Abstract
Alzheimer’s disease (AD) is characterized by the loss of synaptic contacts caused in part by cytoskeleton disruption. Adrenomedullin (AM) is involved in physiological functions such as vasodilation, hormone secretion, antimicrobial activity, cellular growth, and angiogenesis. In neurons, AM and related peptides are associated with some structural and functional cytoskeletal proteins, causing microtubule destabilization. Here, we describe the relationships between AM and other signs of AD in clinical specimens. Frontal cortex from AD patients and controls were studied for AM, acetylated tubulin, NCAM, Ox-42, and neurotransmitters. AM was increased in AD compared with controls, while levels of acetylated tubulin, NCAM, and neurotransmitters were decreased. Interestingly, increases in AM statistically correlated with the decrease in these markers. Furthermore, Ox42 overexpression in AD correlated with levels of AM. It is proposed that AD patients may have neural cytoskeleton failure associated with increase of AM levels, resulting in axon transport collapse and synaptic loss. These observations suggest that reducing AM expression may constitute a new avenue to prevent/treat AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is an irreversible degenerative pathology of the brain characterized by progressive deterioration of cognitive functions, affecting mainly neurons in the hippocampus and the cerebral cortex. Histological features of AD are senile plaques, made up of accumulations of β-amyloid (Aβ) peptide, and neurofibrillary tangles (NFT), which are fibrillar deposits of hyperphosphorylated Tau protein (P-Tau) [1].
There is overwhelming evidence that Aβ accumulation is central to the pathogenesis of AD. One of the consequences of Aβ accumulation is the hyperphosphorylation of a microtubule-associated protein (MAP) known as Tau. Pathological hyperphosphorylation of Tau leads to the destabilization of axonal cytoskeleton and loss of neural connections (synapses), chief markers of clinical manifestation which stem from the inability of Tau to regulate neural microtubule dynamics [2].
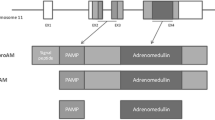
In the search for blood biomarkers of AD, some studies have found that mid-regional proadrenomedullin is elevated in AD patients and that the concentration of this protein could have prognostic value in the progression from predementia to clinical AD [3, 4]. The proadrenomedullin gene, ADM, codes for a 185 amino acid preprohormone which, after post-translational modifications, generates equimolar amounts of 2 biologically active peptides: prodrenomedullin N-terminal 20 peptide (PAMP) and adrenomedullin (AM). Both peptides are amidated at their carboxy terminus, and their their-dimensional structure is based on a central α-helix [5]. These peptides are ubiquitously expressed and perform several functions, including vasodilatation, bronchodilatation, angiogenesis, hormone secretion regulation, growth modulation, and antimicrobial activities, among others [6]. In the central nervous system (CNS), AM is expressed throughout the whole brain and spinal cord [7] and acts as neuromodulator partially through NMDA-dependent mechanisms [8].
An intriguing finding from our laboratory showed that both AM and PAMP decorate the microtubules in a variety of cell types, including neurons [9]. Yeast-2-hybrid analysis demonstrated that AM binds to several MAPs, whereas PAMP binds directly to tubulin and kinesin. Cell physiology studies point to a direct involvement of PAMP in regulating microtubule dynamics and kinesin speed [10]. Downregulation of ADM expression, through either gene knockdown or targeted knockout, results in a massive hyperpolymerization of the tubulin cytoskeleton, an increase on Glu- and acetylated-tubulin, a reduction of kinesin velocity, and the apparition of actin filopodia in CNS stem/progenitor cells [11]. In addition, AM immunoreactivity increases in the brain of mouse models of AD and seems to be associated with activated astrocytes in the vicinity of amyloid plaques [12].
Taking all these into consideration, the aim of the present work was to investigate the potential association of AM with the pathological mechanisms of AD in patient samples.
Materials and Methods
Human Brain Tissue
Brain tissues were obtained from the Oxford Project to Investigate Memory and Aging (OPTIMA, see www.medsci.ox.ac.uk/optima). Subjects for this study constituted a randomly selected subset of the participants, now part of the Thomas Willis Oxford Brain Collection within the Brains for Dementia Research Initiative (BDR). Informed consent was obtained from the patients’ next-of-kin before collection of brains, and the study was approved by the UK National Research Ethics Service. All subjects (n = 19, 7 were used for immunohistochemical studies, and 12 were used for western blotting studies) fulfilled Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) criteria for the neuropathological diagnosis of AD and were staged at Braak V/VI. Memory status in the AD group in the last pre-mortem examination indicated a mini-mental state examination (MMSE) score = 5.8 ± 0.8. Age-matched and sex-matched controls (n = 19, 7 were used for immunohistochemical studies, and 12 were used for western blotting studies) did not have dementia or other neurological diseases, did not meet CERAD criteria for AD diagnosis, and were staged at Braak 0-II. Frontal (Brodmann area [BA]10 or BA9) cortex were dissected free of meninges. To partially mitigate the possible effects of cause of death on neurochemical determinations, brain pH was measured in homogenates of frontal cortex in deionized water as an index of acidosis associated with terminal coma. Brain pH is used as an indication of tissue quality in post-mortem research, with pH > 6.1 considered acceptable [13]. All subsequent analyses were performed blind to clinical information. All biochemical studies (western blot, NCAM, and neurochemical measurements) were performed in the same tissues to allow correlation studies.
Immunohistochemistry
Formalin fixed, wax-embedded blocks (n = 7 in each group), cut into 7-μm sections and mounted onto slides, were used for immunohistochemistry. Briefly, the sections were dewaxed and rehydrated using Histoclear and alcohol dilutions. Antigen retrieval was carried out by microwaving the sections for 10 min in citrate buffer pH 6.0. Following blocking of endogenous peroxidases (0.3% H2O2 in PBS for 30 min), sections were incubated overnight with a polyclonal antibody specific for AM (rabbit polyclonal, 1:200, produced in house). This is a polyclonal antibody that has been previously used to characterize AM distribution in the brain [7, 12]. Development of the sections was performed using biotinylated anti-rabbit secondary antibody, ABC reagents, and a DAB kit (all Vector Laboratories, Peterborough, UK). Sections were dehydrated and mounted with DPX and coverslipped. For control experiments, the secondary biotinylated antibody was omitted. All tissues were processed, reacted, and developed at the same time. Images were captured on a Leica DMRB microscope equipped with DC420 digital camera.
Western Blotting
Samples (12 controls and 12 AD patients) were homogenized in RIPA buffer (Thermo Scientific) containing protease (EDTA-free complete, Roche, Basilea, Switzerland) and phosphatase (PhosStop, Roche) inhibitors. Homogenates were centrifuged for 30 min at 15,000×g and the supernatants collected. Protein concentration was determined by the BCA kit (Pierce, Rockford, IL), with bovine serum albumin as standard, using a spectrophotometer (POLARstar Omega, BMG Labtech, Ortenberg, Germany). Then, 25 μg of each sample was mixed with 4× sample buffer (Invitrogen) and heated for 10 min at 70 °C. Samples were run on 4–12% SDS–polyacrylamide gels. Seeblue plus 2 Prestained Standards (Invitrogen) were used as molecular weight markers. Proteins were transferred onto 0.2-μm nitrocellulose membranes (Amersham GE HealthCare). Membranes were incubated overnight at 4 °C with primary antibodies followed by peroxidase-labeled secondary antibodies. The primary antibodies used were AM antibody (rabbit polyclonal,1:200, produced in house, [7]), acetylated tubulin antibody (mouse monoclonal, 1:15,000, Sigma), and Ox-42 antibody (rabbit polyclonal, 1:500, Thermo Scientific). Immunoreactive bands were visualized using enhanced chemiluminescence and quantified by an image analyzer (Quantity One, Bio-Rad, Hercules, CA, USA). β-Actin (mouse monoclonal, 1:10000, Sigma-Aldrich) was used as an internal loading control. Results were calculated as the percentage of optical density values of normal controls.
Quantification of Total Levels of NCAM
To obtain crude synaptosomal pellets, frontal cortical tissue was homogenized in 10 volumes of ice-cold sucrose (0.32 M) and HEPES (5 mM) buffer that contained a cocktail of protease inhibitors (Complete TM, Boehringer Mannheim, UK) and centrifuged at 1000×g for 5 min. The supernatant was then centrifuged again at 15,000×g for 15 min, and the pellet resuspended in Krebs buffer. NCAM levels were quantified according to a previously described protocol [14]. Flat-bottom 96-well microplates were allowed to adsorb a coating solution (Na2CO3 0.1 M/ NaHCO3, 0.1 M) for 2 h at room temperature. The solution was removed and 50 μl of pellet samples added at a concentration of 10 mg/ml to each well of polystyrene flat-bottom ELISA plates. Plates were incubated overnight at 4 °C and then washed three times with 1 M phosphate-buffered saline (PBS) containing 0.05% Tween 20, pH 7.4. Additional binding sites were blocked with bovine serum albumin (BSA) (3%) for 2 h at room temperature. Wells were incubated with 50 μl aliquots of primary antibody Ab5032 (1:15,000 TBST; Chemicon) for 20–24 h at 4 °C, and subsequently, 50 μl aliquots of anti-rabbit IgG peroxidase conjugate antibody (1:500; Sigma, UK) were added for a 2-h incubation period. TMB (Promega) was used as a chromogenic substrate. The reaction was terminated by the addition of 1 N hydrochloric acid. Absorbances were measured at 450 nm using an automatic ELISA microplate reader. Results were expressed as absolute absorbance values.
Neurochemical Measurements
As previously described [14], concentrations of different neurotransmitters were determined by high performance liquid chromatography (HPLC) with electrochemical detection (Waters Spheribor® S10 0DS2 4,6 × 150 mm), including pre-column derivatization with o-phthaldehyde and β-mercapthoethanol for GABA and glutamate determinations. The limit of detection was 1 pg/10 μl for 5-HT and DA, 20 pg/10 μl for glutamate, and 50 pg/10 μl for GABA content.
Cholinergic activity was measured in terms of cholinacetyltransferase (ChAT) activity. This assay was performed as described [15]. Results were expressed as percentage of control values.
Statistical Analysis
Data were analyzed by SPSS for Windows, release 15.0. Normality was checked by Shapiro-Wilks’s test (p > 0.05). Student’s t test was used in comparisons between controls and AD samples. Correlation studies between biochemical variables were performed by Pearson’s or Spearman’s correlation coefficients, according to the normality of variables.
Results
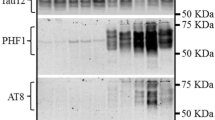
There were no significant differences in age, post-mortem delay, or brain pH between the control and AD groups. As shown in Fig. 1, the AM antibody stained several structures, including neurons, in cortical BA9 area in both AD and control human tissue. AM immunoreactivity was particularly prominent in pyramidal cells of cortical layers IV–V, where either nuclei and/or cytosolic compartments were immunostained. A detailed analysis revealed stronger AM labeling in apical dendrites and axons from AD pyramidal neurons (Fig. 1b) when compared to normal controls (Fig. 1a). Western blot experiments revealed two different bands of about 14 and 55 kDa using the AM antibody (Fig. 2). The 14-kDa band corresponds to the proAM protein which includes PAMP and AM moieties. The second band at around 55 kDa purportedly shows the association between ADM gene products and tubulin as previously described [9]. Significant increases of both AM bands were found in AD compared with controls (Fig. 2a).
Changes of AM expression in Alzheimer’s disease (AD) and normal control patients. Both AM (14 kDa) and AM associated to tubulin (AM-tub, 55 kDa) show significantly increased levels in AD. Panels show percentage of optical density (O.D.) values of control and representative pictures of the blotting. β-Actin is used as internal loading control. *p < 0.05, Student’s t test
Given the demonstrated relationship among AM, PAMP, and tubulin polymerization [9], we studied the expression of acetylated tubulin and found that it was significantly decreased in AD samples (Fig. 3a). These data suggest that the higher levels of AM and/or PAMP could be associated with cytoskeleton destabilization in AD. Supporting this idea, there was a strong trend when correlating products of ADM gene (55 kDa) and acetylated tubulin expression (r = −0.540; p = 0.07, Pearson’s correlation coefficient). The expression of another synaptic plasticity protein, the neural cell adhesion molecule (NCAM), was significantly lower in AD frontal cortex compared to controls (Student’s t test; p < 0.05, Fig. 3b). Decreases in NCAM expression were significantly correlated to increases in AM (14 kDa) levels (r = −0.641; p < 0.05, Pearson’s correlation coefficient).
Decreased levels of acetylated tubulin (Ac-tub, a) and NCAM (b) were found in the frontal cortex (BA10) of Alzheimer’s disease (AD) patients. a Shows percentage of optical density (O.D.) values of control and representative pictures of the blotting. β-Actin is used as internal loading control. NCAM levels are expressed as absolute absorbance value. *p < 0.05, Student’s t-test
The expression of Ox-42, a microglia activation marker, was significantly enhanced in AD over controls (Student’s t test; p < 0.05, Fig. 4). AM (14 kDa) and Ox-42 expression were significantly and positively intercorrelated in AD (r = 0.702; p < 0.05, Pearson’s correlation coefficient). Levels of different neurotransmitters were also measured in cortical samples of AD patients and controls. Significant decreases in ChAT activity and 5-HT, DA, and GABA levels were observed in AD patients (Student’s t test; p < 0.01, Table 1). A significant correlation between the reduced levels of neurotransmitters and increased levels of AM (14 kDa) was found for GABA (r = −0.709; p < 0.05, Spearman’s correlation coefficient) glutamate (r = −0.718; p < 0.05, Spearman’s correlation coefficient).
Increased expression of Ox-42, as marker of activated microglia, in the frontal (BA10) cortex of Alzheimer’s disease (AD) patients. Panel shows percentage of optical density (O.D.) values of control and representative pictures of the blotting. β-Actin is used as internal loading control *p < 0.05, Student’s t test
Discussion
In this study, we have shown that human brains from AD patients have a higher expression of AM than age-matched normal controls. This increased AM correlated with lower levels of acetylated tubulin, NCAM, and neurotransmitters and a higher level of activated microglia.
Previous reports have indicated that mid-regional proadrenomedullin levels may constitute an early prognostic marker of AD [3, 4]. This intermediate peptide does not have a known function but is used as a surrogate of AM expression since it has a longer half-life than the mature peptide [16]. Currently, our study seems to be the first report on the increased expression of mature AM in the brain of AD patients, although a similar observation was made in mouse models of AD [12]. The specific localization of AM-immunoreactivity in the soma and apical dendrites of cortical neurons coincides with original observations in rat brains [7]. Electron microscopy [7] and immunofluorescence [9] studies have shown that intracellular AM is associated to the neuronal microtubules. The fact that the increase on AM immunoreactivity correlates with a reduction in acetylated tubulin levels suggests a role for the proadrenomedullin-derived peptides in neuronal cytoskeleton maintenance. In the case of microtubule dynamics, the contribution of PAMP is likely to exert a more specific contribution to microtubule dynamics than AM, since previous studies have shown the profound impact of PAMP on microtubule fluidity [9].
Tubulin acetylation is a post-translational modification of α-tubulin that sustains microtubule stability [17]. The reduced levels of acetylated tubulin levels in AD patients when compared to non-demented controls suggest the presence of less rigid microtubules in these patients, which might contribute and precipitate synaptic disconnections. We had to consider that our AD patients had a MMSE score of 5.8 ± 0.8, which is considered a telltale for severe cognitive impairment [18]. Other α-tubulin modifications have been also reported to increase in neurodegenerative diseases, including AD [19].
NCAM is part of a family of cell-surface glycoproteins that plays key roles in normal brain development, including axonal/dendritic growth and branching, and synaptic plasticity [20,21,22,23]. NCAMs have been implicated as critical components in the induction of long-term potentiation (LTP) and in memory formation [20, 21]. NCAMs have been shown to play critical roles in ontogenetic development and are thus surrogate markers of age-related pathology, particularly in AD [24, 25].
Synaptic loss is the major neurobiological substrate of cognitive dysfunction in AD. Synaptic failure is an early disease event that can be already detectable in patients with mild cognitive impairment, a prodromal state of AD (reviewed by [26]). This pathological feature progresses during the course of AD though in most early stages involves mechanisms of compensation (synaptic remodeling or synaptogenesis) before reaching a stage of decompensated function (degeneration) [27, 28].
There are previously published studies that have reported either no changes [29] or increased [27, 30] levels of NCAM in the hippocampus of AD patients. The latter observations have been related to enhanced neurogenesis and may be indicative of adaptive brain mechanisms to compensate for the structural and functional damage caused by the disease. Soluble forms of NCAM are increased in the cerebrospinal fluid of both AD and Parkinson disease patients, but these increases seem to be related to aging and neurodegeneration and not to dementia as such [31]. In the serum samples, only levels of low molecular weight forms of NCAM correlated to severity of dementia [32]. In agreement with our observations, decreased levels of NCAM have been found in the frontal cortex of AD patients [33], which might stem from the synaptic loss associated to the course of disease.
The correlation between Ox-42 and AM expression suggests that increased AM expression is somewhat related to the activation of microglia, the resident immune cells of CNS, therefore indicating that increases in brain AM expression could be contributing to cerebral amyloid-associated inflammation in AD. Inflammatory responses in the brain, which can be measured by changes in markers for microglia activation, such as Ox-42, are a common feature of human neurodegenerative diseases. A crucial role has been described for neuroinflammation in AD pathogenesis, and emerging evidence suggests that neuroinflammation could be both a cause and a consequence of AD [34].
Neuron and synapse loss, together with neurotransmitter dysfunction, Aβ deposition, and neurofibrillary tangles, are recognized hallmarks of AD [35]. Furthermore, clinical and preclinical studies point to neuronal loss and associated neurochemical alterations of several transmitter systems as a main factor underlying both cognitive and neuropsychiatric symptoms [36]. The neurodegenerative process, as indicated by neurofibrillary tangle pathology, proceeds from the hippocampus and entorhinal cortex to involve increasingly the glutamatergic neurons of the cortical association areas in a topographical progression [37]. Other studies have reported dysfunction in the major cortical inhibitory GABAergic system in AD which may in part be dependent on disease severity and behavioral symptoms of dementia, such as depression [38].
Clinicopathological correlation studies have been crucial to generate hypotheses about the pathophysiology of the disease and potential targets of intervention. From our present observations in AD postmortem tissue, it might be inferred that therapeutical approaches aimed at reducing AM/PAMP levels may constitute a novel path to prevent/delay AD neurodegeneration. A few years ago, a particular single nucleotide polymorphism (SNP) in the proximity of the ADM gene was found to be associated with reduced circulating levels of AM [39] and lower risk of developing cancer [40]. Therefore, it would be interesting to perform follow-up studies on these carriers in order to evaluate whether this particular haplotype prevents from susceptibility of predeveloping AD. In addition, several physiological inhibitors of AM have been proposed for clinical development, including a monoclonal antibody [41], the peptide fragment AM22–52 [42], and a number of small molecules that target either AM or PAMP [43, 44]. Therefore, some of these inhibitors might be developed for the pharmacological prevention of AD in individuals at high risk [45] or in patients suffering moderate AD in high risk of rapid cognitive decline [46].
Overall, increased AM levels are found in brains of AD patients correlating negatively with markers of cytoskeleton stability and cell-to-cell interactions. Therefore, ADM gene products might represent novel pathological features contributing to perturbations of neuronal maintenance and synaptic function in AD, and their pharmacological inhibition may constitute a novel approach to the treatment of AD.
References
Hernandez F, Lucas JJ, Avila J (2013) GSK3 and tau: two convergence points in Alzheimer’s disease. J Alzheimers Dis 33(Suppl 1):S141–S144
Querfurth HW, LaFerla FM (2010) Alzheimer’s disease. N Engl J Med 362:329–344
Buerger K, Uspenskaya O, Hartmann O et al (2011) Prediction of Alzheimer’s disease using midregional proadrenomedullin and midregional proatrial natriuretic peptide: a retrospective analysis of 134 patients with mild cognitive impairment. J Clin Psychiatry 72:556–563
Henriksen K, O’Bryant SE, Hampel H et al (2014) The future of blood-based biomarkers for Alzheimer’s disease. Alzheimers Dement 10:115–131
Pérez-Castells J, Martín-Santamaría S, Nieto L et al (2012) Structure of micelle-bound adrenomedullin: a first step toward the analysis of its interactions with receptors and small molecules. Biopolymers 97:45–53
López J, Martínez A (2002) Cell and molecular biology of the multifunctional peptide, adrenomedullin. Int Rev Cytol 221:1–92
Serrano J, Uttenthal LO, Martínez A et al (2000) Distribution of adrenomedullin-like immunoreactivity in the rat central nervous system by light and electron microscopy. Brain Res 853:245–268
Xu Y, Krukoff TL (2004) Adrenomedullin in the rostral ventrolateral medulla increases arterial pressure and heart rate: roles of glutamate and nitric oxide. Am J Physiol Regul Integr Comp Physiol 287:R729–R734
Sackett DL, Ozbun L, Zudaire E et al (2008) Intracellular proadrenomedullin-derived peptides decorate the microtubules and contribute to cytoskeleton function. Endocrinology 149:2888–2898
Larráyoz IM, Martínez A (2012) Proadrenomedullin N-terminal 20 peptide increases kinesin’s velocity both in vitro and in vivo. Endocrinology 153:1734–1742
Vergaño-Vera E, Fernández AP, Hurtado-Chong A et al (2010) Lack of adrenomedullin affects growth and differentiation of adult neural stem/progenitor cells. Cell Tissue Res 340:1–11
Fernandez AP, Masa JS, Guedan MA et al (2016) Adrenomedullin expression in Alzheimer’s brain. Curr Alzheimer Res 13:428–438
Kirvell SL, Esiri M, Francis PT (2006) Down-regulation of vesicular glutamate transporters precedes cell loss and pathology in Alzheimer’s disease. J Neurochem 98:939–950
Aisa B, Gil-Bea FJ, Solas M et al (2010) Altered NCAM expression associated with the cholinergic system in Alzheimer’s disease. J Alzheimers Dis 20:659–668
Garcia-Alloza M, Gil-Bea FJ, Diez-Ariza M et al (2005) Cholinergic-serotonergic imbalance contributes to cognitive and behavioral symptoms in Alzheimer’s disease. Neuropsychologia 43:442–449
Morgenthaler NG, Struck J, Alonso C, Bergmann A (2005) Measurement of midregional proadrenomedullin in plasma with an immunoluminometric assay. Clin Chem 51:1823–1829
Strzyz P (2016) Post-translational modifications: extension of the tubulin code. Nat Rev Mol Cell Biol 17:609
Mungas D (1991) In-office mental status testing: a practical guide. Geriatrics 46:54–58 63, 66
Vu HT, Akatsu H, Hashizume Y et al (2017) Increase in α-tubulin modifications in the neuronal processes of hippocampal neurons in both kainic acid-induced epileptic seizure and Alzheimer’s disease. Sci Rep 7:40205
Rønn LC, Berezin V, Bock E The neural cell adhesion molecule in synaptic plasticity and ageing. Int J Dev Neurosci 18:193–199
Kiss JZ, Muller D (2001) Contribution of the neural cell adhesion molecule to neuronal and synaptic plasticity. Rev Neurosci 12:297–310
Walmod PS, Kolkova K, Berezin V, Bock E (2004) Zippers make signals: NCAM-mediated molecular interactions and signal transduction. Neurochem Res 29:2015–2035
Kleene R, Schachner M (2004) Glycans and neural cell interactions. Nat Rev Neurosci 5:195–208
Montag-Sallaz M, Schachner M, Montag D (2002) Misguided axonal projections, neural cell adhesion molecule 180 mRNA upregulation, and altered behavior in mice deficient for the close homolog of L1. Mol Cell Biol 22:7967–7981
Aisa B, Elizalde N, Tordera R et al (2009) Effects of neonatal stress on markers of synaptic plasticity in the hippocampus: implications for spatial memory. Hippocampus 19:1222–1231
Arendt T (2009) Synaptic degeneration in Alzheimer’s disease. Acta Neuropathol 118:167–179
Mikkonen M, Soininen H, Tapiola T et al (1999) Hippocampal plasticity in Alzheimer’s disease: changes in highly polysialylated NCAM immunoreactivity in the hippocampal formation. Eur J Neurosci 11:1754–1764
Mikkonen M, Soininen H, Alafuzof I, Miettinen R (2001) Hippocampal plasticity in Alzheimer’s disease. Rev Neurosci 12:311–325
Gillian AM, Brion JP, Breen KC (1994) Expression of the neural cell adhesion molecule (NCAM) in Alzheimer’s disease. Neurodegeneration 3:283–291
Jin K, Peel AL, Mao XO et al (2004) Increased hippocampal neurogenesis in Alzheimer’s disease. Proc Natl Acad Sci 101:343–347
Strekalova H, Buhmann C, Kleene R et al (2006) Elevated levels of neural recognition molecule L1 in the cerebrospinal fluid of patients with Alzheimer disease and other dementia syndromes. Neurobiol Aging 27:1–9
Todaro L, Puricelli L, Gioseffi H et al (2004) Neural cell adhesion molecule in human serum. Increased levels in dementia of the Alzheimer type. Neurobiol Dis 15:387–393
Yew DT, Li WP, Webb SE et al (1999) Neurotransmitters, peptides, and neural cell adhesion molecules in the cortices of normal elderly humans and Alzheimer patients: a comparison. Exp Gerontol 34:117–133
Calsolaro V, Edison P (2016) Neuroinflammation in Alzheimer’s disease: Current evidence and future directions. Alzheimers Dement 12:719–732
Francis PT (2003) Glutamatergic systems in Alzheimer’s disease. Int J Geriatr Psychiatry 18:S15–S21
Francis PT, Ramírez MJ, Lai MK (2010) Neurochemical basis for symptomatic treatment of Alzheimer’s disease. Neuropharmacology 59:221–229
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259
Garcia-Alloza M, Tsang SW, Gil-Bea FJ et al (2006) Involvement of the GABAergic system in depressive symptoms of Alzheimer’s disease. Neurobiol Aging 27:1110–1117
Cheung BMY, Ong KL, Tso AWK et al (2011) Plasma adrenomedullin level is related to a single nucleotide polymorphism in the adrenomedullin gene. Eur J Endocrinol 165:571–577
Martínez-Herrero S, Martínez A (2013) Cancer protection elicited by a single nucleotide polymorphism close to the adrenomedullin gene. J Clin Endocrinol Metab 98:E807–E810
Martínez A, Weaver C, López J et al (1996) Regulation of insulin secretion and blood glucose metabolism by adrenomedullin. Endocrinology 137:2626–2632
Ishikawa T, Chen J, Wang J et al (2003) Adrenomedullin antagonist suppresses in vivo growth of human pancreatic cancer cells in SCID mice by suppressing angiogenesis. Oncogene 22:1238–1242
Martínez A, Julián M, Bregonzio C et al (2004) Identification of vasoactive nonpeptidic positive and negative modulators of adrenomedullin using a neutralizing antibody-based screening strategy. Endocrinology 145:3858–3865
Roldós V, Carbajo RJ, Schott A-K et al (2012) Identification of first proadrenomedullin N-terminal 20 peptide (PAMP) modulator by means of virtual screening and NMR interaction experiments. Eur J Med Chem 55:262–272
Hickman RA, Faustin A, Wisniewski T (2016) Alzheimer disease and its growing epidemic: risk factors, biomarkers, and the urgent need for therapeutics. Neurol Clin 34:941–953
Barbe C, Morrone I, Novella JL et al (2016) Predictive factors of rapid cognitive decline in patients with Alzheimer disease. Dement Geriatr Cogn Dis Extra 6:549–558
Acknowledgements
H.F. is a recipient of a fellowship from Ministerio de Educación y Ciencia (FPU). I.M.L. and A.M. are funded by Fundación Rioja Salud (FRS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ferrero, H., Larrayoz, I.M., Martisova, E. et al. Increased Levels of Brain Adrenomedullin in the Neuropathology of Alzheimer’s Disease. Mol Neurobiol 55, 5177–5183 (2018). https://doi.org/10.1007/s12035-017-0700-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0700-6