, Brechignac S, Vassilief D, Pascal L, Stamatoullas A, Guerci A, et al. Does iron chelation therapy improve survival in regularly transfused lower risk MDS patients? A multicenter study by the GFM (Groupe Francophone des Myelodysplasies). Leuk Res. 2010;34(7):864–70. https://doi.org/10.1016/j.leukres.2009.12.004.
Raptis A, Duh MS, Wang ST, Dial E, Fanourgiakis I, Fortner B, et al. Treatment of transfusional iron overload in patients with myelodysplastic syndrome or severe anemia: data from multicenter clinical practices. Transfusion. 2010;50(1):190–9. https://doi.org/10.1111/j.1537-2995.2009.02361.x.
Komrokji RS, Al Ali NH, Padron E, Lancet JE, List AF. Impact of iron chelation therapy on overall survival and AML transformation in lower risk MDS patients treated at the Moffitt cancer center. Blood. 2011;118(21):1196–7.
Neukirchen J, Fox F, Kundgen A, Nachtkamp K, Strupp C, Haas R, et al. Improved survival in MDS patients receiving iron chelation therapy—a matched pair analysis of 188 patients from the Dusseldorf MDS registry. Leuk Res. 2012;36(8):1067–70. https://doi.org/10.1016/j.leukres.2012.04.006.
Lyons RM, Marek BJ, Paley C, Esposito J, Garbo L, DiBella N, et al. Comparison of 24-month outcomes in chelated and non-chelated lower-risk patients with myelodysplastic syndromes in a prospective registry. Leuk Res. 2014;38(2):149–54. https://doi.org/10.1016/j.leukres.2013.11.004.
Delforge M, Selleslag D, Beguin Y, Triffet A, Mineur P, Theunissen K, et al. Adequate iron chelation therapy for at least 6 months improves survival in transfusion-dependent patients with lower risk myelodysplastic syndromes. Leuk Res. 2014;38(5):557–63. https://doi.org/10.1016/j.leukres.2014.02.003.
Remacha AF, Arrizabalaga B, Villegas A, Duran MS, Hermosin L, de Paz R, et al. Evolution of iron overload in patients with low-risk myelodysplastic syndrome: iron chelation therapy and organ complications. Ann Hematol. 2015;94(5):779–87. https://doi.org/10.1007/s00277-014-2274-y.
Langemeijer S, De Swart L, Yu G, Smith A, Crouch S, Johnston T, et al. Impact of treatment with iron chelators in lower-risk MDS patients participating in the European leukemianet MDS (EUMDS) registry. Blood. 2016;128(22):3186.
Leitch HA, Parmar A, Wells RA, Chodirker L, Zhu N, Nevill TJ, et al. Overall survival in lower IPSS risk MDS by receipt of iron chelation therapy, adjusting for patient-related factors and measuring from time of first red blood cell transfusion dependence: an MDS-CAN analysis. Br J Haematol. 2017;179(1):83–97. https://doi.org/10.1111/bjh.14825.
Wong SA, Leitch HA. Iron chelation therapy in lower IPSS risk myelodysplastic syndromes; which subtypes benefit? Leuk Res. 2018;64:24–9. https://doi.org/10.1016/j.leukres.2017.11.005.
Angelucci ELJ, Greenberg PL, Depei W, Hou M, Montaño Figueroa E, Rodriguez G, Dong X, Ghosh J, Bornstein O, Garcia-Manero G. Safety and efficacy, including event-free survival, of deferasirox versus placebo in iron-overloaded patients with low- and int-1-risk myelodysplastic syndromes (mds): outcomes from the randomized, double-blind telesto study. Blood. 2018;132(Suppl 1):234.
Zeidan AM, Hendrick F, Friedmann E, Baer MR, Gore SD, Sasane M, et al. Deferasirox therapy is associated with reduced mortality risk in a medicare population with myelodysplastic syndromes. J Comp Eff Res. 2015;4(4):327–40. https://doi.org/10.2217/cer.15.20.
Zeidan AM, Giri S, DeVeaux M, Ballas SK, Duong VH. Systematic review and meta-analysis of the effect of iron chelation therapy on overall survival and disease progression in patients with lower-risk myelodysplastic syndromes. Ann Hematol. 2019;98(12):339–50. https://doi.org/10.1007/s00277-018-3539-7.
Abrahama I, Al Yami M, Yun S, Kim HJ, Vincelette ND, McBride A, et al. Survival outcomes in iron chelated and non-chelated patients with lower-risk myelodysplastic syndromes: review and pooled analysis of observational studies. Leuk Res. 2017;57:104–8. https://doi.org/10.1016/j.leukres.2017.03.007.
Maurillo L, Breccia M, Buccisano F, Voso MT, Niscola P, Trape G, et al. Deferasirox chelation therapy in patients with transfusion-dependent MDS: a “real-world’ report from two regional Italian registries: gruppo Romano Mielodisplasie and Registro Basilicata. Eur J Haematol. 2015;95(1):52–6. https://doi.org/10.1111/ejh.12476.
Gattermann N, Finelli C, Della Porta M, Fenaux P, Stadler M, Guerci-Bresler A, et al. Hematologic responses to deferasirox therapy in transfusion-dependent patients with myelodysplastic syndromes. Haematologica. 2012;97(9):1364–71. https://doi.org/10.3324/haematol.2011.048546.
Nolte F, Hochsmann B, Giagounidis A, Lubbert M, Platzbecker U, Haase D, et al. Results from a 1-year, open-label, single arm, multi-center trial evaluating the efficacy and safety of oral Deferasirox in patients diagnosed with low and int-1 risk myelodysplastic syndrome (MDS) and transfusion-dependent iron overload. Ann Hematol. 2013;92(2):191–8. https://doi.org/10.1007/s00277-012-1594-z.
Goncalves AC, Cortesao E, Oliveiros B, Alves V, Espadana AI, Rito L, et al. Oxidative stress levels are correlated with P15 and P16 gene promoter methylation in myelodysplastic syndrome patients. Clin Exp Med. 2016;16(3):333–43. https://doi.org/10.1007/s10238-015-0357-2.
Di Renzo M, Pasqui AL, Voltolini L, Gotti G, Pompella G, Auteri A. Myelodysplasia and good syndrome A case report. Clin Exp Med. 2008;8(3):171–3. https://doi.org/10.1007/s10238-008-0175-x.
Funding
This manuscript was supported by Shaanxi International Scientific Research Cooperation and Exchange Program (Grant Number: 2016KW-020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
The study was approved by the Second Affiliated Hospital of Xi’an Jiaotong University.
Informed consent
Informed consent was obtained from all individual participants included in this study in their original studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, H., Yang, N., Meng, S. et al. Iron chelation therapy for myelodysplastic syndrome: a systematic review and meta-analysis. Clin Exp Med 20, 1–9 (2020). https://doi.org/10.1007/s10238-019-00592-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-019-00592-5