Abstract
Eosinophilic and non-eosinophilic subtypes of chronic rhinosinusitis with nasal polyp (CRSwNP) have different clinical profile and management. Currently the 2 subtypes are differentiated based on tissue eosinophilic infiltration, which is identified after surgery by histopathological examination. Hence this study was conducted to compare utility of computed tomography (CT) scans, serum IgE levels, absolute eosinophil count (AEC) and Sino-nasal Outcome Test (SNOT)-20 score for discriminating the 2 subtypes. In this prospective study of 1 year duration, patients suspected of CRSwNP were recruited. Serum IgE levels and AEC estimation were performed by ELISA and standard numerical formula respectively, along with histopathological examination of nasal polyp biopsies. CT score and ratio of CT score for ethmoid sinus and maxillary sinus (E/M ratio) were calculated. Patients were asked to fill SNOT-20 questionnaire. Receiver-operating characteristic (ROC) curve analysis was performed. Out of 52 patients studied, 38 and 14 were no. of eosinophilic and non-eosinophilic CRSwNP cases respectively on the basis of histopathological examination. E/M ratio and overall CT score were found to be highly accurate with area under ROC curve of 0.990 and 0.964 respectively, while rest 3 parameters had low accuracy. Optimal cut-off of CT score and E/M ratio for eosinophilic CRSwNP were 6 and 2.065 respectively. This study demonstrated E/M ratio and total CT score as the most useful surrogate markers for preoperative differentiation of eosinophilic and non-eosinophilic CRSwNP, and hence can be used to predetermine postoperative management before surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a chronic inflammatory disease of the nasal and paranasal sinus mucosa persisting for more than 3 months [1]. Chronic rhinosinusitis (CRS) is one of the commonest chronic rhinologic diseases and may significantly reduce the quality of life of affected patients [2]. The characteristic features include decreased sense of smell, posterior nasal drip, nasal obstruction, facial pressure and/or pain, and occasionally, nasal polyposis. Approximately 4% of the adult population affected suffer from a poor quality of life and high medical expenditure as a result of the disease [1, 3].
CRS is usually classified into one of two phenotypes, CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP), based primarily on endoscopic findings [2, 4]. CRSwNP patients can be classified into two subtypes on histopathological examination—eosinophilic and non-eosinophilic nasal polyps [2, 5]. The clinical and pathologic characteristics of the 2 subtypes differ from each other. Eosinophilic and non-eosinophilic CRSwNP patients respond to steroid and macrolide treatment respectively. The presence of severe tissue eosinophilia in eosinophilic CRSwNP patients may account for failed correction of the ostiomeatal complex (OMC) occlusion through endoscopic sinus surgery, and the subsequent development of recurrent nasal polyps [6]. Early administration of high dose topical or systemic steroid therapy in these patients may significantly improve the result [6]. Distinguishing between eosinophilic and noneosinophilic CRSwNP in Asian patients is imperative for appropriate management [2, 7, 8].
Presently eosinophilic and noneosinophilic CRSwNP are differentiated based on tissue eosinophilic infiltration, with eosinophilic CRSwNP defined as the percentage of eosinophils in tissue-infiltrated inflammatory cells exceeding 5% [9, 10]. However, tissue eosinophilic infiltration is usually identified after surgery by histopathological examination. Hence, this approach may be quite impractical since it is difficult to collect the diagnostic information prior to surgery or from the patients undergoing only medical treatment [9]. Therefore, this study was conducted to compare the use of computed tomography (CT) scans, serum IgE levels, absolute eosinophil count and Sino-nasal Outcome Test (SNOT)-20 score in the early diagnosis of eosinophilic and noneosinophilic CRSwNP [11].
Materials and Methods
This was a prospective study conducted in the Department of Microbiology and Department of Otorhinolaryngology, at an 1800-bed tertiary-care hospital in Delhi, during a 1 year period from 1st January 2015 to 31st December 2015. Human ethical clearance was obtained from the institute. Written informed consent was taken from the study subjects.
Patients clinically suspected of CRSwNP attending the Otorhinolaryngology outpatient department and wards of the hospital during the study period were recruited in the study. CRS with nasal polyps was diagnosed based on the criteria of the European Position Paper [4].
Seven ml of blood sample was aseptically collected from the study subjects, of which 3 ml and 4 ml were transferred to haemogram vial and plain vial respectively. From blood collected in plain vial, serum was separated and aliquoted in different vials and stored at −70 °C until tested. Repeated freezing and thawing was avoided. IgE estimation was done using commercially available Enzyme-Linked Immunosorbent Assay (ELISA) Kit (Calbiotech, Spring Valley, USA) as per manufacturer instructions. Absolute eosinophil count (AEC) was calculated using standard numerical formula [12].
Histopathological examination of the nasal polyp biopsies was carried out. Eosinophilic CRSwNP was defined as the percentage of eosinophils in tissue infiltrated inflammatory cells exceeding 5% [9, 10].
CT scan findings were recorded. CT score and ratio of the CT score for ethmoid sinus and maxillary sinus (E/M ratio) were calculated. Clinical details were noted and patients were asked to fill SNOT-20 questionnaire [13].
Statistical Analysis
Frequency distributions were obtained and percentages were calculated accordingly. GraphPad Inc. statistical software (2236 Avenida de la Playa La Jolla, CA 92037, USA) was used for calculation of mean and P value using Unpaired t test. Statistical significance was defined as P value less than 0.05. Receiver-operating characteristic (ROC) curve analysis was performed using IBM SPSS 16 (SPSS, Inc., Chicago, IL, USA) to determine the utility of IgE, AEC, SNOT-20 score and CT score for differentiating between eosinophilic and non-eosinophilic CRSwNP. The area under the ROC curve (AUC) was calculated. Youden’s J (J = sensitivity + specificity − 1) was used to identify the optimal cut-off point [14, 15].
Results
A total of 52 patients presented during the study duration with suspected CRSwNP. of them 38 and 14 were found to be the no. of eosinophilic and non-eosinophilic CRSwNP cases respectively. Age-range was from 10 to 58 years. There were a total of 30 males and 22 females. The mean age of the eosinophilic and non-eosinophilic CRSwNP cases were 30.16 and 27.86 years respectively. The rest of the mean values of serum IgE levels, AEC, SNOT-20 score, and CT score are given in Table 1. The values of the variables were not significantly different between eosinophilic and non-eosinophilic CRSwNP cases except for CT score (P = 0.0016).
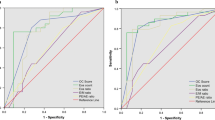
In the ROC curve analyses, the AUC were 0.990, 0.964, 0.632, 0.698 and 0.700 for E/M ratio, overall CT score, IgE, AEC and SNOT-20 score respectively. An ROC curve is created by plotting the true-positive ratio (sensitivity), against the false-positive ratio (1 − specificity). AUC is an index of the precise applicability of a test across the full range of possible cut-off points [14]. Higher values of the AUC signify better precision, with the highest possible value being 1 [14, 16]. Fisher et al. proposed three categories: a test with an AUC greater than 0.9 is said to be highly accurate, while AUC 0.7–0.9 and 0.5–0.7 indicate moderate and low accuracy respectively. An AUC of 0.5 implies a chance result [14, 16]. Hence CT score (Fig. 1) and E/M ratio (Fig. 2) were found to be highly accurate, while rest 3 parameters had low accuracy (Figs. 3, 4, 5). The cut-off of CT score as per Youden’s J for eosinophilic CRSwNP was 6 (sensitivity of 92.9%, specificity of 100%) in the study population, while the cut-off of E/M ratio for eosinophilic CRSwNP was 2.065 (sensitivity of 94.1%, specificity of 100%).
Discussion
Clinically, eosinophilic CRSwNP differs from noneosinophilic CRSwNP with regard to symptoms, site of nasal polyp occurrence, CT scan findings, histological findings of the nasal polyps, blood picture, clinical course post surgery, and comorbid asthma [17]. Chiefly, the presence of severe tissue eosinophilia in eosinophilic CRSwNP patients may account for the failure of correcting the ostiomeatal complex (OMC) occlusion through endoscopic sinus surgery in significantly improving the patients’ condition [6]. In this subgroup interventions focused on correcting the OMC occlusion may not alter chronic mucosal inflammation and instead surgical treatment may lead to recurrent nasal polyps over time, and the timely administration of steroid treatment in these patients may improve their outcomes to a great extent [6]. On the other hand, anatomical obstruction of the OMC compromising ventilation and the drainage of dependent sinuses is well recognized in non-eosinophilic inflammation. These induce a hypoxic state and intensify bacterial colonization in the paranasal sinuses, which in turn causes neutrophilic inflammation, tissue remodeling and polyp formation by activating endothelial cells and fibroblasts to release inflammatory mediators. Nevertheless, OMC occlusion may not be the fundamental predisposing factor for the development of eosinophilic inflammation [6]. As the treatment strategies of eosinophilic and noneosinophilic CRSwNP vary, the 2 subtypes distinction is crucial [18].
In this study, the IgE levels displayed least accuracy in discriminating ECRS and non-ECRS. Various other studies have also found IgE levels to be of no value in making a distinction between the 2 subtypes of CRSwNP [9, 10, 19, 20]. Contrastingly, several reports also exist supporting IgE levels as an useful surrogate marker for ECRS [9, 17, 21, 22]. The AEC demonstrated low accuracy for differentiating eosinophilic and non-eosinophilic CRS in the present study. In agreement to our study, Smith et al. also did not find statistically significant difference between AEC of ECRS and non-ECRS. However several studies have reported blood eosinophil counts to be significantly higher in the eosinophilic CRSwNP group compared to the non-eosinophilic CRSwNP group [11, 18, 24,25,26,26]. SNOT-20, a patient-reported survey of symptoms and health related quality of life, is one of the commonly used tools for gauging disease severity in CRS and is well-accepted due to its high patient compliance [14, 20]. The SNOT-20 score ROC curve in the present study showed moderate accuracy in distinguishing eosinophilic from non-eosinophilic CRSwNP. This is in accordance to a study by Smith et al. [20].
The total CT score, with the cut-off at 6 for eosinophilic CRSwNP, proved to be highly accurate for diagnosing ECRS in the present study. Although few reports have suggested no correlation between CT score and eosinophilic CRS [20, 27], most studies have found higher CT score to be significantly associated with eosinophilic CRSwNP similar to the present study [2, 11, 18, 28,29,30,31,32,33,34,34]. However we did not come across any study stating the exact cut-off of CT score for differentiating between eosinophilic and non-eosinophilic CRSwNP despite extensive literature search. Sinus CT has been a useful tool in evaluating patients with sinus disease, particularly prior to surgery [35]. Lund and Mackay suggested a rhinological staging system on CT scan involving a Lund-Mackay score (LMS) that proved to be an effective assessment method for evaluating the severity of rhinosinusitis [32, 35, 36]. In the Lund-Mackay CT Scoring procedure, the right or left sinuses are respectively divided into six portions, including maxillary sinus, anterior ethmoid sinuses, posterior ethmoid sinuses, sphenoid sinus, frontal sinus, and ostiomeatal complex. The severity of sinus mucosal inflammation or fluid accumulation or mild mucosal thickening without fluid collection is scored as 0 (complete lucency), 1 (partial lucency) or 2 (complete opacity). The ostiomeatal complex is scored as either 0 (not obstructed) or 2 (obstructed) since it is difficult to depict the ostiomeatal complex with any gradation. The ten scores for the various sinuses and bilateral ostiomeatal complexes are then added to give a bilaterally total CT score ranging from 0 (complete lucency of all sinuses) to 24 (complete opacity of all sinuses) [35]. Yan et al. have shown that in eosinophilic CRSwNP the occurrence of bilateral nasal polyps and total number of involved sinuses is significantly higher than in non- eosinophilic CRSwNP, in addition to more severe sinus disease in eosinophilic CRSwNP compared to non- eosinophilic CRSwNP. Therefore the resulting CT score is much higher in eosinophilic CRSwNP than in non- eosinophilic CRSwNP [18].
This study established E/M ratio as the most valuable predictor for the diagnosis of eosinophilic CRSwNP. The cut-off for E/M ratio in the current study was 2.065. We came across only two studies reporting E/M ratio to be a valuable indicator of eosinophilic CRSwNP [2, 11]. Meng et al. found the E/M ratio cut-off point to be more than 2.59 for the diagnosis of eosinophilic CRSwNP, while Kim et al. determined the cut-off point of E/M ratio for eosinophilic CRSwNP to be more than 2.167 [2, 11]. The high E/M ratio in eosinophilic CRSwNP patients implies that mainly the ethmoidal sinuses were affected in eosinophilic CRSwNP, whereas non-eosinophilic CRSwNP showed predominant maxillary involvement. Thus, our figures substantiate that the E/M ratio is one of the most useful surrogate markers for differentiating between eosinophilic and non-eosinophilic subtypes of patients with CRSwNP.
Conclusions
Chronic rhinosinusitis with nasal polyp occurs as eosinophilic and non-eosinophilic CRSwNP, each having different prognoses and ideal management. To the best of our knowledge, this is the first study in India conducted to compare the utility of CT score, IgE levels, AEC and SNOT-20 score for prediction of eosinophilic CRSwNP. Currently, only surgical biopsy, an invasive procedure, allows for their discrimination. We found the CT score (cut-off score-6), particularly the E/M ratio (cut-off score- 2.065), to be the most useful predictor in diagnosis of eosinophilic CRSwNP compared to the IgE levels, absolute eosinophil count and SNOT-20. The E/M ratio had a very high accuracy in the prediction of eosinophilic CRSwNP as per ROC curve analysis. Hence if these parameters are used to differentiate the 2 subtypes prior to surgery, it would be possible to pre-decide the postoperative drugs, i.e. steroids in case of eosinophilic CRSwNP and macrolides in case of non- eosinophilic CRSwNP. Moreover, it would be possible to clarify to patients with eosinophilic CRSwNP that they have a high probability of a poor postoperative prognosis and may require extended post-operative care.
References
Jain S, Das S, Gupta N, Malik JN (2013) Frequency of fungal isolation and antifungal susceptibility pattern of the fungal isolates from nasal polyp of chronic rhinosinusitis patients at a tertiary care centre in north India. Med Mycol 51:164–169
Kim D-K, Jin HR, Eun KM et al (2015) Non-eosinophilic nasal polyps shows increased epithelial proliferation and localized disease pattern in the early stage. PLoS ONE 10(10):e0139945. doi:10.1371/journal.pone.0139945
Fokkens W, Lund V, Mullol J (2007) European position paper on rhinosinusitis and nasal polyps 2007. Rhinol Suppl 20:1–136
Fokkens WJ, Lund VJ, Mullol J et al (2012) EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50(1):1–12
Akdis CA, Bachert C, Cingi C et al (2013) Endotypes and phenotypes of chronic rhinosinusitis: a PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol 131(6):1479–1490. doi:10.1016/j.jaci.2013.02.036
Snidvongs K, Chin D, Sacks R, Earls P, Harvey RJ (2013) Eosinophilic rhinosinusitis is not a disease of ostiomeatal occlusion. Laryngoscope 123:1070–1074
Haruna S, Shimada C, Ozawa M, Fukami S, Moriyama H (2009) A study of poor responders for long-term, low-dose macrolide administration for chronic sinusitis. Rhinology 47(1):66–71
Alatas N, Baba F, San I, Kurcer Z (2006) Nasal polyp diseases in allergic and nonallergic patients and steroid therapy. Otolaryngol Head Neck 135(2):236–242
Wang ET, Zheng Y, Liu PF, Guo LJ (2014) Eosinophilic chronic rhinosinusitis in East Asians. World J Clin Cases 2(12):873–882
Kim JW, Hong SL, Kim YK, Lee CH, Min YG, Rhee CS (2007) Histological and immunological features of non-eosinophilic nasal polyps. Otolaryngol Head Neck Surg 137:925–930
Meng Y, Lou H, Wang C, Zhang L (2016) Predictive significance of computed tomography in eosinophilic chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol 6(8):812–819. doi:10.1002/alr.21749
Ghai CL (2013) A textbook of practical physiology. Jaypee Brothers Medical Publishers (P) Ltd, New Delhi
Schalek P (2011) Rhinosinusitis—its impact on quality of life. In: Marseglia GL (ed) Peculiar aspects of rhinosinusitis. InTech. ISBN: 978-953-307-763-5. http://www.intechopen.com/books/peculiar-aspects-of-rhinosinusitis/rhinosinusitis-its-impact-on-quality-of-life
Nanishi K, Green J, Taguri M, Jimba M (2015) Determining a cut-off point for scores of the breastfeeding self-efficacy scale-short form: secondary data analysis of an intervention study in Japan. PLoS ONE 10(6):e0129698. doi:10.1371/journal.pone.0129698
Perkins NJ, Schisterman EF (2006) The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol 163(7):670–675. doi:10.1093/aje/kwj063
Fischer JE, Bachmann LM, Jaeschke R (2003) A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med 29(7):1043–1051. doi:10.1007/s00134-003-1761-8PMID: 12734652
Ishitoya J, Sakuma Y, Tsukuda M (2010) Eosinophilic chronic rhinosinusitis in Japan. Allergol Int 59:239–245
Yan Z, Pengfei L, Li-chuan K, Tong W (2015) Eosinophilic chronic rhinitis—sinusitis expression and significance of interleukin 13 and its receptor α2 [J]. Chin J Otorhinolaryngol Head Neck 50(3):230–235. doi:10.3760/cma.j.issn.1673-0860.2015.03.011
Ouyang Y, Fan E, Li Y, Wang X, Zhang L (2013) Clinical characteristics and expression of thymic stromal lymphopoetin in eosinophilic and non-eosinophilic chronic rhinosinusitis. ORL J Otorhinolaryngol Relat Spec 75:37–45
Smith AR, John W, Steinke JW, Payne S, Borish L (2015) Sinonasal outcome test questionnaire does not predict pathological diagnosis of chronic sinus disease. J Allergy Clin Immunol Suppl 135(2):AB56
Zhang XH, Lu X, Long XB et al (2009) Chronic rhinosinusitis with and without nasal polyps is associated with decreased expression of glucocorticoid-induced leucine zipper. Clin Exp Allergy 39:647–654
Xu M, Ye X, Zhao F, He Y, Chen L (2015) Allergogenic profile in patients with different subtypes of chronic rhinosinusitis with nasal polyps. ORL 77:10–16. doi:10.1159/000370121
Sakuma Y, Ishitoya J, Komatsu M et al (2011) New clinical diagnostic criteria for eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 38(5):583–588
Snidvongs K, McLachlan R, Chin D et al (2012) Osteitic bone: a surrogate marker of eosinophilia in chronic rhinosinusitis. Rhinology 50(3):299–305
Zuo K, Guo J, Chen F et al (2014) Clinical characteristics and surrogate markers of eosinophilic chronic rhinosinusitis in Southern China. Eur Arch Otorhinolaryngol 271(9):2461–2468. doi:10.1007/s00405-014-2910-0
Hu Y, Cao PP, Liang GT, Cui YH, Liu Z (2012) Diagnostic significance of blood eosinophil count in eosinophilic chronic rhinosinusitis with nasal polyps in Chinese adults. Laryngoscope 122:498–503. doi:10.1002/lary.22507
Hancer TS, Kasapoglu F, Demir UL, Ozmen OA, Coskun H, Basut O (2015) Correlation between clinical findings and eosinophil/neutrophil ratio in patients with nasal polyps. Eur Arch Otorhinolaryngol 272(4):915–921. doi:10.1007/s00405-014-3174-4
Tokunaga T, Sakashita M, Haruna T et al (2015) Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 70:995–1003
Kountakis SE, Arango P, Bradley D, Wade ZK, Borish L (2004) Molecular and cellular staging for the severity of chronic rhinosinusitis. Laryngoscope 114:1895–1905
Szucs E, Ravandi S, Goossens A, Beel M, Clement PAR (2002) Eosinophilia in the ethmoid mucosa and its relationship to the severity of inflammation in chronic rhinosinusitis. Am J Rhinol 16:131–134
Wabnitz DAM, Nair S, Wormald PJ (2005) Correlation between preoperative symptom scores, quality-of-life questionnaires, and staging with computed tomography in patients with chronic rhinosinusitis. Am J Rhinol 19:91–96
Hopkins C, Browne JP, Slack R, Lund V, Brown P (2007) The Lund-Mackay staging system for chronic rhinosinusitis: How is it used and what does it predict? Otolaryngol Head Neck Surg 137:555–561
Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW (2011) Revision rates after endoscopic sinus surgery: a recurrence analysis. Ann Otol Rhinol Laryngol 120:162–166
Batra PS, Tong L, Citardi MJ (2013) Analysis of comorbidities and objective parameters in refractory chronic rhinosinusitis. Laryngoscope 123(Suppl):S1–S11
Chen JJ, Chen DL, Chen CJ (2011) The Lund-Mackay score for adult head and neck computed tomography. J Radiol Sci 36:203–208
Thwin M, Weitzel EK, McMains KC et al (2009) Validating the use of report-derived Lund-MacKay scores. Am J Rhinol Allergy 23:33–35
Acknowledgements
We thankfully acknowledge the financial assistance provided to us by DBT (Department of Biotechnology) for conducting this research work. We also thank Dr. Arunaloke Chakrabarti, Professor and Head, Department of Medical Microbiology, Postgraduate Institute of Medical Education and Research, Chandigarh, as the Consortia Coordinator of the DBT funded project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rai, G., Roy, P., Gupta, N. et al. Computed Tomography Score an Excellent Marker: Differentiates Eosinophilic and Non-eosinophilic Variants of Chronic Rhinosinusitis with Nasal Polyp. Indian J Otolaryngol Head Neck Surg 71 (Suppl 3), 1787–1792 (2019). https://doi.org/10.1007/s12070-017-1154-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-017-1154-x