Abstract
In this study, the impact of plasma cell maturity on the prognoses of multiple myeloma (MM) patients in the era of novel agents was investigated. Myeloma cell maturity was classified via immunophenotyping: myeloma cells showing mature plasma cell 1 (MPC-1)-positive and CD49e-positive cells were considered mature type; MPC-1-positive and CD49e-negative cells were considered intermediate type; and MPC-1-negative cells were considered immature type. This study included 87 newly diagnosed MM patients who were initially treated with bortezomib and/or chemotherapy. Myeloma cell maturity was a critical factor affecting overall survival (OS) in the cohort, with median OS not reached in mature-type, 50 months in intermediate-type, and 20 months in immature-type cells. Multivariate analysis showed that immature type and stage III according to the International Staging System were both independent prognostic factors affecting OS. The findings of this study demonstrate the clinical importance of myeloma cell classification according to immunophenotyping using MPC-1 and CD49e antibodies to determine patient prognosis in this era of novel therapeutic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recent development of novel agents, including bortezomib and lenalidomide, has led to dramatic improvements in the outcomes of patients with multiple myeloma (MM) [1–3]. A large-scale phase III VISTA study testing the efficacy and safety of first-line bortezomib use in combination with melphalan plus prednisolone (VMP) as compared to melphalan plus prednisolone (MP) demonstrated that VMP was superior to MP in terms of overall survival (OS), progression-free survival, and time to next treatment, suggesting that bortezomib in addition to MP can improve patient outcomes [4, 5]. In fact, it has been suggested that treatment regimens including bortezomib may be able to overcome the adverse prognostic impacts of specific abnormalities, such as t(4;14) or chromosome 13q deletion, that are known to be the most critical predictors of the prognoses of patients who have been treated with chemotherapeutic agents [6–9]. Thus, investigations for prognostic factors other than cytogenetics are needed in patients with MM in the era of novel therapeutic agents.
Previous studies have examined the impact of myeloma cell maturity, as classified by morphology, on the prognosis of patients who were treated with chemotherapy without novel agents. Those studies demonstrated that MM patients with plasma cells showing blastic morphology confer poorer prognoses and aggressive clinical features [10, 11]. Although plasma cell maturity may also play a critical role in the prediction of prognosis in the era of novel agents, objective evaluation methods for the classification of myeloma cell maturation have not yet been described.
Immunophenotyping by flow cytometric analysis is widely available for the diagnosis of, evaluation of minimal residual disease in, and prognostic prediction of a variety of hematologic malignancies. Kawano et al. have established a method for the classification of plasma cell maturity according to surface antigen expression as assessed by flow cytometric analysis [12–14]. Plasma cell maturity can be determined with antibodies against mature plasma cell 1 (MPC-1) and very late antigen 5 (CD49e). Plasma cell maturity is classified according to the following combination of these antigens: MPC-1-negative is considered immature type, MPC-1-positive and CD49e-negative is considered intermediate type, and MPC-1-positive and CD49e-positive is considered mature type [12–15]. Unlike normal plasma cells, MM cells are often classified as the intermediate to immature type [12, 14]. Based on these previous studies, we hypothesized that plasma cell maturity as assessed by immunophenotyping may play a critical role in predicting prognosis in patients with MM in the era of novel therapeutic agents. To verify our hypothesis, we investigated the association between prognosis and myeloma cell immunophenotyping in this study and herein describe the significance of myeloma cell maturity on prognosis in the era of novel agents.
Patients and methods
Patients
We conducted a retrospective review of patient data between December 2006 and January 2016. This study comprised patients who were diagnosed with symptomatic MM and received initial anti-MM therapy between December 2006 and August 2015, because bortezomib was approved by Japanese health insurance and became available in December 2006. Patients were eligible regardless of treatment strategy (first-line use of bortezomib or not, or bortezomib treatment in combination with a cytotoxic agent or not). This study was approved by the research ethics board of Nihon University Itabashi Hospital (Identifier: RK-151208-06, approved in January 2016), and the study was conducted in accordance with the principles of the Declaration of Helsinki.
Flow cytometry
Immunophenotyping was performed primarily on bone marrow samples that were collected at the time of diagnosis or prior to bortezomib treatment at Bio Medical Laboratories, Inc. (Tokyo, Japan). Myeloma cells were analyzed using standard immunofluorescence methods and monoclonal antibodies against the CD19, CD38, CD45, CD49e, CD56, and MPC-1 surface antigens. The CD38bright/side scatterlow population represented the plasma cell fraction, and flow cytometric data were analyzed when abnormal plasma cell fractions, for example, CD38bright/CD19− cells, were detected. Samples were considered positive when at least 20 % of the myeloma cells expressed this antigen profile, as previously described [16, 17].
Statistical analysis
Fisher’s exact and Mann–Whitney U tests were used to determine statistical significance. OS was defined as the period from the date on which initial anti-MM treatment was initiated to the date of death. The Kaplan–Meier method was used to estimate OS, and a log-rank test was used to compare groups in relation to OS. Factors that could affect clinical outcome were analyzed using univariate and multivariate Cox proportional hazard regression models. A p value less than 0.05 was considered statistically significant. Statistical analysis was performed using EZR (Saitama Medical Center, Jichi Medical University), which is a graphical user interface using the R programming language (The R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org/) [18].
Results
Patient characteristics and treatment
Of the patients diagnosed with symptomatic MM through the observation period, we were able to analyze 87 via flow cytometry. The characteristics of these enrolled patients are presented in Table 1. The median age at diagnosis was 67 years (range, 36–83 years), and this study included 48 men and 39 women. In the entire cohort, 5 cases were categorized as mature, 65 as intermediate, and 17 as immature type. No significant differences were detected in patient characteristics such as age, sex, immunoglobulin subtype, light chain subtype, or the levels of hemoglobin, platelets, IgG in IgG-type, serum creatinine, β 2 microglobulin, albumin, or ISS among groups classified according to myeloma cell maturity. The probability that patients were administered bortezomib as a first-line treatment was similar between patients with mature-, intermediate-, or immature-type myeloma cells (p = 0.864). Regarding actual treatments administered to patients in the cohort, 79 (91 %) patients received bortezomib, 35 (40 %) lenalidomide, 9 (10 %) thalidomide, and only 4 (5 %) aPBSCT. Five patients were not administered either bortezomib or lenalidomide during the study period.
Myeloma cell maturity and prognosis
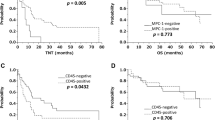
In the cohort, myeloma cell maturity was a critical factor affecting OS as shown by longer median OS in patients with mature or intermediate type as compared to immature type cells, with median OS not reached (NR), 50, and 20 months, respectively (Fig. 1a). In addition, advanced-stage patients as assessed by ISS had poorer prognoses (Fig. 1b).
Kaplan–Meier curves for overall survival (OS) according to myeloma cell maturity as assessed by immunophenotyping profile (a) and international staging system (ISS, B). Myeloma cell maturity was classified as mature plasma cell 1 (MPC-1) positive and CD49e positive (mature), MPC-1 positive and CD49e negative (intermediate), and MPC-1 negative (immature). OS significantly differed according to myeloma cell maturity, with shorter survival in patients with immature-type cells. ISS stage also significantly influenced OS
Prognostic factors for overall survival
Univariate analysis showed that, as compared to MPC-1-positive (mature to intermediate) patients, OS was significantly shorter in MPC-1-negative (immature) patients. Univariate analysis also revealed that ISS stage III was associated with shorter OS. Multivariate analysis confirmed that both MPC-1 negativity and ISS stage III were independent adverse prognostic factors for OS (Table 2). First-line use of bortezomib was not advantageous as compared to its use in a refractory or relapsed setting (Table 2). Other factors such as age, sex, or immunoglobulin subtype had no impact on OS (Table 2).
Discussion
This is the first report demonstrating the importance of myeloma cell maturity as a critical prognostic factor as assessed by flow cytometric analysis. Furthermore, most patients investigated in this study were treated with novel agents such as bortezomib and lenalidomide, and rarely with aPBSCT. Thus, myeloma cell maturity can be considered a critical prognostic factor in the era of novel agents.
Importantly, MM patients showing MPC-1 negativity (immature-type cells) are believed to be refractory to chemotherapeutic agents [19]. In addition, thalidomide treatment has been shown to be ineffective in reducing MPC-1-negative myeloma cells [19]. Taking the inferior treatment results in patients lacking MPC-1 expression as compared to those expressing MPC-1 into consideration, a bortezomib-based regimen may be unable to eradicate MPC-1-negative clones regardless of the combination of cytotoxic agents or thalidomide. Altogether, these prior findings and those of the present study imply that the contribution of a bortezomib-containing regimen is limited. Indeed, one recent randomized study evaluating the efficacy and safety of three bortezomib-containing regimens [bortezomib plus dexamethasone (VD), VMP, and VD in combination with thalidomide (VTD)] showed equivalent treatment efficacy between groups, suggesting that both VTD and VMP confer no advantage as compared to VD alone [20]. However, another randomized study testing the safety and efficacy of regimens that consisted of VD in combination with cyclophosphamide (VCD) and/or lenalidomide (VRD) demonstrated that treatment with VRD yielded higher response rates than VCD [21]. Considering these prior results, we hypothesized that bortezomib in combination with lenalidomide might effectively eradicate immature myeloma cells.
We herein propose a possible mechanism to explain how myeloma cell maturity influences the outcomes of patients in the era of novel agents. Bortezomib leads to an unfolded protein response (UPR), which is a host defense mechanism against the accumulation of misfolded proteins whereby endoplasmic reticulum (ER)-mediated apoptosis is induced when a surplus accumulation of unfolded protein occurs [22–24]. Importantly, ER stress induced by the accumulation of misfolded proteins is regulated by spliced X-box binding protein 1 (XBP1) [25]. XBP1 is a critical transcription factor that regulates plasma cell differentiation from mature B cells [25, 26], and its overexpression is common in myeloma cells [27]. XBP1 knockout has been demonstrated to impair plasma cell differentiation [26]. Thus, lower levels of XBP1 expression are hypothesized to impair plasma cell maturation and lead to insufficient bortezomib-induced, ER stress-mediated myeloma cell apoptosis. Indeed, recent studies evaluating the prognostic significance of XBP1 mRNA expression in bortezomib-treated MM patients demonstrated that patients whose myeloma cells express lower levels of XBP1 mRNA have inferior treatment responses and unfavorable prognoses [28, 29]. Collectively, close correlations between plasma cell maturation, XBP1 expression, induction of ER stress-induced apoptosis, and treatment efficacy with bortezomib confer new insights into myeloma therapy in the era of novel agents. Based on the body of evidence, we believe that these relationships may explain the underlying mechanisms of bortezomib resistance that occur during myeloma treatment. We thus conclude that consecutive immunophenotyping for MPC-1 and CD49e may be useful for treatment decisions in a refractory or relapsed setting.
In this study, cytogenetic analyses using fluorescence in situ hybridization to detect specific cytogenetic abnormalities were not typically performed, representing one of the study’s limitations. Another limitation of this study is possible selection bias, because not all patient samples underwent flow cytometric analysis at the time of diagnosis or before lenalidomide treatment. Furthermore, the treatment strategy was not uniform at our institution because of patient comorbidities, physician discretion, or the unavailability of bortezomib treatment as an initial therapy. Although the effect of initial bortezomib on prognosis was assumed, as has been previously demonstrated, to lead to improved outcomes in patients treated with a first-line bortezomib-containing regimen [4], the current study showed no impact of initial bortezomib treatment. Because we rapidly switched to the bortezomib regimen in patients initially treated with chemotherapy who poorly responded to treatment or had severe renal impairment, the impact of first-line bortezomib might have been obscured. Indeed, the time to bortezomib administration (second-line or later) from initial treatment was relatively short in the study population (median 5 months; range 0–44 months).
In conclusion, patients with MM were stratified according to their myeloma cell maturity, as assessed by immunophenotyping of MPC-1 and CD49e, to predict outcomes. Our findings provide a basis for treatment planning in this era of novel therapeutic agents.
References
Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med. 2003;348:2609–17.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352:2487–98.
Dimopoulos M, Spencer A, Attal M, Prince HM, Harousseau J-L, Dmoszynska A, et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med. 2007;357:2123–32.
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, et al. Persistent overall survival benefit and no increased risk of second malignancies with bortezomib-melphalan-prednisone versus melphalan-prednisone in patients with previously untreated multiple myeloma. J Clin Oncol. 2013;31:448–55.
Mateos M-V, Richardson PG, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, et al. Bortezomib plus melphalan and prednisone compared with melphalan and prednisone in previously untreated multiple myeloma: updated follow-up and impact of subsequent therapy in the phase III VISTA trial. J Clin Oncol. 2010;28:2259–66.
Avet-Loiseau H, Leleu X, Roussel M, Moreau P, Guerin-Charbonnel C, Caillot D, et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol. 2010;28:4630–4.
Chang H, Trieu Y, Qi X, Xu W, Stewart KA, Reece D. Bortezomib therapy response is independent of cytogenetic abnormalities in relapsed/refractory multiple myeloma. Leuk Res. 2007;31:779–82.
Jagannath S, Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, et al. Bortezomib appears to overcome the poor prognosis conferred by chromosome 13 deletion in phase 2 and 3 trials. Leukemia. 2007;21:151–7.
Sagaster V, Ludwig H, Kaufmann H, Odelga V, Zojer N, Ackermann J, et al. Bortezomib in relapsed multiple myeloma: response rates and duration of response are independent of a chromosome 13q-deletion. Leukemia. 2007;21:164–8.
Bartl R, Frisch B, Burkhardt R, Fateh-Moghadam A, Mahl G, Gierster P, et al. Bone marrow histology in myeloma: its importance in diagnosis, prognosis, classification and staging. Br J Haematol. 1982;51:361–75.
Bartl R, Frisch B, Fateh-Moghadam A, Kettner G, Jaeger K, Sommerfeld W. Histologic classification and staging of multiple myeloma: a retrospective and prospective study of 674 cases. Am J Clin Pathol. 1987;87:342–55.
Harada H, Kawano MM, Huang N, Harada Y, Iwato K, Tanabe O, et al. Phenotypic difference of normal plasma cells from mature myeloma cells. Blood. 1993;81:2658–63.
Otsuyama K, Asaoku H, Kawano MM. An increase in MPC-1- and MPC-1-CD45+ immature myeloma cells in the progressive states of bone marrow plasmacytosis: the revised phenotypic classification of monoclonal marrow plasmacytosis (MOMP-2005). Int J Hematol. 2006;83:39–43.
Kawano MM, Mihara K, Tsujimoto T, Huang N, Kuramoto A. A new phenotypic classification of bone marrow plasmacytosis. Int J Hematol. 1995;61:179–88.
Fujii R, Ishikawa H, Mahmoud MS, Asaoku H, Kawano MM. MPC-1-CD49e- immature myeloma cells include CD45+ subpopulations that can proliferate in response to IL-6 in human myelomas. Br J Haematol. 1999;105:131–40.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A, et al. Proposals for the immunological classification of acute leukemias” European group for the immunological characterization of leukemias (EGIL). Leukemia. 1995;9:1783–6.
Iriyama N, Asou N, Miyazaki Y, Yamaguchi S, Sato S, Sakura T, et al. Normal karyotype acute myeloid leukemia with the CD7+ CD15 + CD34+ HLA-DR+ immunophenotype is a clinically distinct entity with a favorable outcome. Ann Hematol. 2014;93:957–63.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Kuroda Y, Sakai A, Okikawa Y, Munemasa S, Katayama Y, Hyodo H, et al. The maturation of myeloma cells correlates with sensitivity to chemotherapeutic agents. Int J Hematol. 2005;81:335–41.
Niesvizky R, Flinn IW, Rifkin R, Gabrail N, Charu V, Clowney B, et al. Community-based phase IIIB trial of three UPFRONT bortezomib-based myeloma regimens. J Clin Oncol. 2015;33:3921–9.
Kumar S, Flinn I, Richardson PG, Hari P, Callander N, Noga SJ, et al. Randomized, multicenter, phase 2 study (EVOLUTION) of combinations of bortezomib, dexamethasone, cyclophosphamide, and lenalidomide in previously untreated multiple myeloma. Blood. 2012;119:4375–82.
Mujtaba T, Dou QP. Advances in the understanding of mechanisms and therapeutic use of bortezomib. Discov Med. 2011;12:471–80.
Vincenz L, Jäger R, O’Dwyer M, Samali A. Endoplasmic reticulum stress and the unfolded protein response: targeting the Achilles heel of multiple myeloma. Mol Cancer Ther. 2013;12:831–43.
Obeng EA, Carlson LM, Gutman DM, Harrington WJ, Lee KP, Boise LH. Proteasome inhibitors induce a terminal unfolded protein response in multiple myeloma cells. Blood. 2006;107:4907–16.
Lin K-I, Tunyaplin C, Calame K. Transcriptional regulatory cascades controlling plasma cell differentiation. Immunol Rev. 2003;194:19–28.
Iwakoshi NN, Lee A-H, Vallabhajosyula P, Otipoby KL, Rajewsky K, Glimcher LH. Plasma cell differentiation and the unfolded protein response intersect at the transcription factor XBP-1. Nat Immunol. 2003;4:321–9.
Munshi NC, Hideshima T, Carrasco D, Shammas M, Auclair D, Davies F, et al. Identification of genes modulated in multiple myeloma using genetically identical twin samples. Blood. 2004;103:1799–806.
Bagratuni T, Wu P, Gonzalez de Castro D, Davenport EL, Dickens NJ, Walker BA, et al. XBP1s levels are implicated in the biology and outcome of myeloma mediating different clinical outcomes to thalidomide-based treatments. Blood. 2010;116:250–3.
Gambella M, Rocci A, Passera R, Gay F, Omedè P, Crippa C, et al. High XBP1 expression is a marker of better outcome in multiple myeloma patients treated with bortezomib. Haematologica. 2014;99:e14–6.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
KM and YH received lecture fees and honoraria from Celgene K.K. and Janssen Pharmaceutical K.K. MT received honoraria from Janssen Pharmaceutical K.K. The remaining authors have no competing interests to declare.
Rights and permissions
About this article
Cite this article
Iriyama, N., Miura, K., Hatta, Y. et al. Plasma cell maturity as a predictor of prognosis in multiple myeloma. Med Oncol 33, 87 (2016). https://doi.org/10.1007/s12032-016-0803-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-016-0803-3