Abstract
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a frequent disease which can be classified as eosinophilic or neutrophilic based on dominant inflammatory cell type at tissue. The aim of this study was to evaluate the clinical relevance of classifying nasal polyps as eosinophilic or neutrophilic on treatment outcomes. The study was conducted with 40 patients who underwent either surgical or medical treatment with the diagnosis of CRSwNP. The patients were classified into two groups for further assessment up to eosinophil intensity at polyp tissue. All patients were examined by nasal endoscopy and paranasal computed tomography (CT). Before treatment, subjective symptom score, nasal endoscopy score, and CT score were measured. Subsequently, they were reevaluated by similar diagnostic tests after either medical or surgical treatment at sixth month. The preoperative subjective symptom score, endoscopy score, and paranasal CT score were compared between chronic rhinosinusitis (CRS) with eosinophilic nasal polyps (E-NP) (CRSwE-NP) group and CRS with neutrophilic nasal polyps group and there was no difference between the two groups (p = 0.369, p = 0.310 and p = 0.494 respectively). Although after treatment in both groups symptom score and endoscopy score were significantly improved but not the CT score, we found no difference in between the groups at sixth month. In most of the previous studies, patients with CRSwE-NP were assumed to have poor prognosis and high recurrence rate despite surgical or medical treatment. However, we did not find any association between eosinophilic or neutrophilic nature of nasal polyp tissue and disease severity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a frequent local inflammatory disease of nasal and paranasal sinus mucosa which has negative impacts on quality of life [1]. It restricts daily physical activity in affected individuals and leads to work absenteeism with increasing health care burden [2–4]. Despite evolving medical and surgical treatment options, many patients still have recurrent or persistent rhinosinusitis. Therefore, the clinical and histopathological parameters which influence the prognosis and severity in CRS are important to identify. To better understand the disease course and predict outcomes of treatment, some authors previously categorized CRS into various subtypes, such as; eosinophilic CRS or noneosinophilic CRS [5, 6], eosinophilic CRS with (CRSwNP) or without nasal polyp (CRSsNP) and noneosinophilic CRSwNP or CRSsNP [7], eosinophilic CRSwNP, neutrophilic CRSwNP or noneosinophilic nonneutrophilic CRSwNP [8].
CRS is recently classified into two broad categories by European Rhinology study group: CRSwNP and CRSsNP [9]. CRSwNP can be further subclassified into eosinophilic CRSwNP or neutrophilic CRSwNP. This latter subclassification is based on predominant inflammatory cell type and cytokine expression that modulate mucosal immunity [8]. In many previous studies, eosinophilic inflammation at nasal mucosa was shown to play a role in nasal polyp pathogenesis and it has negative impacts on prognosis and worse treatment outcomes [6–8, 10–12]. Although the histopathological characteristics of nasal polyps may differ worldwide, in general, Western and European populations have significant mucosal eosinophilia and eosinophilic inflammation at nasal polyps [6, 7, 13, 14]. However, in Asian and Eastern populations, nasal polyps show mostly neutrophilic type inflammation [5, 13, 15, 16]. CRSwNP has different histopathological and clinical aspects; thus, determination of the predictive factors and their clinical significance is important while dealing with those patients.
The aim of this study was to evaluate the clinical relevance of classifying nasal polyps as eosinophilic or neutrophilic in relation with other risk factors and to compare the treatment outcomes between these patients by subjective and objective methods.
Materials and methods
This study was conducted at the University of Uludag, Department of Otolaryngology between December 2011 and December 2012. The study was approved by the ethical committee of medical school and a signed informed consent form was taken from each patient. Forty patients who underwent either surgical or medical treatment with the diagnosis of chronic rhinosinusitis with nasal polyps were enrolled in the study. The diagnostic criteria were in accordance with EPOS guidelines [9]. The exclusion criteria were; (1) unilateral nasal polyp, (2) antrochoanal polyp, (3) inverted papilloma, (4) nasal or paranasal malignancy, and (5) cystic fibrosis.
The medical records of these patients including previous surgery, medical treatment, presence of allergy or asthma, aspirin hypersensitivity, smoking habit, and presence of any systemic disease were retrieved from patients’ files. The subjective symptom score was evaluated by an arbitrary scoring system. In this system, we scored five major complaints (nasal obstruction, rhinorrhea, postnasal discharge, loss of smell, and chronic cough) from 0 to 3 points according to symptom severity. All patients underwent complete examination including nasal endoscopy. Nasal polyps at endoscopy were scored from 0 to 3 points for each nasal cavity and staged according to the system outlined by Lund-Kennedy [17]. We performed skin prick test covering 20 items to each patient and assessed the presence of allergy to these allergens. The diameter of induration and hyperemia above 3 mm was accepted as positive for that item. Nasal biopsy was taken from polypoid lesions under endoscopy at first visit on admission at the outpatient clinic. These tissue specimens were examined at pathology department under microscopy (400×) with H&E stain by same senior pathologist. The pathology colleague counted a total of 100 inflammatory cells (only eosinophils and neutrophils) in the field with the greatest cellular intensity and determined the percentage of each cell type. Nasal polyp was accepted as eosinophilic if the eosinophil count was above 50 % or as neutrophilic if the neutrophil count was above that percentage. All patients underwent paranasal sinus computed tomography (CT) imaging to evaluate the disease severity by radiological staging. The radiological findings were assessed according to Lund-Mackay [18] staging system. We also performed peripheric cell count to measure eosinophil percentage at circulation. Unfortunately, we could attain hemogram results of only 29 patients. We accepted circulating eosinophil count above 7 % as eosinophilia.
Patients were given maximal medical treatment with antibiotics (macrolides 500 mg) for at least 4 weeks, oral corticosteroids (prednisolone 60 mg per day) for 1 week, and nasal topical steroids for 2 months. Subsequently, patients who did not accept surgical treatment were put on topical nasal steroid treatment for further 6 months. Those who decided for surgical treatment underwent endoscopic sinus surgery. We used Messerklinger’s anterior to posterior technique and extended surgical margins to sphenoid or frontal sinus if required. All patients were reevaluated with similar staging and scoring systems at the end of 6 months. The results were compared to pretreatment scores considering other risk factors.
Statistical analysis was carried out using SPSS Statistics 21 (SPSS Inc, IBM, USA). The continuous variables were presented as mean ± standard deviation, median (minimum–maximum) and n (%) according to distribution characteristics. Mann–Whitney U test was performed for comparison of two discrete groups. Wilcoxon test was used for comparison of two dependent groups. p < 0.05 was set at statistical significance and it was used for performing statistical analysis.
Results
The study group consisted of 27 male and 13 female patients with a median age of 43 (13–77) years. These patients were classified as chronic sinusitis with eosinophilic nasal polyps (CRSwE-NP) or chronic sinusitis with neutrophilic nasal polyps (CRSwN-NP) up to eosinophil intensity in polyp tissue. The comparative analysis between two subgroups showed no difference regarding age and gender. These two groups were compared with regard to other risk factors such as asthma, aspirin sensitivity, smoking, and presence of any systemic disease and we found no significance; p = 0.69, p = 1.00, p = 0.437 and p = 0.083, respectively (Table 1). However in CRSwN-NP group, smoking and systemic disease were present in almost half of the patients.
Skin prick test was positive in 25 % (10/40) of all patients but there was no difference in between two groups (p = 0.665). Furthermore, there was no significance regarding to circulating eosinophil count (p = 1.00). We evaluated the association between blood eosinophil count and existence of asthma, prick test positivity and aspirin sensitivity and there was significance between blood eosinophilia and both asthma and aspirin hypersensitivity but not skin prick test positivity (Table 2).
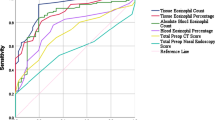
Preoperative subjective symptom score, endoscopy score, and paranasal CT score were compared between CRSwE-NP and CRSwN-NP groups and we found no difference between two groups (p = 0.369, p = 0.310 and p = 0.494 respectively). There was also no difference in these scores between groups after the sixth month of treatment (Table 3). We indicated that symptom score and endoscopy score were significantly improved with treatment in both groups, however, paranasal CT score showed nonsignificant improvement in both groups (p = 0.494 and p = 0.269 respectively) (Table 4).
We performed surgery in 27 patients and among these patients 20 belong to CRSwE-NP group and seven patients belong to CRSwN-NP group. Of these surgeries, seven interventions were primary sinus surgery (7/27, 25.9 %) and two of these primary cases underwent revision surgery at 14th and 16th month due to recurrence. Among CRSwE-NP patients, 80 % (16/20) of surgeries were performed for revision cases and in CRSwN-NP patients, this ratio was lower 57.1 % (4/7). Endoscopic staging of nasal polyps before and after surgery revealed that two patients in both groups had stage 2 nasal polyp recurrence at the end of sixth month. Furthermore, nine patients in CRSwE-NP and one patient in CRSwN-NP group had stage 1 disease after treatment (Fig. 1).
Discussion
Nasal polyp is very frequent among all ethnicities with high prevalence [19, 20]. However, the clinical behavior, predominant inflammatory cell type, and histology of nasal polyps may highly differ between different races and cultures [21, 22]. Although in most of the western populations the dominant inflammatory cells are eosinophils, this is not the case in eastern Asian populations who have noneosinophilic type NP domination [13–16]. However, Caucasian and Asian patients both reveal low T regulation activity and low TGF-b that may play key role in NP pathogenesis [23]. Kim et al. [24] reported that in only 33 % of patients with NP, there was eosinophilic inflammation. In another study, the authors assessed the change at tissue eosinophilia in CRSwNP patients during 17 years period in Korean population. They compared the patients who underwent sinus surgery in 1994 with similar patient group in 2011 and pointed out that eosinophilic NP increased from 24 to 50.9 % during this period [25]. In our study, the eosinophilic NP patients comprised the majority of patients (77.5 %) similar to other caucasian populations.
There are still controversies on the etiology and pathophysiology of nasal polyposis albeit on several ongoing randomized studies. Since the etiological factors are diverse and prognosis highly depends on these factors, it is difficult to predict the outcomes of treatment without understanding them. Tissue eosinophilia in nasal polyp is considered as an important parameter in both treatment strategy and prognosis. In previous studies, eosinophilic inflammation was reported to be related with disease severity. The patients with eosinophilic NP were found refractory to both surgical and medical treatment with high recurrence rates [7, 8, 11, 12]. Thus to differentiate heterogenous group of CRSwNP patients into eosinophilic and noneosinophilic subtypes may have clinical importance in selecting effective therapeutic strategy and predicting prognosis.
Since asthma and nasal polyp may coexist and show similar allergic symptoms, allergy was presumed to be the triggering factor in NP. Furthermore, these patients may have both high IgE count and eosinophilic inflammation at stromal tissue. Asero and Bottazi [26] reported that in 63 % of patients with NP, skin prick test was positive. However in patients with CRSsNP, skin prick test positivity was significantly lower (16.6 %). Similarly, Collins et al. [27] conducted a study with 40 NP patients and compared them with nonallergic control group in order to find the difference between groups in regard to intradermal and skin prick allergy test results. They showed that in patients with NP positivity of these tests was significantly higher; 35 and 19 %, respectively. Ouyang et al. [15] showed that patients with eosinophilic CRS had significantly high positivity to allergy test compared to noneosinophilics; 80.6 and 14 %, respectively. They concluded that clinical findings in eosinophilic CRS are likely to be influenced by atopic status of the patients. Mendelsohn et al. [28] reviewed 549 consecutive patients who underwent endoscopic surgery for NP and they reported that revision rate for recurrent disease was higher in patients with coexisting asthma and Samter’s triad. In our study, 25 % of patients with NP had positive skin prick test. However, there was no difference between eosinophilic and neutrophilic patient groups regarding to skin prick test positivity (p = 0.665).
Mean paranasal CT score in normal adult population by Lund-Mackay scoring system was found 4.26 [29]. Hopkins et al. [30] revealed in a large cohort study that mean CT score with 1,840 CRSwNP patients was 13.6 but it was found 7.0 in patients without NP. Ikeda et al. [8] indicated significantly worse symptom and CT scores in patients with CRSwE-NP. We found mean CT score as 16.8 that was far beyond the normal adult value. However, there was no difference between eosinophilic and neutrophilic NP patient groups. Blood eosinophil count is another parameter used to evaluate and classify patients with nasal polyp. Di Lorenzo et al. [31] compared total serum IgE, eosinophilic cationic protein (ECP), and blood eosinophilia between patients with NP and patients with allergic rhinitis. They reported that eosinophil count was significantly higher in patients with NP but not total IgE and ECP Similarly, Yoshimi et al. [32] found that all patients with coexisting NP and aspirin induced asthma had higher eosinophil count but normal total IgE. We found 10.7 % higher blood eosinophil count in study group but no difference between eosinophilic and neutrophilic NP groups. In addition, we found significant correlation between blood eosinophil percentage and both asthma existence (p = 0.013) and aspirin hypersensitivity (p = 0.033). Up to these findings we argued that blood eosinophilia was not directly reflecting allergic reactions, however, it might have association with formation of NP.
To better understand the pathophysiology of NP, clinical parameters like tissue eosinophila or neutrophilia and their indicators (ECP, ICAM, IL-5 and IL-8) should be investigated. However, definite description and diagnosis of tissue eosinophilia is still controversial. Soler et al. [7] showed that more than 5 eosinophil/HPF can be used as criteria for clinical assessment and more than 10 eosinophil/HPF for quality of life assessment. They indicated that 66.7 % of patients with CRSwNP were eosinophilic, but in all CRS patients eosinophilia was lower (35.8 %). There was no difference between eosinophilic CRSwNP and noneosinophilic CRSwNP in regard to endoscopy score, CT score and quality of life in that study. In another study, Matsuwaki et al. [11] evaluated the factors which influenced the recurrence rate following endoscopic sinus surgery. They showed that more than 120 eosinophil/HPF was a significant indicator of recurrence. In addition, they mentioned that blood eosinophilia and asthma were also significantly related with recurrence. In a recent study, the authors classified CRSwNP patients into eosinophilic and non-eosinophilic according to microscopic (400×) evaluation of nasal polyp tissue. More than 100 eosinophils observed in three fields were accepted as eosinophilic and more than 20 neutrophils as neutrophilic [8]. Sakuma et al. [5] established a new clinical diagnostic criteria for eosinophilic CRS. They pointed out that increased blood eosinophil percentage above normal and CT score ≥1 for both olfactory cleft and posterior ethmoid could be used to differentiate eosinophilic versus noneosinophilic CRS with high accuracy. In our study, we examined tissue sections under microscope (400×) and counted both eosinophils and neutrophils in the field until they reach 100 cells in total. Subsequently, we categorized nasal polyps into eosinophilic if eosinophil count reached ≥50 % or neutrophilic if neutrophil count was ≥50 %.
Eosinophilic inflammation at nasal mucosa was suggested to be more important factor in predicting outcome in CRS rather than nasal polyp itself [12]. In the study of Soler et al. [10] mucosal eosinophilia was shown to be a significant prognostic factor for improvement at disease specific QOL after surgery. Patients with CRSwE-NP had worse prognosis and they were more responsive to steroid treatment but noneosinophilic patients were responsive to macrolides and surgical treatment [5]. Tosun et al. [33] reported that nasal polyp recurrence was more in patients with high tissue eosinophil count. Therefore, those patients did require more revision surgeries. In another study, they categorized 130 patients with CRSwNP into three groups as eosinophilic, neutrophilic, and non-eosinophilic–non-neutrophilic for further assessment. Blood eosinophil count, atopy, symptom score, and CT score were found to be worse in eosinophilic group compared to other groups. They also showed that recurrence and revision rates were significantly higher in eosinophilic group [8]. In a Chinese study including 86 CRS patients, nasal polyp existence was higher in eosinophilic group compared to noneosinophilic; 67.7 and 50 % respectively. In addition, endoscopy score and subjective symptoms such as olfactory loss and cough were significantly worser in eosinophilics [15]. We did not find any difference between groups regarding to symptom score and CT score. We argued that this may be related to low number of patients and relatively short follow-up. In our study, recurrence rate in eosinophilic NP was slightly higher than neutrophilic NP; 55 and 42.8 %, respectively. Thus, we believed that informing all patients with NP about high recurrence rate is very important.
One important aim of treatment in CRSwNP patients is to improve quality of life by relieving nasal obstruction, smell disturbance, and postnasal discharge. In previous studies, the success of endoscopic sinus surgery reported to be very high up to 73–97.5 % [34]. Mehanna et al. [35] showed that most significant improvement after surgery was gained in CRSwNP patients compared to other CRS patients. Soler et al. [10] compared the level of improvement at QOL indices in CRS patients and they revealed that most significant postoperative improvement was across noneosinophilic CRS patients. Medical treatment with oral and nasal steroids was also considered as an option in the treatment of those patients [36]. However, combined surgical and medical treatment showed better improvement regarding CT score and olfactory thresholds compared to single medical treatment [37]. Surgical interventions in patients with NP remove airway obstruction, provide effective sinus drainage and enhance topical application of nasal steroids but does not treat mucosal inflammation. Thus nasal topical steroids are still the mainstay of treatment in long term. We found significant improvement in both eosinophilic and neutrophilic patients in regard to symptom score and endoscopy score following treatment. However, CT score did improved without significance. This finding signified the fact that we, as surgeons, do not treat the imaging but the disease itself with related symptoms.
Surgical interventions not only alleviate the burden of disease but also enhance the efficacy of medical treatment afterwards. Recent advancements in humanized monoclonal antibody medications (anti IL-5) showed that these drugs improved the disease severity by acting on eosinophil maturation and activation [38]. In a study with 20 patients with CRSwE-NP, mepolizumab (3 mg/kg) treatment for 8 weeks decreased blood eosinophil count, ECP level, clinical symptoms, and nasal polyp dimensions [39]. Eosinophil targeted treatments (anti IL-5 and steroid) were favored in patients with CRSwE-NP but surgical treatment is still the mainstay of treatment in CRSwN-NP to relieve sinus obstruction [40]. We mentioned that histological classification of nasal polyps is highly important in deciding treatment modality. Although eosinophil predominance is not necessary for pathogenesis of polyps, it has negative influence on disease severity with poor prognosis especially in caucasians. We believed that further randomized and placebo-controlled clinical trials are required to better understand this association.
Conclusion
In most of the previous studies, patients with CRSwE-NP were assumed to have poor prognosis and more recurrence rates despite advanced surgical or medical treatments. However, we did not find any association between eosinophilic or neutrophilic nature of nasal polyp and the disease severity. In the guidance of our findings, we concluded that precise therapeutic interventions can be established by detailed examination of polyps. Patients should also be informed during clinical consultations about treatment outcomes and likelihood of recurrence.
References
Lange B, Holst R, Thilsing T, Baelum J, Kjeldsen A (2013) Quality of life and associated factors in persons with chronic rhinosinusitis in the general population. Clin Otolaryngol. 2013 Oct 16. doi:10.1111/coa.12189. [Epub ahead of print]
Anand VK (2004) Epidemiology and economic impact of rhinosinusitis. Ann Otol Rhinol Laryngol Suppl 93:3–5. Review
Benninger MS, Sedory Holzer SE, Lau J (2000) Diagnosis and treatment of uncomplicated acute bacterial rhinosinusitis: summary of the agency for health care policy and research evidence-based report. Otolaryngol Head Neck Surg 122:1–7
Soler ZM, Mace JC, Litvack JR, Smith TL (2012) Chronic rhinosinusitis, race, and ethnicity. Am J Rhinol Allergy 26:110–116
Sakuma Y, Ishitoya J, Komatsu M, Shiono O, Hirama M, Yamashita Y et al (2011) New clinical diagnostic criteria for eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 38:583–588
Ferguson BJ (2004) Categorization of eosinophilic chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg 12:237–242
Soler ZM, Sauer DA, Mace J, Smith TL (2009) Relationship between clinical measures and histopathologic findings in chronic rhinosinusitis. Otolaryngol Head Neck Surg 141:454–461
Ikeda K, Shiozawa A, Ono N, Kusunoki T, Hirotsu M, Homma H, Saitoh T, Murata J (2013) Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 123:E1–E9
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F et al (2012) EPOS 2012: european position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50:1–12
Soler ZM, Sauer D, Mace J, Smith TL (2010) Impact of mucosal eosinophilia and nasal polyposis on quality-of-life outcomes after sinus surgery. Otolaryngol Head Neck Surg 142:64–71
Matsuwaki Y, Ookushi T, Asaka D, Mori E, Nakajima T, Yoshida T et al (2008) Chronic rhinosinusitis: risk factors for the recurrence of chronic rhinosinusitis based on 5-year follow-up after endoscopic sinus surgery. Int Arch Allergy Immunol 146(Suppl 1):77–81
Nakayama T, Yoshikawa M, Asaka D, Okushi T, Matsuwaki Y, Otori N et al (2011) Mucosal eosinophilia and recurrence of nasal polyps—new classification of chronic rhinosinusitis. Rhinology 49:392–396
Zhang N, Van Zele T, Perez-Novo C, Van Bruaene N, Holtappels G, DeRuyck N et al (2008) Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol 122:961–968
Ferguson BJ, Seethala R, Wood WA (2007) Eosinophilic bacterial chronic rhinosinusitis. Laryngoscope 117:2036–2040
Ouyang Y, Fan E, Li Y, Wang X, Zhang L (2013) Clinical characteristics and expression of thymic stromal lymphopoetin in eosinophilic and non-eosinophilic chronic rhinosinusitis. ORL J Otorhinolaryngol Relat Spec 75:37–45
Ishitoya J, Sakuma Y, Tsukuda M (2010) Eosinophilic chronic rhinosinusitis in Japan. Allergol Int 59:239–245
Lund VJ, Kennedy DW (1997) Staging for rhinosinusitis. Otolaryngol Head Neck Surg 117:S35–S40
Lund VJ, Mackay IS (1993) Staging in rhinosinusitis. Rhinology 31:183–184
Johansson L, Akerlund A, Holmberg K (2003) Prevalence of nasal polyps in adults: the Skövde population-based study. Ann Otol Rhinol Laryngol 112:625–629
Klossek JM, Neukirch F, Pribil C (2005) Prevalence of nasal polyposis in France: a cross-sectional, case-control study. Allergy 60:233–237
Hu Y, Cao PP, Liang GT, Cui YH, Liu Z (2012) Diagnostic significance of blood eosinophil count in eosinophilic chronic rhinosinusitis with nasal polyps in Chinese adults. Laryngoscope 122:498–503
Lacroix JS, Zheng CG, Goytom SH, Landis B, Szalay-Quinodoz I, Malis DD (2002) Histological comparison of nasal polyposis in black African Chinese and Caucasian patients. Rhinology 40:118–121
Van Crombruggen K, Zhang N, Gevaert P, Tomassen P, Bachert C (2011) Pathogenesis of chronic rhinosinusitis: inflammation. J Allergy Clin Immunol 128:728–732
Kim JW, Hong SL, Kim YK, Lee CH, Min YG, Rhee CS (2007) Histological and immunological features of non-eosinophilic nasal polyps. Otolaryngol Head Neck Surg 137:925–930
Kim SJ, Lee KH, Kim SW, Cho JS, Park YK, Shin SY (2013) Changes in histological features of nasal polyps in a Korean population over a 17-year period. Otolaryngol Head Neck Surg 149:431–437
Asero R, Bottazzi G (2001) Nasal polyposis: a study of its association with airborne allergen hypersensitivity. Ann Allergy Asthma Immunol 86:283–285
Collins MM, Loughran S, Davidson P, Wilson JA (2006) Nasal polyposis: prevalence of positive food and inhalant skin tests. Otolaryngol Head Neck Surg 135:680–683
Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW (2011) Revision rates after endoscopic sinus surgery: a recurrence analysis. Ann Otol Rhinol Laryngol 120:162–166
European academy of All Clin Immun EPOS Rhinol Suppl 2012
Hopkins C, Browne JP, Slack R, Lund V, Brown P (2007) The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryngol Head Neck Surg 137:555–561
Di Lorenzo G, Drago A, Esposito Pellitteri M, Candore G, Colombo A, Gervasi F et al (2001) Measurement of inflammatory mediators of mast cells and eosinophils in native nasal lavage fluid in nasal polyposis. Int Arch Allergy Immunol 125:164–175
Yoshimi R, Takamura H, Takasaki K, Tsurumoto H, Kumagami H (1993) Immunohistological study of eosinophilic infiltration of nasal polyps in aspirin-induced asthma. Nihon Jibiinkoka Gakkai Kaiho 96:1922–1925
Tosun F, Arslan HH, Karslioglu Y, Deveci MS, Durmaz A (2010) Relationship between postoperative recurrence rate and eosinophil density of nasal polyps. Ann Otol Rhinol Laryngol 119:455–459
Terris MH, Davidson TM (1994) Review of published results for endoscopic sinus surgery. Ear Nose Throat J 73:574–580. Review
Mehanna H, Mills J, Kelly B, McGarry GW (2002) Benefit from endoscopic sinus surgery. Clin Otolaryngol Allied Sci 27:464–471
Bhattacharyya N, Kepnes LJ (2013) Medications prescribed at ambulatory visits for nasal polyposis. Am J Rhinol Allergy 27:479–481
Blomqvist EH, Lundblad L, Bergstedt H, Stjärne P (2009) A randomized prospective study comparing medical and medical-surgical treatment of nasal polyposis by CT. Acta Otolaryngol 129:545–549
Bolard F, Gosset P, Lamblin C, Bergoin C, Tonnel AB, Wallaert B (2001) Cell and cytokine profiles in nasal secretions from patients with nasal polyposis: effects of topical steroids and surgical treatment. Allergy 56:333–338
Gevaert P, Van Bruaene N, Cattaert T, Van Steen K, Van Zele T, Acke F et al (2011) Mepolizumab, a humanized anti-IL-5 mAb, as a treatment option for severe nasal polyposis. J Allergy Clin Immunol 128:989–995
Payne SC, Early SB, Huyett P, Han JK, Borish L, Steinke JW (2011) Evidence for distinct histologic profile of nasal polyps with and without eosinophilia. Laryngoscope 121:2262–2267
Conflict of interest
None.
Ethical standards
This study was approved by the ethical committee of Medical School and an informed consent form was assigned by each participant patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tecimer, S.H., Kasapoglu, F., Demir, U.L. et al. Correlation between clinical findings and eosinophil/neutrophil ratio in patients with nasal polyps. Eur Arch Otorhinolaryngol 272, 915–921 (2015). https://doi.org/10.1007/s00405-014-3174-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3174-4