Abstract
Neurological dysfunction as a result of neuroinflammation has been reported in sepsis and cause high mortality. High levels of cytokines stimulate the formation of neurotoxic metabolites by kynurenine (KYN) pathway. Vitamin B6 (vit B6) has anti-inflammatory and antioxidant properties and also acts as a cofactor for enzymes of the KYN pathway. Thus, by using a relevant animal model of polymicrobial sepsis, we studied the effect of vit B6 on the KYN pathway, acute neurochemical and neuroinflammatory parameters, and cognitive dysfunction in rats. Male Wistar rats (250–300 g) were submitted to cecal ligation and perforation (CLP) and divided into sham + saline, sham + vit B6, CLP + saline, and CLP + vit B6 (600 mg/kg, s.c.) groups. Twenty-four hours later, the prefrontal cortex and hippocampus were removed for neurochemical and neuroinflammatory analyses. Animals were followed for 10 days to determine survival rate, when cognitive function was assessed by behavioral tests. Vitamin B6 interfered in the activation of kynurenine pathway, which led to an improvement in neurochemical and neuroinflammatory parameters and, consequently, in the cognitive functions of septic animals. Thus, the results indicate that vit B6 exerts neuroprotective effects in acute and late consequences after sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a common clinical syndrome in intensive care units (ICUs), with mortality rates that reach 60% [1]. The development of organ dysfunction is a complication that contributes to increased mortality in sepsis, and the brain is particularly affected [2, 3].
In sepsis, the acute brain dysfunction is known as sepsis-associated encephalopathy (SAE), which manifests itself in up to 70% of septic patients and is associated with a worst prognosis [4]. Neuroinflammation, ischemia, and neurotoxicity are the main processes implicated in SAE [5,6,7]. Particularly, neuroinflammation increases the metabolic and bioenergetic demands, which may result in oxidative stress and mitochondrial dysfunction [8].
Indeed, early mitochondrial dysfunction has been detected in the brain of septic animals, resulting in the production of reactive oxygen (ROS) and nitrogen (RNS) species. The production of reactive species stimulates a pro-apoptotic state that affects glial cells, neurons, and blood brain barrier (BBB) structure [9].
One pathway that may be related to the progression of neurological damage in sepsis is the kynurenine (KYN) pathway. Critically ill patients may exhibit elevated levels of KYN in the expense of tryptophan (TRP) plasmatic level depletion [10, 11]. During active inflammation, indoleamine 2,3-dioxygenase (IDO) is activated in extrahepatic tissues to convert TRP into KYN [12]. This is followed by the synthesis of enzymes that regulate the generation of neurotoxic metabolites, such as 3-hydroxykynurenine, 3-hydroxyanthranilic acid, and quinolinic acid. The neurotoxicity mediated by these metabolites is related to ROS formation.
Vitamin B6 (vit B6) acts as cofactor of these enzymes and could modulate the production of these metabolic intermediates [13]. In addition, vit B6 performs important functions, including the modulation of inflammatory response and oxidative stress [14]. Reduced plasmatic level of vit B6 is associated with oxidative stress, immune system disorders, and disturbances in glucose metabolism [15,16,17]. On the other hand, adequate levels of vit B6 are positively correlated with increased levels of antioxidant enzymes [18, 19].
These evidences point out to a possible positive role of vit B6 in the genesis of brain dysfunction in sepsis. Thus, the purpose of this study was to examine the effect of vit B6 on survival, kynurenine pathway activation, acute neuroinflammation, and long-term cognitive dysfunction in a preclinical model of sepsis.
Materials and Methods
Animals
Adult male Wistar rats, approximately 60 days old (weighing 250–350 g), from breeding colonies maintained at the Universidade do Sul de Santa Catarina were used. The animals were housed five per cage under controlled conditions of temperature (22 ± 1 °C), relatively humidity (45–55%), and day/light cycle (12:12-h, light on at 0600 hours). Rat chow (standard diet for laboratory animals—NUVILAB CR-1®, Brazil) and tap water were available ad libitum. This study was approved by the Animal Research Ethic Committee of the Universidade do Sul de Santa Catarina (protocol #15.012.4.03.IV). The “Principles of Laboratory Animal Care” (NIH publication no. 80–23, revised 1996) and the “EC Directive 86/609/EEC” were followed in all experiments. All efforts were made to minimize the number of animals used and their suffering.
Sepsis Induction—CLP Model
Rats were subjected to cecal ligation and perforation (CLP) as previously described [20]. Briefly, they were anesthetized intraperitoneally (i.p.) with a mixture of ketamine (80 mg/kg) and xylazine (10 mg/kg). Under aseptic conditions, a 3-cm midline laparotomy was performed to expose the cecum and adjoining intestine. The cecum was tightly ligated with a 3.0 silk suture at its base, below the ileocecal valve, and was perforated once with 14-gauge needle. The cecum was then squeezed gently to extrude a small amount of feces through the perforation site. The cecum was then returned to the peritoneal cavity, and the laparotomy was closed with 4.0 silk sutures. Animals were resuscitated with regular saline (50 mL/kg) subcutaneously (s.c.) immediately after CLP, ceftriaxone (30 mg/kg), and dipyrone (80 mg/kg) s.c. immediately after and 12 h after CLP and were returned to their cages with free access to food and water. In the sham-operated group, the rats were submitted to all surgical procedures, but the cecum was neither ligated nor perforated. To minimize variability between different experiments, the CLP procedure was always performed by the same investigators.
Treatments and Samples Obtention
Vit B6 was obtained from Fagron (São Paulo, BRA) and dissolved in saline immediately before use. Immediately after CLP surgery, rats received 600 mg/kg s.c. of vit B6 or the same volume of saline [21]. Four groups (n = 10 per group) were randomly divided into the following: (1) sham + saline; (2) sham + vit B6, (3) CLP + saline, and (4) CLP + vit B6. For the acute neuroinflammation assays, rats were followed during 24 h (experiments 1 and 2 such as Fig. 1). For survival analysis, animals were followed during 10 days and deaths were counted daily (experiment 3 such as Fig. 1). The long-term cognitive dysfunction was evaluated by behavioral tests initiated on day 10 (experiment 3 such as Fig. 1). After each experimental time-point, animals were subjected to a thiopental overdose (0.5 g/kg) followed by decapitation. The prefrontal cortex and hippocampus were quickly isolated and stored at − 80 °C for subsequent biochemical analysis [22].
Experimental design. The rats were induced to sham (control) or sepsis by CLP. Immediately after CLP surgery, rats received 600 mg/kg s.c. of vit B6 or the same volume of saline. In the experiment 1, after 24 h in the prefrontal cortex and hippocampus, kynurenine, tryptophan, and the tryptophan/kynurenine ratio , oxidative stress, and neuroinflammation were evaluated. In the experiment 2, in the 24 h, the BBB permeability was evaluated, and 10 days after CLP in the experiment 3, behavioral tests and survival was evaluated
IDO Activation
Sample Preparation
Samples were added with three volumes of ice cold methanol (50 μL + 150 μL), vortexed, and centrifuged at 14×g for 10 min (4 °C). Hydrophobic compounds (fatty acids, proteins) were removed from the supernatant using activated C18 resin. The C18 resin was previously activated by conditioning it twice with 300 μL of sample solvent (75% methanol) followed by centrifugation at 14 rpm for 10 min (room temperature). Activated C18 resin was added to the samples at the proportion of 1/5 of the sample mass (10 mg), vortexed, and centrifuged as above. Supernatant was transferred to a new tube and solvent was removed in a SpeedVac. Samples were reconstituted in the same volume of MilliQ water and transferred to 100 μL polypropylene vials and placed in a cooled autosampler (5 °C) until 20 μL was injected in the LC-MS system in the same day.
Liquid Chromatography-Mass Spectrometry
TRP and the KYN standards were purchased from Sigma-Aldrich (St. Louis, MO) with 96% purity. Liquid chromatography-mass spectrometry (LC-MS) analyses were performed on a Nexera Ultra High Performance Liquid Chromatography (UHPLC) system (Shimadzu, Kyoto, Japan) hyphenated to a maXis ETD high-resolution Electrospray ionization quadrupole time-of-flight (ESI-QTOF) mass spectrometer (Bruker, Billerica, MA) and controlled by the Compass 1.5 software package (Bruker). Fifty microliters of standards and samples were injected into a Shimadzu Shim-Pack XR-ODSIII column (C18, 2.2 μm, 80 Å, 2.2 × 200 mm) at 30 °C under a flow rate of 200 μL/min. Elution of TRP and KYN was achieved with the mobile phases A and B (0.1% formic acid in water resp. methanol) as follows: 01 min 3% B, 1–17 min 3 30% B, 17–18 min 30, 100% B, 18–23 min 100% B.
Mass spectra were acquired in positive ion mode between m/z 40,300 and at a spectra rate of 0.5 Hz. Ion source parameters were set to 500 V end plate offset, 4500 V capillary voltage, 2.0 bar nebulizer pressure, 8.0 L/min, and 200 °C dry gas flow resp. ion source temperature. Ion cooler settings were optimized for sensitivity in the mentioned m/z range using 10 mM sodium formate/acetate in 50% 2-propanol as calibrant solution. Mass calibration was achieved by initial ion source infusion of 20 μL calibrant solution and post-acquisition recalibration of the raw data.
Standard mixtures were injected in a concentration range between 0.8 and 1000 ng/mL in phosphate-buffered saline to yield the calibration curves for each compound. Between the samples, individual standard mixtures with 100 ng/mL of each metabolite were injected to monitor the system stability. The calibration as well as the sample data were post-processed and analyzed via the QuantAnalysis software (Bruker) which extracts the high-resolution ion chromatograms (EICs) of the listed target metabolites, and integrates the chromatographic peaks in the retention time windows according to the recorded calibration curves of the respective standard compounds. The curve regression factors within the concerning concentration ranges were 0.995 or higher.
Enzymatic Activity of IDO
The activity of IDO in the prefrontal cortex and hippocampus was determined by the ratio of TRP and KYN concentrations [23].
BBB Permeability Analysis
The integrity of the BBB was investigated using Evans blue dye extravasation [24]. The dye was administered (2% wt/vol in phosphate-buffered saline; PBS) intravenously (3 mL/kg) through the femoral vein. The animals were perfused 1.5 h after using normal saline (250 mL) through the left ventricle at 110 mmHg pressure until colorless perfusion fluid was obtained from the right atrium. Quantitative evaluation of BBB permeability was achieved by measuring the content of Evans blue in the hippocampus and prefrontal cortex by its fluorescence intensity (Spectramax M2 microplate reader, Molecular Devices). The results were expressed as nanogram/milliliter of brain tissue.
Myeloperoxidase Activity
Neutrophil infiltrate in tissues was measured by myeloperoxidase (MPO) activity. Brain tissues were homogenized (50 mg/mL) in 0.5% hexadecyltrimethylammonium bromide and centrifuged at 15,000×g for 40 min. The suspension was then sonicated three times for 30 s. An aliquot of supernatant was mixed with a solution of 1.6 mM tetramethylbenzidine and 1 mM H2O2. Activity was measured spectrophotometrically as the change in absorbance at 650 nm at 37 °C. Data was expressed as milliunits/milligram protein [25].
Cytokine Measurements
The concentrations of tumor necrosis factor alpha (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) in brain structures were determined by a standard sandwich enzyme-linked immunosorbent assay (ELISA), with commercial available kits (R&D Systems, Minneapolis, MN). The results were expressed as picogram/milliliter.
Measurement of Nitrite/Nitrate Concentration
Nitrite/nitrate concentration was assayed spectrophotometrically using Griess reagents [1% sulfanilamide in 5% phosphoric acid and 0.1% N-1-naphthylethylenediamine dihydrochloride in bidistilled H2O (NED solution)] and vanadium(III) chloride as described previously [26]. A standard curve was run simultaneously with each set of samples and the optical density at 550 nm (OD550) was measured using ELISA microplate reader. Data was expressed as nanomole/milligram protein.
Oxidative Damage Parameters
The formation of thiobarbituric acid reactive species (TBARS) during an acid-heating reaction was verified as an index of oxidative damage on lipids, as previously described [27]. Briefly, the samples were mixed with 1 mL of 10% trichloroacetic acid and 1 mL of 0.67% thiobarbituric acid, and then heated in a boiling water bath for 15 min. TBARS was determined by the absorbance at 535 nm using 1,1,3,3-tetramethoxypropane as an external standard. Results were expressed as malondialdehyde equivalents nanomole/milligram protein.
The protein oxidation was assessed by the determination of carbonyl groups based on the reaction with dinitrophenylhidrazine, as previously described [28]. Briefly, proteins were precipitated by the addition of 20% trichloroacetic acid and dissolved in dinitrophenylhidrazine, and the absorbance was read at 370 nm. The results were expressed as protein carbonylation nanomole/milligram protein.
Antioxidant Enzymes Activity
Superoxide dismutase (SOD) (EC 1.15.1.1) activity was determined using a spectrophotometric assay based on superoxide-dependent oxidation of epinephrine to adrenochrome at 32 °C [29]. Absorption was measured at 480 nm. SOD specific activity was represented as milliunits/milligram protein.
Catalase (CAT) (EC 1.11.1.6) activity was assayed by measuring the absorbance decrease at 240 nm in a reaction medium containing 20 mM H2O2, 0.1% Triton X-100, 10 mM potassium phosphate buffer, pH 7.0, and the supernatants containing 0.1–0.3 mg protein mL−1 [30]. The specific activity was expressed as milliunits/milligram protein.
Mitochondrial Electron Transport Chain Enzymes Activity
After sample preparation, mitochondrial respiratory chain enzyme activities complex I was evaluated using the method previously described by measuring the NADH-dependent ferricyanide reduction rates at 420 nm [31]. The activity of complex III was measured by the decrease in absorbance of 2,6-dichloroindophenol. Reading was held in spectrophotometer at 600 nm for 5 min and the absorbance recorded every minute [32]. The complex IV activity was assayed according to the method described by [33], measured by examining the decrease in absorbance at 550 nm due to the oxidation of previously reduced cytochrome c. The activities of the mitochondrial respiratory chain complexes were expressed as nanomole/minute/milligram protein.
Protein Determination
All results are normalized with proteins were measured by the Lowry method [34].
Behavioral Analyses
Open-Field Task
The habituation to the open-field task evaluates motor performance in the training section and non-associative memory in the retention test session. Habituation to an open field was carried out in a 40 × 60 cm open field surrounded by 50-cm-high walls made of brown plywood with a frontal glass wall. The floor of the open field was divided into 12 equal rectangles by black lines. The animals were gently placed on the left rear quadrant and left to explore the arena for 5 min (training session). Immediately following this, the animals were taken back to their home cage and 24 h later submitted again to a similar open-field session (test session). Crossing of the black lines and rearing performed in both sessions were counted. The decrease in the number of crossings and rearings between the two sessions was taken as a measure of the retention of habituation [35].
Object Recognition Task
This task evaluates non-aversive and non-spatial memory. The apparatus and procedures for the object recognition task have been described elsewhere [36, 37]. Briefly, the task took place in a 40 × 50 cm open field surrounded by 50-cm-high walls made of plywood with a frontal glass wall. The floor of the open field was divided into nine equal rectangles by black lines. All animals were submitted to a habituation session where they were allowed to freely explore the open field for 5 min. No objects were placed in the box during the habituation trial. Crossings of the black lines and rearings performed in this session were evaluated as locomotors and exploratory activity, respectively. At different times after habituation, training was conducted by placing individual rats for 5 min in the field, in which two identical objects (objects A1 and A2, both being cubes) were positioned in two adjacent corners, 10 cm from the walls. In a short-term recognition memory test performed 1.5 h after training, the rats explored the open field for 5 min in the presence of one familiar (A) and one novel (B, a pyramid with a square-shaped base) object. All objects had similar textures (smooth), colors (blue), and sizes (weight 150–200 g), but distinctive shapes. A recognition index calculated for each animal is reported as the ratio TB/(TA + TB) (TA = time spent exploring the familiar object A; TB = time spent exploring the novel object B). Recognition memory was evaluated as done for the short-term memory test. Exploration was defined as sniffing (exploring the object 3–5 cm away from it) or touching the object with the nose and/or forepaws [38].
Data Analysis
Results were analyzed by Statistical Package for the Social Sciences software (SPSS, Chicago, IL, USA). Data are expressed as mean ± S.D. Differences among experimental groups were determined by two-way analysis of variance (ANOVA), followed by Tukey or Bonferroni post hoc test, respectively. Data from behavioral analysis were expressed as median and interquartile range, and comparisons among groups were performed using Mann-Whitney U tests, while the within-individual groups were analyzed by Wilcoxon test. The survival analysis was assessed by Kaplan-Meier and log rank test. In all comparisons, statistical significance was set at p < 0.05.
Results
Vit B6 Decreases Disrupted Tryptophan Metabolism
Figure 2 show levels of kynurenine, tryptophan, and the tryptophan/kynurenine ratio in the hippocampus and prefrontal cortex of rats submitted to severe polymicrobial sepsis and treated with vitamin B6.
Levels of kynurenine, tryptophan, and the tryptophan/kynurenine ratio in the hippocampus (a) and prefrontal cortex (b) of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Bonferroni. *p < 0.05, **p < 0.01, and ***p < 0.001
In the hippocampus, we observed that CLP + vit B6 animals presented a significant increase in TRP levels (~ 50%), compared to both CLP + saline and sham + saline animals. With regards to KYN levels, we did not detect statistically significant results among groups; however, we observed a tendency in CLP + vit B6 group in triplicating KYN levels, compared to CLP + saline group. Concerning the TRP/KYN ratio, although statistical analysis did not show significant differences, we can perceive that, since TRP levels increased ~ 50% and there was a threefold increase in KYN levels, the TRP/KYN of CLP + vit B6 group tended to decrease (Fig. 2a).
In the prefrontal cortex, we observed that kynurenine concentrations were significantly affected by sepsis and by vit B6 treatment, while tryptophan concentrations were only affected by sepsis and the TRP/KYN ratio was only interfered by vit B6 treatment. A paired-group comparison detected increased concentrations of tryptophan (~ 25%) and kynurenine (~ 65%) in CLP + vit B6 animals, in relation to CLP + saline rats. As a result, the TRP/KYN ratio did not vary among these groups. When we compared the CLP + vit B6 and sham + saline groups, we noted that vit B6 stimulated a threefold increase in the kynurenine concentrations, but also increased tryptophan concentrations (~ 60%), which explains the significant difference between the TRP/KYN ratios of these two groups (Fig. 2b).
Vit B6 Decreases BBB Permeability
Figure 3 shows BBB permeability measured by Evans blue dye extravasation. BBB permeability was increased in CLP + saline group in the prefrontal cortex and hippocampus, and treatment with vit B6 significantly reduced this alteration in both structures analyzed.
BBB permeability evaluation in the prefrontal cortex and hippocampus of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Tukey. *p < 0.05 compared to sham + saline group and #p < 0.05 compared to CLP + saline group
Vit B6 Attenuates Neuroinflammation in Sepsis
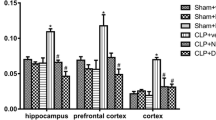
Treatment with vit B6 decreased neutrophil infiltration in the hippocampus (Fig. 4a) of septic rats, compared to CLP + saline. The levels of TNF-α (Fig. 4b) were increased in the prefrontal cortex and hippocampus of rats 24 h after sepsis induction, while vit B6 was effective in decreasing it in both structures. The levels of IL-1β (Fig. 4c) increased significantly only in the hippocampus of CLP + saline animals, and vit B6 treatment significantly reduced these levels. Sepsis elevated IL-6 levels (Fig. 4d) in the prefrontal cortex and hippocampus, compared to sham + saline rats, but vit B6 prevented this increase only in the hippocampus.
Myeloperoxidase activity (a) and levels of proinflammatory cytokines TNF-α (b), IL-1β (c), and IL-6 (d) in the prefrontal cortex and hippocampus of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Tukey. *p < 0.05 compared to sham + saline group and #p < 0.05 compared to CLP + saline group
Vit B6 Reduces Oxidative Stress and Changes in Brain Energy Metabolism after Sepsis
A significant increase in the nitrite/nitrate, an indicator of nitric oxide (NO) degradation, was visualized only in prefrontal cortex of animals submitted to sepsis (Fig. 5) and it was reversed by vit B6 treatment. Lipid peroxidation was enhanced in both brain structures (Fig. 6a), while higher levels of protein carbonylation (Fig. 6b) were found only in the hippocampus of CLP + saline animals, compared to sham + saline rats. Septic animals receiving vit B6, on the contrary, were prevented from lipid and protein oxidative damage caused by sepsis in these brain structures.
Nitrite/nitrate concentration in the prefrontal cortex and hippocampus of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Tukey. *p < 0.05 compared to sham + saline group and #p < 0.05 compared to CLP + saline group
Lipid peroxidation (a), protein carbonylation (b), SOD (c), and CAT (d) activities in the prefrontal cortex and hippocampus of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Tukey. *p < 0.05 compared to sham + saline group and #p < 0.05 compared to CLP + saline group
Panels c and d of Fig. 6, respectively, represent the enzymatic activities of SOD and CAT. Both enzymes had decreased activity only in the hippocampus of CLP + saline animals, compared to sham + saline rats. The administration of vit B6 was effective in preserving SOD activity in this brain structure, but did not positively affect CAT activity.
Regarding the activity of mitochondrial respiratory chain complex, a statistically significant increase was observed in the complex I activity (Fig. 7a) in the prefrontal cortex and hippocampus of CLP + saline rats. Vit B6 reduced complex I activity only in the prefrontal cortex. The activity of complex II-III (Fig. 7b) and IV (Fig. 7c) was not altered in any group.
Activity of complex I (a), complex II-III and complex IV (b) in the prefrontal cortex and hippocampus of rats subjected to polymicrobial sepsis and treated with vit B6 (600 mg/kg). Data are expressed as mean ± standard deviation, analyzed by two-way ANOVA with post hoc Tukey. *p < 0.05 compared to sham + saline group and #p < 0.05 compared to CLP + saline group
Vit B6 Treatment Does Not Improve Mortality after Sepsis
Figure 8 shows the survival analysis. Animals submitted to sham + saline and sham + vit B6 exhibited 100 and 93% survival rates, respectively, during the 10-day follow-up. Animals from CLP + saline group, on the other hand, presented a lower survival rate (31%), while 47% of CLP + vit B6 animals survived at 10 days after sepsis induction, but there was no statistically significant difference among both septic groups.
Vit B6 Treatment Improves Long-Term Cognitive Impairment in Sepsis Survivor Animals
Behavioral analyses demonstrate that CLP + saline animals presented deficits in motor performance and in non-associative memory, which can be observed in the crossing (Fig. 9a), rearing (Fig. 9b), and object recognition (Fig. 9c) measures, respectively. Conversely, the administration of vit B6 significantly improved learning and memory deficits in septic rats in both behavioral tests (Fig. 9a–c).
Number of crossings (a), rearings (b), and object recognition index (c) of rats subjected to polymicrobial sepsis and treated with vit B6 (60 0 mg/kg) 10 days after sepsis induction. Data presented as mean ± standard deviation, analyzed by paired t test and two-way ANOVA with post hoc Tukey for crossing and rearings. Data presented as mean and interquartile range, analyzed by Mann-Whitney U tests. Comparisons between groups in the recognition index objects were performed using Wilcoxon test. **p < 0.01 and *p < 0.05 compared to the training session
Discussion
In this study, we report the acute and long-term neuroprotective effects of vit B6 in a well-established model of experimental sepsis. The acute treatment with vit B6 improved parameters related to brain dysfunction in sepsis, such as neuroinflammation, oxidative stress, BBB permeability, mitochondrial dysfunction, and long-term cognitive impairment. Additionally, here we present the kynurenine pathway activation in brain structures of septic rats and its modulation by vit B6 treatment.
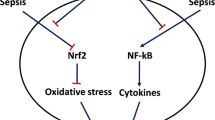
Our results suggest that, in CLP model, treatment with vit B6 led to a pronounced increase in hippocampal and cortical kynurenine concentrations and a more discrete increase in tryptophan concentrations. This accumulation of kynurenine, unaccompanied by the proportional increase in concentrations of its precursor, indicates the reduction of kynurenine metabolism in response to treatment with B6. Kynurenine can be converted to quinurenic acid by the enzyme kynurenine aminotransferase II (KAT-II); in anthranilic acid by the enzyme kynureninase (KYNU), or it can be hydroxylated by the enzyme kynurenine monooxygenase (KMO). Both the transformation of kynurenine by KYNU and KMO directs the route to its neurotoxic branch (3-hydroxyquinurenine, 3-hydroxyanthranilate, quinolinic acid). KAT-II and KYNU depend on B6 as a cofactor [39], while KMO appears to be inhibited by this vitamin [40]. Importantly, as vit B6 may regulate these key enzymes, vit B6 treatment in this study may have influenced two major steps to reduce brain damage after sepsis and regulate KYN pathways: (1) inhibition of KMO activity as an enzymatic antagonist; and (2) enhancement of KAT-II activity as a crucial enzymatic cofactor. Both actions may lead to increased KYN levels and its direction to generate nontoxic metabolites, as we observed positive results regarding cognitive functions in CLP + vit B6 animals.
It is well known that the systemic inflammatory response has a major effect on the development of SAE and long-term cognitive impairment [41, 42]. The metabolic fate of TRP, an essential amino acid, is to be converted into a variety of neuroactive substances, including the well-known neurotransmitters serotonin and melatonin. However, during inflammatory conditions, TRP is metabolized by the extrahepatic enzyme IDO to generate the toxic metabolite kynurenine [43, 44]. This is followed by the synthesis of neurotoxic molecules, such as anthranilic acid, xanthurenic acid, and quinolinic acid, among others, which act as N-methyl-D-aspartate receptor (NMDA) receptor agonists [40]. Sustained activation of NMDA receptors leads to excitotoxicity, a toxic event characterized by continual influx of calcium into the cell that activates the formation of reactive species, culminating in mitochondrial dysfunction.
In metabolomics analysis, KYN has been identified as a predictor of mortality in critically ill [10] and in trauma patients, acting as a clinical outcome indicator for sepsis. Also, increased plasma levels of KYN were associated with the occurrence of acute brain dysfunction in critically ill patients [45]
With regard to IDO activation, evidences suggest that, in addition to several inflammatory mediators, lipopolysaccharide (LPS) can activate IDO in the brain [46, 47], mainly by stimulation of microglial cells [48]. In patients with sepsis, an increase in the activity of plasmatic IDO is directly proportional to sepsis severity, but this scenario can also be observed in sepsis survivors [11]. Recently, a sepsis study using 1-methyl-L-tryptophan, an IDO inhibitor, showed preservation of TRP levels and a decreased conversion to KYN [49].
Additionally, low concentrations of plasma vit B6 are related to increased levels of proinflammatory cytokines [42], and vit B6 supplementation in patients with rheumatoid arthritis was effective in reducing the levels of these cytokines [43]. Immune components, like cytokines, can actively cross the BBB during systemic inflammation [50]. Experimental studies with sepsis models implicate cytokines and reactive species in the increase of BBB permeability and the subsequent edema [49, 51]. The mechanisms that lead to BBB dysfunction are not fully understood, but include the activation, by cytokines and reactive species, of proteases called matrix metalloproteinases (MMP) subtypes 2, 8, and 9, which degrade key proteins responsible to maintain the BBB functionality [51]. We previously demonstrated that sepsis causes an increased BBB permeability in 24 h after CLP surgery [52]. Another study with using CLP model showed rolling processes and neutrophil adhesion in brain microvasculature that were associated with greater cell damage [52]. Also, a study involving patients with systemic inflammation indicated that plasma vit B6 levels were inversely associated with the neutrophil counting in the systemic circulation [19]. Here we verified that vit B6 reduced neutrophil infiltration and, consequently, prevented the damage to BBB permeability in the prefrontal cortex and hippocampus 24 h after sepsis induction.
The increased BBB permeability after sepsis allows not only activated neutrophils but also other circulating molecules to easily permeate the brain, like LPS, cytokines, and reactive species. When glial cells recognize these molecules, the result is an activation of different intracellular pathways with a consequent proinflammatory response [53]. Thus, we found that animals subjected to sepsis had elevated TNF-α and IL-6 levels in the prefrontal cortex and hippocampus and IL-1β only in the hippocampus. Previous studies performed in mouse macrophage RAW264.7 cells indicate that vit B6 displays an important ability to block the effect of LPS in activating the transcription nuclear factor-kappa B (NF-κB) and the NLR family pyrin domain containing 3 (NLRP3) inflammasome, culminating in a suppression of IL-1β production and the inflammatory response [54, 55]. In this study, vit B6 administered immediately after sepsis induction was effective in reducing TNF-α levels in both structures and IL-6 and IL-1β in the hippocampus.
It is noteworthy that inflammatory infiltrate is dominated by neutrophils, which have a considerable capacity to generate ROS and RNS [56]. In this sense, NO, although it plays a physiological role when presented in low concentrations, if available in concentrations beyond a critical level, it becomes enormously cytotoxic. This cytotoxicity occurs mainly due to the reaction with superoxide anion, which in turn forms extremely toxic peroxynitrite, or it can cause cell injury by interacting with proteins, metals, iron-sulfur-containing or heme-containing compounds [57]. Peroxynitrite formation has been proposed as a terminal event contributing to cell death and tissue injury in human sepsis [58], especially in the brain [58,59,60,61,62].
We found that vit B6 reduced the levels of nitrite/nitrate, as a NO marker, in the prefrontal cortex and hippocampus after CLP surgery. A previous study demonstrated that vit B6 can suppress inducible nitric oxide synthase (iNOS) expression induced by LPS, i.e., reduced levels of vit B6 can increase the expression of iNOS, generating higher concentrations of NO [63].
Following nitrite/nitrate decrease, vit B6 prevented lipoperoxidation in both structures, while prevented oxidative damage to proteins in the hippocampus. Vit B6 exhibits an important antioxidant role [64] and its chemical structure is closely related to the ability of eliminating oxidants compounds [65]. Decreased levels of vit B6 are related to elevated lipid peroxidation in plasma [66]. In vitro, vit B6 prevented the formation of O2 · and lipid peroxidation [65], and in patients with Alzheimer’s disease vit B6 supplementation significantly decreased the levels of protein carbonyls [67]. In addition, vit B6 is a cofactor of KYN pathway, it promotes the balance between kynurenic acid, quinolinic acid, and xanthurenic acid [68]. Quinolinic acid and xanthurenic acid are metabolites with direct oxidizing ability and may act as agonists of NMDA receptors, leading to excitotoxic events through the formation of ROS and RNS. Kynurenic acid, on the other hand, acts as an antagonist of NMDA receptors, besides having antioxidant effects [69].
The vulnerability of brain to oxidative stress seems to occur not only because this organ utilizes about one fifth of the total oxygen demand of the body, but also due to a smaller pool of antioxidant enzymes, compared to other organs [58]. In the present study, we found that vit B6 prevented the decrease in SOD activity in hippocampus, contributing to the reduction of oxidative damage generated after sepsis. Higher levels of vit B6 are positively associated with SOD activity in surgical patients [15]. Thus, adequate levels of vit B6 proved to be an important factor to balance the concentration of pro- and antioxidant molecules.
On the other hand, vit B6 had no effect in CAT activity. Among different functions of vit B6, it has an intrinsic relationship with the synthesis of glutathione peroxidase (GPx); thereby, it is possible that this vitamin positively exerted some effect on the GPx availability, which may have contributed to the protective effect against oxidative stress [70, 71].
A major source of ROS production during sepsis is the interaction between the mitochondrial electron transport chain enzymes, leading to changes in cell energy production and enhancing oxidative stress [72]. Here it was identified a significant elevation in the complex I activity in septic animals, compared to control animals, and it was prevented by vit B6 in the prefrontal cortex. As vit B6 acts like a cofactor in the catabolism of amino acids during the urea cycle, it can increase the availability of precursors to generate ATP, thus regulating cellular energy metabolism [73]. In this research, vit B6 may have reduced the oxidative damage to proteins of mitochondrial respiratory chain by regulating the activity of complex I.
Despite the positive results related to vit B6 treatment on neuroinflammation and oxidative stress, this treatment was not associated with higher survivor rates. Gao and colleagues also did not observe an improvement in survival after administrating an IDO inhibitor [74], although they have shown enhancements in memory and cognition as a result of decreased levels of KYN and its metabolites.
Since the control of neuroinflammation did not influence mortality in our model, we aimed at investigating if vit B6 treatment could improve long-term brain dysfunction in sepsis survivors. Human studies show that sepsis leads to cognitive and structural damage in adults [75, 76] and causes cognitive impairment and poor school performance in children who recovered from SAE [77]. We had previously demonstrated that controlling acute neuroinflammation was associated with improved long-term outcome in the CLP model of sepsis [40, 44, 65,66,67]. Here we demonstrated that vit B6 also improves long-term cognitive dysfunction after sepsis recovery in rats.
Activation of KYN pathway can cause behavioral disorders, cognitive and memory impairment [78, 79]. In addition, KYN activation was found in the hippocampus and could explain neurocognitive alterations [80]. Furthermore, IDO activation can lead to decreased levels of serotonin, an important neurotransmitter involved in memory, and diminish the TRP availability [81].
After absorption, significative plasma levels of vit B6 can last up to 20 days [82], but knowing that inflammatory processes lead to vit B6 depletion, we cannot assume that animals presented a sufficient level of vit B6 in the systemic circulatory system to have any long-term effect at the time of behavioral tests. However, it was demonstrated that vit B6 exerts anti-inflammatory, antioxidant, and possibly a KYN pathway regulatory effect 24 h after sepsis induction. Thus, the long-term beneficial effects observed in this study may be due to the acute neuroprotection role exerted by vit B6. A recent study, using the same dose of vit B6 and behavioral tests, showed improved cognition and memory 10 days after meningitis induction [21]. Furthermore, vit B6 is a cofactor in the formation of serotonin pathway [83] and could improve memory and cognition. Importantly, the short-term neuroprotective effects of vit B6 in our study were measured in the prefrontal cortex and hippocampus, which are brain structures related to memory and cognition [38].
Conclusion
The administration of vitamin B6 was effective in preserving the BBB integrity and, consequently, decreasing neuroinflammation and oxidative stress, which resulted in long-term memory and cognition improvement. Thus, in our experimental model, vit B6 increased tryptophan and kynurenine levels in the prefrontal cortex and hippocampus and it may have contributed to protect these brain regions from the damage after sepsis.
References
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150. doi:10.1056/NEJMra021333
Ely EW (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA J Am Med Assoc 291:1753–1762. doi:10.1001/jama.291.14.1753
Lazosky A, Young GB, Ba SZ, Phillips R (2010) Quality of life after septic illness. J Crit Care 25:406–412. doi:10.1016/j.jcrc.2009.10.001
Zhang L, Wang X, Ai Y et al (2012) Epidemiological features and risk factors of sepsis-associated encephalopathy in intensive care unit patients: 2008–2011. Chin Med J 125:2008–2011. doi:10.3760/cma.j.issn.0366-6999.2012.05.018
Silvestre F, Danielski LG, Michels M et al (2014) Effects of organoselenium compounds on early and late brain biochemical alterations in sepsis-survivor rats. Neurotox Res 26:382–391. doi:10.1007/s12640-014-9475-y
Adam N, Kandelman S, Mantz J, et al (2013) Sepsis-induced brain dysfunction. Expert Rev Anti Infect Ther 11(2):211-221. doi:10.1586/eri.12.159.
Taccone FS, Su F, De Deyne C et al (2013) Sepsis is associated with altered cerebral microcirculation and tissue hypoxia in experimental peritonitis. Crit Care Med 42:1–9. doi:10.1097/CCM.0b013e3182a641b8
Lemstra AW, Groen in’t Woud JC, Hoozemans JJ, et al (2007) Microglia activation in sepsis: a case-control study. J Neuroinflammation 4:4. doi:10.1186/1742-2094-4-4
Comim CM, Rezin GT, Scaini G et al (2008) Mitochondrial respiratory chain and creatine kinase activities in rat brain after sepsis induced by cecal ligation and perforation. Mitochondrion 8:313–318. doi:10.1016/j.mito.2008.07.002
Rogers AJ, McGeachie M, Baron RM et al (2014) Metabolomic derangements are associated with mortality in critically ill adult patients. PLoS One 9:e87538. doi:10.1371/journal.pone.0087538
Tattevin P, Monnier D, Tribut O et al (2010) Enhanced Indoleamine 2, 3-dioxygenase activity in patients with severe sepsis and septic shock. J Infect Dis 201(6):956–966. doi:10.1086/650996
Maddison DC, Giorgini F (2015) The kynurenine pathway and neurodegenerative disease. Semin Cell Dev Biol. doi:10.1016/j.semcdb.2015.03.002
Campbell BM, Charych E, Lee AW, Möller T (2014) Kynurenines in CNS disease: regulation by inflammatory cytokines. Front Neurosci 8:12. doi:10.3389/fnins.2014.00012
Midttun O, Ulvik A, Ringdal Pedersen E et al (2011) Low plasma vitamin B-6 status affects metabolism through the kynurenine pathway in cardiovascular patients with systemic inflammation. J Nutr 141:611–617. doi:10.3945/jn.110.133082
Huang Y-C, Lan P-H, Cheng C-H et al (2002) Vitamin B6 intakes and status of mechanically ventilated critically ill patients in Taiwan. Eur J Clin Nutr 56:387–392. doi:10.1038/sj.ejcn.1601321
Huang Y-C, Chang H-H, Huang S-C et al (2005) Plasma pyridoxal 5′-phosphate is a significant indicator of immune responses in the mechanically ventilated critically ill. Nutrition 21:779–785. doi:10.1016/j.nut.2004.11.013
Hou C-T, Wu Y-H, Huang P-N et al (2011) Higher plasma pyridoxal 5′-phosphate is associated with better blood glucose responses in critically ill surgical patients with inadequate vitamin B-6 status. Clin Nutr 30:478–483. doi:10.1016/j.clnu.2011.01.014
Cheng CH, Huang SC, Chiang TY et al (2013) Higher plasma pyridoxal phosphate is associated with increased antioxidant enzyme activities in critically ill surgical patients. Biomed Res Int 2013:572081. doi:10.1155/2013/572081
Cheng CH, Chang SJ, Lee BJ et al (2006) Vitamin B 6 supplementation increases immune responses in critically ill patients. Eur J Clin Nutr 60(10):1207–1213. doi:10.1038/sj.ejcn.1602439
Fink MP, Heard SO (1990) Laboratory models of sepsis and septic shock. J Surg Res 49:186–196
Barichello T, Generoso JS, Simoes LR et al (2014) Vitamin B6 prevents cognitive impairment in experimental pneumococcal meningitis. Exp Biol Med (Maywood) 239(10):1360–1365
Paxinos G, Watson C (2013) The Rat brain in stereotaxic coordinates, 7th edn. Elsevier, Cambridge
Kwidzinski E, Bunse J, Aktas O et al (2005) Indolamine 2,3-dioxygenase is expressed in the CNS and down-regulates autoimmune inflammation. FASEB J 19:1347–1349. doi:10.1096/fj.04-3228fje
Uyama O, Okamura N, Yanase M et al (1988) Quantitative evaluation of vascular permeability in the gerbil brain after transient ischemia using Evans blue fluorescence. J Cereb Blood Flow Metab 8:282–284. doi:10.1038/jcbfm.1988.59
De Young LM, Kheifets JB, Ballaron SJ, Young JM (1989) Edema and cell infiltration in the phorbol ester-treated mouse ear are temporally separate and can be differentially modulated by pharmacologic agents. Agents Actions 26:335–341
Green LC, Wagner DA, Glogowski J, et al (1982) Analysis of nitrate, nitrite, and [15N] nitrate in biological fluids. Anal Biochem 126(1):131–138.
Draper HH, Hadley M (1990) Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol 186:421-431.
Levine RL, Williams JA, Stadtman ER, Shacter E (1994) Carbonyl assays for determination of oxidatively modified proteins. Methods Enzymol 233:346-357.
Bannister JV, Calabrese L (1987) Assays for superoxide dismutase. Methods Biochem Anal 32:279–312
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Cassina A, Radi R (1996) Differential inhibitory action of nitric oxide and peroxynitrite on mitochondrial electron transport. Arch Biochem Biophys 328:309–316. doi:10.1006/abbi.1996.0178
Fischer J, Ruitenbeek W, Ja B et al (1985) Differential investigation of the capacity of succinate oxidation in human skeletal muscle. Clin Chim Acta 153:23–36
Rustin P, Chretien D, Bourgeron T et al (1994) Biochemical and molecular investigations in respiratory chain. Clin Chim Acta 228:35–51
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
de Lima MNM, Laranja DC, Caldana F et al (2005) Reversal of age-related deficits in object recognition memory in rats with l-deprenyl. Exp Gerontol 40:506–511. doi:10.1016/j.exger.2005.03.004
Tuon L, Comim CM, Petronilho F et al (2008) Time-dependent behavioral recovery after sepsis in rats. Intensive Care Med 34:1724–1731. doi:10.1007/s00134-008-1129-1
Barichello T, Martins MR, Reinke A et al (2005) Cognitive impairment in sepsis survivors from cecal ligation and perforation. Crit Care Med 33:221–223. doi:10.1097/01.CCM.0000150741.12906.BD
Vianna MR, Izquierdo LA, Barros DM et al (2000) Short- and long-term memory: differential involvement of neurotransmitter systems and signal transduction cascades. An Acad Bras Cienc 72:353–364
Okada K, Angkawidjaja C, Koga Y, Kanaya S (2014) Structural and mechanistic insights into the kynurenine aminotransferase-mediated excretion of kynurenic acid. J Struct Biol 185:257–266. doi:10.1016/j.jsb.2014.01.009
Reyes Ocampo J, Lugo Huitrón R, González-esquivel D et al (2014) Kynurenines with neuroactive and redox properties: relevance to aging and brain diseases. Oxidative Med Cell Longev 2014:646909. doi:10.1155/2014/646909
Semmler A, Okulla T, Sastre M et al (2005) Systemic inflammation induces apoptosis with variable vulnerability of different brain regions. J Chem Neuroanat 30:144–157. doi:10.1016/j.jchemneu.2005.07.003
Sonneville R, Verdonk F, Rauturier C et al (2013) Understanding brain dysfunction in sepsis. Ann Intensive Care 3:1–11. doi:10.1186/2110-5820-3-15
Kanai M, Funakoshi H, Takahashi H et al (2009) Tryptophan 2,3-dioxygenase is a key modulator of physiological neurogenesis and anxiety-related behavior in mice. Mol Brain 2:8. doi:10.1186/1756-6606-2-8
Murakami Y, Saito K (2013) Species and cell types difference in tryptophan metabolism. Int J Tryptophan Res 6:47–54. doi:10.4137/IJTR.S11558
Changsirivathanathamrong D, Wang Y, Rajbhandari D et al (2011) Tryptophan metabolism to kynurenine is a potential novel contributor to hypotension in human sepsis. Crit Care Med 39:1. doi:10.1097/CCM.0b013e31822827f2
Corona AW, Norden DM, Skendelas JP et al (2013) Indoleamine 2,3-dioxygenase inhibition attenuates lipopolysaccharide induced persistent microglial activation and depressive-like complications in fractalkine receptor (CX3CR1)-deficient mice. Brain Behav Immun 31:134–142. doi:10.1016/j.bbi.2012.08.008
Lawson MA, Parrott JM, McCusker RH et al (2013) Intracerebroventricular administration of lipopolysaccharide induces indoleamine-2,3-dioxygenase-dependent depression-like behaviors. J Neuroinflammation 10:87. doi:10.1186/1742-2094-10-87
Wang Y, Lawson MA, Kelley KW, Dantzer R (2011) Primary murine microglia are resistant to nitric oxide inhibition of indoleamine 2, 3 dioxygenase. Brain Behav Immun 24:1249–1253. doi:10.1016/j.bbi.2010.04.015.Primary
Michels M, Danielski LG, Vieira A et al (2015) CD40–CD40 ligand pathway is a major component of acute neuroinflammation and contributes to long-term cognitive dysfunction after sepsis. Mol Med 21:219–226. doi:10.2119/molmed.2015.00070
Quan N, Banks W a. (2007) Brain-immune communication pathways. Brain Behav Immun 21:727–735. doi:10.1016/j.bbi.2007.05.005
Dal-Pizzol F, Rojas HA, Dos Santos EM et al (2013) Matrix metalloproteinase-2 and metalloproteinase-9 activities are associated with blood-brain barrier dysfunction in an animal model of severe sepsis. Mol Neurobiol 48:62–70. doi:10.1007/s12035-013-8433-7
Comim CM, Vilela MC, Constantino LS et al (2011) Traffic of leukocytes and cytokine up-regulation in the central nervous system in sepsis. Intensive Care Med 37:711–718. doi:10.1007/s00134-011-2151-2
Kacimi R, Giffard RG, Yenari MA (2011) Endotoxin-activated microglia injure brain derived endothelial cells via NF-κB, JAK-STAT and JNK stress kinase pathways. J Inflamm (Lond) 8:7. doi:10.1186/1476-9255-8-7
Yanaka N, Koyama T-A, Komatsu S-I et al (2005) Vitamin B6 suppresses NF-kappaB activation in LPS-stimulated mouse macrophages. Int J Mol Med 16:1071–1075
Zhang P, Tsuchiya K, Kinoshita T et al (2016) Vitamin B6 prevents IL-1β production by inhibiting NLRP3 inflammasome activation. J Biol Chem. doi:10.1074/jbc.M116.743815
Stamler JS (1994) Redox signaling: nitrosylation and related target interactions of nitric oxide. Cell 78:931–936. doi:10.1016/0092-8674(94)90269-0
Lobo SM, Soriano FG, Barbeiro DF et al (2009) Effects of dobutamine on gut mucosal nitric oxide production during endotoxic shock in rabbits. Med Sci Monit 15:BR37–BR42
Berg RMG, Møller K, Bailey DM (2011) Neuro-oxidative-nitrosative stress in sepsis. J Cereb Blood Flow Metab 31:1532–1544. doi:10.1038/jcbfm.2011.48
Santiago APSA, Chaves EA, Oliveira MF, Galina A (2008) Reactive oxygen species generation is modulated by mitochondrial kinases: correlation with mitochondrial antioxidant peroxidases in rat tissues. Biochimie 90:1566–1577. doi:10.1016/j.biochi.2008.06.013
Duma D, Fernandes D, Bonini MG et al (2011) NOS-1-derived NO is an essential triggering signal for the development of systemic inflammatory responses. Eur J Pharmacol 668:285–292. doi:10.1016/j.ejphar.2011.05.065
Fortin CF, McDonald PP, Fülöp T, Lesur O (2010) Sepsis, leukocytes, and nitric oxide (NO): an intricate affair. Shock 33:344–352. doi:10.1097/SHK.0b013e3181c0f068
Coleman N (2001) Antioxidants in critical care medicine. Environ Toxicol Pharmacol 10:183–188
Kanouchi H (2013) Low pyridoxine concentrations enhance lipopolysaccharide-stimulated gene expression of cyclooxygenase-2 and inducible nitric oxide synthase in RAW264.7 cells. J Nutr Sci Vitaminol 7:548–551
Matxain JM, Ristila M, Eriksson LA (2006) Theoretical study of the antioxidant properties of pyridoxine. J Phys Chem A. 110(48):13068–13072
Kannan K, Jain SK (2004) Effect of vitamin B6 on oxygen radicals, mitochondrial membrane potential, and lipid peroxidation in H2o2-treated U937 monocytes. Free Radic Biol Med 36:423–428. doi:10.1016/j.freeradbiomed.2003.09.012
Choi J, Koh S (2008) Role of brain inflammation in epileptogenesis. Yonsei Med J 49(1):1–18. doi:10.3349/ymj.2008.49.1.1
Rommer PS, Leblhuber F (2016) Lowered levels of carbonyl proteins after vitamin B supplementation in patients with mild cognitive impairment and Alzheimer’s disease. Neurodegener Dis 16(3-4):284–289. doi:10.1159/000441565
Stone TW, Darlington LG (2013) The kynurenine pathway as a therapeutic target in cognitive and neurodegenerative disorders. Br J Pharmacol 169:1211–1227. doi:10.1111/bph.12230
Lugo-huitrón R, Blanco-ayala T, Ugalde-muñiz P et al (2011) Neurotoxicology and teratology on the antioxidant properties of kynurenic acid: free radical scavenging activity and inhibition of oxidative stress. Neurotoxicol Teratol 33(5):538–547. doi:10.1016/j.ntt.2011.07.002
Bilski P, Li MY, Ehrenshaft M et al (2000) Symposium-in-print Vitamin B6 (pyridoxine) and its derivatives are efficient singlet oxygen quenchers and potential fungal antioxidants. Photochem Photobiol 71:129–134
Taş S, Sarandöl E, Dirican M (2014) Vitamin B6 supplementation improves oxidative stress and enhances serum paraoxonase/arylesterase activities in streptozotocin-induced diabetic rats. ScientificWorldJournal. doi:10.1155/2014/351598
Kowaltowski AJ, de Souza-pinto NC, Castilho RF, Vercesi AE (2009) Mitochondria and reactive oxygen species. Free Radic Biol Med 47:333–343. doi:10.1016/j.freeradbiomed.2009.05.004
Mooney S, Leuendorf J, Hendrickson C, Hellmann H (2009) Vitamin B6: a long known compound of surprising complexity. Molecules 14(1):329–351. doi:10.3390/molecules14010329
Gao R, Kan MQ, Wang SG et al (2015) Disrupted tryptophan metabolism induced cognitive impairment in a mouse model of sepsis-associated encephalopathy. Inflammation. doi:10.1007/s10753-015-0279-x
Götz ME, Künig G, Riederer P, Youdim MB (1994) Oxidative stress: free radical production in neural degeneration. Pharmacol Ther 63:37–122.
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. J Am Med Assoc 304:1787–1794. doi:10.1001/jama.2010.1553
Kaur J, Singhi P, Singhi S et al (2015) Neurodevelopmental and behavioral outcomes in children with sepsis-associated encephalopathy admitted to pediatric intensive care unit: a prospective case control study. J Child Neurol. doi:10.1177/0883073815610431
Chess AC, Simoni MK, Alling TE, Bucci DJ (2007) Elevations of endogenous kynurenic acid produce spatial working memory deficits. Schizophr Bull 33:797–804. doi:10.1093/schbul/sbl033
Heisler JM, Connor JCO (2015) Brain, behavior, and immunity metabolism mediates inflammation-induced deficit in recognition memory. Brain Behav Immun 2014:1–10. doi:10.1016/j.bbi.2015.06.022
Parrot J, Redus L, O’Connor JC (2016) Kynurenine metabolic balance is disrupted in the hippocampus following peripheral lipopolysaccharide challenge. J Neuroinflammation 13:124
Guo C, Wang P, Zhong M-L et al (2013) Deferoxamine inhibits iron induced hippocampal tau phosphorylation in the Alzheimer transgenic mouse brain. Neurochem Int 62:165–172. doi:10.1016/j.neuint.2012.12.005
Finglas PM (2000) Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin and choline. Trends Food Sci Technol. doi:10.1016/S0924-2244(01)00010-3
Shabbir F, Patel A, Mattison C et al (2013) Neurochemistry international effect of diet on serotonergic neurotransmission in depression. Neurochem Int 62:324–329. doi:10.1016/j.neuint.2012.12.014
Acknowledgements
This research was supported by grants from CNPq (FP). FP, TB, FD-P, and RSC are CNPq Research Fellows.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors or funding sources has conflict of interest.
Rights and permissions
About this article
Cite this article
Danielski, L.G., Giustina, A.D., Goldim, M.P. et al. Vitamin B6 Reduces Neurochemical and Long-Term Cognitive Alterations After Polymicrobial Sepsis: Involvement of the Kynurenine Pathway Modulation. Mol Neurobiol 55, 5255–5268 (2018). https://doi.org/10.1007/s12035-017-0706-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0706-0