Abstract
Tau is a microtubule-associated protein highly expressed in neurons with a chief role in microtubule dynamics and axonal maintenance. Adrenomedullin gene (ADM) codifies for various peptides that exert broad range of actions in the body. Previous works in our groups have shown that increased ADM products are positively correlated to microtubule disruption and tau pathology in Alzheimer’s disease brains. In the present study, we explore the involvement of ADM in the neuropathology of frontotemporal lobar degeneration that presents with primary tauopathy (FTLD-tau). Proteins from frontal cortices of FTLD-tau patients and age- and sex-matched non-demented controls were analyzed with antibodies against different microtubule components, including adrenomedullin, and synaptic markers. Tau pathology in frontal cortex from FTLD patients was confirmed. Levels of total βIII-tubulin as well as acetylated and detyrosinated tubulins, two markers of stabilized and aged microtubules, were significantly reduced and directly correlated with PSD95 and proBDNF in FTLD-tau patients when compared to non-demented controls. In contrast, no change in actin cytoskeleton was found. Interestingly, changes in microtubule elements, indicators of disturbed axonal preservation, were accompanied by decreased levels of free adrenomedullin, although no association was found. Altogether, reduced levels of adrenomedullin might not be directly linked to the microtubule pathology of FTLD-tau, but based on previous works, it is suggested that downregulation of ADM might be an adaptive attempt of neurons to mitigate microtubule disruption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Frontotemporal lobar degeneration (FTLD) is a pathological condition that predominantly presents with frontotemporal dementia (FTD) and results from the selective and progressive deterioration of the frontal and temporal lobes of the brain. Depending on the affected regions, patients with FTLD can display progressive changes in behavior, executive dysfunction, and/or language abnormalities, giving rise to distinct clinical symptoms: behavioral variant of frontotemporal dementia (bvFTD), semantic variant primary progressive aphasia (svPPA), and progressive non-fluent aphasia (PNFA). The neuropathology of FTLD is also heterogeneous, and hence, FTLD has been classified into broad categories according to the type of intracellular protein deposits: tau, transactive response DNA-binding protein 43 (TDP-43), or fused in sarcoma (FUS), being each of them either positive or negative for ubiquitin protein [1].
Primary tauopathies are defined by the presence of insoluble and hyperphosphorylated tau proteins in neurons and glial cells. These disorders fall into the clinical spectrum of FTLD (hereinafter referred as pathological subtype FTLD-tau), predominantly presenting with bvFTD, svPPA, and PNFA but also with atypical parkinsonism syndromes such as progressive supranuclear palsy and corticobasal degeneration [2, 3]. The rest of FTLD cases can be assigned to one of the two other major pathological subtypes: FTLD-FUS and FTLD-TDP [4]. FTLD is highly linked to family history of neurodegenerative disease (around 40% of cases). Mutations in microtubule-associated protein tau (MAPT) gene are frequent in patients with FTLD-tau and cause a subtype of frontotemporal dementia with parkinsonism linked to chromosome 17-tau (FTDP-17T) [5]. Tau is a microtubule-associated protein with a chief role in microtubule stabilization by promoting their polymerization and suppressing their dynamics when assembled. Phosphorylation of tau is important for microtubule dynamics in physiological conditions. However, when tau is abnormally hyperphosphorylated in response to a number of stressors or mutations, tau dissociates from the microtubule cytoskeleton, leading to its instability and causing axonal degeneration [6]. Unbound hyperphosphorylated tau is prone to aggregate and assemble into intracellular fibrillar deposits. In contrast to Alzheimer’s disease (AD), where tau deposits are made up of all isoforms, FTLD-tau fibrils are heterogeneous but usually enriched in one of the six tau isoforms, which actually helps defining neuropathological sub-divisions [7, 8]. However, all these pathological phenotypes share a common feature: abnormal hyperphosphorylation of tau is primary and central to the disease by leading to microtubule disruption and axonal degeneration.
Microtubules are composed of globular tubulin proteins. Post-translational modifications (e.g., acetylation, detyrosination) of tubulins and their binding to other cellular proteins orchestrate the dynamics of microtubule polymerization and depolymerization, which are necessary for proper axonal and dendrite organization in neurons. Previous studies identified novel microtubule interactors with prominent role in tubulin dynamics [9]. In particular, two adrenomedullin (ADM) gene products, proadrenomedullin N-terminal peptide (PAMP) and adrenomedullin (AM), can bind directly to tubulin and kinesin and other microtubule-associated proteins, and participate in specific functions such as destabilization of microtubule polymerization and increased transport velocity through microtubules [9, 10]. Further, increased ADM immunoreactivities were found in apical dendrites and axons in brains from AD patients and mouse models [11, 12], and the fraction of ADM peptides bound to tubulin was reported to be increased in aged and AD brains [11, 13]. It is interesting to note that conditional deletion of ADM is able to revert aged-related memory impairment and abnormal tau phosphorylation in rodent brains [13]. Taking all these data into account, we decided to explore the status of ADM products and its relationship to microtubule dismantlement in a neurodegenerative condition where tauopathy is a primary pathological event, such as FTLD-tau.
To this purpose, brain tissues from FTLD patients were obtained from the Brains for Dementia Research Initiative (BDR, UK). Informed consent was obtained from the patients’ next of kin before collection of brains, and the study was approved by the UK National Research Ethics Service. Demented subjects (n = 10) fulfilled criteria for the clinical diagnosis of FTLD and pathological classification of FTLD-tau according to recent classification [14]. Controls (n = 10) matched for age (62.5 ± 2.2 vs 61.9 ± 3.3, controls and FTLD respectively), sex (5 males/5 females vs 6 males/4 females), and post-mortem delay (34.1 ± 4.9 vs 31.0 ± 4.3 h) did not have dementia or any other neurological diseases and were staged at Braak 0–II. Small frozen and meninge-free pieces of frontal cortices from Brodmann area (BA)10 were used for subsequent analysis, which were performed blind to clinical information. Brain pH measurements were determined for each frontal cortex in deionized water as an index of acidosis associated with terminal coma, and cases were subsequently excluded if the pH was found to be below 6.1. Proteins from BA10 homogenates were isolated in RIPA buffer, resolved by SDS-glycine gel electrophoresis (as described in [11]) and subsequently immunoblotted with different antibodies against cytoskeletal components, including adrenomedullin, and synaptic markers (Table 1).
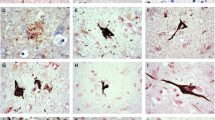
As shown in Fig. 1, the antibody Tau12 showed no particular changes in the amount of total tau in BA10 frontal cortex between FTLD-tau patients and control individuals, but the antibody PHF1 that is specific for pSer-396/pSer-404 detected variable but marked pattern of tau phosphorylation in FTLD-tau brains. In contrast, the antibody AT8, which recognizes pSer-202/pThr-205, showed relative increases of tau phosphorylation in most of the cases. These observations confirm the expected tau pathology in the frontal cortex of FTLD-tau brains, although the explanations for the intra-patient variability and the distinct intensities of tau phosphorylation between antibodies are unclear. Perhaps regional differences may account for the distinct intensity signals given by AT8 and PHF1 antibodies, since the former preferentially recognizes the white matter pathology while the latter has preference for gray matter pathology of AD [15].
Representative western blot images showing tau pathology in BA10 frontal cortex of FTLD-tau patients and matched non-demented controls. Antibody Tau12 does not detect significant changes in total levels of tau protein in FTLD-tau frontal cortices. Antibody PHF1 that recognizes Ser-396/Ser-404 shows a more prominent pattern of tau phosphorylation than antibody AT8 that is specific for Ser-202/Thr-205. N = 10 (controls), n = 10 (FTLD-tau). β-actin is used as internal loading control
Neuron-specific βIII-tubulin was significantly reduced in FTLD-tau when compared to controls (Student’s t test; t(18) = 2.12, P = 0.024; Fig. 2). Post-translational modifications of tubulin, in particular, acetylated tubulin and detyrosinated tubulin (glu-tub), both of which associated with microtubule stabilization, were also significantly decreased in FTLD-tau brains (t(18) = 1.95, P = 0.034; t(18) = 1.91, P = 0.036, respectively; Fig. 2). However, actin cytoskeleton remained unchanged, as shown by similar levels of β-actin between controls and FTLD-tau groups (t(18) = − 0.23, P = 0.41; Fig. 2). Such decreases in microtubule components undoubtedly represent a disassembly of microtubule cytoskeleton in FTLD-tau pathology and confirm the known effects of tauopathy on microtubule stability and axonal degeneration [6]. Marked decreases of βIII-tubulin and other elements of the neurocytoskeleton, such as neurofilament proteins, but no changes in microfilament β-actin protein have been already reported in the frontal cortex of Pick disease patients [16], a dementia syndrome that belongs to the subtype FTLD-tau. Notwithstanding, reduced levels of acetylated and detyrosinated tubulins in brains of FTLD-tau patients have not been reported before to our knowledge, but support previous studies reporting decreases of tubulin acetylation and detyrosination in neurofibrillary tangle-bearing neurons of AD brains and in tau-depleted neurons [17,18,19]. PSD95 and proBDNF proteins, both of which are important for synaptic function and predominantly recruited at post-synaptic sites, were found significantly decreased in FTLD-tau (t(18) = 3.89, P = 0.001 for PSD95; t(18) = 2.99, P = 0.008 for proBDNF; Fig. 3), representing the expected disruption of post-synaptic density that takes place in neurodegenerative dementias [20]. Loss of synapses may account for the observed reductions of microtubule immunoreactivities; hence, stronger synaptic disruption should be accompanied by lower levels of tubulins. However, PSD95 was not correlated with either βIII-tubulin (Spearman’s rho = 0.301, P = 0.39, n = 10), acetylated tubulin (Spearman’s rho = 0.539, P = 0.11, n = 10), or detyrosinated tubulin (Spearman’s rho = 0.03, P = 0.93, n = 10) in FTLD-tau brains. This data suggest that loss of microtubule components might not be related to synaptic loss. Instead, this and the lack of changes in other cytoskeletal proteins suggest the specific vulnerability of microtubule cytoskeleton to tau pathology [8, 21].
Changes of various microtubule elements in frontotemporal lobar degeneration with primary tauopathy (FTLD-tau) when compared to non-demented control patients. Left panels show representative pictures of blotting images (full-length blots are shown in Supplementary Data). Right panel shows percentage of optical density (O.D.) values relativized to the control group, as mean ± SEM. βIII-tubulin, detyrosinated tubulin (glu-tub) and acetylated tubulin (Ac-tub), but not β-actin, are found significantly decreased in FTLD-tau BA10 frontal cortex when compared to non-demented controls. N = 10 (controls), n = 10 (FTLD-tau). *P < 0.05, Student’s t test. Gapdh is used as internal loading control
Decreased levels of PSD95 and proBDNF in BA10 frontal cortex tissue from patients with frontotemporal lobar degeneration with primary tauopathy (FTLD-tau) when compared to non-demented control patients. Left panels show representative pictures of blotting image, and right panel shows percentage of optical density (O.D.) values relativized to the control group, as mean ± SEM. N = 10 (controls), n = 10 (FTLD-tau). *P < 0.01, Student’s t test. β-actin is used as internal loading control
As previously reported, the anti-AM antibody showed two different bands in the brain at around 14 and 55 kDa (Fig. 4) [11, 13]. The lower band is assigned to proAM protein containing PAMP and AM moieties, while the upper band is purportedly assigned to tubulin-bound ADM peptides [9]. As seen in Fig. 4, significant decreases of proAM (Student’s t test; t(18) = 2.72, P = 0.013) parallel those of microtubule components in FTLD-tau brains, although no changes in tubulin-bound adrenomedullin band were found (t(18) = 0.46, P = 0.33). Since ADM peptides have been shown to decorate microtubules [9], the observed reduction of proAM levels might be part of the general disassembly of microtubules in FTLD-tau brains. However, no associations between microtubule components and proAM or tubulin-bound ADM have been found in FTLD-tau brains (data not shown). In contrast to previous studies that have reported increased ADM in AD brains as a seemingly primary event to microtubule disruption and axonal degeneration [11], the defects of ADM that are observed in FTLD-tau brains might not be primary to the neuropathology of these dementia disorders. Instead, as ADM downregulation results in microtubule stabilization and increased post-translational modifications of tubulin such as acetylation and detyrosination in vitro [9], as well as improved cognitive performance in aged mice [13], it is more likely that proAM reductions in FTLD-tau brain are the result of an adaptive but barely successful response of neurons to counteract microtubule destabilization. Hence, it will be challenging to explore whether pharmacological manipulation of ADM peptides by small molecules (as those reported in [22, 23]) will boost microtubule stabilization under these neurodegenerative conditions. Several microtubule-stabilizing drugs, commonly used in the treatment of cancer, have been tested in animal models of neurodegeneration and they provided particular benefit to tauopathies [24]. In view of the present observations and in line with previous research work, small molecules that specifically target and inhibit ADM peptides should be considered candidates for microtubule-stabilizing therapies to treat FTLD-tau in early stages before massive microtubule disassembly takes place.
Changes of ADM gene products in frontotemporal lobar degeneration with primary tauopathy (FTLD-tau) when compared to non-demented control patients. Left panels show representative pictures of blotting images (full-length blots are shown in Supplementary Data). Right panel shows percentage of optical density (O.D.) values relativized to the control group, as mean ± SEM. ProAM peptides (14 kDa) are significantly decreased while tubulin-associated ADM products (AM-tub, 55 kDa) remain unchanged in FTLD-tau BA10 frontal cortex. N = 10 (controls), n = 10 (FTLD-tau). *P < 0.05, Student’s t test. β-actin is used as internal loading control
References
Mann DMA, Snowden JS (2017) Frontotemporal lobar degeneration: pathogenesis, pathology and pathways to phenotype. Brain Pathol 27:723–736. https://doi.org/10.1111/bpa.12486
Kovacs GG (2015) Invited review: neuropathology of tauopathies: principles and practice. Neuropathol Appl Neurobiol 41:3–23. https://doi.org/10.1111/nan.12208
Revesz T, Holton JL (2003) Anatamopathological spectrum of tauopathies. Mov Disord 18:13–20. https://doi.org/10.1002/mds.10558
Mackenzie IRA, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, Kovacs GG, Ghetti B et al (2010) Nomenclature and nosology for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol 119:1–4. https://doi.org/10.1007/s00401-009-0612-2
Rademakers R, Cruts M, van Broeckhoven C (2004) The role of tau (MAPT) in frontotemporal dementia and related tauopathies. Hum Mutat 24:277–295. https://doi.org/10.1002/humu.20086
Iqbal K, Liu F, Gong C-X, Alonso Adel C, Grundke-Iqbal I (2009) Mechanisms of tau-induced neurodegeneration. Acta Neuropathol 118:53–69. https://doi.org/10.1007/s00401-009-0486-3
Goedert M, Spillantini MG, Cairns NJ, Crowther RA (1992) Tau proteins of Alzheimer paired helical filaments: abnormal phosphorylation of all six brain isoforms. Neuron 8:159–168
Rossi G, Tagliavini F (2015) Frontotemporal lobar degeneration: old knowledge and new insight into the pathogenetic mechanisms of tau mutations. Front Aging Neurosci 7:192. https://doi.org/10.3389/fnagi.2015.00192
Sackett DL, Ozbun L, Zudaire E, Wessner L, Chirgwin JM, Cuttitta F, Martínez A (2008) Intracellular proadrenomedullin-derived peptides decorate the microtubules and contribute to cytoskeleton function. Endocrinology 149:2888–2898. https://doi.org/10.1210/en.2007-1763
Larráyoz IM, Martínez A (2012) Proadrenomedullin N-terminal 20 peptide increases kinesin’s velocity both in vitro and in vivo. Endocrinology 153:1734–1742. https://doi.org/10.1210/en.2011-1685
Ferrero H, Larrayoz IM, Martisova E, Solas M, Howlett DR, Francis PT, Gil-Bea FJ, Martínez A et al (2017) Increased levels of brain adrenomedullin in the neuropathology of Alzheimer’s disease. Mol Neurobiol:1–7. https://doi.org/10.1007/s12035-017-0700-6
Fernandez AP, Masa JS, Guedan MA, Futch HS, Martínez-Murillo R (2016) Adrenomedullin expression in Alzheimer’s brain. Curr Alzheimer Res 13:428–438
Larrayoz IM, Ferrero H, Martisova E, Gil-Bea FJ, Ramírez MJ, Martínez A (2017) Adrenomedullin contributes to age-related memory loss in mice and is elevated in aging human brains. Front Mol Neurosci 10:384. https://doi.org/10.3389/fnmol.2017.00384
Mackenzie IRA, Neumann M, Baborie A, Sampathu DM, du Plessis D, Jaros E, Perry RH, Trojanowski JQ et al (2011) A harmonized classification system for FTLD-TDP pathology. Acta Neuropathol 122:111–113. https://doi.org/10.1007/s00401-011-0845-8
Forman MS, Zhukareva V, Bergeron C, Chin SS, Grossman M, Clark C, Lee VM, Trojanowski JQ (2002) Signature tau neuropathology in gray and white matter of corticobasal degeneration. Am J Pathol 160:2045–2053. https://doi.org/10.1016/S0002-9440(10)61154-6
Pollak D, Cairns N, Lubec G (2003) Cytoskeleton derangement in brain of patients with Down syndrome, Alzheimer’s disease and Pick’s disease. J Neural Transm Suppl:149–158
Ma Q-L, Zuo X, Yang F, Ubeda OJ, Gant DJ, Alaverdyan M, Kiosea NC, Nazari S et al (2014) Loss of MAP function leads to hippocampal synapse loss and deficits in the Morris water maze with aging. J Neurosci 34:7124–7136. https://doi.org/10.1523/JNEUROSCI.3439-13.2014
Rapoport M, Dawson HN, Binder LI, Vitek MP, Ferreira A (2002) Tau is essential to beta-amyloid-induced neurotoxicity. Proc Natl Acad Sci 99:6364–6369. https://doi.org/10.1073/pnas.092136199
Hempen B, Brion JP (1996) Reduction of acetylated alpha-tubulin immunoreactivity in neurofibrillary tangle-bearing neurons in Alzheimer’s disease. J Neuropathol Exp Neurol 55:964–972
Yuesong Gong Y, Lippa CF (2010) Review: disruption of the postsynaptic density in Alzheimer’s disease and other neurodegenerative dementias. Am J Alzheimer’s Dis Other Dementiasr 25:547–555. https://doi.org/10.1177/1533317510382893
Guo T, Noble W, Hanger DP (2017) Roles of tau protein in health and disease. Acta Neuropathol 133:665–704. https://doi.org/10.1007/s00401-017-1707-9
Brunden KR, Trojanowski JQ, Smith AB et al (2014) Microtubule-stabilizing agents as potential therapeutics for neurodegenerative disease. Bioorg Med Chem 22:5040–5049. https://doi.org/10.1016/j.bmc.2013.12.046
Ishikawa T, Chen J, Wang J, Okada F, Sugiyama T, Kobayashi T, Shindo M, Higashino F et al (2003) Adrenomedullin antagonist suppresses in vivo growth of human pancreatic cancer cells in SCID mice by suppressing angiogenesis. Oncogene 22:1238–1242. https://doi.org/10.1038/sj.onc.1206207
Robinson SD, Aitken JF, Bailey RJ, Poyner DR, Hay DL (2009) Novel peptide antagonists of adrenomedullin and calcitonin gene-related peptide receptors: identification, pharmacological characterization, and interactions with position 74 in receptor activity-modifying protein 1/3. J Pharmacol Exp Ther 331:513–521. https://doi.org/10.1124/jpet.109.156448
Acknowledgments
We thank the Brains for Dementia Research (BDR) program for the provision of human brain samples.
Funding Information
H.F. is a recipient of a fellowship from the Ministerio de Educación, Cultura y Deporte (FPU). I.M.L. is supported by a Miguel Servet contract (CP15/00198) from the “Instituto de Salud Carlos III-FEDER” (Fondo Europeo de Desarrollo Regional, a way to build Europe) and A.M. is funded by the Fundación Rioja Salud (FRS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from the patients’ next of kin before collection of brains, and the study was approved by the UK National Research Ethics Service.
Electronic supplementary material
ESM 1
(DOCX 1380 kb)
Rights and permissions
About this article
Cite this article
Ferrero, H., Larrayoz, I.M., Solas, M. et al. Reduced Adrenomedullin Parallels Microtubule Dismantlement in Frontotemporal Lobar Degeneration. Mol Neurobiol 55, 9328–9333 (2018). https://doi.org/10.1007/s12035-018-1079-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1079-8