Abstract
In the past years, major efforts have been made to understand the genetics and molecular pathogenesis of Alzheimer’s disease (AD), which has been translated into extensive experimental approaches aimed at slowing down or halting disease progression. Advances in transgenic (Tg) technologies allowed the engineering of different mouse models of AD recapitulating a range of AD-like features. These Tg models provided excellent opportunities to analyze the bases for the temporal evolution of the disease. Several lines of evidence point to synaptic dysfunction as a cause of AD and that synapse loss is a pathological correlate associated with cognitive decline. Therefore, the phenotypic characterization of these animals has included electrophysiological studies to analyze hippocampal synaptic transmission and long-term potentiation, a widely recognized cellular model for learning and memory. Transgenic mice, along with non-Tg models derived mainly from exogenous application of Aβ, have also been useful experimental tools to test the various therapeutic approaches. As a result, numerous pharmacological interventions have been reported to attenuate synaptic dysfunction and improve behavior in the different AD models. To date, however, very few of these findings have resulted in target validation or successful translation into disease-modifying compounds in humans. Here, we will briefly review the synaptic alterations across the different animal models and we will recapitulate the pharmacological strategies aimed at rescuing hippocampal plasticity phenotypes. Finally, we will highlight intrinsic limitations in the use of experimental systems and related challenges in translating preclinical studies into human clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a devastating neurodegenerative disease that affects more than 35 million people worldwide. AD is characterized by gradual and progressive memory impairment associated with deterioration of daily living activities and behavioral disturbances throughout the course of the disease.
Although there has been substantial progress in the therapeutic approach to AD in the past years with the use of cholinesterase inhibitors and the glutamate-modulating drug memantine, treatment for AD still remains a challenge for physicians. In fact, regardless of the therapy prescribed, the current approaches to AD treatment provide only temporary symptomatic relief and do not inhibit and/or reverse the underlying disease mechanisms. This highlights the urgent need for disease-modifying drugs for AD. There are currently approximately 80 compounds at various stages of clinical investigation for the treatment of AD (www.alzforum.org).
From a neuropathological point of view, the AD brain shows senile (neuritic) plaques, neurofibrillary tangles (NFT), and marked atrophy in the brain [1]. The most severe neuropathological changes occur in the hippocampus, followed by the association cortices and subcortical structures, including the amygdala and nucleus basalis of Meynert [2].
In recent years, however, evidence has accumulated demonstrating that synaptic loss, rather than amyloid beta (Aβ) plaques, NFTs, or neuronal loss, is the best pathological correlate of cognitive impairment [1]. Consequently, AD has been suggested to be a form of synaptic plasticity failure [3]. This theory implies that amplification of the plasticity burden at an early stage, leading to a primarily adaptive upregulation of tau phosphorylation and amyloid β precursor protein (AβPP) turnover, may over time contribute to the formation of Aβ and NFTs and eventually precipitate cell death as the final expression of neuroplasticity failure. Consistent with this hypothesis, some brain regions possess more potential for adaptative mechanisms, with neuronal plasticity and synaptic remodeling being particularly elevated in those areas affected early in AD [4]. This indicates that the processes underlying activity-dependent synaptic plasticity in the adult are particularly susceptible to the primary causes of AD.
Of note, impaired synaptic function of the hippocampus appears to be an early event leading to defective hippocampal-dependent memory processing long before the appearance of amyloid plaque burden and neuronal cell death [1, 5]. Therefore, synaptic plasticity is often used to evaluate the phenotype of AD animal models. Accordingly, within the last 20 years, several electrophysiological studies have been performed on several AD experimental models. These models provide important tools to define the temporal evolution of cellular abnormalities in AD brains and to delineate the basic mechanisms that cause synaptic dysfunction. They have also been instrumental in validating drug targets and designing novel pharmacological strategies.
Here we will summarize how hippocampal plasticity is affected across many of these animal models and describe the main pharmacological approaches utilized to rescue synaptic dysfunction.
Experimental Models of AD
There is no existing animal model that resembles all the cognitive, histopathological, biochemical, and behavioral abnormalities observed in AD patients. However, partial reproduction of AD neuropathology and functional deficits has been achieved either with exogenous application of Aβ or through genetically engineered mouse models of AD. A full review of the different experimental AD models is beyond the scope of this work. For more comprehensive reviews, readers may refer to recent reports [6, 7].
Non-transgenic Models
Based on the cholinergic hypothesis, scopolamine-induced amnesia, excitotoxic lesions of the basal forebrain and aged primates have been widely used in the past to evaluate cognitive impairment. Current symptomatic medications for AD were successfully assessed in these models, but their etiological relevance is low [8]. It was originally thought that Aβ plaques, by causing disruption in neural connectivity and function, were responsible for the cognitive decline in AD patients. However, it is now becoming clear that certain of the soluble Aβ species (i.e., monomeric, oligomeric, and protofibrillary Aβ species) seem to be the primary cause for the functional deficits in rodents and probably also contributes to cognitive impairment in AD patients [9]. For these reasons, an alternative approach consisted in the direct in vitro and in vivo application of different synaptotoxic fragments of Aβ. This provided the opportunity to understand how different Aβ-derived diffusible ligands (ADDLs) impact excitatory synaptic transmission and plasticity in the hippocampus.
There is now substantial evidence that ADDLs of synthetic human Aβ inhibit the maintenance of hippocampal long-term potentiation (LTP) if applied in vitro [10, 11] or following intracerebroventricular (i.c.v.) administration [12–14]. Besides synthetic Aβ, also soluble oligomers of cell-derived naturally secreted human Aβ impair LTP at concentrations similar to those found in human cerebrospinal fluid (CSF). This effect has been observed following in vivo infusion in living rats [15] or by direct application to hippocampal slices [16]. In addition, it was demonstrated that mouse slices perfused with Aβ oligomers extracted from the cerebral cortex of AD patients showed reduced LTP and enhanced long-term depression. These effects were specifically attributable to Aβ dimers [17].
Taken together, these results provide evidence that decreased hippocampal LTP can be directly attributed to biochemically defined assemblies of human Aβ (with low-n soluble oligomers possibly ranging from dimers to dodecamers), in absence of amyloid fibrils or protofibrils. Nonetheless, the exact mechanism(s) by which soluble oligomers interact with plasma membranes and bind to receptor and/or channel proteins thereby affecting signaling pathways required for synaptic plasticity still remains poorly understood. One limiting factor derived from these studies is the inability of exogenously applied Aβ to cross the plasmalemma [18], thus not addressing the potentially relevant role of elevated intracellular Aβ.
Transgenic Models
Transgenic (Tg) mouse models that recapitulate the major hallmarks of AD have been utilized since the early 1990s to explore in detail mechanisms underlying disease pathology. Most Tg models of AD have been engineered by inserting mutated human genes in the mouse genome, first identified in early-onset familial cases of AD (FAD). Hereafter, we summarize electrophysiological studies addressing hippocampal synaptic plasticity in the main Tg models.
AβPP-Derived Models
A first effort to create Tg models consisted in overexpressing the entire sequence of the human AβPP gene [19, 20]. Although AβPP transgene was clearly expressed in the brain, it did not lead to significant plaque deposition or any AD-like neuropathological features. Besides AβPP overexpression, the insertion of human AD mutations provided Tg models with elevated levels of Aβ42 [21, 22]. The single mutations inserted in the AβPP gene represent FAD-linked mutations, which are named the Swedish (swe), the Indiana (ind), the London (Ld), and the Arctic (arc) mutations.
These models display age-dependent plaque deposition, hyperphosphorylated tau, neuroinflammation, oxidative stress, and hippocampal-dependent memory deficits resembling human AD. However, they do not exhibit NFTs, cholinergic deficits, nor neuronal loss [7].
Unfortunately, electrophysiological analysis of hippocampal synaptic transmission and plasticity on AβPP-based models has generated inconsistent results. For example, in one study, APPSWE mice exhibit normal basal transmission but impaired LTP [23], while in another study synaptic transmission was impaired but LTP was normal [24]. The reason for this inconsistency is not known but could perhaps be related to differences in the housing conditions, experimental variables, or prior experience of the animals. In line with this, we have recently demonstrated that the plasticity phenotype can be strongly influenced by the cognitive history of the animal. Thus, while LTP was normal at naïve synapses, it was impaired following training of a spatial task in the AβPP23 model [25].
PS1-Derived Models
Presenilin 1 (PS1) is implicated in the proteolysis of AβPP as part of the γ-secretase complex [26]. Tg mice expressing either a wild-type or mutated presenilin gene fail to develop significant AD-like phenotypes, despite the presence of elevated Aβ [27–30]. In the context of synaptic plasticity, PS1-derived models show a biphasic phenotype with increased LTP in young mice and reduced LTP at later stages [31, 32].
Double Transgenic Mice
When mutant PS1 mice were crossed to mutant AβPP mice, formation of Aβ plaques was greatly accelerated [33], indicating that there is a synergistic interaction between both genes. In these models, plaques are composed of the Aβ40 and Aβ42 fragments and are localized in cortical and hippocampal areas [34, 35]. Behavioral deficits in spatial and recognition memory have been found in double Tg mice [35–37], whereas inconsistency between the electrophysiological findings was observed also for this model (reviewed in [38]). In fact, LTP was either reduced [38] or normal [39], possibly depending on the type of PS1 mutation harbored by the mice.
Triple Transgenic Mice
One of the important limitations of the Tg mice described so far is the lack of NFTs despite the presence of hyperphosphorylated tau protein. Oddo et al. [40] generated the first triple transgenic model (3xTg-AD), harboring PS1 (M146V), AβPPSWE, and microtubule-associated protein tau (MAPT, P301L) transgenes. This model accumulates intraneuronal Aβ and subsequently forms amyloid plaques and MAPT lesions in an age-dependent fashion. Over time these mice also develop synaptic dysfunction, including synaptic transmission and LTP deficits that well correlate with the levels of intraneuronal Aβ [41]. Most recently, new triple Tg lines carrying AβPP, PS2, and tau mutations have been created [42, 43].
Pharmacological Strategies to Rescue Synaptic Dysfunction in Experimental AD
Although the exact pathogenesis of AD remains to be fully defined, several pharmacological approaches for the treatment of AD are under active investigation. In this section we will describe the classes of drugs proven effective to rescue synaptic dysfunction in the different preclinical models of AD (summarized in Table 1). It is beyond the scope of this review to include the rescue achieved by genetic approaches. This has been addressed by a recent review [44].
Targeting Aβ
Currently, the amyloid cascade hypothesis is the most important theory of AD postulating that accumulation of Aβ into plaques is the causative pathological event [45]. Based on this hypothesis, interventions that reduce Aβ load in the brain would be likely to attenuate both the neuropathological changes and functional deficits characterizing AD. Indeed, several different Aβ-lowering strategies have been developed over the past years.
Among these, Aβ fibrillogenesis represents a major target for the therapeutic intervention in AD and related human β-amyloidoses [46]. Certain small-molecule inhibitors of synthetic Aβ fibrillogenesis (RS-0406 and RS-0466) inhibit formation of cell-derived, secreted oligomers of Aβ and prevent the impairment of LTP induced by Aβ [47, 48]. Importantly, this protective effect was achieved only under conditions in which they prevented new oligomer formation [49]. In fact, in order to be effective, inhibitors of fibrillogenesis need to be used at the initial stages of oligomerization thus avoiding a paradoxical enhanced neurotoxicity which may derive from active pre-fibrillar assemblies such as low-n oligomers released following inhibition of fibril formation. For these reasons, a promising strategy consisted in preventing the formation of Aβ by enhancing α-secretase activity or inhibiting either β-secretase or γ-secretase activity.
The first attempt to test the potential effects of targeting γ-secretase was conducted by Walsh et al. [15]. In an intriguing study, these authors showed that the cell penetrant γ-secretase inhibitor DAPM was able to restore LTP disruption after i.c.v. infusion of oligomers of human Aβ in rats. A related study showed that 3 days of oral dosing with the γ-secretase inhibitor MK-560 was sufficient to reverse LTP deficit in 6-month-old Tg2576 mice, at a stage when mice show synaptic dysfunction and behavioral changes before significant plaque deposition [50]. This study also highlights the ability of some γ-secretase inhibitors to cross the blood–brain barrier (BBB). Although inhibition of γ-secretase represents a rational pharmacological approach, serious concerns about their toxicity have been raised due to the fact that γ-secretase can cleave several other membrane proteins, the most relevant of which is the Notch protein. The discovery that some NSAIDs behave as γ-secretase modulators, thereby preventing Aβ42 production by binding to AβPP rather than to γ-secretase, suggested a way to avoid Notch toxicity. In line with this, we have recently demonstrated that oral administration of the novel γ-secretase modulator CHF5074 was able to restore synaptic plasticity in 5-month-old Tg2576 mice, and this effect was associated with reduced hyperphosphorylated tau and intraneuronal Aβ [51]. Notably, CHF5074 is currently undergoing phase II clinical trial evaluation. Beyond targeting γ-secretase, also the pharmacological inhibition of AβPP cleavage by β-secretase rescued synaptic deficits in a mouse modeling familial Danish dementia [52].
Immunotherapy
One of the most promising disease-modifying therapies for AD is immunization against Aβ. Intracerebroventricular injection of naturally secreted human Aβ inhibited LTP in rat hippocampus in vivo, but a monoclonal antibody (6E10) to Aβ completely prevented LTP impairment even when injected after Aβ. Partial protection against the block of LTP was also present in rats that were successfully actively immunized with pre-aggregated Aβ [53]. A later report showed that also a single intraperitoneal (i.p.) injection of the antibody 6E10 was able to rescue LTP deficit observed in Tg Arc mice [54]. More recently, it was suggested that systemic passive immunization achieved with intracardiac injection of the monoclonal anti-Aβ antibody 4G8 was able to prevent the disruption of synaptic plasticity by Aβ dimer-containing human CSF in vivo [55].
These findings provide important evidence that antibodies directed to Aβ can rapidly neutralize the synaptic plasticity-disrupting effects of low-n oligomers of Aβ in the brain. Recently, passive immunization with anti-tau antibodies has been shown to reduce tau pathology and slow down disease progression in two Tg models of tauopathy [56]. However no studies addressed so far have demonstrated whether this treatment could also rescue synaptic dysfunction in preclinical models of AD.
Emerging data highlight how the cellular prion protein PrPC can serve as a receptor for Aβ oligomers. Aβ oligomers suppress LTP in murine hippocampal slices but synaptic activity remains preserved in PrPC null mice [57] and following pretreatment with the anti-PrPC antibody 6D11 [58]. LTP was also prevented when AβPP/PS1 mice were intraperitoneally injected with 6D11 [58]. A further study reported that i.c.v. administration of antigen-binding antibody fragment D13, targeting an unknown Aβ-binding site on PrPC, restored LTP deficit induced by AD brain-derived Aβ [59]. While these findings indicate the potential usefulness of immunotherapeutically targeting the binding of synaptotoxic Aβ assemblies to PrPC, two studies [60, 61] and experiments performed in our laboratory (unpublished data) have generated conflicting results.
Tau Kinase Inhibitors
Microtubule-associated protein tau is abnormally hyperphosphorylated in AD. This is likely the result of an imbalance in kinase and phosphatases activities leading to destabilization of microtubules, damage of neuronal cytoskeletal architecture, compromised neuronal transport, dystrophy, and eventually neuronal death [62]. Primary kinases involved in the phosphorylation of tau include glycogen synthase kinase (GSK-3) and cyclin-dependent protein kinase 5 (Cdk-5), thus representing important targets for pharmacological intervention in AD [63]. Several studies, for example, have demonstrated that inhibition of GSK-3 reverses synaptic dysfunction in different models of AD. Accordingly, the selective GSK-3 inhibitor AR-A014418 prevented LTP impairment by human Aβ42 in wild-type slices [64] and either lithium or kenpaullone, two structurally distinct GSK-3 antagonists, rescued LTP deficit in slices from Tg2576 mice [65]. The latter study also provided evidence that upregulation of mTOR signaling mediates this neuroprotective effect, supporting the idea that mTOR pathway is compromised in this Tg model. Similar results were obtained with the more specific GSK-3 inhibitor CT-99021; this was able to prevent Aβ42-induced impairment of LTP both in organotypic hippocampal cultures and in acute slices from 4- to 5-week-old rats [66]. Additionally it was found that Aβ42-induced impairment of LTP was absent in caspase 3 KO mice and that it was inhibited in neurons in organotypic slices that had been transfected with a mutant form of Akt1 that was resistant to cleavage by this caspase [66]. This led to the hypothesis that activation of caspase 3 leads to cleavage of Akt1, thereby removing a tonic inhibition of GSK-3. Besides GSK-3, the pharmacological blockade of Cdk-5 with either butyrolactone or roscovitine also prevented the Aβ-mediated inhibition of LTP [67], confirming previous studies showing that Cdk inhibitors successfully prevent Aβ-induced neurotoxicity [68].
In addition, therapies that stabilize microtubules by compensating for the loss of tau function are nowadays under investigation. Indeed, the reduction in microtubule integrity has been proposed to be an important factor in synaptic dysfunction [69]. Accordingly, taxol was able to protect against synaptic loss in response to lysosomal stress [69]. However, to date, no studies addressing their protective potential in the context of synaptic function have been conducted.
Phosphatase Inhibitors
A growing body of evidence suggests that phosphatases and kinases antagonistically regulate the balance of synaptic strength, thereby serving as a gate for LTP and memory storage [70]. In support of this general model, Aβ-induced LTP deficits could be the consequence of increased phosphatases activity that may shift the gating balance of synaptic plasticity.
Accordingly, it has been shown that blockade of the calcineurin (PP2B) activity with FK506 or cyclosporin A completely prevented Aβ-induced LTP deficits in the hippocampal dentate gyrus [71]. Furthermore the pharmacological inhibition of PP1 with tautomycin was able to reverse the defect in synaptic plasticity in acute hippocampal slices from Tg Arc mice and AβPP/PS1 model [54]. Notably, also genetic inactivation of the striatal-enriched protein tyrosine phosphatase (STEP) reverses cognitive and cellular deficits observed in the triple Tg mouse model [72]. Taken together, these results support an important role for phosphatases in the mechanisms of Aβ oligomer-mediated toxicity, highlighting these proteins as promising targets for the development of potential therapeutic approaches in AD.
Drugs Acting on Cholinergic Transmission
Different strategies have been undertaken to improve cholinergic neurotransmission. These include the increasing of acetylcholine synthesis, facilitation of presynaptic acetylcholine release, stimulation of cholinergic muscarinic and nicotinic receptors, and inhibition of acetylcholine metabolism with cholinesterase inhibitors. A growing body of evidence suggests that Aβ peptide impairs nicotinic acetylcholine receptor (nAChR) function, even though the mechanism remains poorly understood. On the other hand, Aβ42 was found to have a beneficial effect on synaptic plasticity at picomolar concentrations (as found in healthy brains) via the activation of presynaptic α7 nAChRs [73].
Experimental evidence suggests that α4β2 and α7 seem to be required for the Aβ-induced suppression of LTP. Accordingly, diihydro-beta-erythroidine, a selective α4β2 antagonist and methyllycaconitine (MLA), a selective α7 nAChR antagonist, have both proven effective in attenuating Aβ31–35-mediated LTP impairment [74, 75]. Conversely, another study failed to observe any protective effect of MLA, although a different fragment (Aβ42) was used [67]. A further report suggested a protective effect of the α7 agonist dimethoxybenzylidine against Aβ-induced loss of LTP [76]. The different findings may be due to concentration-dependent actions of Aβ, as low levels activate and high levels desensitize α7 [77] and/or interact with other nAChRs subtypes [78]. These data further suggest that the effect of Aβ could be independent from a direct interaction between Aβ and nAChRs.
Also the effect of nicotine has been evaluated in different experimental models of AD. Both acute and chronic nicotine treatments were found to enhance LTP via α7 receptors [79]. Accordingly, recent work showed a protective effect of chronic nicotine treatment in a rat model of AD [80, 81], although a paradoxical depressive effect of nicotine on the impairment of LTP caused by i.c.v. injection of Aβ40 was previously found [82]. Besides nicotine, also donepezil, a widely used drug for the treatment of AD, had neuroprotective effects on synaptic plasticity following Aβ42 [83].
Aβ also exerts effects on the cholinergic system by interacting with G protein-coupled muscarinic acetylcholine receptors (mAChRs). It is widely believed that M2 receptors are reduced in the brains of AD patients [84]. Notably, perfusion of medial septum slices with Aβ40 reduced excitatory transmission and this effect was blocked by calcicludine (a selective L-type Ca2+ channel antagonist) and by pirenzepine, an mAChR antagonist [85]. Interestingly, AβPP/PS1 mice display synaptic dysfunction, which was associated with a decrease in the ability of endogenous mAChR activation to reduce basal glutamatergic transmission in the CA1 area of the hippocampus [86], suggesting that muscarinic receptor dysfunction is among the causes of functional impairment.
Drugs Acting on Glutamate Receptors
There is a growing body of evidence that Aβ soluble oligomers can cause perturbation of glutamatergic signaling, affecting in particular N-methyl-d-aspartate (NMDA) and also metabotropic glutamate receptors (mGluRs). Support for a role of NMDA receptors (NMDARs) in the cognitive deficits of AD is also provided by the current use of memantine in clinical practice. Memantine acts as an uncompetitive inhibitor of NMDARs at therapeutic concentrations [87, 88]. Accordingly, if bath applied at a therapeutically relevant concentration, it has been found to reverse LTP deficiency against the rapid disruptive effects of soluble Aβ42 both in the CA1 [89] and in the DG [90] of the hippocampus.
Aβ42 has been shown to co-immunoprecipitate with the GluN1 and GluN2A subunits of the NMDA receptor [91], and its oligomers bind to excitatory synapses expressing NR1 and NR2B receptors [92]. Moreover, a previous study demonstrated that Aβ activates STEP, which dephosphorylates a regulatory tyrosine site (tyr1472) on the GluN2B subunit, leading to internalization of NMDA receptors [93].
The notion that soluble Aβ-induced impairment of LTP in the CA1 region of hippocampus requires GluN2B-containing NMDARs has been supported by the rescuing effects afforded by the two selective NR2B antagonist ifenprodil and Ro 25-6981 [74, 89]. In an effort to characterize the potential therapeutic value of other allosteric sites on glutamate receptors as alternative targets in the treatment of AD, also MPEP, a specific negative allosteric modulator (NAM) against mGlu5 receptors [94], has been successfully tested [67]. In fact, MPEP can reverse the Aβ42 oligomer-induced inhibition of LTP at nanomolar concentrations [89].
Anti-inflammatory Drugs
Converging lines of evidence suggest that neuroinflammatory processes play important roles in the pathogenesis of neurodegenerative diseases. Accordingly, postmortem examination of AD brain shows extensive evidence of inflammation, including activation and proliferation of glia and elevated concentrations of inflammatory mediators. However, it is not clear how early in the disease process brain inflammation occurs or its relative contribution to disease progression and clinical symptoms [95].
Tumor necrosis factor α (TNFα) is a key cytokine that has been involved in several brain functions, as well as in mediating pro-inflammatory processes in neurodegenerative diseases including AD [96]. Considering that TNFα is increased in the brain of AD patients [97] and that it can directly modulate hippocampal synaptic plasticity [98], the question of whether this cytokine could also mediate the detrimental effects of Aβ on LTP was also addressed. Indeed, the suppression of LTP by Aβ was absent in mutant mice null for TNF receptor type 1 and was prevented by the monoclonal antibody infliximab, the TNF peptide antagonist, and thalidomide, the inhibitor of TNFα production [99].
Besides TNFα, the pro-inflammatory cytokine interleukin 1β (IL-1β) has also been reported to mediate the toxic effects of Aβ peptide [100]. Indeed, i.c.v. administration of interleukin 1 receptor antagonist (IL-1ra) rescued post-tetanic potentiation impairment following injection of Aβ40 [101].
Several studies in transgenic AβPP mice have documented the effects of nonsteroidal anti-inflammatory agents (NSAIDs) on amyloid load and inflammation [102], but only one study so far has addressed the effects of NSAIDs on Aβ-mediated disruption of synaptic plasticity and memory. It was found that both MF tricyclic and Ns-398, two selective COX-2 inhibitors, were effective in preventing the disruption of LTP by synthetic soluble Aβ42. Of note, the same effect was not achieved with the COX-1 inhibitor piroxicam [103].
Antioxidants
Strong evidence has been accumulated to link reactive oxygen species (ROS) with neurodegenerative diseases [104]. In fact, ROS-mediated oxidative stress is used as a valuable AD biomarker and antioxidants offer new hope to patients suffering from AD [105]. However, current clinical trials with antioxidants resulted in mild or no effects to attenuate disease progression and cognitive dysfunction in AD.
Several studies have demonstrated that intraneuronal Aβ is linked to altered mitochondrial function [106]. In fact, Aβ can directly affect mitochondrial function, thus causing oxidative stress [107]. However, the exact mechanisms underlying Aβ-mediated mitochondrial disruption have not yet been fully elucidated. Notably, it recently emerged that Cyclophilin D (CypD), an integral component of the mitochondrial permeability transition pore, can interact with mitochondrial Aβ thereby precipitating neuronal and synaptic stress. In fact, either the genetic removal of this Aβ-binding partner or its pharmacological inhibition with cyclosporin A improved synaptic dysfunction by Aβ42 application. In the presence of the ROS-scavenging enzymes SOD plus catalase, LTP was further alleviated [108]. There are two other structurally distinct ROS scavengers, EUK134 and MitoQ, a synthetic SOD and catalase mimetic and a mitochondria-targeted antioxidant, respectively. They were able to attenuate LTP deficit following Aβ42 application and in AβPP/PS1 mice [109]. A related study demonstrated that rats treated with i.p. injections of SkQR1, a mitochondria-targeted plastoquinone derivative, exhibit normal hippocampal LTP levels in the presence of Aβ42 [110]. This study also highlights the ability of novel antioxidants to cross the BBB.
Insulin and Insulin-Sensitizing Drugs
Several studies show that insulin plays a key role in higher brain functions such as learning and memory [111] and synaptic plasticity [112], whereas impairment of insulin signaling has been linked to neurodegenerative disorders [113]. For example, a clinical study has revealed that the insulin levels in CSF were decreased in patients with sporadic AD [114]. It has also been reported that insulin can protect hippocampal neurons against Aβ-induced cytotoxicity [115], suggesting a potential crosstalk between insulin and Aβ. In a recent work, it was demonstrated that insulin and insulin growth factor 1 (IGF-1) inhibit formation of Aβ oligomers and thus prevent the block of LTP induced by different Aβ fragments [116].
In addition to insulin, also pretreatment with the glucagon-like peptide 1 (GLP-1), which physiologically stimulates insulin release, has been proven effective in reversing LTP following Aβ25–35 [117], Aβ40 [118], and in aged AβPP/PS1 mice [119]. Similar results were also obtained with the novel glucose-dependent insulinotropic polypeptide (GIP), a peptide hormone targeting pancreatic islets to enhance insulin secretion [117].
Insulin-sensitizing drugs such as the thiazolidinediones act as specific agonists of the peroxisome proliferator-activated receptor gamma (PPAR-γ), thereby sensitizing insulin action in the target sites. Different PPAR-γ agonists attenuated the detrimental effects of Aβ40 on LTP [120], and rosiglitazone improved learning and memory deficits in the Tg2576 mouse model [121]. Taken together, these preclinical results raise the possibility that insulin and insulin-sensitizing drugs may serve as therapeutic agents for the treatment of AD.
Neurotrophins
The growing evidence that neurotrophins are essential modulators of synaptic plasticity [122] and that synaptic transmission becomes dysfunctional before the onset of AD raise the question of whether synaptic failure could be ascribed to neurotrophin dysregulation. In line with this notion, a Tg mouse line expressing chronic nerve growth factor (NGF) deprivation displays age-related defects in synaptic plasticity, supporting a “neurotrophic unbalance” hypothesis underlying AD-like neurodegeneration [123]. Accordingly, exogenous supply of neurotrophins was proven effective to restore synaptic alterations in experimental AD. Indeed, it was recently demonstrated that application of neurotrophin 4 (NT4), a neurotrophic factor that signals predominantly through the TrkB receptor tyrosine kinase, prevented LTP deficits induced by Aβ both in the CA1 and DG of rat hippocampal slices [124]. This rescuing effect was associated with enhanced CaMKII autophosphorylation, a signaling event normally stimulated by LTP but suppressed by Aβ42.
On the other hand, Aβ can directly bind to p75 neurotrophin receptors (p75NTR), which are best known for mediating neuronal death and have been consistently linked to the pathology of AD [125]. Therefore, blocking this receptor with the isoleucine derivative LM11A-31 rescued Aβ-induced LTP impairment without affecting baseline transmission [126]. These results highlight neurotrophins or their analogs as a new class of candidate molecule compounds for AD therapeutics. Intriguingly, encapsulated cell biodelivery of NGF to AD patients is currently undergoing phase I clinical trials.
Targeting the CREB–CBP Pathway
Genetic and pharmacological studies in a variety of organisms have demonstrated that cAMP response element-binding protein (CREB)–CREB binding protein (CBP) is a signaling mechanism regulating LTP and is required for long-term memory formation [127]. For these reasons, the synaptic dysfunction associated with experimental AD could result from impaired CREB–CBP signaling. Indeed, reduced expression of the CREB–CBP pathway was found in conditional double knockout mice both lacking both presenilins [128]. In line with this reasoning, several pharmacological approaches targeting the cAMP/PKA/CREB pathway were proven effective in reversing LTP impairment in Tg and non-Tg models of AD.
Accordingly, the phosphodiesterase (PDE) 4 inhibitor rolipram enhanced LTP in wild-type mice [129] and ameliorated LTP deficit either in AβPP/PS1 mice [130] or in acute slices exposed to Aβ [131]. Similarly, also the PDE5 inhibitor sildenafil rescued synaptic deficits in the AβPP/PS1 model, re-establishing normal levels of CREB phosphorylation after tetanic stimulation [132]. Other drugs that stimulate the cAMP/PKA signaling pathway, as the activator of adenylate cyclase forskolin [131] or the β2 adrenoceptor agonist terbutaline [133], showed similar neuroprotective effects.
Considering that cAMP/PKA and NO/cGMP/cGK pathways are known to converge onto CREB to maintain synaptic plasticity [134], another study tested whether targeting the NO/cGMP/cGK/CREB system also alleviated Aβ-induced suppression of LTP. Indeed, application of the NO donor DEA/NO, the sGC stimulator BAY41-2272, and the cGMP analogs 8-Br-cGMP and 8-pCPT-cGMP were all effective in rescuing Aβ-induced LTP impairment and in normalizing phospho-CREB activity during synaptic potentiation [135].
Recent studies have provided evidence that Aβ peptide, possibly through the activation of GluN2B, mGlu5, or α7 nicotinic receptor, could downregulate the ERK/MAPK/CREB cascade, thereby negatively regulating synaptic plasticity. On this line, blockade of the p38 MAPK by SB203580 was able to prevent Aβ-mediated suppression of LTP [67, 74], further confirming that pharmacological modulation of these pathways might be beneficial for AD therapeutics.
Emerging data also point out that epigenetic mechanisms are involved in the altered synaptic function and memory associated with AD [136]. In this scenario, Aβ and tau protein have been shown to interact with CREB/CBP signaling, downregulating CBP and in turn reducing histone acetylation in different preclinical models of neurodegeneration [137, 138]. Therefore, histone deacetylase (HDAC) inhibitors, which are currently being used in clinical trials for the treatment of some forms of cancer, are now also being considered as potential memory enhancers.
Experimental evidence shows that HDAC inhibitors enhance LTP in wild-type mice [139] and rescue hippocampal LTP in AβPP/PS1 mice [140]. In this respect, HDAC inhibitors represent novel compounds to effectively counteract disease progression in AD [141].
Other Neuroprotective Strategies
Several other rescuing strategies were evaluated in experimental AD. These include multitarget drugs or compounds acting with unconventional or still unknown mechanism. Among these, over the past years Humanin (HNG) has received much attention. HNG is a novel peptide cloned from a cDNA library of the occipital lobe of an AD brain [142], which has proven effective against all sorts of AD-relevant insults in vitro. The tyrosine kinase pathway mediated the protective action of HNG against Aβ-induced LTP impairment, since genistein abolished this effect [143, 144].
It has been reported that protein kinase C (PKC) plays a leading role in the cellular signaling cascade targeting protein synthesis and thereby LTP formation [145, 146]. In particular, human studies have shown that PKC and its adaptor protein RACK1 (receptor for activated C kinase 1) are both deficient in AD [147]. In this context, phorbol–myristate–acetate, a membrane-permeable PKC agonist, effectively prevented Aβ31–35-induced deficits in the early and late components of LTP [144].
Another kinase crucially involved in AD pathogenesis is the c-jun N-terminal kinase (JNK) [148]. Indeed Aβ-induced changes in hippocampal plasticity were shown to be dependent upon IL-1β-triggered activation of JNK [149]. Accordingly, different JNK inhibitors rescued LTP deficit induced by synthetic and cell-derived Aβ [67] and in the TgCRND8 mouse model [150].
Overactivation of proteins known as calpains, which are involved in memory formation, has been also linked to AD [151]. Thus, different calpain inhibitors have been shown to reverse synaptic plasticity impairment in AβPP/PS1 slices [37] and in slices exposed to the soluble human Aβ [74].
Other neuroprotective agents reported to rescue hippocampal LTP suppression by different Aβ fragments include the L-type calcium channel (VDCC) blocker verapamil [152], arginine vasopressin [153], neuregulin 1 [154], and the novel phospholipid-based drug formulation VP025 [155]. Protection against Aβ-induced abnormal synaptic function has also been obtained with some traditional medicinal products such as Ginkgo Biloba extracts [156], curcumin [157], huperzine A [158], and the herb mixture Danggui-Shaoyao-San [159].
Other electrophysiological studies performed in Tg models of AD suggest neuroprotective effects of estradiol [160], picrotoxin [161], and the nonselective adrenergic receptor antagonist carvedilol [162].
Limitations of Preclinical Models and Future Challenges
This review has documented how a large variety of pharmacological interventions can rescue synaptic dysfunction in experimental AD, yet this success in rodents has not been translated into successful therapies for humans. There are a number of reasons why preclinical studies may have failed to predict the outcome of clinical studies.
First, the consideration that Tg mice carry FAD mutations, accounting for only 1–10 % of all AD cases in humans, rather than the prevalent sporadic (SAD) form. Also, while these models develop specific hallmarks of AD, they do not recapitulate every aspect of the complex human disease. An important issue that needs to be considered is whether the similar temporal profile of disease progression in AD patients is also conserved in Tg mice. For example, while in Tg mice cognitive deficits precede plaque load, in human patients the latter is more likely to happen first. Second, the weakness with Tg mice is that there is almost no neuronal cell death, differently from the substantial neurodegeneration occurring in the human AD brain.
In general, it can be assumed that animal models of AD are more useful as models of specific disease targets and pathways. For this reason, they serve as tools for testing the efficacy of candidate molecules on drug targets that may be involved in AD pathogenesis. This target-driven approach in animal models has translated over the past years to several therapeutic studies in humans (see Table 1).
Besides the intrinsic limitations of animal models, experimental studies are also susceptible to experimental bias. The most frequently underestimated issues are related to gender- and litter-dependent differences, variances in transgene expression across generations, and diverse genetic background between drug- and placebo-treated groups. Other intrinsic limitations to be considered in translation are differences between mouse/human species including diversities in cerebrovascular anatomy, neuronal network physiology, disease susceptibility, and perhaps most importantly dynamics of drug-target interactions. For these reasons, therapeutic studies carried out in vivo should include a complete pharmacokinetics/pharmacodynamics profile to maintain appropriate dosing and timing of treatment. Toxicological studies should be addressed in order to minimize putative off-target influence on the results. Ideally, positive results should be re-evaluated in multiple lines of mice, preferably in several laboratories, and negative results should also be published in the scientific literature. Certainly, raising the quality of preclinical research can make the translation to human clinical trials more efficient and reliable.
Conclusions
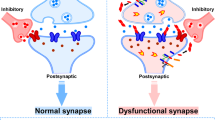
Looking ahead, prevalence of AD will overtake cardiovascular diseases and AIDS in its prevalence (World Health Organization). Therefore, continuous efforts are geared towards the discovery of new anti-AD agents. The plastic nature of synapses and their early involvement in the cognitive decline associated with AD models provide new potential targets for pharmacological intervention. It is becoming clear that therapeutic approaches cannot be directed to single targets, but to a combination of targets which should be considered for effective therapies (summarized in Fig. 1). Certainly, to ensure a successful outcome, therapy should start at the very early stage. In addition, highly sensitive and specific biomarkers for diagnosing AD need to be identified in order to recognize AD patients at the onset of the disease. Besides diagnosis, markers would also be essential to follow-up disease progression, to monitor the efficacy of treatments during preclinical studies, and to predict potential therapeutic effects in humans.
Proposed molecular mechanisms behind the experimental treatment approaches to Alzheimer’s disease. Crucial to AD is the differential processing of the integral membrane protein amyloid β precursor protein (AβPP) in the normal versus diseased state. In the normal state, cleavage of APP by α-secretase generates soluble amino-terminal ectodomain of AβPP (sAβPPα) and C83 C-terminal stub. The physiological role of sAβPPα is associated with neuronal survival, neurite outgrowth, synaptic plasticity, and learning and memory. In the disease state, AβPP is sequentially cleaved by β-secretase and γ-secretase to form soluble AβPP (sAβPP). Aβ is secreted into the extracellular spaces and accumulates to form oligomers, fibrils and eventually senile plaques. Aβ40/42 oligomers bind to several surface receptors, disrupt membrane integrity, perturb calcium homeostasis, trigger inflammatory state and mitochondrial oxidative stress, ultimately leading to neuronal cell death. The microtubule-associated protein tau is abnormally hyperphosphorylated in AD and accumulates in neurons forming neurofibrillary tangle. The major sites for pharmacological intervention are also highlighted (see text for details)
In spite of their limitations, experimental models of AD still remain the most important scientific tool to understand the basic mechanisms underlying AD. Indeed, a more careful design of preclinical studies will provide important contributions to the development of the first approved disease-modifying drug for AD.
References
Selkoe DJ (2002) Alzheimer’s disease is a synaptic failure. Science 298:789–791
Arnold SE, Lee VM, Gur RE, Trojanowski JQ (1991) Abnormal expression of two microtubule-associated proteins (MAP2 and MAP5) in specific subfields of the hippocampal formation in schizophrenia. Proc Natl Acad Sci U S A 88:10850–10854
Nisticò R, Collingridge GL (2012) The synaptic basis of Alzheimer’s disease. Eur J Neurodeg Dis 1:21–33
Arendt T (2001) Disturbance of neuronal plasticity is a critical pathogenetic event in Alzheimer’s disease. Int J Dev Neurosci 19:231–245
Tanzi RE (2005) The synaptic Abeta hypothesis of Alzheimer disease. Nat Neurosci 8:977–979
Götz J, Ittner LM (2008) Animal models of Alzheimer’s disease and frontotemporal dementia. Nat Rev Neurosci 9:532–544
Götz J, Eckert A, Matamales M, Ittner LM, Liu X (2011) Modes of Aβ toxicity in Alzheimer’s disease. Cell Mol Life Sci 68:3359–3375
Bartus RT (2000) On neurodegenerative diseases, models, and treatment strategies: lessons learned and lessons forgotten a generation following the cholinergic hypothesis. Exp Neurol 163:495–529
Selkoe DJ (2008) Biochemistry and molecular biology of amyloid beta-protein and the mechanism of Alzheimer’s disease. Handb Clin Neurol 89:245–260
Chen QS, Kagan BL, Hirakura Y, Xie CW (2000) Impairment of hippocampal long-term potentiation by Alzheimer amyloid beta-peptides. J Neurosci Res 60:65–72
Wang HW, Pasternak JF, Kuo H, Ristic H, Lambert MP, Chromy B, Viola KL, Klein WL, Stine WB, Krafft GA, Trommer BL (2002) Soluble oligomers of beta amyloid (1–42) inhibit long-term potentiation but not long-term depression in rat dentate gyrus. Brain Res 924:133–140
Cullen KM, Halliday GM, Double KL, Brooks WS, Creasey H, Broe GA (1997) Cell loss in the nucleus basalis is related to regional cortical atrophy in Alzheimer’s disease. Neuroscience 78:641–652
Itoh Y, Yamada M, Sodeyama N, Suematsu N, Matsushita M, Otomo E, Mizusawa H (1999) Atherosclerosis is not implicated in association of APOE epsilon4 with AD. Neurology 53:236–237
Freir DB, Holscher C, Herron CE (2001) Blockade of long-term potentiation by beta-amyloid peptides in the CA1 region of the rat hippocampus in vivo. J Neurophysiol 85:708–713
Walsh DM, Klyubin I, Fadeeva JV, Cullen WK, Anwyl R, Wolfe MS, Rowan MJ, Selkoe DJ (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 416:535–539
Townsend M, Cleary JP, Mehta T, Hofmeister J, Lesne S, O’Hare E, Walsh DM, Selkoe DJ (2006) Orally available compound prevents deficits in memory caused by the Alzheimer amyloid-beta oligomers. Ann Neurol 60:668–676
Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, Brett FM, Farrell MA, Rowan MJ, Lemere CA, Regan CM, Walsh DM, Sabatini BL, Selkoe DJ (2008) Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat Med 14:837–842
Bi X, Gall CM, Zhou J, Lynch G (2002) Uptake and pathogenic effects of amyloid beta peptide 1-42 are enhanced by integrin antagonists and blocked by NMDA receptor antagonists. Neuroscience 112:827–840
Buxbaum JD, Christensen JL, Ruefli AA, Greengard P, Loring JF (1993) Expression of APP in brains of transgenic mice containing the entire human APP gene. Biochem Biophys Res Commun 197:639–645
Lamb BT, Sisodia SS, Lawler AM, Slunt HH, Kitt CA, Kearns WG, Pearson PL, Price DL, Gearhart JD (1993) Introduction and expression of the 400 kilobase amyloid precursor protein gene in transgenic mice. Nat Genet 5:22–30
Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S, Yang F, Cole G (1996) Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science 274:99–102
Moechars D, Dewachter I, Lorent K, Reversé D, Baekelandt V, Naidu A, Tesseur I, Spittaels K, Haute CV, Checler F, Godaux E, Cordell B, Van Leuven F (1999) Early phenotypic changes in transgenic mice that overexpress different mutants of amyloid precursor protein in brain. J Biol Chem 274:6483–6492
Chapman PF, White GL, Jones MW, Cooper-Blacketer D, Marshall VJ, Irizarry M, Younkin L, Good MA, Bliss TV, Hyman BT, Younkin SG, Hsiao KK (1999) Impaired synaptic plasticity and learning in aged amyloid precursor protein transgenic mice. Nat Neurosci 2:271–276
Fitzjohn SM, Morton RA, Kuenzi F, Rosahl TW, Shearman M, Lewis H, Smith D, Reynolds DS, Davies CH, Collingridge GL, Seabrook GR (2001) Age-related impairment of synaptic transmission but normal long-term potentiation in transgenic mice that overexpress the human APP695SWE mutant form of amyloid precursor protein. J Neurosci 21:4691–4698
Middei S, Roberto A, Berretta N, Panico MB, Lista S, Bernardi G, Mercuri NB, Ammassari-Teule M, Nisticò R (2010) Learning discloses abnormal structural and functional plasticity at hippocampal synapses in the APP23 mouse model of Alzheimer’s disease. Learn Mem 17:236–240
Wakabayashi T, De Strooper B (2008) Presenilins: members of the gamma-secretase quartets, but part-time soloists too. Physiology (Bethesda) 23:194–204
Borchelt DR, Thinakaran G, Eckman CB, Lee MK, Davenport F, Ratovitsky T, Prada CM, Kim G, Seekins S, Yager D, Slunt HH, Wang R, Seeger M, Levey AI, Gandy SE, Copeland NG, Jenkins NA, Price DL, Younkin SG, Sisodia SS (1996) Familial Alzheimer’s disease-linked presenilin 1 variants elevate Abeta1-42/1-40 ratio in vitro and in vivo. Neuron 17:1005–1013
Chui DH, Tanahashi H, Ozawa K, Ikeda S, Checler F, Ueda O, Suzuki H, Araki W, Inoue H, Shirotani K, Takahashi K, Gallyas F, Tabira T (1999) Transgenic mice with Alzheimer presenilin 1 mutations show accelerated neurodegeneration without amyloid plaque formation. Nat Med 5:560–564
Citron M, Westaway D, Xia W, Carlson G, Diehl T, Levesque G, Johnson-Wood K, Lee M, Seubert P, Davis A, Kholodenko D, Motter R, Sherrington R, Perry B, Yao H, Strome R, Lieberburg I, Rommens J, Kim S, Schenk D, Fraser P, St George Hyslop P, Selkoe DJ (1997) Mutant presenilins of Alzheimer’s disease increase production of 42-residue amyloid beta-protein in both transfected cells and transgenic mice. Nat Med 3:67–72
Duff K, Eckman C, Zehr C, Yu X, Prada CM, Perez-tur J, Hutton M, Buee L, Harigaya Y, Yager D, Morgan D, Gordon MN, Holcomb L, Refolo L, Zenk B, Hardy J, Younkin S (1996) Increased amyloid-beta42(43) in brains of mice expressing mutant presenilin 1. Nature 383:710–713
Auffret A, Gautheron V, Repici M, Kraftsik R, Mount HT, Mariani J, Rovira C (2009) Age-dependent impairment of spine morphology and synaptic plasticity in hippocampal CA1 neurons of a presenilin 1 transgenic mouse model of Alzheimer’s disease. J Neurosci 29:10144–10152
Auffret A, Gautheron V, Mattson MP, Mariani J, Rovira C (2010) Progressive age-related impairment of the late long-term potentiation in Alzheimer’s disease presenilin-1 mutant knock-in mice. J Alzheim Dis 19:1021–1033
Holcomb L, Gordon MN, McGowan E, Yu X, Benkovic S, Jantzen P, Wright K, Saad I, Mueller R, Morgan D, Sanders S, Zehr C, O’Campo K, Hardy J, Prada CM, Eckman C, Younkin S, Hsiao K, Duff K (1998) Accelerated Alzheimer-type phenotype in transgenic mice carrying both mutant amyloid precursor protein and presenilin 1 transgenes. Nat Med 4:97–100
McGowan E, Sanders S, Iwatsubo T, Takeuchi A, Saido T, Zehr C, Yu X, Uljon S, Wang R, Mann D, Dickson D, Duff K (1999) Amyloid phenotype characterization of transgenic mice overexpressing both mutant amyloid precursor protein and mutant presenilin 1 transgenes. Neurobiol Dis 6:231–244
Howlett DR, Richardson JC, Austin A, Parsons AA, Bate ST, Davies DC, Gonzalez MI (2004) Cognitive correlates of Abeta deposition in male and female mice bearing amyloid precursor protein and presenilin-1 mutant transgenes. Brain Res 1017:130–136
Dinamarca MC, Arrázola M, Toledo E, Cerpa WF, Hancke J, Inestrosa NC (2008) Release of acetylcholinesterase (AChE) from beta-amyloid plaques assemblies improves the spatial memory impairments in APP-transgenic mice. Chem Biol Interact 175:142–149
Trinchese F, Fa’ M, Liu S, Zhang H, Hidalgo A, Schmidt SD, Yamaguchi H, Yoshii N, Mathews PM, Nixon RA, Arancio O (2008) Inhibition of calpains improves memory and synaptic transmission in a mouse model of Alzheimer disease. J Clin Invest 118:2796–2807
Volianskis A, Køstner R, Mølgaard M, Hass S, Jensen MS (2010) Episodic memory deficits are not related to altered glutamatergic synaptic transmission and plasticity in the CA1 hippocampus of the APPswe/PS1δE9-deleted transgenic mice model of β-amyloidosis. Neurobiol Aging 31:1173–1187
Fitzjohn SM, Kuenzi F, Morton RA, Rosahl TW, Lewis H, Smith D, Seabrook GR, Collingridge GL (2010) A study of long-term potentiation in transgenic micover-expressing mutant forms of both amyloid precursor protein and presenilin. Mol Brain 14:3–21
Oddo S, Caccamo A, Kitazawa M, Tseng BP, LaFerla FM (2003) Amyloid deposition precedes tangle formation in a triple transgenic model of Alzheimer’s disease. Neurobiol Aging 24:1063–1070
Oddo S, Caccamo A, Shepherd JD, Murphy MP, Golde TE, Kayed R, Metherate R, Mattson MP, Akbari Y, LaFerla FM (2003) Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron 39:409–421
Rhein V, Song X, Wiesner A, Ittner LM, Baysang G, Meier F, Ozmen L, Bluethmann H, Dröse S, Brandt U, Savaskan E, Czech C, Götz J, Eckert A (2009) Amyloid-beta and tau synergistically impair the oxidative phosphorylation system in triple transgenic Alzheimer’s disease mice. Proc Natl Acad Sci U S A 106:20057–20062
Grueninger F, Bohrmann B, Czech C, Ballard TM, Frey JR, Weidensteiner C, von Kienlin M, Ozmen L (2010) Phosphorylation of Tau at S422 is enhanced by Abeta in TauPS2APP triple transgenic mice. Neurobiol Dis 37:294–306
Marchetti C, Marie H (2011) Hippocampal synaptic plasticity in Alzheimer’s disease: what have we learned so far from transgenic models? Rev Neurosci 22:373–402
Hardy J, Allsop D (1991) Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends Pharmacol Sci 12:383–388
Findeis MA (2002) Peptide inhibitors of beta amyloid aggregation. Curr Top Med Chem 2:417–423
Nakagami Y, Nishimura S, Murasugi T, Kubo T, Kaneko I, Meguro M, Marumoto S, Kogen H, Koyama K, Oda T (2002) A novel compound RS-0466 reverses beta-amyloid-induced cytotoxicity through the Akt signaling pathway in vitro. Eur J Pharmacol 457:11–17
Nakagami Y, Nishimura S, Murasugi T, Kaneko I, Meguro M, Marumoto S, Kogen H, Koyama K, Oda T (2002) A novel beta-sheet breaker, RS-0406, reverses amyloid beta-induced cytotoxicity and impairment of long-term potentiation in vitro. Br J Pharmacol 137:676–682
Walsh DM, Klyubin I, Shankar GM, Townsend M, Fadeeva JV, Betts V, Podlisny MB, Cleary JP, Ashe KH, Rowan MJ, Selkoe DJ (2005) The role of cell-derived oligomers of Abeta in Alzheimer’s disease and avenues for therapeutic intervention. Biochem Soc Trans 33:1087–1090
Townsend M, Qu Y, Gray A, Wu Z, Seto T, Hutton M, Shearman MS, Middleton RE (2010) Oral treatment with a gamma-secretase inhibitor improves long-term potentiation in a mouse model of Alzheimer’s disease. J Pharmacol Exp Ther 333:110–119
Balducci C, Mehdawy B, Mare L, Giuliani A, Lorenzini L, Sivilia S, Giardino L, Calzà L, Lanzillotta A, Sarnico I, Pizzi M, Usiello A, Viscomi AR, Ottonello S, Villetti G, Imbimbo BP, Nisticò G, Forloni G, Nisticò R (2011) The γ-secretase modulator CHF5074 restores memory and hippocampal synaptic plasticity in plaque-free Tg2576 mice. J Alzheim 24:799–816
Tamayev R, Matsuda S, Arancio O, D’Adamio L (2011) β- but not γ-secretase proteolysis of APP causes synaptic and memory deficits in a mouse model of dementia. EMBO Mol Med. doi:10.1002/emmm.201100195
Klyubin I, Walsh DM, Lemere CA, Cullen WK, Shankar GM, Betts V, Spooner ET, Jiang L, Anwyl R, Selkoe DJ, Rowan MJ (2008) Amyloid beta protein immunotherapy neutralizes Abeta oligomers that disrupt synaptic plasticity in vivo. Nat Med 11:556–561
Knobloch M, Farinelli M, Konietzko U, Nitsch RM, Mansuy IM (2007) Abeta oligomer-mediated long-term potentiation impairment involves protein phosphatase 1-dependent mechanisms. J Neurosci 27:7648–7653
Klyubin I, Betts V, Welzel AT, Blennow K, Zetterberg H, Wallin A, Lemere CA, Cullen WK, Peng Y, Wisniewski T, Selkoe DJ, Anwyl R, Walsh DM, Rowan MJ (2008) Amyloid beta protein dimer-containing human CSF disrupts synaptic plasticity: prevention by systemic passive immunization. J Neurosci 28:4231–4237
Chai X, Wu S, Murray TK, Kinley R, Cella CV, Sims H, Buckner N, Hanmer J, Davies P, O’Neill MJ, Hutton ML, Citron M (2011) Passive immunization with anti-Tau antibodies in two transgenic models: reduction of Tau pathology and delay of disease progression. J Biol Chem 286:34457–34467
Laurén J, Gimbel DA, Nygaard HB, Gilbert JW, Strittmatter SM (2009) Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers. Nature 457:1128–1132
Chung E, Ji Y, Sun Y, Kascsak RJ, Kascsak RB, Mehta PD, Strittmatter SM, Wisniewski T (2010) Anti-PrPC monoclonal antibody infusion as a novel treatment for cognitive deficits in an Alzheimer’s disease model mouse. BMC Neurosci 11:130
Barry AE, Klyubin I, Mc Donald JM, Mably AJ, Farrell MA, Scott M, Walsh DM, Rowan MJ (2011) Alzheimer’s disease brain-derived amyloid-β-mediated inhibition of LTP in vivo is prevented by immunotargeting cellular prion protein. J Neurosci 31:7259–7263
Balducci C, Beeg M, Stravalaci M, Bastone A, Sclip A, Biasini E, Tapella L, Colombo L, Manzoni C, Borsello T, Chiesa R, Gobbi M, Salmona M, Forloni G (2010) Synthetic amyloid-beta oligomers impair long-term memory independently of cellular prion protein. Proc Natl Acad Sci U S A 107:2295–2300
Kessels HW, Nguyen LN, Nabavi S, Malinow R (2010) The prion protein as a receptor for amyloid-beta. Nature 466:E3–E4, discussion E4-5
Iqbal K, Liu F, Gong CX, Grundke-Iqbal I (2010) Tau in Alzheimer disease and related tauopathies. Curr Alzheimer Res 7:656–664
Pritchard SM, Dolan PJ, Vitkus A, Johnson GV (2011) The toxicity of tau in Alzheimer disease: turnover, targets and potential therapeutics. J Cell Mol Med 15:1621–1635
Shipton OA, Leitz JR, Dworzak J, Acton CE, Tunbridge EM, Denk F, Dawson HN, Vitek MP, Wade-Martins R, Paulsen O, Vargas-Caballero M (2011) Tau protein is required for amyloid {beta}-induced impairment of hippocampal long-term potentiation. J Neurosci 31:1688–1692
Ma T, Hoeffer CA, Capetillo-Zarate E, Yu F, Wong H, Lin MT, Tampellini D, Klann E, Blitzer RD, Gouras GK (2010) Dysregulation of the mTOR pathway mediates impairment of synaptic plasticity in a mouse model of Alzheimer’s disease. PLoS One 5 pii: e12845
Jo J, Whitcomb DJ, Olsen KM, Kerrigan TL, Lo SC, Bru-Mercier G, Dickinson B, Scullion S, Sheng M, Collingridge G, Cho K (2011) Aβ(1–42) inhibition of LTP is mediated by a signaling pathway involving caspase-3, Akt1 and GSK-3β. Nat Neurosci 14:545–547
Wang Q, Walsh DM, Rowan MJ, Selkoe DJ, Anwyl R (2004) Block of long-term potentiation by naturally secreted and synthetic amyloid beta-peptide in hippocampal slices is mediated via activation of the kinases c-Jun N-terminal kinase, cyclin-dependent kinase 5, and p38 mitogen-activated protein kinase as well as metabotropic glutamate receptor type 5. J Neurosci 24:3370–3378
Alvarez A, Toro R, Cáceres A, Maccioni RB (1999) Inhibition of tau phosphorylating protein kinase cdk5 prevents beta-amyloid-induced neuronal death. FEBS Lett 459:421–426
Butler D, Bendiske J, Michaelis ML, Karanian DA, Bahr BA (2007) Microtubule-stabilizing agent prevents protein accumulation-induced loss of synaptic markers. Eur J Pharmacol 562:20–27
Norris CM, Halpain S, Foster TC (1998) Reversal of age-related alterations in synaptic plasticity by blockade of L-type Ca2+ channels. J Neurosci 18:3171–3179
Chen QS, Wei WZ, Shimahara T, Xie CW (2002) Alzheimer amyloid beta-peptide inhibits the late phase of long-term potentiation through calcineurin-dependent mechanisms in the hippocampal dentate gyrus. Neurobiol Learn Mem 77:354–371
Zhang Y, Kurup P, Xu J, Carty N, Fernandez SM, Nygaard HB, Pittenger C, Greengard P, Strittmatter SM, Nairn AC, Lombroso PJ (2010) Genetic reduction of striatal-enriched tyrosine phosphatase (STEP) reverses cognitive and cellular deficits in an Alzheimer’s disease mouse model. Proc Natl Acad Sci U S A 107:19014–19019
Puzzo D, Privitera L, Leznik E, Fà M, Staniszewski A, Palmeri A, Arancio O (2008) Picomolar amyloid-beta positively modulates synaptic plasticity and memory in hippocampus. J Neurosci 28:14537–14545
Li S, Jin M, Koeglsperger T, Shepardson NE, Shankar GM, Selkoe DJ (2011) Soluble Aβ oligomers inhibit long-term potentiation through a mechanism involving excessive activation of extrasynaptic NR2B-containing NMDA receptors. J Neurosci 31:6627–6638
Wu MN, He YX, Guo F, Qi JS (2008) Alpha4beta2 nicotinic acetylcholine receptors are required for the amyloid beta protein-induced suppression of long-term potentiation in rat hippocampal CA1 region in vivo. Brain Res Bull 77:84–90
Chen L, Yamada K, Nabeshima T, Sokabe M (2006) α7 nicotinic acetylcholine receptor as a target to rescue deficit in hippocampal LTP induction in beta-amyloid infused rats. Neuropharmacology 50:254–268
Dineley KT, Bell KA, Bui D, Sweatt JD (2002) Beta-amyloid peptide activates alpha 7 nicotinic acetylcholine receptors expressed in Xenopus oocytes. J Biol Chem 277:25056–25061
Oddo S, LaFerla FM (2006) The role of nicotinic acetylcholine receptors in Alzheimer’s disease. J Physiol Paris 99:172–179
Matsuyama S, Matsumoto A, Enomoto T, Nishizaki T (2000) Activation of nicotinic acetylcholine receptors induces long-term potentiation in vivo in the intact mouse dentate gyrus. Eur J Neurosci 12:3741–3747
Srivareerat M, Tran TT, Alzoubi KH, Alkadhi KA (2009) Chronic psychosocial stress exacerbates impairment of cognition and long-term potentiation in beta-amyloid rat model of Alzheimer’s disease. Biol Psychiatry 65:918–926
Alkadhi KA, Alzoubi KH, Srivareerat M, Tran TT (2011) Chronic psychosocial stress exacerbates impairment of synaptic plasticity in β-amyloid rat model of Alzheimer’s disease: prevention by nicotine. Curr Alzheimer Res 8:718–731
Freir DB, Herron CE (2003) Nicotine enhances the depressive actions of A beta 1–40 on long-term potentiation in the rat hippocampal CA1 region in vivo. J Neurophysiol 89:2917–2922
Kapai NA, Bukanova JV, Solntseva EI, Skrebitsky VG (2011) Donepezil in a narrow concentration range augments control and impaired by beta-amyloid peptide hippocampal LTP in NMDAR-independent manner. Cell Mol Neurobiol 32:219–226
Nordberg A, Alafuzoff I, Winblad B (1992) Nicotinic and muscarinic subtypes in the human brain: changes with aging and dementia. J Neurosci Res 31:103–111
Santos-Torres J, Fuente A, Criado JM, Riolobos AS, Heredia M, Yajeya J (2007) Glutamatergic synaptic depression by synthetic amyloid beta-peptide in the medial septum. J Neurosci Res 85:634–648
Goto Y, Niidome T, Hongo H, Akaike A, Kihara T, Sugimoto H (2008) Impaired muscarinic regulation of excitatory synaptic transmission in the APPswe/PS1dE9 mouse model of Alzheimer’s disease. Eur J Pharmacol 583:84–91
Lipton SA (2007) Pathologically-activated therapeutics for neuroprotection: mechanism of NMDA receptor block by memantine and S-nitrosylation. Curr Drug Targets 8:621–632
Parsons CG, Stöffler A, Wn D (2007) Memantine: a NMDA receptor antagonist that improves memory by restoration of homeostasis in the glutamatergic system—too little activation is bad, too much is even worse. Neuropharmacology 53:699–723
Rammes G, Hasenjäger A, Sroka-Saidi K, Deussing JM, Parsons CG (2011) Therapeutic significance of NR2B-containing NMDA receptors and mGluR5 metabotropic glutamate receptors in mediating the synaptotoxic effects of β-amyloid oligomers on long-term potentiation (LTP) in murine hippocampal slices. Neuropharmacology 60:982–990
Klyubin I, Wang Q, Reed MN, Irving EA, Upton N, Hofmeister J, Cleary JP, Anwyl R, Rowan MJ (2011) Protection against Aβ-mediated rapid disruption of synaptic plasticity and memory by memantine. Neurobiol Aging 32:614–623
Venkitaramani DV, Chin J, Netzer WJ, Gouras GK, Lesne S, Malinow R, Lombroso PJ (2007) Beta-amyloid modulation of synaptic transmission and plasticity. J Neurosci 27:11832–11837
Lacor PN, Buniel MC, Furlow PW, Clemente AS, Velasco PT, Wood M, Viola KL, Klein WL (2007) Abeta oligomer-induced aberrations in synapse composition, shape, and density provide a molecular basis for loss of connectivity in Alzheimer’s disease. J Neurosci 27:796–807
Snyder EM, Nong Y, Almeida CG, Paul S, Moran T, Choi EY, Nairn AC, Salter MW, Lombroso PJ, Gouras GK, Greengard P (2005) Regulation of NMDA receptor trafficking by amyloid-beta. Nat Neurosci 8:1051–1058
Gasparini F, Lingenhöhl K, Stoehr N, Flor PJ, Heinrich M, Vranesic I, Biollaz M, Allgeier H, Heckendorn R, Urwyler S, Varney MA, Johnson EC, Hess SD, Rao SP, Sacaan AI, Santori EM, Veliçelebi G, Kuhn R (1999) 2-methyl-6-(phenylethynyl)-pyridine (MPEP), a potent, selective and systemically active mGlu5 receptor antagonist. Neuropharmacology 38:1493–1503
Wyss-Coray T (2006) Inflammation in Alzheimer disease: driving force, bystander or beneficial response? Nat Med 12:1005–1015
Perry VH, Nicoll JA, Holmes C (2010) Microglia in neurodegenerative disease. Nat Rev Neurol 6:193–201
Tarkowski E, Blennow K, Wallin A, Tarkowski A (1999) Intracerebral production of tumor necrosis factor-alpha, a local neuroprotective agent, in Alzheimer disease and vascular dementia. J Clin Immunol 19:223–230
Stellwagen D, Malenka RC (2006) Synaptic scaling mediated by glial TNF-alpha. Nature 440:1054–1059
Wang Q, Wu J, Rowan MJ, Anwyl R (2005) Beta-amyloid inhibition of long-term potentiation is mediated via tumor necrosis factor. Eur J Neurosci 22:2827–2832
Mrak RE, Griffin WS (2001) Interleukin-1, neuroinflammation, and Alzheimer’s disease. Neurobiol Aging 22:903–908
Schmid AW, Lynch MA, Herron CE (2009) The effects of IL-1 receptor antagonist on beta amyloid mediated depression of LTP in the rat CA1 in vivo. Hippocampus 19:670–676
McGeer PL, McGeer EG (2007) NSAIDs and Alzheimer disease: epidemiological, animal model and clinical studies. Neurobiol Aging 28:639–647
Kotilinek LA, Westerman MA, Wang Q, Panizzon K, Lim GP, Simonyi A, Lesne S, Falinska A, Younkin LH, Younkin SG, Rowan M, Cleary J, Wallis RA, Sun GY, Cole G, Frautschy S, Anwyl R, Ashe KH (2008) Cyclooxygenase-2 inhibition improves amyloid-beta-mediated suppression of memory and synaptic plasticity. Brain 131:651–664
Lin MT, Beal MF (2006) Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443:787–795
Aliev G, Obrenovich ME, Reddy VP, Shenk JC, Moreira PI, Nunomura A, Zhu X, Smith MA, Perry G (2008) Antioxidant therapy in Alzheimer’s disease: theory and practice. Mini Rev Med Chem 8:1395–1406
Caspersen C, Wang N, Yao J, Sosunov A, Chen X, Lustbader JW, Xu HW, Stern D, McKhann G, Yan SD (2005) Mitochondrial Abeta: a potential focal point for neuronal metabolic dysfunction in Alzheimer’s disease. FASEB J 19:2040–2041
Cardoso SM, Santos S, Swerdlow RH, Oliveira CR (2001) Functional mitochondria are required for amyloid beta-mediated neurotoxicity. FASEB J 15:1439–1441
Du H, Guo L, Fang F, Chen D, Sosunov AA, McKhann GM, Yan Y, Wang C, Zhang H, Molkentin JD, Gunn-Moore FJ, Vonsattel JP, Arancio O, Chen JX, Yan SD (2008) Cyclophilin D deficiency attenuates mitochondrial and neuronal perturbation and ameliorates learning and memory in Alzheimer’s disease. Nat Med 14:1097–1105
Ma T, Hoeffer CA, Wong H, Massaad CA, Zhou P, Iadecola C, Murphy MP, Pautler RG, Klann E (2011) Amyloid β-induced impairments in hippocampal synaptic plasticity are rescued by decreasing mitochondrial superoxide. J Neurosci 31:5589–5595
Kapay NA, Isaev NK, Stelmashook EV, Popova OV, Zorov DB, Skrebitsky VG, Skulachev VP (2011) In vivo injected mitochondria-targeted plastoquinone antioxidant SkQR1 prevents β-amyloid-induced decay of long-term potentiation in rat hippocampal slices. Biochemistry (Mosc) 76:1367–1370
Dou JT, Chen M, Dufour F, Alkon DL, Zhao WQ (2005) Insulin receptor signaling in long-term memory consolidation following spatial learning. Learn Mem 12:646–655
van der Heide LP, Kamal A, Artola A, Gispen WH, Ramakers GM (2005) Insulin modulates hippocampal activity-dependent synaptic plasticity in a N-methyl-d-aspartate receptor and phosphatidyl-inositol-3-kinase-dependent manner. J Neurochem 94:1158–1166
Gasparini L, Xu H (2003) Potential roles of insulin and IGF-1 in Alzheimer’s disease. Trends Neurosci 26:404–406
Craft S, Peskind E, Schwartz MW, Schellenberg GD, Raskind M, Porte D Jr (1998) Cerebrospinal fluid and plasma insulin levels in Alzheimer’s disease: relationship to severity of dementia and apolipoprotein E genotype. Neurology 50:164–168
Takadera T, Sakura N, Mohri T, Hashimoto T (1993) Toxic effect of a beta-amyloid peptide (beta 22–35) on the hippocampal neuron and its prevention. Neurosci Lett 161:41–44
Lee CC, Kuo YM, Huang CC, Hsu KS (2009) Insulin rescues amyloid beta-induced impairment of hippocampal long-term potentiation. Neurobiol Aging 30:377–387
Gault VA, Hölscher C (2008) GLP-1 agonists facilitate hippocampal LTP and reverse the impairment of LTP induced by beta-amyloid. Eur J Pharmacol 587:112–117
Wang XH, Li L, Hölscher C, Pan YF, Chen XR, Qi JS (2010) Val8-glucagon-like peptide-1 protects against Aβ1-40-induced impairment of hippocampal late-phase long-term potentiation and spatial learning in rats. Neuroscience 170:1239–1248
Gengler S, McClean PL, McCurtin R, Gault VA, Hölscher C (2012) Val(8)GLP-1 rescues synaptic plasticity and reduces dense core plaques in APP/PS1 mice. Neurobiol Aging 33:265–276
Costello DA, O’Leary DM, Herron C (2005) Agonists of peroxisome proliferator-activated receptor-gamma attenuate the Abeta-mediated impairment of LTP in the hippocampus in vitro. Neuropharmacology 49:359–366
Pedersen WA, McMillan PJ, Kulstad JJ, Leverenz JB, Craft S, Haynatzki GR (2006) Rosiglitazone attenuates learning and memory deficits in Tg2576 Alzheimer mice. Exp Neurol 199:265–273
Kang H, Schuman EM (1995) Long-lasting neurotrophin-induced enhancement of synaptic transmission in the adult hippocampus. Science 267:1658–1662
Houeland G, Romani A, Marchetti C, Amato G, Capsoni S, Cattaneo A, Marie H (2010) Transgenic mice with chronic NGF deprivation and Alzheimer’s disease-like pathology display hippocampal region-specific impairments in short- and long-term plasticities. J Neurosci 30:13089–13094
Zeng Y, Zhao D, Xie CW (2010) Neurotrophins enhance CaMKII activity and rescue amyloid-β-induced deficits in hippocampal synaptic plasticity. J Alzheim Dis 21:823–831
Sotthibundhu A, Sykes AM, Fox B, Underwood CK, Thangnipon W, Coulson EJ (2008) Beta-amyloid(1–42) induces neuronal death through the p75 neurotrophin receptor. J Neurosci 28:3941–3946
Yang T, Knowles JK, Lu Q, Zhang H, Arancio O, Moore LA, Chang T, Wang Q, Andreasson K, Rajadas J, Fuller GG, Xie Y, Massa SM, Longo FM (2008) Small molecule, non-peptide p75 ligands inhibit Abeta-induced neurodegeneration and synaptic impairment. PLoS One 3:e3604
Alberini CM (2009) Transcription factors in long-term memory and synaptic plasticity. Physiol Rev 89:121–145
Saura CA, Choi SY, Beglopoulos V, Malkani S, Zhang D, Shankaranarayana Rao BS, Chattarji S, Kelleher RJ 3rd, Kandel ER, Duff K, Kirkwood A, Shen J (2004) Loss of presenilin function causes impairments of memory and synaptic plasticity followed by age-dependent neurodegeneration. Neuron 42:23–36
Barad M, Bourtchouladze R, Winder DG, Golan H, Kandel E (1998) Rolipram, a type IV-specific phosphodiesterase inhibitor, facilitates the establishment of long-lasting long-term potentiation and improves memory. Proc Natl Acad Sci U S A 95:15020–15025
Gong B, Vitolo OV, Trinchese F, Liu S, Shelanski M, Arancio O (2004) Persistent improvement in synaptic and cognitive functions in an Alzheimer mouse model after rolipram treatment. J Clin Invest 114:1624–1634
Vitolo OV, Sant’Angelo A, Costanzo V, Battaglia F, Arancio O, Shelanski M (2002) Amyloid beta-peptide inhibition of the PKA/CREB pathway and long-term potentiation: reversibility by drugs that enhance cAMP signaling. Proc Natl Acad Sci U S A 99:13217–13221
Puzzo D, Staniszewski A, Deng SX, Privitera L, Leznik E, Liu S, Zhang H, Feng Y, Palmeri A, Landry DW, Arancio O (2009) Phosphodiesterase 5 inhibition improves synaptic function, memory, and amyloid-beta load in an Alzheimer’s disease mouse model. J Neurosci 29:8075–8086
Wang QW, Rowan MJ, Anwyl R (2009) Inhibition of LTP by beta-amyloid is prevented by activation of beta2 adrenoceptors and stimulation of the cAMP/PKA signaling pathway. Neurobiol Aging 30:1608–1613
Lu YF, Kandel ER, Hawkins RD (1999) Nitric oxide signaling contributes to late-phase LTP and CREB phosphorylation in the hippocampus. J Neurosci 19:10250–10261
Puzzo D, Vitolo O, Trinchese F, Jacob JP, Palmeri A, Arancio O (2005) Amyloid-beta peptide inhibits activation of the nitric oxide/cGMP/cAMP-responsive element-binding protein pathway during hippocampal synaptic plasticity. J Neurosci 25:6887–6897
Chouliaras L, Rutten BP, Kenis G, Peerbooms O, Visser PJ, Verhey F, van Os J, Steinbusch HW, van den Hove DL (2010) Epigenetic regulation in the pathophysiology of Alzheimer’s disease. Prog Neurobiol 90:498–510
Abel T, Zukin RS (2008) Epigenetic targets of HDAC inhibition in neurodegenerative and psychiatric disorders. Curr Opin Pharmacol 8:57–64
Rouaux C, Jokic N, Mbebi C, Boutillier S, Loeffler JP, Boutillier AL (2003) Critical loss of CBP/p300 histone acetylase activity by caspase-6 during neurodegeneration. EMBO J 22:6537–6549
Alarcón JM, Malleret G, Touzani K, Vronskaya S, Ishii S, Kandel ER, Barco A (2004) Chromatin acetylation, memory, and LTP are impaired in CBP+/− mice: a model for the cognitive deficit in Rubinstein-Taybi syndrome and its amelioration. Neuron 42:947–959
Francis YI, Fà M, Ashraf H, Zhang H, Staniszewski A, Latchman DS, Arancio O (2009) Dysregulation of histone acetylation in the APP/PS1 mouse model of Alzheimer’s disease. J Alzheim Dis 18:131–139
Mikaelsson MA, Miller CA (2011) The path to epigenetic treatment of memory disorders. Neurobiol Learn Mem. doi:10.1016/j.nlm.2011.02.003
Hashimoto Y, Niikura T, Tajima H, Yasukawa T, Sudo H, Ito Y, Kita Y, Kawasumi M, Kouyama K, Doyu M, Sobue G, Koide T, Tsuji S, Lang J, Kurokawa K, Nishimoto I (2001) A rescue factor abolishing neuronal cell death by a wide spectrum of familial Alzheimer’s disease genes and Abeta. Proc Natl Acad Sci U S A 98:6336–6341
Guo F, Jing W, Ma CG, Wu MN, Zhang JF, Li XY, Qi JS (2010) [Gly(14)]-humanin rescues long-term potentiation from amyloid beta protein-induced impairment in the rat hippocampal CA1 region in vivo. Synapse 64:83–91
Zhang W, Miao J, Hao J, Li Z, Xu J, Liu R, Cao F, Wang R, Chen J, Li Z (2009) Protective effect of S14G-humanin against beta-amyloid induced LTP inhibition in mouse hippocampal slices. Peptides 30:1197–1202
Chen W, Wieraszko A, Hogan MV, Yang HA, Kornecki E, Ehrlich YH (1996) Surface protein phosphorylation by ecto-protein kinase is required for the maintenance of hippocampal long-term potentiation. Proc Natl Acad Sci U S A 93:8688–8693
Roisin MP, Leinekugel X, Tremblay E (1997) Implication of protein kinase C in mechanisms of potassium-induced long-term potentiation in rat hippocampal slices. Brain Res 745:222–230
Battaini F, Pascale A (2005) Protein kinase C signal transduction regulation in physiological and pathological aging. Ann N Y Acad Sci 1057:177–192
Ploia C, Antoniou X, Sclip A, Grande V, Cardinetti D, Colombo A, Canu N, Benussi L, Ghidoni R, Forloni G, Borsello T (2011) JNK plays a key role in tau hyperphosphorylation in Alzheimer’s disease models. J Alzheim Dis 26:315–329
Minogue AM, Schmid AW, Fogarty MP, Moore AC, Campbell VA, Herron CE, Lynch MA (2003) Activation of the c-Jun N-terminal kinase signaling cascade mediates the effect of amyloid-beta on long term potentiation and cell death in hippocampus: a role for interleukin-1beta? J Biol Chem 278:27971–27980
Sclip A, Antoniou X, Colombo A, Camici GG, Pozzi L, Cardinetti D, Feligioni M, Veglianese P, Bahlmann FH, Cervo L, Balducci C, Costa C, Tozzi A, Calabresi P, Forloni G, Borsello T (2011) c-Jun N-terminal kinase regulates soluble Aβ oligomers and cognitive impairment in AD mouse model. J Biol Chem 286:43871–43880
Raynaud F, Marcilhac A (2006) Implication of calpain in neuronal apoptosis. A possible regulation of Alzheimer’s disease. FEBS J 273:3437–3443
Freir DB, Herron CE (2003) Inhibition of L-type voltage dependent calcium channels causes impairment of long-term potentiation in the hippocampal CA1 region in vivo. Brain Res 967:27–36
Jing W, Guo F, Cheng L, Zhang JF, Qi JS (2009) Arginine vasopressin prevents amyloid beta protein-induced impairment of long-term potentiation in rat hippocampus in vivo. Neurosci Lett 450:306–310
Min SS, An J, Lee JH, Seol GH, Im JH, Kim HS, Baik TK, Woo RS (2011) Neuregulin-1 prevents amyloid β-induced impairment of long-term potentiation in hippocampal slices via ErbB4. Neurosci Lett 505:6–9
Miller AM, Piazza A, Martin DS, Walsh M, Mandel A, Bolton AE, Lynch MA (2009) The deficit in long-term potentiation induced by chronic administration of amyloid-beta is attenuated by treatment of rats with a novel phospholipid-based drug formulation, VP025. Exp Gerontol 44:300–304
Vitolo O, Gong B, Cao Z, Ishii H, Jaracz S, Nakanishi K, Arancio O, Dzyuba SV, Lefort R, Shelanski M (2009) Protection against beta-amyloid induced abnormal synaptic function and cell death by Ginkgolide. J Neurobiol Aging 30:257–265
Ahmed T, Enam SA, Gilani AH (2010) Curcuminoids enhance memory in an amyloid-infused rat model of Alzheimer’s disease. Neuroscience 169:1296–1306
Ye JW, Cai JX, Wang LM, Tang XC (1999) Improving effects of huperzine A on spatial working memory in aged monkeys and young adult monkeys with experimental cognitive impairment. J Pharmacol Exp Ther 288:814–819
Hu ZY, Liu G, Yuan H, Yang S, Zhou WX, Zhang YX, Qiao SY (2010) Danggui-Shaoyao-San and its active fraction JD-30 improve Abeta-induced spatial recognition deficits in mice. J Ethnopharmacol 128:365–372
Yun SH, Park KA, Kwon S, Woolley CS, Sullivan PM, Pasternak JF, Trommer BL (2007) Estradiol enhances long term potentiation in hippocampal slices from aged apoE4-TR mice. Hippocampus 17:1153–1157
Yoshiike Y, Kimura T, Yamashita S, Furudate H, Mizoroki T, Murayama M, Takashima A (2008) GABA(A) receptor-mediated acceleration of aging-associated memory decline in APP/PS1 mice and its pharmacological treatment by picrotoxin. PLoS One 3:e3029
Arrieta-Cruz I, Wang J, Pavlides C, Pasinetti GM (2010) Carvedilol reestablishes long-term potentiation in a mouse model of Alzheimer’s disease. J Alzheim Dis 21:649–654
Acknowledgments
We apologize to our colleagues whose work may have inadvertently been omitted. We thank Dr. D’Amelio for critical reading of the manuscript. GLC is supported by the MRC and Korean WCU Program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nisticò, R., Pignatelli, M., Piccinin, S. et al. Targeting Synaptic Dysfunction in Alzheimer’s Disease Therapy. Mol Neurobiol 46, 572–587 (2012). https://doi.org/10.1007/s12035-012-8324-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-012-8324-3